Abstract
Vitamin A (retinol) and its active derivatives (retinoic acids) are essential for growth and development of the mammalian fetus. Maternally derived retinol must pass the placenta to reach the developing fetus. Despite its apparent importance, little is known concerning placental transfer and metabolism of retinol, and particularly of placental production and storage of retinyl esters. To elucidate this metabolic pathway, we incubated, in the presence of retinol, 1) human full-term placental explants and 2) primary cultures of major cells types contributing to placental function: trophoblasts and villous mesenchymal fibroblasts. We used HPLC to determine the types and concentrations of retinyl esters produced by these explants and cells. About 14% of total cellular retinol in placental explants was esterified. The most abundant esters were myristate and palmitate. Primary cell cultures showed that fibroblasts efficiently produced retinyl esters, but trophoblasts did not. In both types of experiments, no retinyl esters were detected in the culture medium, suggesting that retinyl esters were produced for storage purpose. These results suggest that villous mesenchymal fibroblasts are primary sites of retinol esterification and storage in the placenta.
Similar content being viewed by others
Main
In addition to their essential roles in vision, growth, and maintenance of differentiated epithelia, vitamin A (retinol) and its active derivatives, the RAs, are required for normal mammalian reproduction and fetal development (1, 2). Maternal vitamin A deficiency can result in fetal death or in a spectrum of malformations, the fetal vitamin A deficiency syndrome (3–6). Excessive vitamin A intake can also produce a spectrum of congenital defects, in a dose- and developmental stage–dependent manner (7, 8). Because there is no de novo fetal synthesis of retinol, the developing mammalian embryo is dependent on the maternal circulation for its vitamin A intake. The presence of measurable hepatic vitamin A stored at birth is indicative of the functionality and importance of placental transport during pregnancy (9, 10). Abnormalities of placental transfer could have serious consequences on fetal development and integrity.
Despite its apparent importance, little is known about placental transfer and metabolism of retinoids. This question has been approached in animal models (sheep, mouse, monkey), but the placental metabolism of retinoids is difficult to deduce from studies in the intact animal, and extrapolation of these results to humans is uncertain (11–13). Measurements of human placental, maternal, and cord retinoid concentrations have been reported, but they shed little light on the metabolic pathway (14, 15). Experiments using human perfused placenta and full-term human placental tissues in vitro have yielded controversial results concerning retinoid metabolism, especially the ability of the placenta to produce and store retinyl esters from retinol (16, 17).
To better characterize retinoid metabolism, we have investigated placental capacity to esterify retinol into retinyl esters of full-term placental explants. Primary cultures of the major types of cells contributing to the placenta (trophoblasts and mesenchymal fibroblasts) were tested to determine their individual capacity for esterification.
METHODS
Chemicals.
All-trans retinol, trypsin, DNase,collagenase H, and human purified RBP were purchased from SigmaChemical Co.-Aldrich (L'isle d'Abeau, Chesnes, France). HBSS,DMEM, RPMI 1640, glutamine, penicillin/streptomycin, and FCS werepurchased from Life Technologies (Cergy, France). For all experiments,retinol was prepared as 1000× stock solution in ethanol. Themaximal ethanol concentration to which the cells and tissues wereexposed was 0.1%. Retinol-RBP complex was prepared and purified aspreviously described (18).
Placentas.
Nine placentas from normal pregnancies were collected in the Department of Obstetrics and Gynecology at the Maternity of Hôtel-Dieu Hospital (Clermont-Ferrand, France). All the mothers gave their written informed consent before participation in accordance with the ethical principles expressed in the Declaration of Helsinki regarding human experimentation. The local Institutional Review Board has approved all the human studies. Term placentas of clinically normal pregnancies were obtained after delivery by cesarean section (placentas from vaginal deliveries were excluded to reduce risks of potential infections and tissue degradation). They were immediately collected and used within 15 to 30 min. Characteristics of the pregnant women and their babies are presented in Table 1. All the babies were healthy, and their morphometry scores were in the standard range for French babies (19). Growth, development, and postpartum changes were normal for all mothers and babies based on a medical examination that occurred in the 7 d after delivery.
