Abstract
The cosecretion of pancreatic lipase and colipase are important in normal fat digestion. As adsorption of phosphatidylcholine to the lipid substrate interferes with lipase activity, hydrolysis to lysophosphatidylcholine with subsequent desorption is also essential for fat digestion. There are some data regarding the secretion of pancreatic phospholipases in normal adults but none in children or patients with pancreatic disease. In the present study, we aimed a) to develop an accurate fast assay method to measure phospholipase A2 and b) to determine the secretion rate of pancreatic phospholipase A2 and whether it is cosecreted with lipase and colipase in children with exocrine pancreatic dysfunction. Nine male patients aged 0.5 to 16 y (seven with cystic fibrosis, two with malabsorption) underwent pancreatic stimulation tests. Their colipase and lipase secretion rates were measured by titrimetric methods and phospholipase A2 and A1 by phosphorus magnetic resonance spectroscopy (31P NMR). It was found that the phospholipases, colipase, and lipase were absent in the two patients with pancreatic insufficiency. In patients with normal absorption, there were marked inter-and intrasubject variations of lipase, colipase, and phospholipase secretion rates that were consistent with the degree of exocrine pancreatic dysfunction. However, in the three 20-min stimulation periods of the pancreatic function test, pancreatic phospholipase is cosecreted with lipase and colipase, and average colipase and phospholipase A2 secretion rates follow a similar or parallel pattern. These findings are consistent with the important role of pancreatic phospholipases in intestinal phospholipid hydrolysis leading to the desorption of phospholipids from the lipid substrate and enhancing lipid hydrolysis and phospholipid absorption.
Similar content being viewed by others
Main
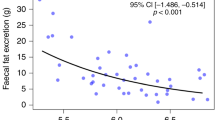
Exocrine pancreatic function has been well characterized in children with pancreatic disease with the use of quantitative pancreatic function tests(1–3). To determine the relationship between residual pancreatic function and fat absorption, sensitive titrimetric assays were developed for lipase and the lipase cofactor colipase(4) and their secretion rates compared with fecal fat excretions in children with CF, Shwachman syndrome, or controls(3, 5). These studies demonstrated that patients with normal fat absorption had a wide range of enzyme/coenzyme secretion from less than 5% up to within the normal control range; and the threshold for lipolytic failure was near 1% of average control colipase values, i.e. patients with values below this level had fat malabsorption and above this level normal absorption. These observations led to the currently accepted definition that patients with malabsorption are PI and those with normal absorption are PS, indicating that they have either insufficient or sufficient endogenous enzyme output, respectively, to prevent malabsorption(6). The results also emphasized the important role of colipase in vivo, as, in a group of patients with seemingly adequate lipase output above the threshold level, fat malabsorption occurred because of inadequate cosecretion of colipase. This confirmed in vitro observations that lipase in the presence of supramicellar concentrations of bile salts is only active if colipase is present and remains inactive in the absence of colipase(4, 7, 8).
The exocrine pancreas also secretes another group of lipolytic enzymes, the phospholipid-hydrolyzing enzymes including PLA1 (EC 3.1.1.32), PLA2 (EC 3.1.1.4), and CEH (EC 3.1.1.1)(9). PLA1 and PLA2 are secreted in their zymogen form and activated by trypsin on entering the duodenum(10). In intraluminal digestion, PLA2 is primarily responsible for hydrolyzing PC to 2-lysoPC. This reaction is important in triglyceride digestion as the amphipathic PC, in a manner similar to bile salts, will adsorb to the surface of the lipid droplets, preventing contact between the lipase-colipase complex and its lipid substrate(11). Hydrolysis of PC by PLA2 will allow desorption of lysoPC, which is water soluble. The subsequent mucosal absorption of lysoPC is important in the generation of enterocyte phospholipids(12) and lipoproteins and, thus, chylomicron formation(13).
The above indicates an important physiologic function for PLA2. However, although PLA2 has been measured in duodenal juice in normal adult volunteers during a Lundh test meal(14), there is no information regarding pancreatic PLA2 secretion rates in children or in patients with exocrine pancreatic disease(15). Previously, by using 31P NMR, we demonstrated that PLA2 can be assayed in incubated duodenal fluid from PS patients by measuring the rate of 2-lysoPC formation from the hydrolysis of PC(16). In the present study, we have modified the assay by using PC in the duodenal fluid of PI patients, which lacks phospholipid-hydrolyzing enzymes as the substrate, and have assessed the secretion rate of PLA2 in both PI and PS patients during pancreatic stimulation tests in relation to lipase and colipase secretion.
