Abstract
Activation of P1 purinergic receptors by adenosine and P2 receptors by ATP plays an important role in pulmonary vasodilation that occurs at birth in fetal lambs. Purine receptors occur in several subtypes, and the effects of their stimulation vary with the specific type involved. We characterized the subtypes of P1 receptors in fetal lamb pulmonary circulation at 128–132 d gestation by investigating the effects of the following adenosine analogs:N6-cyclopentyl adenosine (A1 selective), 2-phenylaminoadenosine (A2 selective), 2-p-(2-carboxyethyl)phenethylamino-5′-N-ethylcarboxamidoadenosine (A2A selective), N6-benzyl-5′-N-ethylcarboxamidoadenosine (A3 selective), and adenosine and 5′-N-ethylcarboxamidoadenosine (nonselective). We repeated the studies after treatment of animals with A1 antagonist 1,3-dipropyl-8-cyclopentylxanthine or A2 antagonist 1,3-dipropyl-7-methylxanthine. Identification of P2 receptors was done by investigation of the effects of P2x agonist β,γ-methylene-L-ATP and P2x and P2y agonist ATP. The studies were repeated after the treatment of animals with P2x antagonist suramin and the P2y antagonist cibacron blue. N6-cyclopentyl adenosine caused a significant decrease in heart rate and did not change pulmonary blood flow or pulmonary vascular resistance (PVR). The effect of N6-cyclopentyl adenosine on heart rate was abolished by 1,3-dipropyl-8-cyclopentylxanthine but not by 1,3-dipropyl-7-methylxanthine. 2-Phenylaminoadenosine, 2-p-(2-carboxyethyl)phenethylamino-5′-N-ethylcarboxamidoadenosine, 5′-N-ethylcarboxamidoadenosine, and adenosine caused significant increases in pulmonary flow and decreases in PVR, and their vasodilator effects were attenuated by the A2 antagonist 1,3-dipropyl-7-methylxanthine and not by 1,3-dipropyl-8-cyclopentylxanthine. N6-benzyl-5′-N-ethylcarboxamidoadenosine did not alter pulmonary flow or PVR. The P2x agonist β,γ-methylene-L-ATP caused a decrease in heart rate and had no effect on pulmonary flow and PVR. ATP caused a significant increase in pulmonary flow and decrease in PVR without affecting heart rate. The vasodilator effects of ATP were attenuated by cibacron blue and not by suramin. These data demonstrate that adenosine and ATP cause pulmonary vasodilation by activation of A2A and P2y receptors, respectively, in fetal lambs.
Similar content being viewed by others
Main
The purine nucleotide ATP and its nucleoside adenosine play a major role in birth-related transition in pulmonary circulation (1–3). Exposure of fetal lambs to oxygen at birth causes an increased release of ATP into pulmonary circulation (1, 2). ATP and its breakdown product adenosine are potent pulmonary vasodilators in the perinatal lamb (3). The vasodilator effects of adenosine and ATP appear to be nitric oxide-dependent (4). However, the specific receptors that mediate the effects of adenosine and ATP in the fetal pulmonary circulation are unknown. Identification of these receptors is essential to characterize their maturation and to investigate the specific signaling pathways that cause vasodilation in response to their activation.
Previous studies demonstrated that extracellular adenosine and ATP exert their biologic effects by activation of P1 and P2 purinergic receptors, respectively (5). These receptors are widely distributed in tissues, and their stimulation results in very diverse physiologic effects (6). The adenosine sensitive P1 receptors are known to have 4 subtypes, classified as A1, A2A, A2B, and A3, based on pharmacologic tools and molecular cloning (7, 8). The ATP-sensitive P2 receptors are classified as P2x and P2y subtypes (9). It is now recognized that the biologic effects of adenosine and ATP depend on the predominance of specific receptor subtype in the tissue being studied (6, 7, 10, 11).
Attempts to characterize the P1 receptors in pulmonary circulation were previously done in postnatal animals. Studies in isolated blood-perfused lungs of adult rats indicated that adenosine-induced vasodilation is mediated by the A2B adenosine receptor (12). Studies in vascular rings from juvenile rabbit pulmonary arteries and veins demonstrated that adenosine causes vasodilation by stimulation of A2 receptors (13). The pulmonary vascular bed (14, 15) of adult cats shows tone-dependent responses to adenosine, a vasoconstrictor response when the preexisting tone is low and vasodilation when the preexisting tone is high. The vasoconstrictor and dilator responses appear to be mediated by A1 and A2 receptors, respectively. In contrast, adenosine consistently elicits a vasodilator response in the perinatal lamb (3, 16). These studies indicate marked species and age-related differences in the response to purinergic stimulation. Therefore, identification of specific purine receptor subtypes in fetal pulmonary circulation is essential for investigation of their role in causing birth-related pulmonary vasodilation. The objective of the experiments described here is to characterize the purine receptor subtypes in the pulmonary circulation of the intact fetal lamb by comparison of the effects of selective agonists and antagonists for P1 and P2 purinergic receptors (Fig 1).
