Abstract
Streptococcus agalactiae (group B streptococcus, GBS) is the major pathogen of neonatal sepsis. In some newborns, GBS sepsis may have a severe course, including septic shock with a high mortality rate, whereas other newborns are colonized with GBS on their surfaces without any clinical signs of bacterial infection. The reason for this discrepancy is far from clear. We sought, in this study, to compare cytokine expression in cord blood mononuclear cells after stimulation with GBS strains isolated from newborns with sepsis, and strains isolated from newborns without any symptoms of invasive infection. Cord blood mononuclear cells were incubated with either heat-killed bacteria of different strains or lipopolysaccharide, respectively. After 6 and 24 h, cells were harvested and cytokine mRNA-expression was analyzed by reverse-transcriptase PCR. Likewise, supernatants were tested for IL-6 and tumor necrosis factor-α concentrations by enzyme immunoassay. When comparing IL-6 and tumor necrosis factor-α secretion, there were significantly higher IL-6 levels after stimulation with sepsis than with colonizing isolates. Likewise, mRNA expression of IL-6, IL-1β, and IL-12p40 was significantly higher after stimulation with sepsis isolates. This was also true when normalizing to cytokine expression after stimulation with lipopolysaccharide. These findings indicate that the different clinical pictures in response to GBS, either septic infection or colonization, might reflect strain-specific properties. If the respective characteristics can be defined, it might become possible to distinguish by molecular methods potentially “dangerous” from “harmless” strains. Moreover, our findings underline the essential role of these cytokines in the pathogenesis of neonatal GBS sepsis.
Similar content being viewed by others
Main
Bacterial sepsis remains one of the leading causes of neonatal morbidity and mortality worldwide(1–3). Susceptibility to bacterial infections is thought to be due to an immature neonatal immune system with a decreased power of antimicrobial defense mechanisms. Reduced secretion of cytokines like TNF-α, IFN-γ, IL-1β, IL-6, IL-8, and IL-12 has been described in neonatal cells when compared with adult cells(4–11). In contrast, it has been shown in vivo by several groups, including our own, that in neonatal sepsis, plasma levels and mRNA expression of cytokines are highly elevated(12, 13).
Bacterial sepsis occurs in the neonatal period more frequently than in any other period in life. Streptococcus agalactiae (GBS), in particular, is the most important single pathogen, accounting for as much as one third to one half of all cases of neonatal early-onset sepsis(2, 3). The mechanisms leading to this predominance of GBS, which was established in the 1960s, are far from clear. A large variety of pathogenic bacteria colonize the maternal genital tract but only rarely cause septic infection of the neonate. There might be virulence factors of GBS that promote colonization of the neonate during labor with subsequent invasive disease. For example, the C protein β-antigen of GBS, with its unique property of binding to the Fc portion of human IgA, has been thought to be involved in the pathogenesis of GBS sepsis(14, 15). Other virulence factors include the expression of polysaccharide antigens, especially that of serotype III(16), the hemolysins(17), and laminin(18). However, these factors can be found among both invasive and colonizing strains, suggesting that there are additional factors involved in pathogenicity(15). It has been shown for several other pathogens that there are strain-specific properties that distinguish colonizing from disease-causing strains. Of Streptococcus pyogenes it has been stated that invasion of eukaryotic cells is different between invasive and sore throat–causing isolates(19).
In this study, we sought to compare the expression of different proinflammatory cytokines in cord blood cells in response to stimulation by different ex vivo isolates of GBS. We compared isolates from patients with sepsis and isolates from healthy colonized neonates. For the majority of GBS isolates from patients with sepsis, data on cytokine plasma levels from cord blood samples were available. We aimed to investigate in a cell culture model whether the in vivo finding of a high cytokine expression induced by “sepsis strains” is reproducible in vitro, and whether cytokine expression is more pronounced upon stimulation with “sepsis” than with “colonizing strains.” CBMNC from healthy newborns were used as a model to study the cytokine expression induced by heat-killed clinical strains of GBS. We investigated TNF-α and IL-1β as representative cytokines of the first-line immune response, IL-6 and IL-8 as second-line following the expression of TNF-α and IL-1β, and IL-12 as a key mediator for priming T-helper clones upon antigenic stimulation for development into the subtype of T-helper 1 cells, which are essential for T-cellular antimicrobial defense mechanisms.