Explant tissue incubation.
Placental tissue (chorionic villus) was minced (1 to 2 mm3) and washed three times in sterile cold HBSS before incubation. Explants were immersed in Falcon flasks containing 50 mL of DMEM supplemented with 20 mM glutamine, 10 U/mL penicillin, 100 μg/mL streptomycin, and 10% FCS (16). Retinol (free or bound to RBP) was added at a final concentration of 2 μM. When retinol was added free and diluted in ethanol, the maximal ethanol concentration to which the explants were exposed was <0.1%. As a negative control, explants were incubated only with vehicle (ethanol). Incubations were performed at 37°C in a humidified incubator with 5% CO2/95% air at 37°C. Incubations were terminated by washing the placental explants twice with cold PBS. All tissue samples were blotted dry and stored under nitrogen at −70°C until further processing.
Primary placental fibroblast purification and incubation.
Villous fibroblasts from placental mesenchyme were obtained using the modified method of Schwab et al. (20). Briefly, chorionic villi were washed with sterile cold HBSS. The tissue was coarsely minced and digested in 2 mL of 0.25% trypsin in HBSS without calcium and magnesium for 45 min at 37°C. The first digest product was transferred and incubated for 1 h at 37°C in a second medium (0.1% trypsin and 0.1% collagenase H in HBSS without calcium and magnesium). This digest was centrifuged at 4000 rpm, and the supernatant was discarded. The pellet was resuspended in 6 mL of RPMI 1640 containing 20 mM glutamine, 10 U/mL penicillin, 100 μg/mL streptomycin, and 10% FCS. Purity of isolated fibroblasts was examined by morphologic and immunologic (cytoplasmic vimentin-positive immunoreactivity) characteristics (21, 22). Fibroblasts at 50 to 60% confluence were incubated with 2 μM retinol (free or bound to RBP). When retinol was added free and diluted in ethanol, the maximal ethanol concentration to which the fibroblasts were exposed was <0.1%. As a negative control, fibroblasts were incubated with vehicle (ethanol). Primary purified cutaneous (skin) and MRC5 (pulmonary embryonic fibroblast cell line) fibroblasts were also cultured and incubated in RPMI 1640 as above. All the cultures and incubations were performed in a humidified incubator with 5% CO2/95% air at 37°C.
Purification, differentiation, and incubation of primarycytotrophoblasts.
Cytotrophoblasts were obtained by using the modified method of Kliman et al. (23). Villous tissue was dissected free of membranes and vessels. They were minced in cold sterile HBSS and subjected to repeated trypsin-DNase digestions as described (23). The resulting cell suspension was carefully layered over a discontinuous Percoll gradient (5 to 70%) and centrifuged (20 min, 1500 rpm). The homogeneous population of mononuclear cells, contained in the middle layer (density 1.048–1.062 g/L) consisted of >95% cytotrophoblast cells. For primary culture, the cells were plated in 90-mm Petri culture dishes (5 × 106 cells per dish) with DMEM supplemented with 20 mM glutamine, 10 U/mL penicillin, 100 μg/mL streptomycin, and 10% FCS. Cultures and retinol incubations were always performed in humidified 5% CO2/95% air incubator at 37°C (as described for fibroblasts). Purity of primary cytotrophoblasts was verified by morphologic and immunologic characteristics [cytokeratin- and human placental lactogen–positive immunoreactivity (23–25)]. Differentiation of cytotrophoblasts into syncytiotrophoblasts was monitored by measuring chorionic gonadotrophic hormone in the culture medium by immunochemiluminescent assay (ACS 180, Ciba Corning). Retinol and ethanol incubations were performed as described above.
Chromatographic analysis.