METHODS
We studied 18 fetal lambs, instrumented at 124 d of gestation (term gestation = 140 d). Nine fetal lambs underwent studies with adenosine analogs and adenosine receptor antagonists. Nine other fetal lambs were studied with agonists and antagonists for P2 receptors. The experiments with the agonists and antagonists were done on separate days, and the order of the experiments was randomized for each animal. The studies were approved by the Human and Animal Investigation Committee of Wayne State University, Detroit, Michigan.
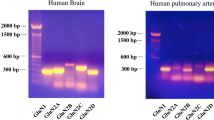
The receptor specific and nonspecific agents used in our studies are summarized in Figure 1. These agents were chosen based on selective affinity for different receptor subtypes. CPA and DPCPX were shown to be highly selective for the A1 receptor in the rat CNS and pulmonary circulation (8, 12, 14). CGS21680 has been shown to bind with high affinity to the A2A purine receptor in rat CNS and in systemic circulation (8, 17). CV1808 binds with the A2A receptor with high affinity and the A2B receptor with low affinity (18) in the rat vas deferens and CNS. MDPX is a highly selective A2 receptor antagonist in rat CNS and in human platelets (19). Human and rat A3 receptors bind N6-benzyl-NECA preferentially in the nervous system and in systemic circulation (20, 21). L-AMP PCP is a known specific P2x agonist, based on lack of stereo specificity of the P2x receptor to L- or naturally occurring D-enantiomers of ATP (22). Suramin has been shown to bind the P2x receptor in guinea pig vas deferens and urinary bladder preferentially (23), and cibacron blue is a selective P2y receptor antagonist in rabbit mesenteric artery (9).
Drug preparation.
CPA, CV1808, and NECA [Research Biochemical International (RBI), Natick, MA] were dissolved in sterile water with a concentration of 200 μg/mL. N6-benzyl-NECA (RBI) was dissolved in a concentration of 100 μg/mL in sterile water. CGS21680 HCl (RBI) was initially dissolved in ethyl alcohol in a concentration of 1 mg/mL and was subsequently diluted with sterile water to give a final concentration of 50 μg/mL. Adenosine and ATP (Sigma Chemical Co., St. Louis, MO) were dissolved in sterile water in a concentration of 2 mg/mL. DPCPX and MDPX (RBI) were dissolved in ethyl alcohol in a concentration of 2 mg/mL and subsequently diluted with sterile water to a final concentration of 0.5 mg/mL. Suramin (RBI) and cibacron blue (Sigma Chemical Co.) were dissolved in sterile water in a concentration of 5 mg/mL.
Surgical instrumentation.
Pregnant sheep were brought into the facility at 118 d of gestation. Instrumentation of the sheep was done after a 4–6-d period of acclimatization to the facility. Solid food was withheld for 24 h and water was withheld for 12 h before instrumentation. Sterile surgery on the sheep was done under general anesthesia with isoflurane and oxygen administered via an endotracheal tube. The fetus was approached via a subumbilical midline incision and a hysterotomy incision. Catheters made from Tygon tubing (Baxter Diagnostics, McGraw Park, IL) were inserted into the right atrium and ascending aorta of the fetus via the left external jugular vein and left common carotid artery. Then a left lateral thoracotomy was done on the fetus, and catheters were placed in the left pulmonary artery and in the left atrium by direct puncture. An ultrasonic flow transducer (4S or 6S, Transonic Systems, Inc., Ithaca, NY) was inserted around the left pulmonary artery to measure the blood flow to the left lung. All the catheters and the cable for the transducer were exteriorized to the flank of the ewe. A catheter was placed in the amniotic cavity to measure the amniotic fluid pressure that served as zero reference for the fetal intravascular pressures. The fetal lamb and ewe were allowed to recover for 3 d before doing experiments.
The fetal intravascular pressures and pulmonary flow were continuously recorded on a Grass model 7D physiograph. Data for mean vascular pressures and mean pulmonary flow were reported in the graphs. The fetal blood gas tensions and blood pH were measured with a blood gas analyzer (ABL 30, Radiometer, Inc., Copenhagen, Denmark).
