Abstract
The pulmonary vasculature of newborns with persistent pulmonary hypertension is characterized by active vasoconstriction and vascular remodeling. It has been suggested that endothelin-1 (ET-1), a potent vasoconstrictor and growth promoter, may be involved in the pathogenesis of persistent pulmonary hypertension of the newborn. To determine whether treatment with an ETA receptor antagonist can reverse pulmonary hypertension in the neonate, 1-d-old piglets were exposed to hypoxia for 3 d to induce pulmonary hypertension and then treated for the remainder of the 14 d with an orally active, nonpeptidic ETA antagonist (TBC3711, 22 mg·kg−1·d−1). At the end of the exposure, Hb, pulmonary artery pressure, right ventricle to left ventricle plus septum weight ratio, percentage wall thickness, ET-1 circulating levels, perfusion pressure, and dilator response to the nitric oxide (NO) donor, SIN-1 (3-morpholinosydnonimine-N-ethylcarbamide) in isolated perfused lungs were determined. Exhaled NO and hemodynamic variables were also examined in an intact anesthetized animal preparation that had undergone the same treatment. By 3 d of exposure to hypoxia, piglets had already developed significant pulmonary hypertension as estimated by their pulmonary artery pressure (24.0 ± 1.3 mm Hg versus 14.2 ± 3.4 mm Hg) and percentage wall thickness (26.6 ± 5.9%versus 18.7 ± 2.4% for vessels 0–30 μm). Whereas further exposure to hypoxia for 14 d did not enhance the increase in pulmonary artery pressure and percentage wall thickness, it did augment the right ventricle to left ventricle plus septum weight ratio (0.71 ± 0.09 versus 0.35 ± 0.01). ET-1 circulating levels were increased only when exposure to hypoxia was prolonged to 14 d (5.1 ± 2.4 pg/mL versus 1.0 ± 0.4 pg/mL). Treatment with TBC3711 from d 3 to d 14, once pulmonary hypertensive changes were established and while hypoxic exposure persisted, caused significant reduction in the right ventricle to left ventricle plus septum weight ratio (0.60 ± 0.06), pulmonary artery pressure (20.0 ± 4.8 mm Hg), and percentage wall thickness (18.5 ± 3.3%) and restored the dilator response to the NO donor SIN-1. Prolonged hypoxia markedly reduced exhaled NO concentrations (0.3 ± 0.6 ppb), although treatment of hypoxic animals with TBC3711 restored the concentration of exhaled NO (4.4 ± 2.8 ppb) to the level of normoxic controls (4.9 ± 3.0 ppb). Lastly, treatment with TBC3711 increased ET-1 circulating levels in both the normoxic (5.4 ± 2.8 pg/mL) and hypoxic (13.0 ± 6.3 pg/mL) groups. In conclusion, the specific ETA receptor antagonist, TBC3711, can significantly ameliorate the morphologic changes encountered in hypoxia-induced pulmonary hypertension in the newborn piglet and may improve the dilator response to NO.
Similar content being viewed by others
Main
At birth, PVR falls with the initiation of ventilation (1). This reduction in PVR is thought to relate to the mechanical distension of the lungs, the change in oxygen tension and pH, the release of vasoactive substances, and the involution of smooth muscle cells in the pulmonary vascular bed (2, 3). In PPHN, these changes fail to occur normally. The pulmonary vasculature of these newborns is then characterized by active vasoconstriction and vascular remodeling (4). Although inhaled NO has been shown to be helpful in the management of these newborns, it is effective in only 50% of them (5). ET-1, a potent vasoconstrictor and growth promoter, may be involved in the pathogenesis of PPHN. ET-1 is present (6) and is vasoactive in fetal and perinatal lung (7, 8). The actions of ET-1 are dependent on activation of at least two receptor subtypes, ETA and ETB(9). ETA receptors are located on smooth muscle cells and mediate vasoconstriction and smooth muscle cell proliferation. Binding to endothelial ETB receptors causes vasodilation through release of NO and results in clearance of ET-1 from the circulation (10). ETB receptors appear to play an important role in the maintenance of low vascular tone in the neonate as chronic blockade leads to pulmonary hypertensive changes (11). As in the human pulmonary arteries, ETA receptors are predominant in piglet pulmonary arteries (12, 13). Supporting its role in the pathogenesis of PPHN, high circulating levels of ET-1 have been found in newborns with PPHN (14). Furthermore, it has been shown that pulmonary hypertension in neonatal animals is associated with a loss of ETB-mediated vasodilation, sustained ETA-mediated vasoconstriction, and increased lung ET-1 content (15–17).
Postnatal exposure of neonatal piglets to hypoxia has been shown to prevent the normal birth-related changes in the pulmonary circulation (15, 18, 19). Even though alveolar hypoxia is not a typical feature of neonatal pulmonary hypertension, this experimental model allows us to study the structural and functional changes associated with neonatal pulmonary hypertension (15, 18, 19). We hypothesized that treatment with a specific ETA receptor antagonist of neonatal piglets with established hypoxia-induced pulmonary hypertension may reverse the morphologic and physiologic changes by blocking the ETA receptor, therefore maximizing the beneficial role of the ETB receptor through its link with the NO system. As a consequence, blockade of ET-1 may improve the vasodilator response to NO. To test these hypotheses, we used an orally active nonpeptidic ETA receptor antagonist, TBC3711 (20), in neonatal piglets that had already developed pulmonary hypertension, making the experimental condition more relevant to the clinical condition.
METHODS
Characterization of TBC3711.