MATERIALS AND METHODS
Blood samples
Blood samples from the umbilical cords of 11 healthy, full-term neonates after scheduled cesarean section (n = 5) or vaginal delivery (n = 6) were obtained by puncture of the cord immediately after delivery. Newborns were free of bacterial infection during a follow-up of 1 wk. The samples were collected in heparinized syringes and processed within 2 h of collection. Parental informed consent was obtained for every patient before entry in the study. The study was approved by the local ethics committee.
Isolation of CBMNC
Before preparation by Ficoll-Hypaque gradients, cord blood was diluted 1:1 by Hanks’ balanced salt solution (HBSS). Mononuclear cells were separated from whole blood by sedimentation on Ficoll-Hypaque gradients (density = 1.077 g/mL) (GIBCO BRL, Eggenstein, Germany) for 30 min. The cells were washed twice with endotoxin-free HBSS and resuspended for culture in RPMI 1640 (GIBCO BRL) culture medium supplemented with 10% heat-inactivated FCS (GIBCO BRL). Mononuclear cells were purified by this method to homogeneity of >90%. Cell viability, as measured by trypan blue exclusion, was >99%. The cells were plated at a density of 1 × 106 cells/mL in culture medium at a final volume of 1 mL in 24-well plates (Falcon, Becton-Dickinson, Lincoln Park, NJ, U.S.A.). The number of stimulation experiments that was performed with each cord blood sample was dependent on the volume of cord blood obtained. As a rule, four to eight stimulation experiments per cord blood sample could be performed.
Bacterial isolates
The strains used for stimulation experiments were isolated from neonates with sepsis (group 1), who have been characterized in previous studies(12, 13). Strains were collected immediately after birth either from the blood or cerebrospinal fluid (n = 6) or from the urine or meconium (n = 8) of newborns who developed signs and symptoms of severe bacterial sepsis. As a control, GBS isolates were used from the superficial swabs of healthy newborns (n = 8) taken within 24 h after birth who remained free of clinical or laboratory signs of infection (group 0). As a rule, bacteria cultured from clinical specimens were subcultured on a blood agar plate to identify single colonies. From these colonies, cultures were directly—without further cultural steps—grown in brain heart infusion broth (BHI) for 6 to 8 h and collected during the logarithmic bacterial growth phase. Bacteria were washed several times in endotoxin-free HBSS and then stocked in 30% glycerol at −70°C. For stimulation experiments, bacterial stocks were thawed once, washed several times with HBSS, and then diluted up to the appropriate concentration. Colony forming units were determined for each experiment by serial dilution and plating on Mueller-Hinton agar. GBS strains from group 1 belonged to the serotypes Ia, Ib, II, or III, and strains from group 0 belonged to the serotypes Ia, Ia/c, or III or were nontypeable (Table 1).
Stimulation experiments
In total, 41 stimulation experiments were performed for GBS strains of the septic group, and 24 experiments for colonizing strains. Stimulation experiments were performed in triplicate for each strain with CBMNC from different donors. For one strain of the septic group, stimulation experiments with only two different CBMNC samples could be performed due to technical problems. Cells were stimulated with heat-killed bacteria at 107/mL and, as a control, with LPS (from Escherichia coli O111:B4) (Sigma Chemical Co., St. Louis, MO, U.S.A.) at 2 μg/mL. After 6 and 24 h of incubation at 37°C at 5% CO2 atmosphere, cells were harvested and lysed in a buffer containing guanidinium thiocyanate, sodium citrate, sarkosyl, and mercaptoethanol for RNA analysis. The supernatant was stored at −30°C until use in the enzyme-linked immunoassay (EIA).