Protocol for P1 (adenosine) receptor studies.
The ewe was brought to the study area and was kept in a cage with continuous access to food and water. For the control studies, the vehicle used to dissolve DPCPX and MDPX was infused into the left pulmonary artery and baseline hemodynamic and blood gas measurements were obtained after 20 min. Then a continuous infusion of one of the adenosine analogs was given into the left pulmonary artery of the fetus over 5 min. The animal was allowed to recover for 10 to 15 min before the next dose was infused. Each analog was infused at 0.15, 0.30, and 0.60-μmol doses. At the completion of each analog infusion, the animal was allowed to recover for at least 2 h before another study. Each animal had no more than two infusion studies per day, and the order of infusions was randomized. The hemodynamic variables were recorded at each dose of the analog at the end of a 5-min infusion period. Arterial blood gas tensions and blood pH were measured at the end of each analog infusion study. On a separate day, the fetal lamb was pretreated with either 10 mg of DPCPX or 5 mg of MDPX given into the left pulmonary artery over 5 min as an infusion. Baseline hemodynamic variables were recorded 20 min after the infusion of one of these agents. Then the infusion of the analogs into the left pulmonary artery was repeated as described previously.
Protocol for P2 receptor studies.
Control studies were done after infusion of the vehicle used to dissolve suramin and cibacron blue into the left pulmonary artery. Baseline measurements were obtained 20 min after the infusion of the vehicle. Infusion of L-AMP PCP or ATP was given into the left pulmonary artery in doses of 0.15, 0.3, and 0.6 μmol. Higher doses of L-AMP PCP caused significant bradycardia in the fetal lamb. Each dose of the agonist was infused over 5 min, and hemodynamic variables were measured at the end of the 5-min period. Arterial blood gas tensions and blood pH were measured at baseline and at the end of each infusion. Infusion with L-AMP PCP and ATP were done 4 h apart. On separate days, the animal was pretreated with either 50 mg of suramin, a P2x antagonist (23), or 15 mg of cibacron blue, a P2y receptor antagonist (9). Hemodynamic variables were measured 20 min after the infusion of the antagonists. Then the infusion of ATP was given into the left pulmonary artery as described before.
Statistical analysis.
A sample size of eight animals for each infusion study was estimated in the following manner. The number of animals required to detect a 50% change in left pulmonary flow from 65 ± 32 and 50% change in PVR from 2.2 ± 1 (mean ± SD for baseline from pilot studies) with an α of 0.05 and 80% power was eight, using repeated measures ANOVA. Our estimated survival of fetal lambs from complications of surgery and infusion studies was 80%. Thus 10 fetal lambs were instrumented for each group of studies for P1 and P2 receptors. Nine lambs each assigned to P1 and P2 receptor studies have survived to complete all the experiments. One animal in each group died after prolonged bradycardia observed with infusions of CPA and L-AMP PCP. All data are expressed as mean ± 1 SD. Baseline variables measured on different days were compared by 1-way ANOVA to see if they were similar on each study day. The changes in hemodynamic variables during agonist infusions in control studies were compared by 2-way ANOVA with the type of agonist and dose of the agonist as two factors influencing the outcome. Similarly, control data were compared with receptor blocker studies by 2-way ANOVA with the dose of the agonist and the presence or absence of a blocker as the two factors. When a significant change, defined as p < 0.05, was found, a Duncan's multiple range test was done to determine where the differences were.
RESULTS
The fetal lambs were studied at 129 ± 3 d of gestation. They had normal weight at necropsy (3.1 ± 0.4 kg) and had normal pH (7.40 ± 0.1) and arterial pressure of O2 (PaO2) (2.56 ± 0.2 kPa) at the time of the study. The arterial pH (7.36 ± 0.03 to 7.42 ± 0.02), arterial pressure of CO2 (PaCO2) (4.5 ± 0.3 to 5.5 ± 0.5 kPa), and PaO2 (2.3 ± 0.1 to 3.2 ± 0.5 kPa) did not change significantly during the studies.
P1 Receptor Characterization
Effect of P1 agonists on heart rate.