Tissues and cells were harvested in cold PBS. The cells were collected by scraping, resuspended in PBS, and sonicated on ice. All-trans retinol and retinyl esters were assayed from 1g of placental tissue, 5 × 106 cells, or 0.5 mL of culture medium, as previously described with some minor modifications (26, 27). An equal volume of ethanol containing an internal standard (retinyl laurate for vitamin A) was added to each sample. They were then extracted twice with 2 volumes of hexane. After evaporation to dryness, the extract was dissolved in 250 μL of a mixture of dichloromethane–methanol (35:65; vol/vol). The compounds were analyzed by reverse-phase HPLC on a Waters apparatus equipped with a 600 pump, a 710 automatic injector, a 996 diode array detector and controlled by Millenium software 2.1. For retinol and retinyl ester determinations, the samples were eluted on a C18 column (Nucleosil, 250 × 4.6 mm) with pure methanol as the mobile phase (2 mL/min); the detection was performed at 325 nm and 292 nm. Identification was based on co-elution with authentic standards and UV spectrum comparisons. Quantification involved internal standardization and dose-response curves established with authentic standards.
DNA and protein concentration determinations.
In all the studies, retinoid concentration assays were normalized to DNA or protein concentrations. DNA concentration was measured by a spectrofluorometric method described previously by Labarca and Paigen (28). Protein concentrations of the cellular homogenates were determined using the Biuret method on the Hitachi 911 from Boehringer Mannheim Diagnostics (29). Similar results were obtained when retinoid concentrations were normalized to DNA content or protein concentration; we chose to express our results normalized to DNA content for all the cell culture experiments.
Statistical analysis.
All experiments were repeated on nine placental explants or primary cell cultures. Mean values and SD were calculated for all retinoid variables. Statistical comparisons were performed using ANOVA and Fisher's exact test. Statistical procedures were performed with the StatView program (Abacus Concepts, Inc., Berkeley, CA, U.S.A.). For all the studies, statistical significance was considered at p < 0.05.
RESULTS
Retinyl ester production in placental explants.
As vitamin A is usually esterified within tissues, the production of vitamin A esters in full-term placental explants was investigated. To explore retinyl ester production, retinol was added directly to the medium or bound to its blood carrier protein, RBP. During all the tissue or cell incubations, we checked the stability of the in vitro-generated RBP-retinol complex and the absence of nonspecific release of retinol from this complex (data not shown). Table 2 shows the concentrations of retinol and retinyl fatty acyl esters in placental extracts obtained 6 and 24 h after incubation with retinol (free or bound to RBP). We found that maximal esterification of free retinol was already achieved after 6 h of incubation (14.3% of the total cellular retinol esterified). In contrast, a quantitative increase of cellular retinyl esters was observed between 6 (10.2%) and 24 h (14.9%) of incubation with retinol bound to RBP. However, at the end of incubation (24 h), no statistical difference could be observed between the percentage of retinyl esters produced by retinol free of and bound to RBP. The values obtained in these experiments are comparable to those obtained in previous studies (30).
HPLC was able to distinguish between retinyl myristate, palmitate, and stearate concentrations (26, 27). Only retinyl myristate was present at significant levels before retinol incubation (Table 2). After retinol incubation bound or unbound to RBP, the most abundant esters, in decreasing order of abundance, were myristate, palmitate, and stearate. Retinyl esters were not detected in the culture medium, suggesting an absence of release of retinyl esters formed in situ. To elucidate which cells are involved in placental esterification of retinol, we studied this biochemical reaction in primary cultures of the different cell types constitutive of the human placenta.
Esterification of retinol by primary placental fibroblasts inculture.