RNA isolation and reverse transcription
Total RNA was prepared using the phenol-chloroform extraction method reported by Chromczynski and Sacchi(20) and described in detail previously(12). For reverse-transcriptase reaction, an aliquot of 50 ng RNA in a volume of 8.5 μL was incubated with 2 μL oligo-dT (10 to 18mer, 25 ng/μL) at 65°C for 10 min. After cooling on ice, the mixture was incubated with 4 μL 5 × reverse-transcriptase buffer (250 mM Tris-HCl, pH 8.3, 375 mM KCl, 15 mM MgCl2), 2 μL DTT (0.1 M), 2 μL deoxyribonucleoside triphosphate (dNTP) (10 mM), 0.5 μL RNase inhibitor (Boehringer, Mannheim, Germany), and 1 μL Moloney murine leukemia virus reverse transcriptase (Superscript®, GIBCO BRL) in a final volume of 20 μL for 60 min at 37°C, then heated to 95°C for 10 min and cooled on ice. Resulting cDNA was stored at −30°C until further use.
PCR-assisted mRNA amplification
Five microliters of cDNA was amplified in the presence of 10 pM final concentration of the respective primer pairs (Table 2)(21), 200 μM dNTP, 1 U of Taq polymerase (Pharmacia, Freiburg, Germany), and 5 μL 10 × PCR buffer (500 mM KCl, 15 mM MgCl2, 100 mM Tris-HCl pH 9.0) in a final volume of 50 μL. The reaction mixture was overlaid with the same volume of light mineral oil, and PCR was performed in a DNA thermal cycler (OmniGene, Hybaid, Teddington, England) for 30 cycles in all experiments: 60 s denaturation at 94°C, 60 s annealing at 56°C, and 60 s extension at 72°C(21). PCR-assisted mRNA amplification was repeated at least twice for each sample. Cellular samples were considered to be evaluable if mRNA of β-actin was detectable. The reaction product was visualized by subjecting to electrophoresis 20 μL of the reaction mix at 80 V in 2% agarose in 0.5 × TBE (Tris-borate-EDTA) buffer. Specificity of the amplified bands was validated by their predicted size. Because the primers used in this study surround splice sites in the cellular targets, PCR products of the cDNA were different in size from the respective genomic DNA PCR product. In addition, control PCR reaction with total RNA was carried out to exclude genomic contamination. The expected sizes of the cDNA PCR products were 237 bp for β-actin, 263 bp for IL-1β, 427 bp for TNF-α, 260 bp for IL-6, and 247 bp for IL-8. For IL-12, which is a heterodimeric cytokine composed of the covalently linked subunits, p35 and p40, we examined the mRNA expression of the p40 subunit, which has been shown to be accumulated in cord blood mononuclear cells following bacterial stimulation(9). The expected size of the IL-12p40 PCR product was 296 bp.
For semiquantitative evaluation of cytokine expression, mRNA expression was ranked from 0 to 4 and normalized visually to the expression of β-actin, as described previously(13). In brief, PCR was performed on target cDNA serially diluted 4-fold. Samples were determined to contain similar amounts of amplifiable cDNA when the dilution at which equally dense bands were visualized during electrophoresis was the same for both samples tested. In addition, cytokine mRNA expression after stimulation with GBS was compared for each cytokine with that of LPS. Evaluation was performed without knowledge of the evaluating person to which group the stimulating GBS strain belonged. Cytokine mRNA levels are given as means and SEM.
IL-6 and TNF-α EIA
Frozen aliquots of cell culture supernatants were thawed on ice at the time of analysis. Cytokine concentrations were measured by a double-sandwich EIA technique using a commercial kit specific for IL-6 and TNF-α (Milenia, DPC Biermann, Bad Nauheim, Germany). The detection limits of both assays are defined as the lowest concentration of the calibrator provided by the test kits. As indicated by the manufacturer, these are 15.6 pg/mL for both IL-6 and TNF-α. Duplicate measurements were performed for each sample. Samples were diluted before analysis if necessary. Dilution buffer was provided by the manufacturer. Cytokine values are expressed as medians, quartiles, and ranges.