METHODS
Materials.
PC and 2-lysoPC were obtained from Sigma Chemical Co. (St. Louis, MO, U.S.A.). D2O (99.75%) was from the Australian Institute of Nuclear Science and Engineering (Lucas Heights, N.S.W., Australia). All other chemicals were analytical grade.
Patients.
Nine male patients aged from 0.5 to 16 y underwent pancreatic stimulation tests: seven were PS and two were PI. Of the PS patients, five had CF (CF-PS), one MCC with persistent hypocalcemia, and one who was investigated for short stature with possible Shwachman syndrome and was ultimately shown to have normal pancreatic function. Both PI patients had CF (CF-PI).
Pancreatic stimulation tests.
Pancreatic stimulation tests were performed as previously described(1–3). Briefly, after an overnight fast (except the children under age 2 y and the MCC patient who fasted for 4 h), a double-lumen catheter was inserted into the duodenum. One lumen for infusion had a single port located proximally near the ampulla of Vater, and the second aspiration lumen had multiple ports at least 5 cm distal to the ampulla and approximately 1 cm apart. A nonabsorbable marker solution [gentamicin 10 μg/mL in 5% mannitol (wt/vol)] was infused at a constant rate of 1.25 mL/min through the proximal port, and the mixture of marker and pancreatic juice was aspirated by low-pressure suction from the distal ports. Aspirates were collected in four 20-min periods, one initial period without stimulation and three periods during which a continuous i.v. infusion of secretin and cholecystokinin was maintained as described previously(1, 6). The use of the marker perfusion solution enabled precise determination of the quantity of marker and, thus, pancreaticobiliary fluid that was not aspirated during the procedure(1, 6). All samples were collected on ice, and the fluid from each interval was aliquotted into smaller samples and stored immediately at −70°C.
Lipase and colipase assays.
Lipase and colipase concentrations were measured, and their rates of secretion were calculated as previously described(3, 4). The titrimetric enzyme assays were carried out at 37°C with glycerol tributyrate as the lipid substrate. Colipase activity was determined in the presence of 4 mM sodium taurodeoxycholate, and lipase activity was determined by using a saturating concentration of porcine colipase. Pancreatic function was defined as sufficient if colipase output was greater than 1% of the mean normal level (120 U·kg−1·h−1) and insufficient if less than 1% of the mean normal level(3).
NMR experiments.
Our previous work in measuring phospholipid concentration in samples of duodenal juice collected during pancreatic stimulation indicated variable concentrations of PC and lysoPC therein(16). To standardize the procedure for measuring PLA2 and PLA1, we used the pooled pancreaticobiliary juices from five CF-PI patients with absent PLA2 and PLA1 activities. Samples from pancreatic stimulation tests of patients with pancreatic sufficiency or insufficiency (1.2 mL) were added to the pooled pancreaticobiliary juice from CF-PI patients (1.3 mL) and transferred to 10-mm NMR tubes. The volume was brought up to 3 mL by adding 0.5 mL D2O with 5 mM EDTA and an internal standard (trimethyl phosphate) to the NMR tube. The samples were then ready for incubation at 37°C and NMR measurements. Unless otherwise stated, all incubations were performed at pH 7.44. Standard samples were prepared by adding a known concentration of lysoPC in D2O to samples of pancreaticobiliary secretions from PI-CF patients.
Quantitative analysis of the concentrations of phospholipids was performed as previously described(17–20).
NMR spectroscopy.
31P NMR spectra were recorded on a Bruker DRX (Avance) 400 spectrometer operating at 161.98 MHz in the Fourier transform mode with the probe temperature controlled to 37 + 1°C. Broadband proton irradiation was applied to eliminate 1H/31P NMR coupling. All measurements were performed on 3-mL samples in 10-mm NMR tubes with D2O as the internal field/frequency lock. Samples were spun at 12 Hz. Rapid pulsing was used to acquire the spectra. Each spectrum was derived by Fourier transformation of 600 summed transients with a spectral accumulation time of approximately 5.5 min, and FID (free induction decay) were processed with 3-Hz line broadening. Other NMR parameters were as follows: transient acquisition time, 0.256 s; data size, 16 k; 50° pulse, duration 10 μs; intertransit delay, 300 ms.