Binding assays were performed using membranes from two cell lines: TE-671 human rhabdomyosarcoma expressing ETA receptor (HTB 139, American Type Tissue Culture Collection, Rockville, MD, U.S.A.) and COS cells transfected with human ETB receptor (21). Studies were conducted in the presence of 4 pM 125I-ET-1 (Amersham, Piscataway, NJ, U.S.A.) at 24°C in a final volume of 200 μL of N-2-hydroxyethylpiperazine-N′-2ethanesulfonic acid (HEPES)-buffered salt solution (pH 7.5) containing 0.5% BSA with varying concentrations of TBC3711. The binding reaction was initiated by the addition of the membrane preparation (4 μg of protein/tube for TE-671 cells and 0.25 μg of protein/tube for COS ETB cells) to the incubation media. The reaction mixture was incubated for 18 h at 24°C and stopped by addition of 1 mL of cold PBS, and separation of bound tracer from free tracer was performed by centrifugation at 3500 ×g for 40 min at 4°C. After decanting the supernatant, tubes were counted for 1 min in a GeneSys gamma counter. Nonspecific binding for 125I-ET-1 was measured in the presence of at least 1000× excess of the unlabeled ligand.
Inhibition studies (n = 3) were conducted in isolated perfused lungs in which ET-1 was added to the perfusion bath using 5- to 6-d-old Yorkshire-Landrace piglets raised on the farm and used immediately after arrival in accordance with the McGill University guidelines for the use of experimental animals.
Animals for chronic studies.
Experiments were performed on 1-d-old piglets with the approval of the Animal Care Committee of the McGill University. As previously described (15, 18, 19), piglets were maintained in a 440-L Plexiglas chamber in Fio2 0.10 ± 0.005 (hypoxia) or room air (control) for a period of either 3 or 14 d. Hypoxia was achieved by a continuous mixture of separate sources of air and nitrogen (Floxal, VitalAire, Montreal, PQ, Canada). Fio2 and Fico2 were measured at least three times per day with an electrochemical cell O2 analyzer (model S3-A/1) and sensor (model N-22M, Ametek, Pittsburgh, PA, U.S.A.) and an infrared CO2 analyzer (model CD-3A) and sensor (model P-61B, Ametek). Fio2 was also continuously monitored with an Oxychek oximeter (Critikon, Tampa, FL, U.S.A.). Fico2 was kept <0.005 via adjustment of total gas flow. Piglets were maintained in a thermoneutral environment, and temperature was adjusted (26–33°C) according to age using a heater (model PCW-4, Noma, ON, Canada) with a temperature controller (model 689–0000, Barmant, Barrington, IL, U.S.A.). Humidity level was maintained <70% using a condensing coil as a dehumidifier. A dark-light cycle of 12 h/12 h was established, and animals were fed ad libitum with balanced artificial milk (Wet Nurser, Jefo Import Export, Ste-Hyacinthe, PQ, Canada). Daily care of the animals was done without interruption of hypoxia, except for the time when they received the medication. Control piglets were raised under identical conditions, except that Fio2 was maintained at 0.21. All piglets received an intramuscular injection of iron at arrival. After 3 d of exposure to hypoxia or normoxia, animals were assigned to receive or not TBC3711 (11 mg·kg−1·dose−1), orally, twice a day, by capsule for the remainder of the 14-d exposure. Control animals did not receive anything except that they were taken out of the chamber for the same length of time. In the first part of the study, the animals from six different groups [normoxia 3-d control (n = 6), normoxia 14-d control (n = 10), normoxia 14-d treated with TBC3711 (n = 8), hypoxia 3-d control (n = 6), hypoxia 14-d control (n = 21), and hypoxia 14-d treated with TBC3711 (n = 16)] underwent a thoracotomy to assess morphometric changes in lungs fixed in formalin or for measurement of acute physiologic variables and vascular reactivity to a vasodilator, SIN-1, in isolated perfused lungs. In the second part of the study, hemodynamic measurements as well as assessment of exhaled NO were done in the anesthetized intact animal that had been previously exposed to normoxia for 14 d, hypoxia for 14 d, and hypoxia for 14 d while being treated with TBC3711 (n = 4–5).
Physiologic measurements in thoracotomized animals.
The animals were weighed daily during the exposure. On the day of physiologic measurements, animals were anesthetized with sodium pentobarbital (65 mg/kg i.p.), and a tracheostomy was performed. They were then ventilated with 25% O2-5% CO2 in N2 with a tidal volume of 20 mL/kg, resulting in an arterial blood pH between 7.35 and 7.45. After a sternotomy, PAP was measured by direct puncture with an 18-gauge needle connected to a transducer (model P2310, Gould Instruments, Cleveland, OH, U.S.A.) and a chart recorder (model 7E, Grass Instruments, Quincy, MA, U.S.A.). Blood was sampled from the left ventricle for measurement of Hb concentration and ET-1 plasma level. Lungs were then used for morphometric measurements or organ perfusion. Finally, hearts were removed and dissected into right ventricle and left ventricle plus septum. The ratio of RV/LV+S weight was then calculated as an index of right ventricular hypertrophy.
Morphometric measurements.
The lungs were fixed in the distended state by the infusion of 10% buffered formalin into the pulmonary artery and trachea at 100 and 25 cm H2O pressure, respectively, for 1 min. The pulmonary artery and veins were clamped, and the entire specimen was placed in a bath of 10% buffered formalin for 24 h, as described by Di Carlo et al.(22). Next, 1- to 2-cm blocks were taken from the right and left lower lobes at two thirds of the distance from the hilum to the pleural surface along the bronchial axis and fixed in paraffin. Tissue was cut in sections 3 μm thick, and elastic fibers were stained with Verhoeff for light microscopy. With the use of a calibrated eyepiece micrometer (Olympus BX40, Olympus Corp., Lake Success, NY, U.S.A.), using the external and internal elastic laminae as the perimeters, the ID and ED were measured (23). Obliquely cut arteries were measured along their shortest axis. From these two measurements (ED and ID), two variables were calculated. The %WT was defined as [(ED − ID)/ED] × 100, and MSA was defined as the area within the circle described by the external elastic lamina minus the area within the circle described by the internal elastic lamina. The %WT and MSA of at least 10 consecutive pulmonary arteries of each of the following diameters (0–30, 30–60, 60–90, 90–120, and >120 μm) were determined at ×400 and ×1000 magnification in a blinded manner.
Isolated perfused lung.