Infusion of CPA caused a significant and dose-dependent decrease in the heart rate at 0.3 and 0.6-μmol doses (Fig. 2). Infusion of CV1808 and N6-benzyl-NECA did not alter the heart rate significantly (Fig. 2). Infusion of adenosine and CGS21680 caused an increase in heart rate at the 0.6-μmol dose (Fig. 2). The effect of CPA on heart rate was inhibited by A1 blocker DPCPX but not by A2 blocker MDPX (Fig. 3). The effects of CGS21680 (Fig. 3) and adenosine (data not shown) on heart rate were inhibited by MDPX and not by DPCPX. These data indicate that A1 receptor stimulation causes a bradycardia response and A2 receptor stimulation causes tachycardia.
Effect of P1 receptor antagonists on changes in heart rate caused by A1 agonist CPA (left) and A2A agonist CGS21680 (right). Data are mean ± SD for n = 9. Drug = data obtained 20 min after infusion of antagonist or its vehicle (control). Dose of each agonist in μmol is shown as independent variable. ★p < 0.05 from BL for each study group.
Effect of P1 agonists on pulmonary circulation.
The A1 agonist CPA and A3 agonist N6-benzyl-NECA did not alter pulmonary blood flow (Fig. 4). Infusions of A2 agonists CV1808 and CGS21680 and nonspecific agonists adenosine and NECA caused significant and dose-dependent increases in pulmonary flow (Fig. 4). CV1808 had a greater effect than CGS21680, and NECA had a greater effect than adenosine at comparable doses (Fig. 4). The A1 receptor antagonist DPCPX did not alter the baseline vascular pressures, flow, or heart rate. The A2 receptor antagonist MDPX increased the baseline pulmonary artery pressure by 12% but did not alter the pulmonary flow or heart rate. The increases in pulmonary flow caused by CV1808, CGS21680 (Fig. 5), NECA, and adenosine (data not shown) were inhibited by A2 antagonist MDPX and not by A1 antagonist DPCPX. CPA and N6-benzyl-NECA did not alter the PVR significantly (Fig. 6). Infusions of CV1808, CGS21680, NECA, and adenosine decreased the PVR in a dose-dependent manner (Fig. 6). The decreases in PVR caused by CV1808, CGS 21680 (Fig. 7), NECA, and adenosine (data not shown) were significantly inhibited by MDPX and not by DPCPX. These data indicate that A2 receptors and not A1 or A3 receptors mediate the pulmonary vasodilation caused by adenosine.
Effect of P1 receptor agonists CPA (A1), CV1808 (A2), N6-benzyl-NECA (A3), CGS21680 (A2A), NECA (P1), and adenosine (P1) on left pulmonary blood flow, shown as mL/min. Dose of each agonist in μmol is shown as independent variable. Data are mean ± SD for n = 9. ★p < 0.05 from BL for each study group, #p < 0.05 between CGS21680 and CV1808 and @ between adenosine and NECA.
Effect of P1 receptor antagonists on pulmonary vasodilation caused by CV1808 (left) and CGS21680 (right). Data are mean ± SD for n = 9. Drug = data obtained 20 min after infusion of antagonist or its vehicle (control). Dose of each agonist in μmol is shown as independent variable. ★p < 0.05 from BL for each study group and # from control data obtained at the same dose of agonist.
Effect of P1 receptor antagonists on changes in PVR caused by CV1808 (left) and CGS21680 (right). Data are mean ± SD for n = 9. Drug = data obtained 20 min after infusion of antagonist or its vehicle (control). Dose of each agonist in μmol is shown as independent variable. ★p < 0.05 from BL for each study group and # from control data obtained at the same dose of agonist.
Effect of P1 agonists on systemic pressure.
CPA decreased the systemic arterial pressure at the 0.6-μmol dose that also caused significant bradycardia. The decrease in systemic pressure was abolished when the bradycardia response was prevented by DPCPX. MDPX did not alter the bradycardia or hypotension caused by CPA. The other adenosine analogs did not alter the systemic pressure.
P2 Receptor Characterization
Infusion of the P2x agonist L-AMP PCP caused a decrease in heart rate at the 0.6-μmol dose (Fig. 8). The P2x antagonist suramin inhibited the decrease in heart rate caused by L-AMP PCP (data not shown). ATP did not alter the heart rate significantly (Fig. 8). L-AMP PCP had no effect on pulmonary blood flow (Fig. 8), pulmonary artery pressure, or PVR. Infusion of ATP caused a significant and dose-dependent increase in pulmonary flow and decrease in PVR at all three doses (Figs. 8 and 9). The increase in pulmonary flow and decrease in PVR caused by ATP were not altered by the P2x antagonist suramin but were attenuated by the P2y receptor antagonist cibacron blue (Fig. 9). These data indicate that the vasodilation caused by ATP is due, in part, to stimulation of P2y receptors in the pulmonary arteries.