Statistical analysis
The differences between the mean values of cytokine mRNA levels were analyzed by the unpaired t test. The differences between the median values of cytokine concentrations were analyzed by the Wilcoxon-Mann-Whitney test. Analyses were performed using the SPSS software package (version 8.0, SPSS, Chicago, IL, U.S.A.). Differences were considered significant at p < 0.05.
RESULTS
Patient characteristics
One half of the sepsis isolates were cultured from either the blood or cerebrospinal fluid. The other half of the strains were recovered from the urine or meconium of newborns suffering from severe sepsis syndrome, but whose blood cultures, for some reason, had remained sterile. The majority of newborns with sepsis (12/14) had been characterized with respect to cytokine plasma levels in previous studies(12, 13). In brief, plasma levels of newborns with GBS sepsis were highly elevated, with a median of 6029 pg/mL for IL-6 (100 pg/mL), 6630 pg/mL for IL-8 (300 pg/mL), 11,690 pg/mL for granulocyte-colony stimulating factor (500 pg/mL), and 67 mg/L for CRP (6 mg/L). The cut-off values for the detection of neonatal sepsis as used previously are given in brackets(12).
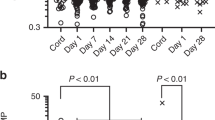
Cytokine mRNA expression
In each cellular sample, mRNA of β-actin was detected, confirming that all stimulation experiments were evaluable for analysis. For each experiment, TNF-α, IL-1β, IL-6, IL-8, and IL-12p40 mRNA expression after stimulation with GBS strains was compared with that after stimulation with LPS. To rule out blood sample–specific differences, the cytokine mRNA expression after stimulation with sepsis or colonizing GBS strains was normalized to the cytokine expression in the same experiment after stimulation with LPS. When comparing IL-6, IL-1β, and IL-12p40 expression after 24 h between sepsis and colonizing strains of GBS, a significant difference was observed, whereas no statistically significant difference was observed for the expression of TNF-α and IL-8 (Fig. 1, A–E). Generally, it was observed that cytokine mRNA expression was higher after 6 h than after 24 h. Within the septic group, there was no difference in cytokine expression after stimulation with strains isolated from the blood (or cerebrospinal fluid) and those isolated from the urine or meconium (data not shown). Likewise, there was no difference in cytokine expression after stimulating CBMNC collected after cesarean section or spontaneous delivery, neither within the group of sepsis strains nor within the group of colonizing strains (data not shown).
Comparison of cytokine gene expression after stimulation of CBMNC with colonizing (black columns) or sepsis (open columns) strains of GBS for 6 h (left side) and 24 h (right side), respectively: (A) IL-1β, (B) IL-6, (C) IL-8, (D) IL-12p40, and (E) TNF-α. For semiquantitative evaluation of cytokine expression, mRNA expression was ranked from 0 to 4 and normalized visually to the expression of β-actin, as described previously(13). The mean rank and SEM are indicated. Differences were considered significant at p < 0.05.
IL-6 and TNF-α EIA
When comparing IL-6 concentrations in supernatants of CBMNC cultures after stimulation for 24 h, there was a significantly higher expression of IL-6 after stimulation with sepsis than with colonizing strains (9126 versus 4632 pg/mL, p < 0.05). TNF-α concentrations, likewise, were higher after stimulation with sepsis than with colonizing strains (5124 versus 3951 pg/mL). This difference, however, did not reach statistical significance (Table 2). Furthermore, when calculating the ratio of IL-6 expression after stimulation with sepsis strains and after that with LPS, and comparing it to the ratio of IL-6 expression after stimulation with colonizing strains and after that with LPS, a significant difference was observed after incubating for 24 h (12.8 versus 1.4, p < 0.05). The ratio in comparison to LPS illustrates the strong capacity of sepsis strains to stimulate cord blood cells for cytokine secretion.
When comparing sepsis and colonizing strains of serotype III, which was the most common serotype used in our experiments, we observed a higher cytokine secretion in stimulation experiments with sepsis (n = 12) than with colonizing strains (n = 6). This difference, however, did not reach statistical significance (p = 0.34), probably due to the limited number of experiments. The median concentration of IL-6 at 24 h of stimulation was 12,300 pg/mL (quartiles 2318–15,994) versus 2389 pg/mL (quartiles 1725–7814).