The present study was approved by the Ethics Committee of the Royal Alexandra Hospital for Children, and parents provided written informed consent for pancreatic function studies.
RESULTS
31P NMR of pancreaticobiliary fluid.
The31P NMR spectrum obtained from a sample of biliary-pancreatic secretions from a CF-PS patient is shown in Figure 1A. The resonance at −0.06 ppm was assigned to PC and those at 0.25 and 0.42 ppm to its hydrolytic products, 1-lysoPC and 2-lysoPC, respectively. After incubation of the sample for 39 min at 37°C, there was substantial hydrolysis of PC and, thus, an increase in the two lysoPC peak intensities as shown in Figure 1B. The same experiment in a CF-PI patient is illustrated in Figure 1, C and D , demonstrating the preservation of the PC peak after even prolonged incubation (167 min) and absent lysoPC peaks, both observations indicating the lack of phospholipase activities.
The 31P NMR peak assignments in Figure 1 were confirmed by adding authentic phospholipids to the sample of biliary-pancreatic secretions and observing the corresponding increase in signal amplitude and intensity. The resonance for 1-lysoPC was assigned by subjecting a sample of biliary-pancreatic secretions to phospholipase B activity(16). Chemical shift assignments were referenced relative to external 85% orthophosphoric acid at 0.000 ppm.
PLA2 and PLA1 assays.
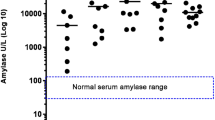
NMR-based phospholipase assays were developed by subjecting the pooled pancreaticobiliary fluid from CF-PI patients (substrate) to phospholipase activities by the addition of pancreaticobiliary fluid from a subject under study (enzyme source). The samples were then incubated at 37°C, and sequential 31P NMR spectra were acquired. It was observed that the 2-lysoPC and 1-lysoPC concentrations progressively increased with the time. Under the assay conditions, the lysoPC was not further hydrolyzed to GPC due to the CEH activity. However, a small amount of GPC was produced after a prolonged incubation and only after complete hydrolysis of the substrate (PC). PLA2 and PLA1 activities were calculated from the initial slopes of 2-lysoPC and 1-lysoPC concentration increase, respectively(16, 17). The total phospholipase secretion was expressed as the activity (mmol·mL−1·h−1) times the total volume of duodenal aspirate during 1 h of stimulation (three 20-min periods) per kilogram of body weight. Table 1 lists the secretion rate of PLA2 and PLA1 together with the secretions of lipase and colipase from patients with pancreatic sufficiency and compares them with samples from those patients who had pancreatic insufficiency. As shown in Table 1, the total secretion of PLA2 and PLA1 per kg/h was remarkably similar between patients in the CF-PS group, despite some variation of their lipase, colipase secretion rates and regardless of the patient's age. Substantially lower levels of PLA2 and PLA1 were seen in the MCC patient, possibly related to hypocalcemia (serum Ca2+ < 2 mmol/L) as calcium is required for PLA2 and PLA1 activity. Both PLA2 and PLA1 activities were absent from the two PI patients.
Parallel secretion of phospholipase, lipase, and colipase.
As shown in Table 1, two age groups of patients with pancreatic sufficiency were studied, three less than and four more than 2 y of age. The three patients less than 2 y of age and the one patient with MCC underwent only a short fast of 4 h before their pancreatic stimulation tests; a more prolonged fast was considered inappropriate for the younger patients or the patient with MCC in view of his hypocalcemia. All other patients were fasted for more than 12 h. Figure 2A presents the mean secretion rates of PLA2 and colipase of patients more than 2 y old (after 12 h fasting) during the three 20-min stimulation periods. As evident from Figure 2A, the secretion of PLA2 and colipase was in parallel. The mean secretions of PLA2 and colipase of patients less than 2 y old (nonfasting) during the stimulation periods are shown in Figure 2B. Although the basal values for PLA2 and colipase secretions were considerably higher than their stimulated ones, their stimulated mean values were in parallel.