Effect of P2 receptor antagonists suramin (P2X) and cibacron blue (P2Y) on changes in pulmonary flow (left) and PVR (right) caused by ATP. Data are mean ± SD for n = 9. Drug = data obtained 20 min after infusion of antagonist or its vehicle (control). Dose of each agonist in μmol is shown as independent variable. ★p < 0.05 from BL for each study group and # from control data obtained at the same dose of agonist.
DISCUSSION
Our study demonstrates that the pulmonary vasodilation caused by adenosine is mediated by A2 adenosine receptor and the vasodilation caused by ATP is mediated by P2y purine receptor in the fetal lamb. These receptors appear to be functional and active in the fetal lamb pulmonary circulation by 128 d of gestation. Our studies were done in the intact fetal lamb after recovery from effects of surgery. This in vivo characterization confirms the significance of these receptors in mediating pulmonary vasodilation caused by purine nucleotides in the fetal lamb in its physiologic state. However, our studies cannot address the localization of the receptors to vascular endothelium or the vascular smooth muscle cell.
The classification of purine receptors as P1 and P2 was based on their preferential activation by adenosine or ATP, sensitivity of P1 receptors to inhibition by methylxanthines, and mediation of P1 receptor effects by cAMP (5). These receptors are now known to occur in several subtypes that elicit very different responses with activation (6). The A1 and A3 subtypes of P1 receptors decrease the adenylate cyclase activity, and A2A and A2B receptors promote the activity of this enzyme, resulting in altered cAMP levels (8). The A1 and A3 adenosine receptors in the heart mediate the negative chronotropic, inotropic, and dromotropic effects of adenosine (8). The vasodilation and the inhibition of platelet aggregation caused by adenosine are mediated predominantly by A2A and A2B receptors (8). The biologic effects of P2 receptor activation are generally independent of intracellular cAMP levels. The P2x subtype of P2 receptors are ligand gated cation channels found on vascular and visceral smooth muscle where they mediate a constrictor response (10) and in the CNS (6). The P2y receptors are a family of G-protein coupled receptors found on vascular endothelial cells, pulmonary epithelium, and in CNS (10, 11). Studies in adult animals have given variable results with respect to the role of these receptors in mediating these responses (8, 12, 14, 15). Our studies in fetal lambs have shown that vasodilator responses to adenosine and ATP are mediated predominantly by A2 and P2y receptors, respectively. The proposed receptor distribution and the possible effects of their stimulation on the fetal cardiovascular system are shown in Figure 10.
Our studies demonstrated that A1 receptor stimulation causes bradycardia without altering the pulmonary flow or PVR. A2 receptor stimulation causes vasodilation without eliciting a bradycardia response. These data suggest that the A1 receptors appear predominantly in the heart where they mediate a negative chronotropic effect. A1 receptors are probably not involved in mediating pulmonary vasodilator responses in the fetal lamb. The decreases in systemic and pulmonary vascular pressures during CPA infusion only occurred at the doses that caused significant bradycardia. The fall in vascular pressures was not accompanied by significant changes in pulmonary flow or PVR. The decrease in pulmonary artery pressure at the 0.6-μmol dose of CPA was accompanied by a decrease in left atrial pressure from 8 ± 3 to 3 ± 2, keeping the PVR unchanged. The decrease in pulmonary artery pressure was prevented by the A1 antagonist DPCPX, which also allowed the heart rate to remain normal during CPA infusion. These data are consistent with previous reports that the A1 receptors are not involved in mediating the vasodilator effects of adenosine in adult rat pulmonary circulation (12). This conclusion is also supported by radioligand-binding studies that demonstrated a low density of A1 receptors in human lung tissue (25).