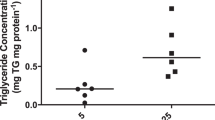
Figure 1 shows the intracellular concentrations of retinol and retinyl fatty acyl esters in primary fibroblast cultures collected from 3 to 24 h after incubation with retinol (free or bound to RBP), or with ethanol as a control. As presented in Figure 1A, free retinol added to the culture medium is rapidly taken up by fibroblasts, and little change in cellular retinol content is observed after 3 h. The uptake of retinol bound to RBP occurs more slowly (but linearly) than when retinol was added directly to the culture medium of mesenchymal fibroblasts. The time course of retinol esterification is presented in Figure 1B. As previously described for human skin fibroblasts (31, 32), primary human placental fibroblasts are able to esterify retinol. Conversion of free retinol into retinyl esters is rapid: at the earliest sampling time (3 h), significant production of retinyl palmitate was observed. The accumulated amount of retinyl esters increased steadily to reach a maximum of about 10.8% of total cellular retinol at 24 h of incubation time with free retinol. Retinyl palmitate was always the major ester produced for all times of incubation with free retinol (Fig. 1B). No significant ester production was detected with ethanol incubation (Fig. 1B). Retinol delivered via RBP was also converted to retinyl esters; but more slowly than after incubation with free retinol: no significant increase of retinyl esters (2.1%) was detected at 3 h in contrast to 3 h of free retinol incubation (3.7%). At the end of incubation (24 h), the percentage of retinol converted into retinyl esters (10,8%) was the same whether the retinol was added directly to the medium or bound to RBP. In conclusion, although amounts of retinol taken up and converted into retinyl esters by fibroblasts are different depending on whether it is delivered free or bound to RBP, we could not find any differences in the relative percentage and profile of retinyl esters formed. Experiments using primary cutaneous and MRC5 (pulmonary embryonic fibroblast cell line) fibroblasts gave similar results for the rate of free retinol esterification (Table 3). This suggests that the ability of placental fibroblasts to esterify retinol is not tissue-specific but rather reflects an intrinsic and ubiquitous property of human fibroblasts.
Intracellular concentrations of retinol (Rol;A) and retinyl esters (B) in placental fibroblasts after retinol incubation. Primary placental fibroblasts were treated with 2 μmol/L retinol (added directly to the culture medium or bound to RBP) during different times of incubation (3 to 24 h). The intracellular retinol concentrations (A) and retinyl ester concentrations (B) correspond to the means and SD values obtained from nine different culture experiments. Error bars represent the SD of the nine experiments. Where error bars are not visible, they were smaller than the diameter of the symbol. For each incubation time, an asterisk denotes statistical differences between intracellular retinol, retinyl palmitate, or retinyl myristate values obtained from free retinol and retinol bound to RBP incubation (tested by Fisher's exact test;p < 0.05).
Absence of esterification by primary cytotrophoblasts andsyncytiotrophoblasts in culture.
It is well established that cytotrophoblasts and syncytiotrophoblasts are the cells involved in the transfer of a large number of nutrients from the mother to the fetus and their metabolism. Therefore, we studied the ability of these cells to esterify retinol free and bound to RBP. In all the experiments, the initial cellular material was found to contain retinyl myristate. As presented in Figure 2A, the uptake of retinol bound to RBP occurs more slowly than when retinol was added directly to the culture medium of trophoblastic cells. Note that decrease of intracellular retinol levels between 6 and 24 h was found in both types of retinol incubation. Figure 2B shows that retinol incubation did not lead to a significant retinyl myristate production, but was associated with a weak (but significant) esterification of retinol into retinyl palmitate by trophoblasts. Stearate was never detected at any step of the incubation. We could not find any differences in the relative percentage and profile of retinyl esters formed between incubation with retinol free or bound to RBP (Fig. 2B). Cytotrophoblasts are known to differentiate into syncytiotrophoblasts during normal culture (19). We performed 24-h retinol incubation after various times of trophoblastic cell culture (24, 48, and 72 h), which correspond respectively to the cytotrophoblast, intermediary, and syncytiotrophoblast stages. Similar retinoid profiles were obtained at all these steps (data not shown).
Intracellular concentrations of retinol (Rol;A) and retinyl esters (B) in trophoblastic cells after retinol incubation. Primary trophoblastic cells were treated with a final 2 μmol/L retinol (diluted in ethanol or bound to RBP), during different times of incubation (3 to 24 h). Means of intracellular retinol concentrations (A) and retinyl ester concentrations (B) obtained from nine different culture experiments were presented with their SD. Error bars represent the SD of the nine experiments. Where error bars are not visible, they were smaller than the diameter of the symbol. For each incubation time, an asterisk denotes statistical differences between intracellular retinol, retinyl palmitate, or retinyl myristate values obtained from free retinol and retinol bound to RBP incubation (tested by Fisher's exact test;p < 0.05).
