Abstract
The risk of osteomyelitis is increased in the premature and critically ill neonate. Although potential sites of bacterial entry are present in many of these infants, the source of infection frequently cannot be established. This study was performed to assess the possible role of bacterial translocation from the intestine in the origin of bone infection using models of breast-fed and formula-fed rat pups. Newborn Sprague-Dawley rats suckled either ad libitum by the dam (n = 30), or were fed a rat milk-simulated formula (n = 30). After 3 d, the animals were killed, and the left femur, heart blood, mesenteric lymph nodes, liver, spleen, and terminal ileum were excised. Organs were analyzed for bacteria by standard microbiologic procedures. Bacterial translocation occurred in 23% of breast-fed rats; the bone was not infected in any of these animals. After feeding of formula diet, bacterial counts of the ileum were markedly elevated (p < 0.001), and the composition of the gut flora was disrupted. Bacterial translocation was noted in all formula-fed rats. Bone cultures were positive in 23 of 30 (77%) rats after formula-feeding (p < 0.001 versus breast-feeding). Organisms translocated to the bone included Enterococci, Proteus, Enterobacter, and Escherichia coli. Bacterial species cultured from the bone correlated with the individual colonization pattern of other extraintestinal organs and with the composition of the ileal flora. Members of the gut flora can escape the intestine and colonize the bone in formula-fed rats. The gut should be considered as a potential source for osteomyelitis in the neonate.
Similar content being viewed by others
Main
Acute osteomyelitis in the neonate is a leading cause of destruction of the physis resulting in high rates of permanent handicaps (1–3). Because the major route of infection is via the bloodstream, opportunities for organisms to gain access to the circulation may favor the development of osteomyelitis. Premature and sick neonates represent the high-risk group, and in this population potential sites of bacterial entrance are frequently present. Many of these infants undergo vascular manipulation including insertion of central catheters for total parenteral nutrition or invasive monitoring, which have long been linked to the development of skeletal infection. In most cases, however, the origin of bacterial entry remains unknown (4). Therefore, alternative routes of infection should be considered.
Among the organisms causing neonatal osteomyelitis, Staphylococcus aureus is most common, followed by group B streptococci and Gram-negative bacteria (1, 5–7). All of these organisms have the ability to colonize the neonatal gut. They may represent normal luminal residents, or members of an abnormal microflora, as frequently seen in hospitalized neonates (8). It is now widely accepted that organisms can escape from the gastrointestinal tract and invade extraintestinal organs, a process termed as bacterial translocation (9, 10). In normal adult individuals, translocation of bacteria from the gastrointestinal tract is limited by a normal permeability of the intestinal mucosa, a well-established intestinal microflora, and a normal functioning of the immune system (11). Each of these factors is potentially altered in neonatal animals (12–15) and infants (16, 17), especially when premature and critically ill, and by feeding of a formula diet (18). Consequently, it has been argued that bacterial translocation is facilitated early in life (19). In support of this concept, translocation of parts of the intestinal flora occurs spontaneously and decreases with age in conventionally reared neonatal rodents (20, 21), with the intensity of translocation apparently being higher in rats (which are relatively immature at birth) than in the more mature rabbit pups. The age-dependant fall in spontaneous bacterial translocation is associated with a reduction of the intestinal permeability to small molecular weight particles (22), with the maturation of the gut-associated lymphoid tissue (23), and with the establishment of a normal gut flora (20). Whereas the spontaneous escape of bacteria from the intestine has no documented adverse effects in normal breast-fed animals, more pronounced translocation, as observed after artificial feeding (24) or induced by oral inoculation of various strains of Escherichia coli(25–27) and group B streptococcus (28), can result in septicemia (24–28), pneumonia (28), meningitis (26, 28), and death (26, 28).
The present experiments were performed to assess the possible role of bacterial translocation from the intestine in the etiology of bone infection in the premature neonate. Newborn rats were chosen as subjects for two reasons. First, these animals are relatively immature and therefore serve as a model for the preterm neonate (29), in whom the risk of neonatal osteomyelitis is highest. Second, we knew from previous experiments that rat pups are prone to bacterial translocation, especially when fed a formula diet (24).
METHODS
Animals.