Structure activity data and radioligand-binding studies have suggested two subtypes within the A2 receptor, and these are classified as A2A and A2B (8). This classification is based on high or low affinity of the receptor for adenosine. The A2A adenosine receptor binds at high affinity to both NECA and CGS21680, whereas the A2B adenosine receptor binds to NECA with a low affinity and does not bind CGS21680. Human lung tissue was found to express both A2A and A2B adenosine receptors. Joad and Kott (26) reported that both NECA and CGS21680 increased cAMP concentrations in the human peripheral lung tissue. We attempted to characterize the A2 receptor and identify whether the vasodilation was caused by activation of the A2A or A2B receptor in our studies. The vasodilator response to CV1808 and CGS21680 suggests a role for A2 receptors in mediating this effect. Inhibition of vasodilation caused by nonspecific agents NECA and adenosine by A2 selective antagonist MDPX but not by A1 selective DPCPX also suggests that A2 receptors mediate this response. We also demonstrated that A2A receptor stimulation in fetal lambs causes vasodilation, an effect that is different from the observations made in adult rat pulmonary circulation (12). Our conclusion is based on a) significant pulmonary vasodilation caused by CGS21680 and b) by prolonged vasodilation observed after infusions of CGS21680 and NECA, indicating a role for high affinity A2A receptor in causing this response. Although CGS21680 caused an increase in heart rate at the 0.6-μmol dose, the vasodilator effect is unlikely to be from increased heart rate. Significant pulmonary vasodilation was seen at the lower dose that did not alter the heart rate. MDPX caused a significant inhibition of the vasodilator response to CGS21680 even though the heart rate was only 13% lower than during control infusion. The increase in pulmonary blood flow during CGS21680 was accompanied by a 19% decrease in pulmonary artery pressure (data not shown) and a 10-fold reduction in PVR. These findings differ from the report of Haynes et al. (12) in adult rat pulmonary circulation. They demonstrated that CGS21680 does not attenuate the hypoxic pressor response in the rat pulmonary circulation, whereas both adenosine and NECA cause significant attenuation of the hypoxic pressor response. On the basis of these findings, they suggested that the pulmonary vasodilation caused by adenosine in pulmonary circulation is probably mediated by A2B receptor. The differences in our findings may be due to maturational changes in the receptor population in the lung, a result of difference in the preexisting vascular tone, or species-related differences. The fetus under physiologic condition has a high pulmonary vascular resistance and high pulmonary artery pressure. Therefore, we did not use hypoxic or pharmacologic vasoconstriction in the fetus at baseline. Haynes et al. (12) used hypoxic stimulus to increase the pulmonary vascular tone at baseline in the adult rats. It is possible that this stimulus may alter the activity of the specific receptor subtypes. The possibility of species-related differences are supported by our previous study demonstrating inhibition of adenosine-induced vasodilation by N-nitro-L-arginine in fetal lambs (4), whereas Haynes et al. (12) did not observe an alteration in adenosine-induced vasodilation by L-NAME in rats. Currently there are no specific agonists or antagonists for the A2B receptor that will allow more direct evaluation of their role in mediating vasodilation under different physiologic conditions (8).
We observed that A3 receptor stimulation by N6-benzyl-NECA did not alter the heart rate, a response that was distinct from that observed with A1 agonist CPA. N6-benzyl-NECA did not cause pulmonary vasodilation, a response different from that seen with A2 agonists. The receptor activated by N6-benzyl-NECA is probably distinct from the receptors activated by NECA, CV1808, and CGS21680. These results suggest that although A3 receptors are present in both human and sheep lungs (20, 25), their role in eliciting a pulmonary vasodilator response is probably not significant. Recent studies by Salvatore et al. (20) on molecular cloning and characterization of the human A3 adenosine receptor confirm the widespread distribution of A3 receptors in several tissues including brain, lung, and testes. However, the precise physiologic role for the A3 adenosine receptor is yet to be determined.
We attempted to characterize the P2 purinergic receptor by using the differences in the sensitivity of P2x and P2y subtypes to D- and L-enantiomers of ATP. The naturally occurring ATP contains the ribose moiety in the dextro configuration. The P2x receptors are not stereo specific and are activated by both L- and D-enantiomers (27). The P2y receptor, however, is sensitive only to naturally occurring D-enantiomers. Therefore, L-AMP PCP is a specific P2x agonist (22). Our studies showed that L-AMP PCP is devoid of vasodilator effects in the fetal lamb pulmonary circulation and elicits only a bradycardia response. The naturally occurring ATP, on the other hand, causes potent pulmonary vasodilation. Therefore, it appears that the P2x receptor is found predominantly in the heart where it has a negative chronotropic effect. The vasodilator response to ATP appears to be due to activation of the P2y receptor. This finding is further supported by a significant inhibition of the ATP-induced vasodilation by the P2y specific antagonist cibacron blue and not by the P2x antagonist suramin (23). Previous studies have shown that the P2y receptor in the rat lung facilitates surfactant release from type 2 pneumocytes (28). Cloning of the P2y receptor has been recently accomplished (11). Our previous studies have documented a significant role for ATP in mediating oxygen-induced pulmonary vasodilation in the fetal lamb (1, 2). Identification of the specific receptor that mediates the effects of ATP is an important step in defining its role in birth-related transition in the pulmonary circulation.