Animals were anesthetized with sodium pentobarbital (65 mg/kg i.p.), tracheostomized, and ventilated with 25% O2-5% CO2 in N2 with a tidal volume of 20 mL/kg. The isolated perfused lung was set up as previously described (15). Briefly, a cannula was placed in the pulmonary artery, and the lungs were perfused with Krebs solution supplemented with 5% BSA at a constant flow of 30 mL·min−1·kg−1 body weight using a peristaltic pump (Masterflex, model 7553–30, Cole-Parmer, Chicago, IL, U.S.A.). This flow rate represents 10–20% of normal pulmonary blood flow. Perfusate drained by gravity through a cannula placed in the left ventricle. Venous pressure was then equal to atmospheric pressure. Throughout the experiments, perfusion pressure, which reflects pulmonary artery inflow pressure, was monitored with a transducer (model P2310, Gould Instruments) and a chart recorder (model 7E, Grass Instruments). Baseline perfusion pressure has been shown previously to be stable for ≥2.5 h. Integrity of the preparation was assessed by the stability of the baseline perfusion pressure or by the presence of edema as revealed by macroscopic examination.
Lung preparations were allowed to stabilize for 30 min after being mounted and perfused inside the chamber. To achieve comparable baseline perfusion pressures among all four groups, vascular tone was raised as needed by adding the endoperoxide analog, U-46619, to the perfusate after the stabilization period. The NO donor, SIN-1, was then added to the perfusion bath and continuously recirculated through the preparation. An interval of at least 20 min was allowed between each concentration of SIN-1 tested.
Measurement of ET-1 plasma levels.
After thoracotomy and before lung excision, blood was sampled from the left ventricle and placed in chilled tubes with EDTA. Blood was immediately centrifuged at 3000 × g at 4°C for 20 min, and the plasma was stored at −70°C until analyzed.
Plasma ET-1 concentration was measured by quantitative sandwich enzyme immunoassay technique, using QuantiGlo human ET-1 immunoassay kits from R&D Systems (Minneapolis, MN, U.S.A.). Samples were analyzed in duplicate. Two antibodies, directed at different epitopes of the ET-1 molecule, were used. An enhanced luminol/peroxide substrate solution was added, and the intensity of the light emitted was measured with a microplate luminometer (MicroLumat Plus LB96V, EG & Berthold, Bad Wildbad, Germany). The intraassay coefficient of variation for the kit is 2.4%. The sensitivity of the assay for ET-1 is 0.16 pg/mL. The cross-reactivity with human ET-2 is 27.4%, and with human ET-3, 7.8%. The cross-reactivities for human bigET-2, porcine bigET-39, human bigET-38, bovine bigET-39, rat bigET-39, and sarafotoxin are minimal, i.e. <0.05%.
Measurements in anesthetized intact animals.
On the day of study, the animals were anesthetized with 3% halothane until reflexes were abolished. A tracheostomy was then performed, and the halothane reduced to 1.25%. Volume-controlled ventilation was commenced using a Harvard small animal ventilator (Harvard, South Natick, MA, U.S.A.) at a volume of 15 mL/kg with 40% O2. The ventilator rate was adjusted to keep the arterial Pco2 between 36 and 44 mm Hg. After tracheostomy, a bolus of 100 μg/kg fentanyl was given, and an infusion of 200 μg·kg−1·h−1(24) was commenced. An infusion of thiopental at a rate of 5 mg·kg−1·h−1 was also started, and halothane was discontinued. A femoral artery was catheterized and connected to a pressure transducer for monitoring of systemic blood pressure and arterial blood gases. A 5F catheter was inserted into the right axillary vein and positioned in the mid right atrium using fluoroscopy. A 6F sheath was inserted into the right external jugular vein, through which a 5F flow-directed balloon-tipped thermodilution catheter was advanced into the main pulmonary artery through the sheath. Position was confirmed by fluoroscopy, pressure waveform, and the ability to obtain a typical wedge pressure tracing on inflation of the balloon. Central venous and arterial pressures were monitored using a Grass polygraph. Pulmonary pressures were monitored from the distal tip of the balloon-tipped catheter. Thermodilution cardiac output was measured by an Edwards cardiac output computer (model COM-1, American Edwards Laboratories, Irvine, CA, U.S.A.) with the use of 3 mL of iced saline, manually injected as quickly as possible during expiration, into the axillary vein catheter. Thermodilution estimates were always performed in triplicate. Sao2 was monitored using a transcutaneous pulse oximeter (N100; Nellcor Inc., Hayward, CA, U.S.A.). Hemodynamic variables were recorded after 30 min of stabilization. Immediately preceding the measurement of hemodynamic variables, expiratory gas was collected for 5 min in a nondiffusing gas collection bag (Hans Rudolph, Kansas City, MO, U.S.A.) from the expiratory limb of the ventilator for determination of exhaled NO concentration. Ventilation with an NO-free gas mixture was assured by passing the gas mixture through activated charcoal and potassium permanganate on alum (Purafil, Thermoelectron, Doraville, GA, U.S.A.), ensuring that measured exhaled NO solely reflected NO production by the animal.
Exhaled NO measurement.
The exhaled gas from the lungs was collected in a Hans Rudolph bag and analyzed for NO. Before each collection, residual gas from the bag was removed by vacuum after being flushed with an NO-free gas. A chemiluminescence technique was used for determination of exhaled NO output. Gas sample was immediately passed through a chemiluminescence analyzer (model 280 NOA; Sievers, Boulder, CO, U.S.A.). The analyzer was calibrated before each sample analysis using a gas mixture of NO in N2 (0.692 parts per million in N2; Matheson, Whitby, ON, Canada) and an NO-free gas produced by passing air through activated charcoal and potassium permanganate on alum. The range of detection of NO of the apparatus was from <1 to 500,000 ppb. Exhaled NO output was calculated from the measured NO concentration, the ventilation rate, and the tidal volume.
Drugs.