Time-gestation pregnant Sprague-Dawley rats were purchased from the Himberg Breeding Laboratories (Vienna, Austria). The animals had free access to water and regular chow and were kept on a 12-h light-dark cycle. The rats were allowed to deliver spontaneously. Only witnessed births were used for these experiments. The studies have been approved by the institutional review board.
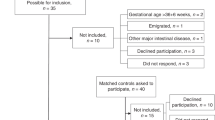
Experimental groups.
Sixty newborn male and female rat pups from nine litters were randomly assigned to one of two groups: in the first group, rats were fed adequate amounts of formula per gavage calculated to provide a daily energy intake of 500 kcal/kg as described previously in more detail (24, 30). In the second group, rats suckled ad libitum by the dam and were sham intubated every 6 h. An additional group of 17 rat pups were studied immediately after delivery and served as newborn controls. All organs cultured from this control group remained sterile. Formula-fed pups were housed in individual Styrofoam cups floated in a water bath maintained at 37°C. The rat milk formula (Milupa Nutrition Co., Austria) was composed according to published data on rat milk composition (31). Each 100 mL contained 175 kcal, 9.6 g of protein, 2.9 g of carbohydrate, and 12.9 g of fat with minerals and vitamins approximating that present in rat milk.
Testing for bacterial translocation.
After 3 d the animals were killed by cervical dislocation. Using sterile techniques, the left femur was removed under lens magnification. The femur was used for microbiologic investigation because rapidly growing ends of the large long bones, especially those of the lower extremity, are major sites of osteomyelitis in the neonate (7, 32). The femur was cut longitudinally, and the bone marrow was removed and homogenized with 9 volumes of brain heart infusion using sterile ground glass stoppers. Then, the chest and abdominal cavities were opened. Blood was obtained by cardiac puncture under direct visualization, and 100 μL was incubated for 24 h at 37°C in 5 mL of brain heart infusion. The mesenteric lymph node complex, liver, and spleen were removed, and all organs were weighed and homogenized with 9 volumes of brain heart infusion. To determine bacterial concentrations, homogenates of the bone marrow, liver, and spleen were serially diluted from 101 to 106 in sterile saline. Finally, the distal ileum was excised, weighed, and homogenized. Homogenates were serially diluted from 101 to 1010. Portions (0.1 mL from the various dilutions and 0.1 mL from the remaining organ homogenates) were plated on blood agar to culture for aerobic and facultative anaerobic Gram-positive bacteria, on Endoagar to culture for aerobic and facultative anaerobic Gram-negative bacilli, and on MRS agar to culture for lactobacilli (Oxoid Company, Hampshire, UK). The homogenized mesenteric lymph nodes and the remaining homogenates of the bone marrow from the femur, liver, and spleen were incubated aerobically in 5 mL of brain heart infusion at 37°C and then subcultured on the three different agar plates. Hypothetically, as few as one viable bacterium in the homogenates of the organs can be detected using these culturing procedures. All agar plates were incubated at 37°C under aerobic conditions. After 24 h the cultures were analyzed by a microbiologist who was unaware of the study design. The Gram-negative bacteria were identified with the API 20 E system (Analytab Products, Plainview, NY, U.S.A.) and the Gram-positive cocci by standard microbiologic procedures. Quantitative culture results were determined by the number of CFU per gram of tissue calculated from the dilutions of organ homogenates and positive tissue cultures.
Statistics.
Continuous data were compared using the unpaired t test. Discontinuous data were evaluated by χ2 analysis;p values < 0.05 were considered statistically significant.
RESULTS
Bacterial colonization of the ileum.
As shown in Table 1, formula-feeding resulted in an increase in the ileal concentration of all bacterial species, and the total bacterial counts were substantially higher than those in breast-fed animals. Furthermore, the ilea of formula-fed pups were colonized with a higher variety of species, and also included Proteus, Enterobacter, and Acinetobacter, organisms that were not found in breast-fed animals.
Bacterial translocation.
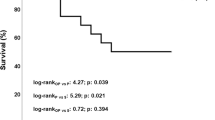
Table 2 compares the frequency of bacterial translocation to extraintestinal organs. After 3 d of breast-feeding, bacteria were cultured from the mesenteric lymph nodes in 20%, and from the liver and spleen in 10% of rats. All cultures from the blood or from the bone remained sterile in breast-fed rats. Formula-feeding dramatically increased bacterial translocation to all organs investigated. Blood cultures were positive in 63%, and in 77% of formula-fed pups enteric bacteria had translocated to the bone.