The role of purine receptors in maintaining basal vascular tone in the fetal lamb was not clear from our study. Infusion of purine receptor antagonists in our study had variable hemodynamic effects. Since A1 and A2 receptors appear to have negative chronotropic and vasodilator effects, respectively, we expected to see an increase in heart rate with DPCPX and an increase in vascular pressure with MDPX. However, the high resting heart rate and high resting pulmonary vascular tone normally seen in the fetus may attenuate the responses to these agents in the fetal circulation. An alternate explanation may be that purine receptors do not play a significant role in maintaining the resting heart rate or vascular tone in the fetal lamb.
We previously reported that both adenosine and ATP cause pulmonary vasodilation by a nitric oxide-dependent mechanism (29). The arginine analog N-nitro-L-arginine inhibits the vasodilation caused by adenosine and ATP in the intact fetal lamb. Nitro-L-arginine also inhibits pulmonary vasodilation caused by ATP-MgCl2 in newborn lambs with pulmonary hypertension induced by U46619 (30). We also reported that the vasodilator effects of adenosine are inhibited by glybenclamide, a K+ATP channel antagonist (29). These data suggest that purine receptor stimulation is followed by important biologic effects such as activation of ion channels and release of nitric oxide in the fetal lamb pulmonary circulation. The specific signaling pathways that mediate the effects of purine receptor stimulation are yet to be determined. Further studies are also needed to document the maturation of the A2 and P2y receptors during fetal life. This information is essential to understand their role in physiologic events that occur at birth in the fetus.
Abbreviations
- CPA:
-
N6-cyclopentyl adenosine
- CV1808:
-
2-phenylaminoadenosine
- CGS21680:
-
2-p-(2-carboxyethyl)phenethylamino-5′-N-ethylcarboxamidoadenosine
- NECA:
-
5′-N-ethylcarboxamidoadenosine
- N6-benzyl-NECA:
-
N6-benzyl-5′-N-ethylcarboxamidoadenosine
- DPCPX:
-
1,3-dipropyl-8-cyclopentylxanthine
- MDPX:
-
1,3-dipropyl-7-methylxanthine
- ATP:
-
adenosine 5′-triphosphate
- L-AMP PCP:
-
β,γ-methylene-L-ATP
- PVR:
-
pulmonary vascular resistance
References
Konduri GG, Gervasio CT, Theodorou AA 1993 Role of adenosine triphosphate and adenosine in oxygen-induced pulmonary vasodilation in fetal lambs. Pediatr Res 33: 533–539.
Konduri GG, Mital S, Gervasio CT, Rotta AT, Forman K 1997 Purine nucleotides contribute to pulmonary vasodilation caused by birth-related stimuli in the ovine fetus. Am J Physiol 272: H2377–H2384.
Konduri GG, Theodorou AA, Mukhopadhyay A, Deshmukh DR 1992 Adenosine triphosphate and adenosine increase pulmonary blood flow to postnatal levels in fetal lambs. Pediatr Res 31: 451–457.
Konduri GG, Theodorou AA 1992 Nitro-L-arginine attenuates pulmonary vasodilation caused by adenosine in fetal lambs. Pediatr Res 31: 62A
Burnstock G 1978 A basis for distinguishing two types of purinergic receptor. In: Straub RW, Bolis L (eds) Cell Membrane Receptors for Drugs and Hormones: A Multi-Disciplinary Approach. Raven Press, New York, 107–115.
Burnstock G 1997 The past, present, and future of purine nucleotides as signalling molecules. Neuropharmacology 36: 1127–1139.
Olah ME, Stiles GL 1995 Adenosine receptor subtypes: characterization and therapeutic regulation. Annu Rev Pharmacol Toxicol 35: 581–606.
Shryock JL, Belardinelli L 1997 Adenosine and adenosine receptors in the cardiovascular system: biochemistry, physiology, and pharmacology. Am J Cardiol 79: 2–10.
Burnstock G, Warland JJI 1987 P2-purinoceptors of two subtypes in the rabbit mesenteric artery: reactive blue 2 selectively inhibits responses mediated via the P2y- but not P2x-purinoceptor. Br J Pharmacol 90: 383–391.
Houston DA, Burnstock G, Vanhoutte PM 1987 Different P2-purinergic receptor subtypes of endothelium and smooth muscle in canine blood vessels. J Pharmacol Exp Ther 241: 501–506.