The total retinyl esters found after 24 h of retinol incubation in placental fibroblasts and trophoblastic cells is 51.8 and 8.7 μmol/μg of DNA, respectively. A 14.6-fold and 1.4-fold (not significant) increase in total retinyl esters during 24 h of retinol incubation was found in fibroblasts and trophoblasts, respectively, implying that the placental cells responsible for retinol esterification are fibroblasts.
DISCUSSION
Vitamin A and its active derivatives, the retinoids, are fundamental for development of the mammalian fetus (2, 6, 10). The placenta plays a crucial role in regulation of transport and metabolism of maternal nutrients transferred to the fetus. Abnormalities in these placental functions can have deleterious consequences on fetal development (8, 33). Little is known about human placental retinol transfer and metabolism. Creech-Kraft et al. (34) demonstrated that even 96 h after administration of 13-cis RA, all-trans RA and 4-oxo metabolites are still found in the early human placenta. More recently, co-oxidation of all-trans retinyl acetate by lipoxygenase has been demonstrated in the human placenta (35). All these results indicate that the human placenta has the ability to isomerize and oxidize retinoids.
Our study demonstrates that human placental tissues at term and, more precisely, the villous mesenchymal fibroblasts, are able to esterify retinol. Human primary cutaneous fibroblasts are known to have this ability and to express the intracellular proteins (cellular RBP-1) and the necessary metabolic enzymes (32, 36) that allow this function. A recent study demonstrated the presence of cellular RBP-1 in villous mesenchymal cells of the human placenta (37). Added to our results, this implies that maternal retinol could be trapped by the mesenchymal fibroblasts and esterified in situ. Note that our preliminary results suggest the presence of one or both retinol esterifying enzymes, the lecithin retinol acyl transferase in these placental cells.
However, cytotrophoblasts or syncytiotrophoblasts express the putative placental RBP receptor (37) and are unable to esterify retinol in a significant manner. This study suggests that these trophoblastic cells are more involved in the transfer of retinol between mother and fetus, rather than in its metabolism. The retinyl esters that we detected after cytotrophoblast purification are probably related to the capture of maternal chylomicrons charged with newly digested retinyl esters (38). It has been established that trophoblastic cells express the receptors for LDL and VLDL lipoproteins (39, 40) and are able to take up and use lipoproteins (41). Furthermore, considering the life span (96 h) and the perpetual regeneration of the trophoblasts, stocks of retinyl esters have to be located in villous mesenchymal cells (fibroblasts) to be protected from a rapid and nonspecific hydrolysis and liberation.
We report here that the rate of esterification of retinol by mesenchymal fibroblasts and the types of retinyl esters synthesized are the same whether retinol is delivered free or bound to RBP. This agrees with other previous results observed for rat liver parenchymal cells (42) or human foreskin keratinocytes (43), suggesting an absence of cell surface RBP receptors on mesenchymal fibroblasts. Recently, an immunohistologic study showed that staining for the RBP receptor protein was only observed in the apical part of the villous syncytiotrophoblast and in the placental macrophages (Hofbauer cells) (37). Because of the closed cellular contact between trophoblasts and fibroblasts in term placental villi, we propose that maternal retinol complexed with RBP could be captured by trophoblasts, then freely transferred to fibroblasts.
A discrepancy is observed between the esterification profiles obtained on tissue and cell culture experiments. In explants, retinyl myristate is the major ester formed, whereas in fibroblast cultures, an equilibrium between retinyl myristate and palmitate occurs. It has already been well demonstrated that vitamin A metabolism (especially retinyl ester production, storage, and hydrolysis) may be affected by the characteristics of the surrounding extracellular matrix, by soluble cytokine mediators (44), and by growth factors (epidermal growth factor) specific to placental tissue. In the primary isolated cell cultures, absence of such a complex placental environment could contribute to the differences observed in the profile and rate of retinyl ester production.