Mean ± SD basal and stimulated values for PLA2 and colipase secretion (see Table 1 for comments on the secretion units) in PS patients more than 2 y old after 12 h fasting (A) and in PS patients less than 2 y old after 4 h fasting (B).
DISCUSSION
Our results demonstrate that CF-PI patients had no phospholipid-hydrolyzing enzymes including PLA2 and PLA1 activities in their duodenal juice even after prolonged incubation time (Fig. 1, C and D ), consistent with their degree of exocrine pancreatic dysfunction as evident from their absent lipase and colipase secretion. In contrast, PS patients demonstrated substantial PLA1 and PLA2 activities by incubation of samples for 39 min as in Figure 1, A and B , as well as lipase and colipase secretions as listed in Table 1. In a previous study, normal values of colipase secretion among a group of normal young adult controls were more than 6500 U·kg-1·h−1, with an average value of 12,740 U·kg−1·h−1(3). The values in the current study were consistent with values obtained previously in PS patients(2–4), noting that the one normal subject with a value of 5100 U·kg−1·h−1 was younger than previous normal controls. The patient with MCC had a lower output of colipase activity but comparable to one of the CF-PS patients (Table 1). He also had persistent hypocalcemia, a factor that may have impaired colipase activity in the titrimetric assay that was performed. The PLA1 and PLA2 values were consistent in the PS patients except for the lower value in the patient with MCC; again, an observation that could be accounted for by hypocalcemia, as PLA1 and PLA2 activity is calcium dependent. Both PLA1 and PLA2 did not appear to vary with age, with some of the younger CF-PS patients who were less than 12 mo old having secretion levels comparable to older children or adolescents and higher than the one normal patient in the study.
In the two age groups, depending on the duration of fasting, the pattern of PLA2 secretion was very similar to colipase secretion (cf. Fig. 2, A and B ), thus indicating the occurrence of parallel secretion of PLA2 and colipase, a known marker of pancreatic lipolysis. The cosecretion of PLA2 with other pancreatic enzymes or coenzymes could have been predicted from other studies demonstrating parallel pancreatic cosecretion of lipase and colipase(3) and also of nonlipolytic enzymes, proteases, and amylase(21, 22). This observation is also consistent with the role of phospholipases in intraluminal phospholipid and triglyceride digestion and the subsequent role of phospholipids in enterocyte lipid transport. In the small intestine, amphipathic biliary and dietary phospholipids, mainly PC, are adsorbed to ingested triglyceride and can impair the action of the pancreatic lipase-colipase complex during triglyceride digestion(11). PLA2, by hydrolyzing PC, results in desorption of phospholipids from the triglyceride substrate and, thus, facilitates normal lipolysis. The major product of PC digestion, lysoPC, is water soluble and readily absorbed by enterocytes. It is a major source of enterocyte phospholipids for the generation of lipoproteins, and chylomicron formation as shown in the multidrug resistant P-glycoprotein knockout mice(23), for transport of triglyceride from the cell to lymph and for replenishment of membrane phospholipids used in exocytosis(12, 13, 24, 25). Lack of cosecretion of PLA2 could substantially impair these processes. Unhydrolyzed phospholipids substantially impair absorption of fatty acids and cholesterol(26) and interfere with bile salt binding to the bile salt receptors in the terminal ileum, impairing its absorption and increasing fecal bile salt losses(27). The cosecretion of pancreatic phospholipase with other components of the lipolytic system is, thus, rational from a physiologic point of view, noting that whereas its major role is hydrolyzing phospholipids in the intestine, by so doing it is an adjunctive enzyme to triglyceride hydrolysis.
The variation in the pattern of PLA2 and colipase secretion dependent on the duration of fasting was not investigated further in the current study. The high basal levels before pancreatic stimulation of those with a short duration of fasting (Fig. 2B) could reflect prior release at the time of formula or liquid meals and, thus, lack of stimulation at the time of i.v. stimulation of the pancreas. This could be explained by the considerable variation in gastric emptying times between individual children and the recognized slow intestinal transit times described in CF-PS patients(28). Consequently, pancreatic stimulation could be delayed after a test meal, thus accounting for the late or persistent appearance of the lipolytic enzymes. This phenomenon requires further investigation.