The incidences and concentrations of viable species translocated to the various organs are summarized in Table 3. In breast-fed pups, translocated organisms were identified as E. coli, Enterococcus, Lactobacilli, and Staphylococcus epidermidis. In addition to these organisms, formula-feeding was associated with translocation of Proteus and Enterobacter, species that were not present in organs of breast-fed pups.
Bacteria translocated to the bone.
In normal suckling rats all cultures from the bone remained sterile. Among formula-fed animals, 23 of 30 (77%) had positive bone cultures. Different translocated bacterial species included Enterococci, Proteus, Enterobacter, and E. coli; the mean concentrations of these species varied between 2.8 and 5.4 log CFU/g tissue (Table 3). Bacterial species cultured from the bone were correlated with the individual colonization pattern of other extraintestinal organs and with the composition of the bacterial flora in the ileum.
DISCUSSION
Various animal models of osteomyelitis have been developed to study the pathophysiology of this disease and to compare the efficacy of different antibiotic regimens (33–36). However, no reports exist that address the role of the gut as a possible source of neonatal bone infection. Our current findings confirm and expand the results of a previous study, showing that formula-feeding dramatically increases bacterial translocation in formula-fed rat pups (24). Using the same model, we now demonstrate that bacteria may escape the intestine and colonize the bone.
For the onset of hematogenous osteomyelitis bone lodgment of circulating bacteria is crucial. Experimental data indicate that among the factors that determine the ability of a microbe to colonize bone tissue and eventually induce osteomyelitis, the concentration and specific virulence factors of the offending organism have importance. For example, Emslie and Nade (33) injected S. aureus i.v. in chickens and observed that the incidence of osteomyelitis increased in a dose-dependent fashion. In their model, the 50% inhibitory dose for osteomyelitis was estimated as 5.5 × 105 viable organisms per kg of body weight. Others inoculated S. aureus UAMS-1 directly into the bone marrow of adult rabbits, and required 2 × 104 CFU to produce histologic and radiographic features of osteomyelitis (37). After inoculation of less virulent strains, bone lodgment of bacteria was rare or absent, despite the fact that a 100-fold dose of bacteria was used. During the current experiments we did not examine the bone histologically, and thus our findings do not prove that osteomyelitis was actually present. However, the presence of an average of 1.8 × 104 CFU of viable gut bacteria in the bone of our formula-fed rats clearly demonstrates that, under certain circumstances, members of the intestinal microflora can colonize bone tissue and thus become a potential source of osteomyelitis.
Several factors might explain the high incidence of positive bone cultures in our formula-fed rats. Formula-feeding dramatically enhances the concentration of enteric organisms and disturbs the composition of the gut flora. In addition, formula diet lacks the antiinfective properties normally present in breast milk (38, 39) and may thus further compromise the already limited host defense mechanisms present in the rats during the neonatal period. This may have resulted in the high load of systemically spreading organisms, which per se can increase the risk of bacterial lodgment to the bone. Various factors are known to favor the deposition of bacteria in neonatal bone tissue, including the sluggish circulation near the growth plate (40), specific virulence factors of the offending organisms (41), a particular tropism to the growth-plate cartilage matrix (42) of some species, and a deficiency of local host defense mechanisms (43). It is not surprising that in the presence of a deficient immune system and a high load of circulating bacteria, the clearance of organisms from the bone is incomplete, allowing the bacteria to multiply. Bacterial translocation to systemic organs (liver and spleen) was also observed in breast-fed animals; however, in none of them the bone was colonized. This may be explained by a lower intensity of translocation in combination with a better functioning of the immune defense system in the breast-fed rats.