TBC3711 was provided by Dr. George W. Holland from Texas Biotechnology Corporation, Houston, TX, U.S.A. The Krebs solution for the isolated lung experiments had the following composition (in mM): 119 NaCl, 4.0 KCl, 1.2 MgSO4, 1.2 KH2PO4, 2.5 CaCl2, 5.5 dextrose, and 25 NaHCO3. The solution was supplemented with 50 g/L BSA. The following compounds were used: BSA (Sigma Chemical Co., St. Louis, MO, U.S.A.), SIN-1 hydrochloride (Calbiochem, San Diego, CA, U.S.A.), and the stable endoperoxide analog 9,11-dideoxy-9α,11α-methanoepoxy prostaglandin F2α (U-46619; Biomol Research Laboratories, Plymouth Meeting, PA, U.S.A.).
Data analysis.
Data are presented as mean ± SD. Analysis of binding data was done with Prism 3.0 (Graph Pad, GraphPad Software, San Diego, CA, U.S.A.) to determine IC50. Statistical analysis of physiologic data, %WT and MSA, ET-1 plasma levels, and exhaled NO was performed using an ANOVA with a p < 0.05 being considered significant.
The dilator responses to SIN-1 were evaluated by measuring the lowest perfusion pressure reached for each concentration tested. The significance of the effect of SIN-1 on perfusion pressure at different concentrations was assessed statistically using ANOVA for repeated measures. A p < 0.05 was considered significant.
RESULTS
Characterization of TBC3711
The 125I-ET-1 binding was completely displaced by TBC3711 in TE-671 cells with an IC50 of 0.08 nM (Fig. 1). In ETB-transfected cells, TBC3711 very poorly displaced ET-1 binding (IC50 = 26.3 μM). In other words, ETA/ETB selectivity was >100,000 for TBC3711.
At the concentrations tested (5 × 10−9 and 10−8 M), ET-1 caused potent vasoconstriction in isolated perfused lungs (Fig. 2). The vasoconstrictor response to ET-1 was greatly reduced when the lung preparations were treated with TBC3711 at 5 × 10−7 M (p < 0.001) and almost completely abolished at 4 × 10−6 M.
Vasoconstrictor response to ET-1, alone (•, n = 6) and in the presence of TBC3711, 5 × 10−7M (○, n = 3) and 4 × 10−6M (▾, n = 3), in isolated perfused lungs of normoxic newborn piglets. Responses are the highest perfusion pressure reached for each concentration of ET-1 tested. Values are mean ± SD. TBC3711 reduced significantly (p < 0.001) the constrictor response to ET-1 at both concentrations.
Chronic Studies
Physiologic measurements.
As expected in normoxia, the RV/LV+S decreased from d 3 to d 14 (p < 0.005;Fig. 3). After 14 d of exposure to hypoxia, this ratio was increased compared with the 3-d hypoxia group (p < 0.001) and was significantly greater than in the 14-d normoxia group (p < 0.001). In normoxia, when animals were treated with TBC3711, the ratio was unchanged. However, in the hypoxia TBC3711-treated group, the ratio was lower compared with the hypoxic control (p < 0.01). PAP was increased after 3 d of exposure to hypoxia (p < 0.001) compared with normoxia (Fig. 3), but did not further increase when exposure was prolonged to 14 d. Treatment with TBC3711 significantly reduced PAP in the hypoxic animals compared with hypoxic controls (p < 0.005).
Effect of hypoxia (Fio2 0.10) compared with normoxia on RV/LV+S and on PAP measured in thoracotomized animals after exposure to 3 d, 14 d, or 14 d with treatment with TBC3711. Values are mean ± SD. A, p < 0.005 compared with 3-d normoxia;B, p < 0.001 compared with 3-d hypoxia;C, p < 0.001 compared with 14-d hypoxia;D, p < 0.001 compared with respective normoxic control;E, p < 0.005 compared with 14-d hypoxia.
Animals raised in hypoxia experienced a lower weight gain compared with those raised in normoxia, with significance being reached after 14 d of exposure (p < 0.05;Table 1). Treatment with TBC3711 did not alter the weight gain compared with respective controls. In normoxic exposure, there was a decrease in Hb concentration with age (Table 1). In hypoxia, however, the Hb concentration failed to decrease and was elevated compared with normoxic controls at 14 d (p < 0.005). Treatment with TBC3711 reduced significantly the Hb concentration in hypoxia compared with controls (p < 0.005). Left ventricular pressure was reduced in hypoxic animals treated with TBC3711 compared with the hypoxic controls (p < 0.05;Table 1), although the pressure measured was similar to the one obtained in normoxic animals.
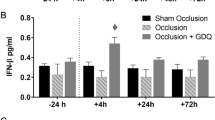
ET-1 circulating levels.
In these animals, age did not affect plasma ET-1 levels. Although exposure to hypoxia for 3 d did not significantly alter plasma ET-1 levels, exposure to hypoxia for 14 d was associated with a 5-fold increase in circulating levels (p < 0.005;Table 2). Furthermore, treatment with TBC3711 more than doubled the levels measured in both hypoxia (p < 0.001) and normoxia treated animals compared with controls (p < 0.005).
Morphometric analysis.
As expected, %WT was increased after 3 and 14 d of exposure to hypoxia (Fig. 4). Of interest, this increase appeared to peak after 3 d of hypoxia and was not further increased by prolonging the exposure to hypoxia for 14 d. Findings were very similar for MSA measurements (results not shown). Treatment with TBC3711 did not affect %WT (Fig. 5) or MSA (results not shown) in normoxic animals. However, in hypoxic animals, treatment with TBC3711 from d 3 to d 14 was associated with significant reductions in %WT (Fig. 5) and MSA (results not shown).
Effect of hypoxia (Fio2 0.10) compared with normoxia on pulmonary arterial %WT of different vessel sizes [0–30, 30–60, 60–90, 90–120, and >120 μm] in newborn piglets exposed for 3 or 14 d. Values are mean ± SD. *p < 0.05 compared with normoxic group of corresponding age; †p < 0.001 compared with normoxic group of corresponding age; ‡p < 0.005 compared with normoxic group of corresponding age.