In the present study, we did not assess the pancreatic secretion of other phospholipid-hydrolyzing enzymes including the CEH responsible for intraluminal hydrolysis of lysoPC(9). This enzyme is of interest as it appears identical to the bile salt-stimulated lipase in human milk(29). The presence of this enzyme in the intestine from either the pancreas or human milk indicates that a certain proportion of lysoPC remains unabsorbed in both normal breast-fed infants and older children/adults. The physiologic reason for this incomplete absorption of lysoPC remains unclear, but, of interest, lysoPC has a known toxic effect on epithelial cells(30). Although in normal subjects the lysoPC could be hydrolyzed in the presence of CEH, the low activity of CEH in oral enzyme therapy given to PI subjects(31) could allow toxic levels of lysoPC to accumulate in the intestinal lumen and account for some of the intestinal disease seen in CF subjects. Further work is required to assess the pancreatic secretion and activity of CEH in CF and other patients with exocrine pancreatic dysfunction.
The NMR assay method for determining pancreatic PLA2 and PLA1 secretion in this study represented an extension of a method that was introduced in our previous work(16). In the previous study, phospholipase activities were measured using the pancreaticobiliary fluid as both substrate and enzyme source, whereas, in the present study, the source of the PC substrate was the pooled pancreaticobiliary juice from CF-PI patients. Use of the pooled human fluid in this study had the advantage of 1) satisfying all the necessary physiologic requirements for phospholipase activity including appropriate bile salt concentrations and 2) introducing additional PC to phospholipase exposure, thus avoiding product inhibition. We had also previously observed in PS subjects that PLA2 activity was remarkably fast and that a considerable amount of the endogenous PC had already been hydrolyzed to lysoPC during the sample collection. The current assay system with the additional PC, thus, also circumvented this problem.
A variety of methods have been used for the determination of PLA2 and PLA1 activities including titrimetric, radiochemical, immunologic, and HPLC(32–37). These methods in general are multistep, tedious, and time consuming. The classic titrimetric methods are insensitive(32), nonspecific, and require individual phospholipase purification(32, 33). Radiochemical procedures are sensitive but suffer from the disadvantages of being discontinuous and involve radioactive handling that is undesirable(32). Immunologic procedures are also sensitive but can only be used for the determination of the quantities of lipolytic enzymes. Other methods including HPLC usually involve sample extraction using organic solvent mixture. Selective loss of lysoPC, the product of PLA2 and PLA1 activities, is one of the great disadvantages of widely used extraction procedures(20, 30, 38). The NMR assay method for measuring PLA2 and PLA1 used in this study, on the other hand, is convenient, one-step, and nondestructive and does not require extraction of phospholipids. It is, therefore, possible to monitor both PLA2 and PLA1 activities simultaneously in a complex mixture of body fluids such as duodenal juice(16).
In conclusion, we have developed a sensitive and noninvasive assay method for measuring phospholipase activity by using NMR spectroscopy. During pancreatic stimulation tests, CF-PI patients had absent PLA2 and PLA1 activities. In contrast, those with pancreatic sufficiency had pancreatic lipase/colipase secretions up to and within the normal range, with parallel phospholipase secretions.
Abbreviations
- CEH:
-
carboxyl ester hydrolase
- CF:
-
cystic fibrosis
- GPC:
-
glycerophosphocholine
- lysoPC:
-
lysophosphatidylcholine
- MCC:
-
mucocutaneous candidiasis and polyendocrinopathy
- NMR:
-
nuclear magnetic resonance
- PC:
-
phosphatidylcholine
- PLA1:
-
phospholipase A1
- PLA2:
-
phospholipase A2
- PI:
-
pancreatic insufficient
- PS:
-
pancreatic sufficient
References
Gaskin KJ, Durie PR, Corey M, Wei P, Forstner GG 1982 Evidence for a primary defect of pancreatic HCO3− secretion in cystic fibrosis. Pediatr Res 16: 554–557.
Kopelman H, Durie P, Gaskin K, Weizman Z, Forstner GG 1985 Pancreatic fluid secretion and protein hyperconcentration in cystic fibrosis. N Engl J Med 312: 329–334.
Gaskin KJ, Durie PR, Lee L, Forstner GG 1984 Colipase and lipase secretion in childhood-onset pancreatic insufficiency: delineation of patients with steatorrhea secondary to relative colipase deficiency. Gastroenterology 86: 1–7.