DISCUSSION
In this study, we demonstrated that GBS strains isolated from neonates with sepsis had a significantly higher inductive capacity to stimulate cytokine expression in CBMNC than strains from healthy newborns who were colonized with GBS without any clinical or laboratory evidence of infection. We assumed in this model that in vitro cytokine expression in cord blood cells might be a reliable surrogate marker for bacterial virulence in the setting of neonatal sepsis. In recent years, several groups, including our own, have demonstrated that neonatal sepsis is accompanied in vivo by highly elevated cytokine plasma levels(12). It has been shown that cytokine production is endogenous to the neonate by demonstrating mRNA expression in cord blood cells ex vivo(13). In the present study, CBMNC were used to determine the capacity of different GBS isolates to induce cytokine production. Given the fact that sepsis is associated with high cytokine production in vivo, cytokine production in vitro might offer a model to study virulence of different bacterial strains.
We consciously chose in this study to use ex vivo clinical isolates and not reference strains or isogenic mutants. Our intention was to test whether sepsis strains irrespective of their serotypes or other well-defined determinants induce a higher cytokine response than colonizing strains in vitro as they do in vivo. There are known virulence factors of GBS, such as the capsular polysaccharide of serotype III, a major subgroup of invasive isolates belongs to serotype III, but there are noninvasive strains of the same serotype. The same is true for other virulence factors, such as the expression of the C protein β-antigen. Although the number of strains of serotype III tested in our study was rather small, and therefore conclusions have to be drawn with caution, we found a more pronounced—but not statistically significant—inductive capacity of sepsis than of colonizing strains of this serotype. This observation would support the data reported by Williams et al.(11), who demonstrated that production of TNF-α after stimulation with encapsulated and unencapsulated isogenic mutant of type III GBS was similar. Moreover, these findings suggest that there must be additional characteristics of GBS that have a major impact on the induction of the inflammatory response. Further research is needed to define these strain-specific properties that—according to their association to cytokine expression and, therefore, disease—are to be considered as true factors correlated with pathogenicity.
We included in our study strains from septic patients that did not grow in the blood but in the meconium or in the urine. In these cases, we assumed that the strains were identical to the septicemic strains. This, in fact, is only an assumption. It seems rather probable, however, that GBS first colonize the gastrointestinal tract and thereafter invade the host. Therefore, it is reasonable to believe that the bacteria isolated from the a priori sterile meconium or urine will be the ones responsible for septicemia. It cannot be excluded, however, that only certain clones of a bacterial species that colonizes the gastrointestinal tract are invading their host. In addition, one might consider that whatever differences are observed may not reflect true strain differences but rather may be due to the expression of virulence factors in vivo; during invasive infection, bacteria may switch on virulence genes that are not expressed during the colonization stage. We used in this study the same laboratory conditions for isolating and growing colonizing and sepsis strains, and we consciously avoided multiple cultural steps. Therefore, we suppose that strain-specific characteristics were indeed analyzed in our experimental setting. One might consider in further studies, however, analyzing, for example, meconium isolates of GBS from newborns who subsequently develop sepsis and comparing these isolates with those obtained from the blood of the same patients during sepsis.