What is the function of retinyl esters in placenta? The fact that these compounds were never detected in our experimental conditions (i.e. without stimulus) in the culture medium suggests that retinyl esters are produced for storage. In agreement with this observation, retinyl esters also were never detected in human umbilical blood at delivery (15). It is well accepted that the placenta could be considered as a transitory, primitive functional liver during the first stages of development. During this period, the placenta stores retinol, waiting for liver maturity and functionality marked by the capacity to secrete RBP. In our study, the capacity of the human placenta at term to esterify retinol could be residual activity otherwise strongly present during early embryonic and fetal development.
This hypothesis is supported by results concerning the switch in retinoid content of embryonic and placental compartments during the development of the mouse conceptus (9). During early organogenesis, the retinyl ester content of the placenta is nearly 8-fold higher than the content of the embryo, whereas at the end of gestation, the retinyl ester content of embryo is nearly 4-fold greater than that of the placenta. The timing of this crossover correlates with the apparent onset of retinol storage by the embryonic liver.
According to its capacity to rapidly store retinyl esters, the placenta could be considered as an efficient buffer to control retinol delivery between mother and fetus by 1) releasing retinol to the fetus when maternal intake is deficient, and 2) protecting the embryo from a potential excess of maternal retinol. Even if maternal retinoid concentrations were abnormally fluctuant, the placenta could prevent strong variability in quantity and quality of retinoids delivered to the fetus. By this mechanism, the placenta could play a preventive role against retinoid teratogenicity. This role is probably limited to physiologic retinol variations, and overwhelmed by medical or dietary maternal ingestion of retinoids responsible for fetal teratogenicity resulting from hypervitaminosis A. In addition, placental retinyl stores could be considered as a local reserve for placental use. Transformation of retinyl esters into active retinol derivatives (RAs) could be a simple way to regulate in situ cellular proliferation and differentiation. But to our knowledge, this retinoid metabolism has only been described in mouse and porcine placenta (45). During human pregnancy, maternal exposure to substances able to alter placental retinoid metabolism could provide a novel, additional explanation for fetal teratogenic pathology.
Abbreviations
- RA:
-
retinoic acid
- RBP:
-
retinol binding protein
- HBSS:
-
Hanks' balanced salt solution
- DMEM:
-
Dulbecco's modified Eagle medium
References
Wilson JG, Roth CB, Warkany J 1953 An analysis of the syndrome of malformations induced by maternal A deficiency: effects of restoration of vitamin A at various times in gestation. Am J Anat 92: 189–217
Chambon P 1994 The retinoid signalling pathway: molecular and genetic analyses. Semin Cell Biol 5: 115–125
Mason KE 1935 Foetal death, prolonged gestation and difficult parturition in the rat as result of vitamin A. Am J Anat 57: 303–311
Wallingford JC, Underwood BA 1986 Vitamin A deficiency in pregnancy, lactation and the nursing child. In: Bauernfeind CJ (ed) Vitamin A Deficiency and Its Control. Academic Press, New York, pp 47–64
Takahashi YI, Smith JE, Winick M, Goodman DS 1975 Vitamin A deficiency and fetal growth and development in the rat. Am J Physiol 233: E263
Morriss-Kay GM, Ward SJ 1999 Retinoids and embryonic development. Int Rev Cytol 188: 73–133
Cohlan SQ 1953 Excessive intake of vitamin A as a cause of congenital anomalies in the rat. Science 117: 535–536
Miller RK, Faber W, Asai M, D'Gregorio RP, Ng WW, Shah Y, Neth-Jessee L 1993 The role of the human placenta in embryonic nutrition: impact of environmental and social factors. Ann N Y Acad Sci 678: 92–107