Effect of TBC3711 (11 mg·kg−1·dose−1, twice a day) on pulmonary arterial %WT of different vessel sizes [0–30, 30–60, 60–90, 90–120, and >120 μm] in newborn piglets exposed for 14 d to normoxia or hypoxia (Fio2 0.10). Values are mean ± SD. *p < 0.001 compared with normoxic control group; †p < 0.001 compared with hypoxic control group; ‡p < 0.01 compared with hypoxic control group.
Pulmonary vascular response to SIN-1.
Baseline perfusion pressure was increased in animals raised in hypoxia compared with normoxia (p < 0.005;Fig. 6). Of interest, in animals treated with TBC3711, baseline perfusion pressure was similar to normoxic controls.
Vasodilator response to SIN-1 in isolated perfused lungs of newborn piglets exposed to normoxia or hypoxia for 14 d with or without treatment with TBC3711 (11 mg·kg−1·dose−1, twice a day). Responses are the lowest perfusion pressure reached for each concentration tested. Values are mean ± SD. B, baseline perfusion pressure;RB, baseline perfusion pressure raised by the addition of the endoperoxide analog, U-46619.
SIN-1 caused a dose-dependent decrease in perfusion pressure in all four study groups. However, in hypoxia the dilator response was significantly reduced compared with normoxic controls (p < 0.05). Interestingly, in hypoxic animals treated with TBC3711, the dilator response to SIN-1 was restored, rendering the response identical to that seen in normoxic controls.
Hemodynamic measurements in anesthetized intact animals.
Measurements of PAP, pulmonary wedge pressure, cardiac output, aortic pressure, central venous pressure, Sao2, and calculated PVR [(PAP minus pulmonary wedge pressure)/cardiac output] and systemic vascular resistance [(aortic pressure minus central venous pressure)/cardiac output] in anesthetized piglets are shown in Table 3. PAP and PVR were significantly (p < 0.05) greater in the chronically hypoxic piglets compared with the normoxic ones. Furthermore, Sao2 was lower in the hypoxic animals than in the normoxic controls (p < 0.05). In the chronically hypoxic animals treated with TBC3711, PVR was reduced by 40% and the Sao2 was ameliorated without reaching significance. Furthermore, even though systemic vascular resistance was decreased in the hypoxic treated animals (p < 0.05), aortic pressure was not significantly affected.
Exhaled NO measurement.
In the anesthetized animals, exhaled NO concentration and NO output were dramatically reduced (p < 0.05) in chronically hypoxic animals compared with normoxic controls (Table 4). Of interest, in the chronically hypoxic animals, treatment with TBC3711 restored the exhaled NO concentration to the level of normoxic controls and increased NO production by the lungs without quite reaching significance (p = 0.098;Table 4).
DISCUSSION
These findings provide strong evidence that, in the neonate, endogenous ET-1 is a major mediator of sustained pulmonary hypertension and pulmonary vascular remodeling seen in chronic hypoxia. More importantly, this is the first demonstration that chronic blockade of ETA receptors with an orally active nonpeptidic ETA receptor antagonist can significantly reduce established hypoxia-induced neonatal pulmonary hypertension while hypoxic exposure remains. Our results in the neonate are similar to the ones reported in the adult rat, in which BQ-123 and the nonpeptidic ET antagonists, bosentan and TBC11251, were able to reverse hypoxia-induced pulmonary hypertensive changes (22, 25, 26). A previous demonstration in an ovine fetal preparation had also shown that preventive treatment with BQ-123 could attenuate chronic pulmonary hypertension (27).
As we have previously shown (18), our model is effective in producing significant pulmonary hypertension as seen by the presence of an increased RV/LV+S, an increase in PAP, and an augmentation in the %WT and MSA of pulmonary vessels. The fact that after only 3 d of hypoxic exposure, PAP and medial thickness had reached a maximal level further demonstrates that these changes occur rapidly. The RV/LV+S was improved in animals treated with TBC3711; however, it did not reach the values seen in the normoxic animal. Although it is mainly through ETA receptor stimulation that vasoconstriction and smooth muscle proliferation occur, the role of ETB2 (constrictor) receptors in this animal model cannot be excluded (13). In addition, the origin of right ventricular hypertrophy is most likely multifactorial and includes increased pressure load from remodeling and vasoconstriction, increased ET-1 myocardial expression, or increased myocardial protein kinases (28), or some combination of these factors. Additionally, histologic changes in the right ventricular myocardium have been reported in adult rats exposed to prolonged hypoxia (29). Consequently, treatment with TBC3711 may help to counteract some, but not all, of these mechanisms. Although Ivy et al.(27) have described improvement of right ventricular hypertrophy after 8 d of preventive treatment with BQ-123 in an ovine model of pulmonary hypertension, complete reversal of right ventricular hypertrophy in our model may take longer. Furthermore, it is unknown, in our model, how the pharmacologic recovery compares with the rate of recovery once exposure to hypoxia is terminated.
Alveolar hypoxia is a potent constrictor of pulmonary resistance vessels, and exposure to chronic hypoxia causes smooth muscle cell growth and wall thickening in small peripheral pulmonary arteries (30, 31). As expected, significant medial hypertrophy was observed in the piglets exposed to hypoxia. Of great interest is the demonstration that treatment with ETA receptor antagonist, TBC3711, during continued exposure to hypoxia significantly reversed, in part, established vascular remodeling. The inability to completely reverse established hypoxia-induced pulmonary hypertension could be related to the brevity of treatment or most likely to the fact that other mechanisms are also implicated in the pathogenesis of pulmonary hypertension (32).
As shown in Figure 3, PAP measured in thoracotomized animals was significantly reduced by treatment with TBC3711 in our piglet model, without reaching the value of normoxic controls. However, PAP measured in the anesthetized intact animal was not significantly improved by treatment with TBC3711, although a reduction was certainly noted. The apparent discrepancy may be owing to the different anesthesia (pentobarbital versus fentanyl), tidal volume (20 versus 15 mL/kg), or Fio2 (0.25 versus 0.40) used in thoracotomized animals compared with anesthetized intact animals. In fact, in the intact animal, the higher Fio2 may have contributed to reducing the differences between the hypoxic control group and the hypoxic treated group. Supporting this possibility is the fact that once the lungs were isolated and perfused, measurements of perfusion pressure showed complete recovery. Measurement of perfusion pressure in this preparation reflects PVR and excludes confounding variables from changes in the cardiac output and possibly from the ductus arteriosus, although the latter was not found to be contributing (results not shown). Furthermore, it is possible that significance was not reached because of the limited number of studies.