Gaskin KJ, Durie PR, Hill RE, Lee L, Forstner GG 1982 Colipase and maximally activated pancreatic lipase in normal subjects and patients with steatorrhea. J Clin Invest 69: 427–434.
Hill RE, Durie PR, Gaskin KJ, Davidson GP, Forstner GG 1982 Steatorrhea and pancreatic insufficiency in Shwachman syndrome. Gastroenterology 83: 22–27.
Forstner G, Durie PR 1991 Cystic fibrosis. In: Walker A, Durie P, Hamilton JR, Walker-Smith J, Watkins J(eds) Pediatric Gastrointestinal Disease. BC Decker Inc, Toronto, 1179–1197.
Morgan R, Barrowman J, Borgstrom B 1969 The effect of sodium taurodeoxycholate and pH on the gel filtration behaviour of rat pancreatic protein and lipase. Biochim Biophys Acta 175: 65–75.
Morgan R, Hoffman N 1971 The interaction of lipase, lipase cofactor, and bile salts in triglyceride hydrolysis. Biochim Biophys Acta 248: 143–148.
Duan RD, Borgstrom B 1993 Is there a specific lysophospholipase in human pancreatic juice?. Biochim Biophys Acta 1167: 326
Roy CC, Weber AM, Lepage G, Smith L, Levy E 1988 Digestive and absorptive phase anomalies associated with the exocrine pancreatic insufficiency of cystic fibrosis. J Pediatr Gastro Nutr 7: 51–57.
Borgstrom B 1980 Importance of phospholipids, pancreatic phospholipase A2, and fatty acids for the digestion of dietary fat:in vitro experiments with the porcine enzymes. Gastroenterology 78: 954–962.
Nilsson A 1968 Intestinal absorption of lecithin and lysolecithin by lymph fistula rats. Biochim Biophys Acta 137: 240–254.
Clark SB 1978 Chylomicron composition during duodenal triglyceride and lecithin infusion. Am J Physiol 235: E183
Sternby B, Nilsson A, Melin T, Borgstrom B 1991 Pancreatic lipolytic enzymes in human duodenal contents. Scand J Gastroenterol 26: 859–866.
Weber AM, Roy CC 1984 Intraduodenal events in cystic fibrosis. J Pediatr Gastroenterol Nutr 3: S113
Nouri-Sorkhabi MH, Gruca MA, Kuchel PW, Gaskin KJ 1999 Phospholipid changes in children with pancreatic sufficiency and insufficiency. Clin Chim Acta 281: 89–100.
Nouri-Sorkhabi MH, Sullivan DR, Benton CM, Kuchel PW 1996 Changes in plasma phospholipids in the presence and absence of erythrocytes: 31P NMR time-course studies. Eur J Biochem 235: 648–652.
Nouri-Sorkhabi MH, Agar NS, Sullivan DR, Kuchel PW 1996 Phospholipid composition of erythrocyte membranes and plasma of mammalian blood including Australian marsupials; 31P NMR analysis using detergents. Comp Biochem Physiol B 113: 221–227.
Wright LC, Nouri-Sorkhabi MH, May GL, Danckwerts LS, Kuchel PW, Sorrell TC 1997 Changes in cellular and plasma membrane phospholipid composition after lipopolysaccharide stimulation of human neutrophils, studied by 31P NMR. Eur J Biochem 243: 328–335.
Nouri-Sorkhabi MH, Wright L, Sullivan DR, Kuchel PW 1996 Quantitative 31P NMR analysis of phospholipid composition of erythrocyte membranes using detergent. Lipids 31: 765–770.
Scheele GA, Palade GE 1975 Studies of the guinea pig pancreas: parallel discharge of exocrine enzyme activities. J Biol Chem 250: 2660–2670.
Steer ML, Glezer G 1976 Parallel secretion of digestive enzymes by the in vitro rabbit pancreas. Am J Physiol 231: 1860–1865.
Voshol PJ, Minich DM, Havinga R, Oude Elferink RPJ, Verkade HJ, Groen AK, Kuipers F 2000 Postprandial chylomicron formation and fat absorption in multidrug resistance gene 2 P-glycoprotein-deficient mice. Gastroenterology 118: 173–182.