Satre MA, Ugen KE, Kochhar DM 1992 Developmental changes in endogenous retinoids during pregnancy and embryogenesis in the mouse. Biol Reprod 46: 802–810
Ross AC, Gardner EM 1994 The function of vitamin A in cellular growth and differentiation, and its roles during pregnancy and lactation. Adv Exp Med Biol 352: 187–200
Ismadi SD, Olson JA 1982 Dynamics of the fetal distribution and transfer of vitamin A between rat fetuses and their mother. Int J Vitam Nutr Res 52: 112–119
Donoghue S, Richardson DW, Sklan D, Kronfeld DS 1982 Placental transport of retinol in sheep. J Nutr 112: 2197–2203
Vahlquist A, Nilsson S 1984 Vitamin A transfer to the fetus and to the amniotic fluid in rhesus monkey (Macaca mulatta). Ann Nutr Metab 28: 321–333
Dimenstein R, Trugo NM, Donangelo CM, Trugo LC, Anastacio AS 1996 Effect of subadequate maternal vitamin-A status on placental transfer of retinol and beta-carotene to the human fetus. Biol Neonate 69: 230–234
Sapin V, Alexandre MC, Cha239'95b S, Bournazeau JA, Sauvant P, Borel P, Jacquetin B, Grolier P, Lémery D, Dastugue B, Aza239'95s-Braesco V 1999 Vitamin A status at the end of term pregnancy in well-nourished French women: evidence of modified retinol-binding protein saturation with retinol. Am J Clin Nutr 71: 537–543
Torma H, Vahlquist A 1986 Uptake of vitamin A and retinol-binding protein by human placenta in vitro. Placenta 7: 295–305
Dancis J, Levitz M, Katz J, Wilson D, Blaner WS, Piantedosi R, Goodman DS 1992 Transfer and metabolism of retinol by the perfused human placenta. Pediatr Res 32: 195–199
Siegenthaler G 1990 Gel electrophoresis of cellular retinoic acid binding proteins, cellular retinol binding proteins and serum retinol binding protein. Methods Enzymol 189: 299–307
Leroy B, Lefort F 1971 The weight and size of newborn infants at birth. Rev Fr Gynecol Obstet 66: 391–396
Schwab ME, Muller C, Schmid-Tannwald I 1984 Fast and reliable culture method for cells from 8–10 week trophoblast tissue. Lancet 12: 1082–1084
Nakamura Y, Ohta Y 1990 Immunohistochemical study of human placental stromal cells. Hum Pathol 21: 936–940
Kohnen G, Kertschanska S, Demir R, Kaufmann P 1996 Placental villous stroma as a model system for myofibroblast differentiation. Histochem Cell Biol 105: 415–429
Kliman HJ, Nestler JE, Sermasi E, Sanger JM, Strauss JF 3d 1986 Purification, characterization, and in vitro differentiation of cytotrophoblasts from human term placentae. Endocrinology 118: 1567–1582
Daya D, Sabet L 1991 The use of cytokeratin as a sensitive and reliable marker for trophoblastic tissue. Am J Clin Pathol 95: 137–141
Polliotti BM, Abramowsky C, Schwartz DA, Keesling SS, Lee GR, Caba J, Zhang W, Panigel M, Nahmias AJ 1995 Culture of first-trimester and full-term human chorionic villus explants: role of human chorionic gonadotropin and human placental lactogen as a viability index. Early Pregnancy 1: 270–280
Borel P, Tyssandier V, Mekki N, Grolier P, Rochette Y, Alexandre-Gouabau MC, Lairon D, Azais-Braesco V 1998 Chylomicron beta-carotene and retinyl palmitate responses are dramatically diminished when men ingest beta-carotene with medium-chain rather than long-chain triglycerides. Nutrition 128: 1361–1367
Borel P, Dubois C, Mekki N, Grolier P, Partier A, Alexandre-Gouabau MC, Lairon D, Azais-Braesco V 1997 Dietary triglycerides, up to 40 g/meal, do not affect preformed vitamin A bioavailability in humans. Eur J Clin Nutr 51: 717–722
Labarca C, Paigen K 1980 A simple, rapid, and sensitive DNA assay procedure. Anal Biochem 102: 344–352
Camara PD, Wright C, Dextraze P, Griffiths WC 1991 Comparison of a commercial method for total protein with a candidate reference method. Ann Clin Lab Sci 21: 335–339
Goodman DS, Blaner WS 1984 Biosynthesis, absorption and hepatic metabolism of retinol. In: Sporn MB, Roberts AB, Goodman DS (ed) The Retinoids, Vol 2. Academic Press, Orlando, FL, pp 2–39