Left ventricular pressure was found to be reduced in the hypoxic group treated with TBC3711 compared with the hypoxic control group (Table 1). One explanation would be that TBC3711 causes systemic vasodilation. However, it is uncertain whether this change is physiologically significant because the values obtained in the hypoxic treated group do not differ from the normoxic groups. Studies in the intact anesthetized animal (Table 3) also suggest that TBC3711 reduces systemic vascular resistance without causing significant hypotension as cardiac output is, in fact, increased. Obviously, left ventricular pressure measured before lung removal is much lower than the aortic pressure obtained in the intact anesthetized animal. Most likely, this results from the effect of pentobarbital on the myocardium.
Saturation measured in the intact hypoxic animal was significantly decreased compared with the normoxic animal. Pulmonary vasoconstriction and vascular remodeling may lead to hypoxemia. However, we cannot exclude the presence of lung disease in these animals, which may have added to the aforementioned factors. In fact, in thoracotomized hypoxic animals, cardiomegaly was found to be associated with atelectasis. In these animals, we ensured full lung recruitment before making any measurement. Absence of atelectasis could not be ascertained in the intact hypoxic animal and may have contributed to the hypoxemia. Lastly, it is possible that a shunt at the atrial or ductal level may have also come into play.
In agreement with the work of others (33), we also found that chronic hypoxia is associated with decreased weight gain. In animals treated with TBC3711, weight gain was not improved compared with their respective controls. This probably suggests that diminished weight gain in hypoxia does not result, at least uniquely, from the presence of pulmonary hypertension, and is probably more related to changes in metabolism (34). As expected, Hb concentration increased in hypoxia. Of interest, Hb concentration failed to increase in the hypoxic animals treated with TBC3711. The reason for this finding is unclear. However, it has been suggested that both ET-1 and erythropoietin gene expression are stimulated by hypoxia and hypoperfusion (35, 36). Therefore, improving renal perfusion through ETA receptor blockade may reduce erythropoietin expression and, consequently, Hb. To confirm our hypothesis, one would have to measure systemic and renal blood flow in a conscious animal, and that was not done in this study.
In this setting, ET-1 circulating levels were increased by hypoxia. Similar findings were reported in an ovine model of pulmonary hypertension (16) and in human neonates with pulmonary hypertension (14). This differs from our previous report (15), in which we did not find an increase in ET-1 circulating levels with hypoxia, although receptor studies suggested that ET-1 levels must be increased. We think that the use of a better technology, QuantiGlo (R&D Systems), is responsible for this difference in findings. Increased circulating levels of ET-1 can be explained by the fact that hypoxia can both stimulate ET-1 gene and protein expression, as well as decrease ETB gene and protein expression in the ovine model (17) and the number of ETB binding sites (clearance receptor) in our piglet model (15). A decrease in the number of clearance receptors would result in increased ET-1 circulating levels. The fact that ET-1 levels were increased when the animals were treated with TBC3711, whether in normoxia or hypoxia, could suggest that this antagonist binds to ETB receptors or stimulates the synthesis or release of ET-1. However, binding studies confirmed that TBC3711 is highly specific for ETA receptors, and its specificity is even better than that reported for BQ-123 (37), making this explanation unlikely. Therefore, further studies should examine the effect of TBC3711 on ET-1 gene and peptide expression. One could question the impact of increased ET-1 circulating levels on pulmonary hemodynamics. In the context of ETA blockade, it could be beneficial. In other words, ET-1, by binding to ETB receptors, could enhance the release of NO and cause vasorelaxation and smooth muscle cell involution. ETB receptors have been shown to play an important role in the maintenance of pulmonary vascular tone (11). Further studies would need to be done to examine the consequences of increased ET-1 circulating levels when ETA blockade is abruptly interrupted.
In our neonatal model of hypoxia-induced pulmonary hypertension, we also showed that chronic treatment with a nonpeptidic specific ETA receptor antagonist not only reduces pulmonary vascular remodeling, but also appears to improve the dilator response to NO. In previous studies, we have shown that chronic hypoxia reduces the synthesis and vasodilator response to NO (18). As shown by Ivy et al.(27) in a preventive study with BQ-123, blockade of ETA receptor improves the dilator response to NO. One could argue that this improved dilator response solely reflects changes in vascular remodeling. Also, it is not excluded that U-46619, used mainly in normoxic and hypoxic-treated preparations, may have conditioned the response to the NO donor, SIN-1, or may have interacted with TBC3711. However, the use of U-46619 is justified by the fact that comparison of vasodilator responses among the different groups has to be made at comparable basal tone. As a matter of fact, we had shown previously that basal tone has an impact on the magnitude of the dilator response (8). With respect to the restored dilator response to NO, others have also suggested that treatment with an ET-1 antagonist of rats with monocrotaline-induced pulmonary hypertension increases endothelium-dependent and -independent vasodilation to NO (38) and corrects endothelial dysfunction (39). It is understood that our experiments only look at the response to NO after treatment with TBC3711, and not at how this antagonist affects the synthesis or release of NO. However, the fact that the reduction in exhaled NO seen in hypoxia was improved by treatment with TBC3711 may suggest that TBC3711 may also improve cellular function. Of course, the source of NO measured in expiration would have to be determined to make this conclusion. Although the upper airway had been excluded by the tracheostomy, exhaled NO could come from pulmonary vascular endothelium as well as airway epithelium and nerves (40). Further experiments using NO-dependent vasodilators are needed to confirm our findings with exhaled NO. Regarding the possible link between ETA antagonism and improved dilator response or endothelial function, further studies will have to be done to determine how TBC3711 may up-regulate NO synthesis or potentiate the dilator response. Knowing that ET-1 can activate protein kinase C, which is a link to vasoconstriction and vascular remodeling (41, 42), one could speculate that ETA receptor blockade may reduce protein kinase C activation, and therefore favor the response to NO.