The role of Gram-positive bacteria in causing release of cytokines such as TNF-α, IL-1β, or IL-6 by human neonatal cells has not been thoroughly explored. Gram-positive cell wall components like lipoteichoic acid(22) and DNA of Gram-positive bacteria displaying a relative abundance of unmethylated CpG motifs have been shown recently to contribute to activation of the monocyte/macrophage system(23). β2 integrins like the complement receptors 3 and 4 as well as human Toll-like receptors have been reported to be involved in the cytokine response to GBS and Listeria monocytogenes. Although they might have a crucial function in the pathogenesis of sepsis caused by Gram-positive bacteria(24, 25), their role in neonatal GBS sepsis, however, remains elusive. Whereas Williams et al.(11) described an increased release of TNF-α from neonatal cells after stimulation with GBS compared with that from adults, others reported a reduced capacity of blood cells from neonates to express IL-6 in response to GBS(26). In this study, we examined a number of cytokines that are thought to be essentially involved in the activation of the immune system by Gram-positive pathogens and to be key mediators in the pathogenesis of sepsis syndrome(27). We showed that IL-1β and IL-6 were significantly elevated after stimulation with sepsis strains, reflecting the high induction of gene expression of first- and second-line proinflammatory cytokines. This confirms strongly the essential role of these mediators in the pathogenesis of GBS sepsis. Moreover, we found a higher gene expression of the p40 subunit of IL-12 after stimulation with sepsis strains. This is in support of data of Scott et al., who described high-level IL-12 production in CBMNC, but in contrast to Lee et al.(5), who observed a decreased IL-12 expression from activated cord versus adult peripheral blood mononuclear cells. Scott et al.(9) stimulated with a Gram-positive bacterial pathogen (Staphylococcus aureus), and we also stimulated with Gram-positive bacteria (GBS). It has been shown recently that Gram-positive bacteria seem to induce preferentially IL-12 production(28).
Whereas the expression of IL-1β, IL-12p40, and IL-6 was increased after 24 h of stimulation, the expression of IL-8 and TNF-α was not significantly enhanced. The reason for this discrepancy is not very clear. One might speculate that there is an a priori reduced capacity of neonatal cells to produce TNF-α and IL-8. Therefore, a difference between invasive and colonizing isolates might not be detectable. It has been shown that in cord blood cells the expression of certain cytokines such as IL-6 is higher when compared with adult blood cells, whereas that of other cytokines such as IL-2, IFN-γ, or TNF-α is decreased(29, 30). Although the findings of high levels of mRNA expression and plasma levels of both TNF-α and IL-8 in vivo do not support the hypothesis(12, 13), we suppose that this phenomenon might have had some influence on our results. Furthermore, due to the physiologic variation between cytokine expression in individual cord blood samples, the number of experiments in this study might have been too small to detect statistically significant differences. Interestingly, for TNF-α, in contrast to the other cytokines, a greater difference—although not statistically significant—was observed after 6 than after 24 h (Table 3), which might be explained by the immediate expression of TNF-α upon stimulation of virulent bacteria.
In summary, one can speculate that, if the evidence provided by our results is supported by additional experimental data, the identification of the factors associated with immunostimulation could change clinical practice. It might become possible to screen GBS isolates from maternal swabs for their pathogenic properties. At present, prevention strategies of GBS sepsis include large-scale peripartal antibiotic administration to those mothers who are identified as at an increased risk, e.g. having a history of a previous infant with GBS disease or GBS bacteriuria during pregnancy(31–33). However, if strain-specific characteristics can be identified, it will be cost-effective in the long run—both in a microbiological and an economic sense—to screen vaginal swabs for virulence factors of GBS and to treat only the subgroup of those mothers who are colonized with pathogenic strains.