Despite the growing evidence derived from experimental animals, as alluded to in the “Introduction,” there exist no systematic studies documenting that bacterial translocation occurs commonly and causes clinically significant disease in human neonates. Some limited and circumstantial data, however, support the existence and pathogenetic impact of translocation in the pediatric population. For example, Albers et al.(44) cultured bacteria from the peripheral blood in 21 of 131 normal 3-d-old infants, and in three of them blood cultures remained positive for the same organisms for 4 to 6 d. The authors argued that this was a benign phase that some infants undergo during the process of acquiring normal bacterial flora. Goldmann (8) found that infection caused by Gram-negative bacilli usually occurs in neonates already colonized with these organisms in the pharynx or intestine. Further, Lambert-Zechovsky et al.(45) described a 2150-g male infant born at 33 wk of gestation who demonstrated systemic bacteremia and meningitis caused by Enterobacter cloacae. Using molecular analysis, the authors provided genetic evidence that the strains isolated sequentially from cultures of stool, blood, and cerebrospinal fluid were identical. Pierro et al.(46) studied neonates and infants receiving long-term parenteral nutrition. The authors found that six of 94 patients experienced 15 episodes of septicemia caused by bacteria of enteric origin; in all six patients, the causative organisms were also present in the throat or rectum. We are aware of two studies on bacterial translocation in infants in which cultures from the mesenteric lymph nodes or the liver were performed in an effort to better trace the path of bacterial entrance. Cicalese et al.(47) studied 50 children undergoing small bowel transplantation. Blood, stool, liver biopsies, and peritoneal fluid were collected when infection was clinically suspected. Bacterial translocation (defined as the simultaneous presence of microorganisms in blood or liver biopsy and feces) was present in 44% of patients. Finally, among 28 infants with short bowel syndrome and sepsis, 19 harbored the causative organisms in the fecal flora, and in 12 of them the pathogens were present in the mesenteric lymph nodes (48).
Although our findings in rats cannot be directly applied to the situation in infants, several observations are consistent with the hypothesis that skeletal infection of the neonate may be caused by translocation of bacteria from the gut. Unlike in the older child, organisms frequently present in the neonatal gastrointestinal tract, like E. coli, Klebsiella, Enterobacter, and Enterococci, are pathogens for osteomyelitis in this age group (1, 6). It is conceivable that these organisms could pass through the immature intestinal barrier and cause manifest infection in the neonatal host with an unusual susceptibility to many organisms that may be considered normal flora. Further, S. aureus and group B streptococcus, the most frequently encountered causative species of neonatal skeletal infection, may also colonize the intestine (8), particularly in hospitalized neonates, in whom the risk of osteomyelitis is increased. The ability of these bacteria to translocate from the gut into the systemic circulation has been documented in experimental animals (28, 49), and may be operative when asymptomatic bacteremia develops in human neonates (44). It is interesting to note that in the present study S. aureus was not detected in the bone, despite the fact that some rat pups harbored this organism in the small intestine. Possible explanations for the failure of S. aureus to translocate include the relatively low intestinal concentration and the small number of rats colonized with this species.
In conclusion, we have shown that intestinal bacteria escape the gut and can colonize bone tissue in formula-fed rat pups. It is tempting to speculate that neonatal osteomyelitis is mediated by bacterial translocation in a subgroup of patients, especially in those who are premature and sick. To substantiate this hypothesis, clinical studies are required that are designed to identify the causative organisms of osteomyelitis in the patient's own gut flora. The absence of bacteria in bone tissue of suckling rats supports the importance of breast-feeding.
Abbreviations
- CFU:
-
colony forming units
References
Bergdahl S, Ekengren K, Eriksson M 1985 Neonatal hematogenous osteomyelitis: risk factors for long-term sequelae. J Pediatr Orthop 5: 564–568
Betz RR, Cooperman DR, Wopperer JM, Sutherland RD, White JJ, Schaaf HW, Aschliman MR, Choi IH, Bowen JR, Gillespie R 1990 Late sequelae of septic arthritis of the hip in infancy and childhood. J Pediatr Orthop 10: 365–372
Mok PM, Reilly BJ, Ash JM 1982 Osteomyelitis in the neonate. Radiology 145: 677–682
Bishara J, Freij GH, McCracken 1994 Acute infections. In: Avery GB, Fletcher MA, MacDonald MG (eds) Neonatology: Pathophysiology and Management of the Newborn. JB Lippincott, Philadelphia, 1082–1116.