Thus, our findings suggest that the selective ETA receptor antagonist, TBC3711, offers promise for the treatment of neonatal pulmonary hypertension because of its ability to decrease pulmonary vascular remodeling in the neonate and to possibly improve the dilator response to NO. Further studies are required to determine the mechanisms by which TBC3711 causes smooth muscle cell involution and may affect endothelial function.
Abbreviations
- ED:
-
external diameter
- ET-1:
-
endothelin-1
- ETA:
-
endothelin A receptor subtype
- ETB:
-
endothelin B receptor subtype
- Fico2:
-
fraction of inspired carbon dioxide
- Fio2:
-
fraction of inspired oxygen
- IC50:
-
concentration producing 50% inhibition
- ID:
-
internal diameter
- MSA:
-
medial surface area
- NO:
-
nitric oxide
- PAP:
-
pulmonary artery pressure
- ppb:
-
parts per billion
- PPHN:
-
persistent pulmonary hypertension of the newborn
- PVR:
-
pulmonary vascular resistance
- RV/LV+S:
-
right ventricle to left ventricle plus septum weight ratio
- Sao2:
-
arterial oxygen saturation
- SIN-1:
-
3-morpholinosydnonimine-N-ethylcarbamide
- WT:
-
wall thickness
References
Rudolph AM, Auld PA, Golinko RJ, Paul MH 1961 Pulmonary vascular adjustments in the neonatal period. Pediatrics 28: 28–34
Dukarm RC, Steinhorn RH, Morin FC III 1996 The normal pulmonary vascular transition at birth. In: Glick PL, Irish MS, Holm BA (eds) New Insights into the Pathophysiology of Congenital Diaphragmatic Hernia. Clinics in Perinatology; W.B. Saunders, Philadelphia, pp 711–726
Teitel DF, Iwamoto HS, Rudolph AM 1990 Changes in the pulmonary circulation during birth-related events. Pediatr Res 27: 372–378
Murphy JD, Rabinovitch M, Goldstein JD, Reid LM 1981 The structural basis of persistent pulmonary hypertension of the newborn infant. J Pediatr 98: 962–967
The Neonatal Inhaled Nitric Oxide Study Group 1997 Inhaled nitric oxide in full-term and nearly full-term infants with hypoxic respiratory failure. N Engl J Med 336: 597–604
MacCumber MW, Ross CA, Glaser BM, Snyder SH 1989 Endothelin: visualization of mRNAs by in situ hybridization provides evidence for local action. Proc Natl Acad Sci USA 86: 7285–7289
Chatfield BA, McMurtry IF, Hall SL, Abman SH 1991 Hemodynamic effects of endothelin-1 on ovine fetal pulmonary circulation. Am J Physiol 261: R182–R187
Perreault T, De Marte J 1991 Endothelin-1 has a dilator effect on the neonatal pig pulmonary vasculature. J Cardiovasc Pharmacol 18: 43–50
Masaki T, Vane JR, Vanhoutte PM 1994 International union of pharmacology nomenclature of endothelin receptors. Pharmacol Rev 46: 137–142
Fukuroda T, Fujikawa T, Ozaki S, Ishikawa K, Yano M, Nishikibe M 1994 Clearance of circulating endothelin-1 by ETB receptors in rats. Biochem Biophys Res Commun 199: 1461–1465
Ivy DD, Parker TA, Abman SH 2000 Prolonged endothelin B receptor blockade causes pulmonary hypertension in the ovine fetus. Am J Physiol 279: L758–L765
Fukuroda T, Kobayashi M, Ozaki S, Yano M, Miyauchi T, Onizuka M, Sugishita Y, Goto K, Nishikibe M 1994 Endothelin receptor subtypes in human versus rabbit pulmonary arteries. J Appl Physiol 76: 1976–1982
Perreault T, Baribeau J 1995 Characterization of endothelin receptors in newborn piglet lung. Am J Physiol 268: L607–L614
Rosenberg AA, Kennaugh AJ, Koppenhafer SL, Loomis M, Chatfield BA, Abman SH 1993 Elevated immunoreactive endothelin-1 levels in newborn infants with persistent pulmonary hypertension of the newborn. J Pediatr 123: 109–114
Gosselin R, Gutkowska J, Baribeau J, Perreault T 1997 Endothelin receptor changes in hypoxia-induced pulmonary hypertension in the newborn piglet. Am J Physiol 273: L72–L79
Ivy DD, Ziegler JW, Dubus MF, Fox JJ, Kinsella JP, Abman SH 1996 Chronic intrauterine pulmonary hypertension alters endothelin receptor activity in the ovine fetal lung. Pediatr Res 39: 435–442
Ivy DD, Le Cras TD, Horan MP, Abman SH 1998 Increased lung preproET-1 and decreased ETB-receptor gene expression in fetal pulmonary hypertension. Am J Physiol 274: L535–L541
Berkenbosch JW, Baribeau J, Perreault T 2000 Decreased synthesis and vasodilation to nitric oxide in piglets with hypoxia-induced pulmonary hypertension. Am J Physiol 278: L276–L283
Perreault T, Baribeau J, Gosselin R, Gutkowska J 1997 Reduced vasodilator response to ANF in hypoxia-induced pulmonary hypertension in the newborn piglet. Am J Physiol 273: L289–L295
Wu C, Decker ER, Blok N, Bui H, Knowles V, Bourgoyne A, Holland GW, Brock TA, Dixon RAF 2000 Discovery of potent, orally available, ETA selective endothelin antagonists: TBC3214 and TBC3711. Book of Abstracts 219th American Chemical Society National Meeting: San Francisco, CA, March 26–30, Abstract no. 233
Stavros FD, Hassel KW, Okun I, Baldwin J, Freriks K 1993 COS-7 cells stably transfected to express the human ETB receptor provide a useful screen for endothelin receptor antagonists. J Cardiovasc Pharmacol 22(suppl): S34–S37