Abbreviations
- CBMNC:
-
cord blood mononuclear cells
- CRP:
-
C-reactive protein
- GBS:
-
group B streptococci
- IFN-γ:
-
interferon-γ
- LPS:
-
lipopolysaccharide
- MNC:
-
mononuclear cells
- TNF-α:
-
tumor necrosis factor-α
REFERENCES
Siegel JD, McCracken GH Jr 1981 Sepsis neonatorum. N Engl J Med 304: 642–647
Berner R, Schumacher RF, Bartelt S, Forster J, Brandis M 1998 Bacteremia in hospitalized children: predisposing conditions and case-related microorganisms. Eur J Clin Microbiol Infect Dis 17: 337–340
Gladstone IM, Ehrenkranz RA, Edberg SC, Baltimore RS 1990 A ten-year review of neonatal sepsis and comparison with the previous fifty-year experience. Pediatr Infect Dis J 9: 819–825
Ansart-Pirenne H, Soulimani N, Tartour E, Blot P, Sterkers G 1999 Defective IL2 gene expression in newborn is accompanied with impaired tyrosine-phosphorylation in T cells. Pediatr Res 45: 453–459
Lee SM, Suen Y, Chang L, Bruner V, Qian J, Indes J, Knoppel E, Van de Ven C, Cairo MS 1996 Decreased interleukin-12 (IL-12) from activated cord versus adult peripheral blood mononuclear cells and upregulation of interferon-γ, natural killer, and lymphokine-activated killer activity by IL-12 in cord blood mononuclear cells. Blood 88: 945–954
Lewis DB, Wilson CB 1995 Developmental immunology and role of host defenses in neonatal susceptibility to infection. In: Remington JS, Klein JO (eds) Infectious Diseases of the Fetus and Newborn Infant, 4th Ed. Saunders, Philadelphia, pp 20–99
Schibler KR, Liechty KW, White WL, Rothstein G, Christensen RD 1992 Defective production of interleukin-6 by monocytes: a possible mechanism underlying several host deficiencies of neonates. Pediatr Res 31: 18–21
Schultz S, Rott C, Richter N, Bucsky P, Reiss I, Gortner L 1999 Intracytoplasmatic detection of cytokines in neonatal lymphocytes and monocytes by flow cytometry. Blood 93: 3566–3567
Scott ME, Kubin M, Kohl S 1997 High level interleukin-12 production, but diminished interferon-γ production, by cord blood mononuclear cells. Pediatr Res 41: 547–553
Weatherstone K, Rich E 1989 Tumor necrosis factor/cachectin and interleukin-1 secretion by cord blood monocytes from premature and term neonates. Pediatr Res 25: 342–346
Williams PA, Bohnsack JF, Augustine NH, Drummond WK, Rubens CE, Hill HR 1993 Production of tumor necrosis factor by human cells in vitro and in vivo, induced by group B streptococci. J Pediatr 123: 292–300
Berner R, Niemeyer CM, Leititis JU, Funke A, Schwab C, Rau U, Richter K, Tawfeek MSK, Clad A, Brandis M 1998 Plasma levels and gene-expression of G-CSF, TNF-α, IL-1β, IL-6, IL-8, and sICAM-1 in neonatal early-onset sepsis. Pediatr Res 44: 469–477
Berner R, Tüxen B, Clad A, Forster J, Brandis M 2000 Elevated gene-expression of interleukin-8 in cord blood is a sensitive marker of neonatal infection. Eur J Pediatr 159: 205–210
Chun CSY, Brady LJ, Boyle MDP, Dillon HC, Ayoub EM 1991 Group B streptococcal C protein-associated antigens: association with neonatal sepsis. J Infect Dis 163: 786–791
Berner R, Bender A, Rensing C, Forster J, Brandis M 1999 Low prevalence of the immunoglobulin A binding β antigen of the C protein among Streptococcus agalactiae isolates causing neonatal sepsis. Eur J Clin Microbiol Infect Dis 18: 545–550
Schuchat A 1998 Epidemiology of group B streptococcal disease in the United States: shifting paradigms. Clin Microbiol Rev 11: 497–513
Spellerberg B, Pohl B, Haase B, Martin S, Weber-Heynemann J, Lütticken R 1999 Identification of genetic determinants for the hemolytic acitivity of Streptococcus agalactiae by ISS1 transposition. J Bacteriol 181: 3212–3219
Spellerberg B, Rodzinski E, Martin S, Weber-Heynemann J, Schnitzler N, Lütticken R, Podbielski A 1999 Lmb, a protein with similarities to the LraI adhesin family, mediates attachment of Streptococcus agalactiae to human laminin. Infect Immun 67: 871–878