Edwards MS, Baker CJ, Wagner ML, Taber LH, Barrett FF 1978 An etiologic shift in infantile osteomyelitis: the emergence of the group B streptococcus. J Pediatr 93: 578–583
Dan M 1983 Neonatal septic arthritis. Isr J Med Sci 19: 967–971
Fox L, Sprunt K 1978 Neonatal osteomyelitis. Pediatrics 62: 535–542
Goldmann DA 1981 Bacterial colonization and infection in the neonate. Am J Med 70: 417–422
Berg RD, Garlington AW 1979 Translocation of certain indigenous bacteria from the gastrointestinal tract to the mesenteric lymph nodes and other organs in a gnotobiotic mouse model. Infect Immun 23: 403–411
Wells CL, Maddaus MA, Simmons RL 1988 Proposed mechanisms for the translocation of intestinal bacteria. Rev Infect Dis 10: 958–979
Deitch EA, Berg RD 1987 Bacterial translocation from the gastrointestinal tract: a mechanism of infection. J Burn Care Rehab 8: 475–482
Israel EJ, Pang KY, Harmatz PR, Walker WA 1987 Structural and functional maturation of rat gastrointestinal barrier with thyroxine. Am J Physiol 252: G762–G767
Udall JN, Pang K, Fritze L, Kleinman R, Walker WA 1981 Development of gastrointestinal mucosal barrier. I. The effect of age on intestinal permeability to macromolecules. Pediatr Res 15: 241–244
Brunel A, Gouet P 1982 Kinetics of the establishment of gastrointestinal microflora in the conventional new-born rat. Ann Microbiol Paris 133B: 325–334
Guy-Grand D, Griscelli C, Vassalli P 1978 The mouse gut T lymphocyte, a novel type of T cell. Nature, origin, and traffic in mice in normal and graft-versus-host conditions. J Exp Med 148: 1661–1677
Lassiter HA, Tanner JE, Miller RD 1992 Inefficient bacteriolysis of Escherichia coli by serum from human neonates. J Infect Dis 165: 290–298
Perkkiö M, Savilathi E 1980 Time of appearance of immunoglobulin-containing cells in the mucosa of the neonatal intestine. Pediatr Res 14: 953–955
Balmer SE, Wharton BA 1989 Diet and fecal flora in the newborn: breast milk and infant formula. Arch Dis Child 64: 1672–1677
Van Camp JM, Tomaselli V, Coran AG 1994 Bacterial translocation in the neonate. Curr Opin Pediatr 6: 327–333
Wenzl HH, Schimpl G, Feierl G, Steinwender G 2001 Time course of spontaneous bacterial translocation from the gastrointestinal tract and its relationship to the intestinal microflora in conventionally reared infant rats. Dig Dis Sci 46: 1120–1126
Van Camp JM, Tomaselli V, Drongowski R, Coran AG 1995 Bacterial translocation in the newborn rabbit: effect of age on frequency of translocation. Pediatr Surg Int 10: 134–137
Urao M, Okuyama H, Drongowski RA, Teitelbaum DH, Coran AG 1997 Intestinal permeability to small- and large-molecular-weight substances in the newborn rabbit. J Pediatr Surg 32: 1424–1428
Urao M, Teitelbaum DH, Drongowski RA, Coran AG 1996 The association of gut-associated lymphoid tissue and bacterial translocation in the newborn rabbit. J Pediatr Surg 31: 1482–1487
Steinwender G, Schimpl G, Sixl B, Kerbler S, Ratschek M, Kilzer S, Höllwarth ME, Wenzl HH 1996 Effect of early nutritional deprivation and diet on translocation of bacteria from the gastrointestinal tract in the newborn rat. Pediatr Res 39: 415–420
Scannapieco FA, Guerina NG, Goldmann DA 1982 Comparison of virulence and colonizing capacity of Escherichia coli K1 and non-K1 strains in neonatal rats. Infect Immun 37: 830–832
Glode MP, Sutton A, Moxon R, Robbins JB 1977 Pathogenesis of neonatal Escherichia coli meningitis: induction of bacteremia and meningitis in infant rats fed E. coli K1. Infect Immun 16: 75–80
Murata H, Yaguchi H, Namioka S 1979 Relationship between the intestinal permeability to macromolecules and invasion of septicemia-inducing Escherichia coli in neonatal piglets. Infect Immun 26: 339–347