Di Carlo VS, Chen S-J, Meng QC, Durand J, Yano M, Chen Y-F, Oparil S 1995 ETA-receptor antagonist prevents and reverses chronic hypoxia-induced pulmonary hypertension in rat. Am J Physiol 269: L690–L697
Colpaert C, Hogan J, Stark AR, Genest DR, Roberts D, Reid L, Kozakewich H 1995 Increased muscularization of small pulmonary arteries in preterm infants of diabetic mothers: a morphometric study in noninflated, noninjected, routinely fixed lungs. Pediatr Pathol Lab Med 15: 689–705
Moon PF, Scarlett JM, Ludders JW, Conway TA, Lamb SV 1995 Effect of fentanyl on the minimum alveolar concentration of isoflurane in swine. Anesthesiology 83: 535–542
Chen S-J, Chen Y-J, Meng QC, Durand J, Di Carlo VS, Oparil S 1995 Endothelin-receptor antagonist bosentan prevents and reverses hypoxic pulmonary hypertension in rats. J Appl Physiol 79: 2122–2131
Tilton RG, Munsch CL, Sherwood SJ, Chen S-J, Chen Y-F, Wu C, Block N, Dixon RAF, Brock TA 2000 Attenuation of pulmonary vascular hypertension and cardiac hypertrophy with sitaxentan sodium, an orally active ETA receptor antagonist. Pulm Pharmacol Ther 13: 87–97
Ivy DD, Parker TA, Ziegler JW, Galan HL, Kinsella JP, Tuder RM, Abman SH 1997 Prolonged endothelin A receptor blockade attenuates chronic pulmonary hypertension in the ovine fetus. J Clin Invest 99: 1179–1186
Albert CJ, Ford DA 1999 Protein kinase C translocation and PKC-dependent protein phosphorylation during myocardial ischemia. Am J Physiol 276: H642–H650
Widimsky J, Urbanova D, Ressel J, Qstadal B, Pelouch V, Prochazka J 1973 Effect of intermittent altitude hypoxia on the myocardium and lesser circulation in the rat. Cardiovasc Res 7: 798–808
Abraham AS, Key JM, Cole RB, Pincock AC 1971 Haemodynamic and pathological study of the effect of chronic hypoxia and subsequent recovery of the heart and pulmonary vasculature of the rat. Cardiovasc Res 5: 95–102
Rabinovitch M, Gamble W, Nadas AS, Miettinen OS, Reid L 1979 Rat pulmonary circulation after chronic hypoxia: hemodynamic and structural features. Am J Physiol 236: H818–H827
Stenmark KR, Mecham RP 1997 Cellular and molecular mechanisms of pulmonary vascular remodeling. Annu Rev Physiol 59: 89–144
Fike CD, Kaplowitz MR 1996 Chronic hypoxia alters nitric oxide-dependent pulmonary vascular responses in lungs of newborn pigs. J Appl Physiol 81: 2078–2087
Mortola JP, Gautier H 1995 Interaction between metabolism and ventilation: effects of respiratory gases and temperature. In: Dempsey JA, Pack AI (eds) Regulation of Breathing, 2nd Ed. Marcel Dekker, New York, pp 1011–1064
Ratcliffe PJ, Jones RW, Philipps RE, Nicholls LG, Bell JI 1990 Oxygen-dependent modulation of erythropoietin mRNA levels. J Exp Med 172: 657–660
Ritthaler T, Gopfert T, Firth JD, Ratcliffe PJ, Kramer BK, Kurtz A 1996 Influence of hypoxia on hepatic and renal endothelin gene expression. Pflugers Arch 431: 587–593
Ihara M, Noguchi K, Saeki T, Fukuroda T, Tsuchida S, Kimura S, Fukami T, Ishikawa K, Nishikibe M, Yano M 1992 Biological profiles of highly potent novel endothelin antagonists selective for the ETA receptor. Life Sci 50: 247–255
Prié S, Stewart DJ, Dupuis J 1998 EndothelinA receptor blockade improves nitric oxide-mediated vasodilation in monocrotaline-induced pulmonary hypertension. Circulation 97: 2169–2174
Prié S, Leung TK, Cernacek P, Ryan JW, Dupuis J 1997 The orally active ETA receptor antagonist (+)-(S)-2-(4,6-dimethoxy-pyridin-2-yloxy)-3-methoxy-3,3-diphenyl-propionic acid (LU 135252) prevents the development of pulmonary hypertension and endothelial metabolic dysfunction in monocrotaline-treated rats. J Pharmacol Exp Ther 282: 1312–1318
Kobzik L, Bredt DS, Lowenstein CJ, Drazen J, Gaston B, Sugarbaker D, Stamler JS 1993 Nitric oxide synthase in human and rat lung; immunocytochemical and histochemical localization. Am J Respir Cell Biol 9: 371–377
Assender JW, Irenius E, Fredholm BB 1996 Endothelin-1 causes a prolonged protein kinase C activation and acts as a co-mitogen in vascular smooth muscle cells. Acta Physiol Scand 157: 451–460
Ohno S 1997 The distinct biological potential of PKC isotypes. In: Parker P, Dekker LV (eds) Protein Kinase C. Springer, London, pp 75–95
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by the Medical Research Council (MT-12973) and La Fondation du Québec des maladies du coeur.
Rights and permissions
About this article
Cite this article
Perreault, T., Berkenbosch, J., Barrington, K. et al. TBC3711, an ETA Receptor Antagonist, Reduces Neonatal Hypoxia-Induced Pulmonary Hypertension in Piglets. Pediatr Res 50, 374–383 (2001). https://doi.org/10.1203/00006450-200109000-00013
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200109000-00013
This article is cited by
-
Therapeutic efficacy of TBC3711 in monocrotaline-induced pulmonary hypertension
Respiratory Research (2011)
-
Intravenous tezosentan improves gas exchange and hemodynamics in acute lung injury secondary to meconium aspiration
Intensive Care Medicine (2008)