Simon J, Webb TE, King BF, Burnstock G, Barnard EA 1995 Characterization of a recombinant P2y purinoceptor. Eur J Pharmacol 291: 281–289.
Haynes J, Obiako B, Thompson WJ, Downey J 1995 Adenosine-induced vasodilation: receptor characterization in pulmonary circulation. Am J Physiol 268: H1862–H1868.
Steinhorn RH, Molin FL, Van Wylen DGL, Gugino SF, Giese EC, Russell JA 1994 Endothelium-dependent relaxations to adenosine in juvenile rabbit pulmonary arteries and veins. Am J Physiol 266: H2001–H2006.
Neely CF, Matot I 1996 Pharmacologic probes for A1 and A2 adenosine receptors in vivo in feline pulmonary vascular bed. Am J Physiol 270: H610–H619.
Cheng DY, Dewitt BJ, Suzuki F, Neely CF, Kadowitz PJ 1996 Adenosine A1 and A2 receptors mediate tone-dependent responses in feline pulmonary vascular bed. Am J Physiol 270: H200–H207.
Konduri GG, Woodard LL, Mukhopadyay A, Deshmukh DR 1992 Adenosine is a pulmonary vasodilator in newborn lamb. Am Rev Respir Dis 146: 670–676.
Hutchison AJ, Webb RL, Oei HH, Ghai GR, Zimmerman MB, Williams M 1989 CGS21680C, an A2 selective agonist with preferential hypotensive activity. J Pharmacol Exp Ther 251: 47–55.
Taylor DA, Williams M 1982 Interaction of 2-phenylaminoadenosine (CV1808) with adenosine systems in rat tissues. Eur J Pharmacol 85: 335–338.
Ukena D, Shamim MT, Padgett W, Daly JW 1986 Analogs of caffeine: antagonists with selectivity for A2 adenosine receptors. Life Sci 39: 743–750.
Salvatore CA, Jacobson MA, Taylor HE, Linden J, Johnson RG 1993 Molecular cloning and characterization of the human A3 adenosine receptor. Proc Natl Acad Sci USA 90: 10365–10369.
Fozard JR, Carruthers AM 1993 Adenosine A3 receptors mediate hypotension in the angiotensin II supported circulation of the pithed rat. Br J Pharmacol 109: 3–5.
Hourani SMO, Loizou GD, Cusack NJ 1986 Pharmacologic effects of L -AMP PCP on ATP receptors in smooth muscle. Eur J Pharmacol 131: 99–103.
Bailey SJ, Hourani SM 1994 Differential effects of suramin on P2-purinoceptors mediating contraction of the guinea pig vas deferens and urinary bladder. Br J Pharmacol 112: 219–225.
Chow SC, Kass GEN, Orrenius S 1997 Purines and their role in apoptosis. Neuropharmacology 36: 1149–1156.
Joad JP 1990 Characterization of the human peripheral lung adenosine receptor. Am J Respir Cell Mol Biol 2: 193–198.
Joad JP, Kott KS 1993 Effect of adenosine receptor ligands on cAMP content in human airways and peripheral lung. Am J Respir Cell Mol Biol 9: 134–140.
Cusack NJ, Hourani SMO 1990 Subtypes of P2-purinoceptors. Ann NY Acad Sci 603: 172–181.
Gobran LI, Rooney SA 1997 Adenylate cyclase-coupled ATP receptor and surfactant secretion in type II pneumocytes from newborn rats. Am J Physiol 272: L187–L196.
Konduri GG 1993 Adenosine causes K+ ATP channel mediated release of endothelium-derived nitric oxide in ovine fetal pulmonary arteries. Pediatr Res 33: 248A
Fineman JR, Heymann MA, Soifer SJ 1991 N-nitro-L-arginine attenuates endothelium-dependent pulmonary vasodilation in lambs. Am J Physiol 260: H1299–H1306.
Author information
Authors and Affiliations
Additional information
Supported by a grant from Children's Hospital of Michigan Research Endowment Fund and a FIRST award (HL44533) from NHLBI.
Rights and permissions
About this article
Cite this article
Konduri, G., Forman, K. & Mital, S. Characterization of Purine Receptors in Fetal Lamb Pulmonary Circulation. Pediatr Res 47, 114 (2000). https://doi.org/10.1203/00006450-200001000-00020
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200001000-00020
This article is cited by
-
Purinergic signalling during development and ageing
Purinergic Signalling (2015)
-
Purinergic signaling in embryonic and stem cell development
Cellular and Molecular Life Sciences (2011)