Molinari G, Chhatwal GS 1998 Invasion and survival of Streptococcus pyogenes in eukaryotic cells correlates with the source of the clinical isolates. J Infect Dis 177: 1600–1607
Chomczynski P, Sacchi N 1987 Single-step method of RNA isolation by acid guanidium thiocyanate-phenol-chloroform extraction. Anal Biochem 162: 156–163
Bouaboula M, Legoux P, Pessegue, Delpech B, Dumont X, Piechaczyk M, Casellas P, Shire D 1992 Standardization of mRNA titration using a polymerase chain reaction method involving co-amplification with a multispecific internal control. J Biol Chem 267: 21830-21838–21838
Medvedev AE, Flo T, Ingalls RR, Golenbock DT, Teti G, Vogel SN, Espevik T 1998 Involvement of CD14 and complement receptors CR3 and CR4 in nuclear factor-B activation and TNF production induced by lipopolysaccharide and group B streptococcal cell walls. J Immunol 160: 4535–4542
Sparwasser T, Miethke T, Lipford G, Erdmann A, Häcker H, Heeg K, Wagner H 1997 Macrophages sense pathogens via DNA motifs: induction of tumor necrosis factor-alpha-mediated shock. Eur J Immunol 27: 1671–1679
Cuzzola M, Mancuso G, Beninati C, Biondo C, Genovese F, Tomasello F, Flo TH, Espevik T, Teti G 2000 β2 integrins are involved in cytokine responses to whole gram-positive bacteria. J Immunol 164: 5871–5876
Flo TH, Halaas O, Lien E, Ryan L, Teti G, Golenbock DT, Sundan A, Espevik T 2000 Human Toll-like receptor 2 mediates monocyte activation by Listeria monocytogenes, but not by group B streptococci or lipopolysaccharide. J Immunol 164: 2064–2069
Yachie A, Takano N, Ohta K, Uehara T, Fujita S, Miyawaki T, Taniguchi N 1992 Defective production of IL-6 in very small premature infants in response to bacterial pathogens. Infect Immun 60: 749–753
Sáez-Llorens X, McCracken GH Jr 1992 Sepsis syndrome and septic shock in pediatrics: current concepts of terminology, pathophysiology, and management. J Pediatr 123: 497–508
Hessle C, Anderson B, Wold AE 2000 Gram-positive bacteria are potent inducers of monocytic interleukin-12 (IL-12) while gram-negative bacteria preferentially stimulate IL-10 production. Infect Immun 68: 3581–3586
Chalmers IMH, Janossy G, Contrera M, Navarrete C 1998 Intracellular cytokine profile of cord and adult blood lymphocytes. Blood 92: 11–18
Chang M, Suen Y, Lee SM, Baly D, Buzby JS, Knoppel E, Wolpe S, Cairo MS 1994 Transforming growth factor-β1, macrophage inflammatory proteine-1α, and interleukin-8 gene expression is lower in stimulated human neonatal compared with adult mononuclear cells. Blood 84: 118–124
Schrag SJ, Zywicki S, Farley MM, Reingold AL, Harrison LH, Lefkowitz LB, Hadler JL, Danila R, Cieslak PR, Schuchat A 2000 Group B streptococcal disease in the era of intrapartum prophylaxis. N Engl J Med 342: 15–20
Centers for Disease Control 1996 Prevention of perinatal group B streptococcal disease: a public health perspective. MMWR Morb Mortal Wkly Rep 45: 1–24
American Academy of Pediatrics. Committee on Infectious Disease and Committee on Fetus and Newborn 1997 Revised guidelines for prevention of early-onset group B streptococcal (GBS) infection. Pediatrics 99: 489–496
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported, in part, by grants of the Deutsche Forschungsgemeinschaft (Be 1756/2–1).
Rights and permissions
About this article
Cite this article
Berner, R., Csorba, J. & Brandis, M. Different Cytokine Expression in Cord Blood Mononuclear Cells after Stimulation with Neonatal Sepsis or Colonizing Strains of Streptococcus agalactiae. Pediatr Res 49, 691–697 (2001). https://doi.org/10.1203/00006450-200105000-00014
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200105000-00014
This article is cited by
-
Neonatal immune cells have heightened responses following in-utero exposure to chorioamnionitis or COVID-19
Pediatric Research (2023)
-
Group B streptococci infection model shows decreased regulatory capacity of cord blood cells
Pediatric Research (2022)
-
Early neonatal streptococcal infection
The Indian Journal of Pediatrics (2006)