O'Doherty PJA, Kakis G, Kuksis A 1973 Role of luminal lecithin in intestinal fat absorption. Lipids 8: 249–255.
Tso P, Lam J, Simmonds WJ 1978 The importance of lysophosphatidylcholine and choline moiety of bile phosphatidylcholine in lymphatic transport of fat. Biochim Biophys Acta 528: 364–372.
Saunders DR, Sillery J 1976 Lecithin inhibits fatty acid and bile salt absorption from rat small intestine in vivo. Lipids 11: 830–832.
O'Connor PJ, Loiudice TA, Bochenek W, Bodgers JB 1987 Effect of diester and diether phosphatidylcholine on intestinal absorption of neutral and acidic sterols. Am J Dig Dis 23: 316–320.
Mack DR, Flick JA, Durie PR, Rosenstein BJ, Ellis LE, Perman JA 1992 Correlation of intestinal lactulose permeability with exocrine pancreatic dysfunction. J Pediatr 120: 696–701.
Hansson L, Blackberg L, Edlund M, Lundberg L, Stromqvist M, Hernell O 1993 Recombinant human milk bile salt-stimulated lipase. J Biol Chem 268: 26692–26698.
Shimada K, Yanagisawa J, Nakayama F 1991 Increased lysophosphatidylcholine and pancreatic enzyme content in bile of patients with anomalous pancreaticobiliary ductal junction. Hepatology 13: 438–444.
Sternby B, Nilsson A 1997 Carboxyl ester lipase (bile salt-stimulated lipase), colipase, lipase, and phospholipase A2 levels in pancreatic enzyme supplements. Scand J Gastroenterol 32: 261–267.
Farooqui AA, Horrocks LA 1988 Determination of phospholipases, lipases, and lysophospholipases. In: Boulton AA, Baker GB, Horrocks LA(eds) Lipids and Related Compounds. The Humana Press, Inc, Clifton, NJ, 179–209.
De Haas GH, Postema NM, Nieuwenhuizen W, van Deenen LM 1967 Purification and properties of phospholipase A from porcine pancreas. Biochim Biophys Acta 159: 103–117.
Nishijima J, Okamoto M, Ogawa M, Kosaki G, Yamano T 1983 Purification and characterization of human pancreatic phospholipase A2 and development of a radioimmunoassay. J Biochem 94: 137–147.
Eskola JU, Nevalainen TJ, Lovgren NE 1983 Time-resolved fluoroimmunoassay of human pancreatic phospholipase A2 . Clin Chem 29: 1777–1780.
Schulz R, Strynadka KD, Panas DL, Olley PM, Lopaschul GD 1993 Analysis of myocardial plasmalogen and diacyl phospholipids and their arachidonic acid content using high-performance liquid chromatography. Anal Biochem 213: 140–146.
Waite M 1991 Phospholipases. In: Vance DE, Vance J(eds) Biochemistry of Lipids, Lipoproteins, and Membranes. Elsevier Science Publishers BV, Amsterdam, 269–295.
Bjerve KS, Daae LNW, Bremer J 1974 The selective loss of lysophospholipids in some commonly used lipid-extraction procedures. Anal Biochem 58: 238–245.
Acknowledgements
The authors thank Dr. W.A. Bubb and W.G. Lowe for their assistance with NMR spectroscopy and laboratory techniques, respectively. The authors also thank C. Frazer for assistance in the preparation of the manuscript.
Author information
Authors and Affiliations
Additional information
Supported by a grant from The University of Sydney, Australian Cystic Fibrosis Research Trust, and James Fairfax Institute (M.H.N-S., K.J.G.) and a grant from the Australian Research Council (P.W.K., B.E.C.).
Rights and permissions
About this article
Cite this article
Nouri-Sorkhabi, M., Chapman, B., Kuchel, P. et al. Parallel Secretion of Pancreatic Phospholipase A2, Phospholipase A1, Lipase, and Colipase in Children with Exocrine Pancreatic Dysfunction. Pediatr Res 48, 735–740 (2000). https://doi.org/10.1203/00006450-200012000-00006
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200012000-00006
This article is cited by
-
Mechanisms of lipid malabsorption in Cystic Fibrosis: the impact of essential fatty acids deficiency
Nutrition & Metabolism (2005)