Korner T, Rath FW, Schmidt H 1988 The ability of cultivated human skin fibroblasts to store vitamin A: a contribution to the cytogenesis of the Ito cells of the liver. Exp Pathol 35: 247–251
Takagawa K, Hirosawa K 1989 Uptake of retinol by cultured fibroblasts. Cell Struct Funct 14: 353–362
Cross JC, Werb Z, Fisher SJ 1994 Implantation and the placenta: key pieces of the development puzzle. Science 266: 1508–1518
Creech-Kraft J, Nau H, Lammer E, Olney A 1987 Embryonic retinoid concentration after maternal intake of isotretinoin. N Engl J Med 321: 262–264
Datta K, Kulkarni AP 1996 Co-oxidation of all-trans retinol acetate by human term placental lipoxygenase and soybean lipoxygenase. Reprod Toxicol 10: 105–112
Torma H, Lontz W, Liu W, Rollman O, Vahlquist A 1994 Expression of cytosolic retinoid-binding protein genes in human skin biopsies and cultured keratinocytes and fibroblasts. Br J Dermatol 131: 243–249
Johansson S, Gustafson A, Donovan M, Eriksson U, Dencker L 1999 Retinoid binding proteins-expression patterns in the human placenta. Placenta 20: 459–465
Blomhoff R 1994 Transport and metabolism of vitamin A. Nutr Rev 52: S13
Grimes RW, Pepe GJ, Albrecht ED 1996 Regulation of human placental trophoblast low-density lipoprotein uptake in vitro by estrogen. J Clin Endocrinol Metab 81: 2675–2679
Murata M, Kodama H, Goto K, Hirano H, Tanaka T 1996 Decreased very-low-density lipoprotein and low-density lipoprotein receptor messenger ribonucleic acid expression in placentas from preeclamptic pregnancies. Am J Obstet Gynecol 175: 1551–1556
Winkel CA, Gilmore J, MacDonald PC, Simpson ER 1980 Uptake and degradation of lipoproteins by human trophoblastic cells in primary culture. Endocrinology 107: 1892–1898
Van Bennekum AM, Blaner WS, Seifert-Bock I, Moukides M, Brouwer A, Hendriks HF 1993 Retinol uptake from retinol-binding protein (RBP) by liver parenchymal cells in vitro does not specifically depend on its binding to RBP. Biochemistry 32: 1727–1733
Hodam JR, Creek KE 1998 Comparison of the metabolism of retinol delivered to human keratinocytes either bound to serum retinol-binding protein or added directly to the culture medium. Exp Cell Res 10: 257–264
Davis BH, Vucic A 1989 Modulation of vitamin A metabolism during hepatic and intestinal cell culture. Biochim Biophys Acta 6: 318–324
Parrow V, Horton C, Maden M, Laurie S, Notarianni E 1998 Retinoids are endogenous to the porcine blastocyst and secreted by trophectoderm cells at functionally-active levels. Int J Dev Biol 42: 629–632
Acknowledgements
The authors thank Simon Ward, Dominey Yallop, and Pascal Dollé for critically reading the manuscript, and all the midwives for their availability, professional competence and kindness, which have made this study possible. We also thank the technicians of the Laboratory of Biochemistry and Immunology of Center Hospitalier Universitaire (Clermont-Ferrand) for their kind help.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Sapin, V., Chaïb, S., Blanchon, L. et al. Esterification of Vitamin A by the Human Placenta Involves Villous Mesenchymal Fibroblasts. Pediatr Res 48, 565–572 (2000). https://doi.org/10.1203/00006450-200010000-00024
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200010000-00024
This article is cited by
-
Antenatal retinoic acid administration increases trophoblastic retinol-binding protein dependent retinol transport in the nitrofen model of congenital diaphragmatic hernia
Pediatric Research (2016)
-
Nitrofen increases total retinol levels in placenta during lung morphogenesis in the nitrofen model of congenital diaphragmatic hernia
Pediatric Surgery International (2014)
-
Nitrofen interferes with trophoblastic expression of retinol-binding protein and transthyretin during lung morphogenesis in the nitrofen-induced congenital diaphragmatic hernia model
Pediatric Surgery International (2012)