Weisman LE, McKinney LA, Villalobos R 1990 Systemic group B streptococcal disease in the neonate: characterization of an oral colonization model using the suckling rat. Microbiol Immunol 34: 755–764
Israel EJ, Schiffrin EJ, Carter EA, Freiberg E, Walker WA 1990 Prevention of necrotizing enterocolitis in the rat with prenatal cortisone. Gastroenterology 99: 1333–1338
Moore MC, Greene HL, Said HM, Ghishan FK, Orth DN 1986 Effect of epidermal growth factor (EGF) and artificial feeding in suckling rats. Pediatr Res 20: 1248–1251
Dymsza HA, Czajka DM, Miller SA 1964 Influence of artificial diet on weight gain and body composition of the neonatal rat. J Nutr 84: 100–106
Frederiksen B, Christiansen B, Knudsen FU 1993 Acute osteomyelitis and septic arthritis in the neonate, risk factors and outcome. Eur J Pediatr 152: 577–580
Emslie KR, Nade S 1983 Acute hematogenous staphylococcal osteomyelitis. A description of the natural history in an avian model. Am J Pathol 110: 333–345
Whalen JL, Fitzgerald RH, Morrissy RT 1988 A histological study of acute hematogenous osteomyelitis following physeal injuries in rabbits. J Bone Joint Surg Am 70: 1383–1392
Norden CW, Kennedy E 1970 Experimental osteomyelitis I. A description of the model. J Infect Dis 122: 410–418
Norden CW, Shiners A 1985 Ciprofloxacin as therapy for experimental osteomyelitis caused by Pseudomonas aeruginosa. J Infect Dis 151: 291–294
Smeltzer MS, Thomas JR, Hickmon SG, Skinner RA, Nelson CL, Griffith D, Parr TR, Evans RP 1997 Characterization of a rabbit model of staphylococcal osteomyelitis. J Orthop Res 15: 414–421
Williams RC, Gibbons RJ 1972 Inhibition of bacterial adherence by secretory immunoglobulin A: a mechanism of antigen disposal. Science 177: 697–699
Welsh JK, May JT 1979 Anti-infective properties of breast milk. J Pediatr 118: 1–9
Ogden JA 1979 Pediatric osteomyelitis and septic arthritis. The pathology of neonatal disease. Yale J Biol Med 52: 423–448
Matsushita K, Hamabe M, Matsuoka M, Aoki H, Miyoshi K, Ichiman Y, Shimada J 1997 Experimental hematogenous osteomyelitis by Staphylococcus aureus. Clin Orthop 334: 291–297
Alderson M, Speers D, Emslie K, Nade S 1986 Acute haematogenous osteomyelitis and septic arthritis—a single disease. J Bone Joint Surg Br 68: 268–274
Morrissy RT, Haynes DW 1989 Acute hematogenous osteomyelitis: a model with trauma as an etiology. J Pediatr Orthop 9: 447–456
Albers WH, Tyler CW, Boxerbaum B 1966 Asymptomatic bacteremia in the newborn infant. J Pediatr 69: 193–197
Lambert-Zechovsky N, Bingen E, Denamur E, Brahimi N, Brun B, Mathieu H, Elion J 1992 Molecular analysis provides evidence for endogenous origin of bacteremia and meningitis due to Enterobacter cloacae in an infant. Clin Infect Dis 15: 30–32
Pierro A, van Saene HK, Donnell SC, Hughes J, Ewan C, Nunn AJ, Lloyd DA 1996 Microbial translocation in neonates and infants receiving long-term parenteral nutrition. Arch Surg 131: 176–179
Cicalese L, Sileri P, Green M, Abu-Elmagd K, Fung JJ, Starzl TE, Reyes J 2000 Bacterial translocation in clinical intestinal transplantation. Transplant Proc 32: 1210
Kurkchubasche AG, Smith SD, Rowe MI 1992 Catheter sepsis in short-bowel syndrome. Arch Surg 127: 21–24
Ford HR, Avanoğlu A, Boechat PR, Melgoza D, LumCheong RS, Boyle P, Garrett M, Rowe MI 1996 The microenvironment influences the pattern of bacterial translocation in formula-fed neonates. J Pediatr Surg 31: 486–489
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Steinwender, G., Schimpl, G., Sixl, B. et al. Gut-Derived Bone Infection in the Neonatal Rat. Pediatr Res 50, 767–771 (2001). https://doi.org/10.1203/00006450-200112000-00023
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200112000-00023