Abstract
An elevated level of baseline parasympathetic activity was noted in a group of premature infants suffering from bradycardia during feeding. At approximately 34 wk post-conceptional age, the heart rates of 12 infants with feeding bradycardia (birth weight = 1539 ± 279 g; gestational age = 31.0 ± 1.6 wk) and 10 controls (birth weight = 1710 ± 304 g; gestational age = 32.0 ± 1.4 wk) were recorded 1 h before and 1 h after feeding. EKG data were digitized and 3.2-min segments of data were analyzed to determine the spectral power at very low (VLF = 0.003–0.03 Hz), low (LF = 0.03–0.39 Hz), and high (HF = 0.40–1.00 Hz) frequencies. In preterm infants with feeding bradycardia, an elevation in baseline parasympathetic activity was evident before feeding, as indicated by significantly higher HF power and a lower LF/HF ratio. This elevation in baseline parasympathetic activity may contribute to the observed bradycardia during feeding.
Similar content being viewed by others
Main
The noninvasive assessment of autonomic function has recently become the focus of research exploring the associations between the autonomic nervous system and neonatal pathology. Sudden infant death syndrome (SIDS), a disorder that is believed to be associated with autonomic dysfunction, has generated the most work using heart rate variability analysis as an index of autonomic activity (1–11). Other applications of neonatal heart rate variability analysis, however, have been scant (12–18).
Apnea and bradycardia are common in premature infants, and are accepted as a manifestation of immature cardiorespiratory control (19). However, preterm infants, and indeed some term infants, can suffer bradycardia during feeding, despite the absence of other cardiorespiratory symptoms and the lack of clinical gastroesophageal reflux. The nature of the autonomic nervous system's contribution to these symptoms is not well understood. Although reflex increases in parasympathetic activity are known to produce bradycardia, the susceptibility of some infants to feeding bradycardia remains to be explained.
In recent years, the development of spectral analysis techniques has allowed researchers to quantify the cyclic nature of variations in instantaneous heart rate (IHR) (20). In the human, the power spectra of adult (21, 22), child (15), and infant (14) heart rate variability contain two principle peaks. The first is a “low frequency” peak occurring at or below 0.12 Hz. Low frequency fluctuations in heart rate are jointly mediated by the sympathetic and parasympathetic nervous systems. The second “high frequency” peak represents fluctuations that are mediated solely by the parasympathetic system.
The aim of this study was to identify whether heart rate spectral power, an index of autonomic activity, differs between infants suffering feeding bradycardia, and asymptomatic controls. Because high frequency spectral power is a reflection of parasympathetic activity, we hypothesized that infants suffering bradycardia during feedings would have elevated baseline parasympathetic activity compared with their asymptomatic peers.
METHODS
Patient selection.
Over a 6-mo period, we studied 22 healthy preterm infants from the Special Care Nursery at St. Peter's University Hospital. Infants were considered for inclusion when they were receiving full oral feedings and had successfully weaned to a bassinet. Infants were excluded if they had suffered any prenatal complications preceding preterm labor, if they had any congenital anomalies, cardiac disease, CNS lesions, were receiving any medications, were clinically suspected of having gastroesophageal reflux, or required any supplemental oxygen or respiratory support at the time of study. Although a history of respiratory distress syndrome was not an exclusion criterion, infants were excluded if they had experienced any other complications during their hospital stay. The experimental group consisted of 12 infants suffering only feeding bradycardia (heart rate < 100 for ≥5 s during feeding), and 10 asymptomatic infants served as controls. Infants were being bottle fed every 3 h, and symptomatic infants typically suffered bradycardia during several (1–3) feedings each day, but not during every feeding. In this group of infants, bradycardia was either self-limited, or responded to mild stimulation. To avoid the potential effects of painful stimuli upon heart rate, these infants had not yet been immunized, and males had not yet been circumcised. Institutional Review Board approval was obtained before the launch of this study. The mother of each infant considered for study was asked to sign an informed consent before any data were collected.
Data collection and spectral analysis.
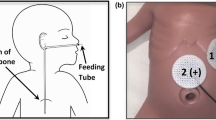
All recordings were performed in the Special Care Nursery, and the infants were fed by trained Neonatal Intensive Care Unit nurses. Between feedings, infants were placed in bassinets, and positioned on their right side, propped by a blanket roll. Infants were wrapped by a single blanket, and loosely covered by another. The infants were under observation by the investigator and a diary was kept of the events during the study.
Recordings were conducted using a Log-a-Rhythm Signal Acquisition Unit (Nian-Crae, Inc. Somerset, NJ), which used conventional electrocardiographic (EKG) monitoring techniques at a sampling rate of 1 KHz. The EKG data were then digitized and RR intervals stored by this unit with a resolution of 4 ms. A tracing of instantaneous heart rate was generated digitally using the stored RR interval data. To provide equally spaced samples, the final sampling rate of the IHR series was 4 Hz. Using IBM compatible software, developed by Nian-Crae, Inc., the EKG data were analyzed to determine the power spectrum of heart rate variability.
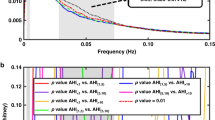
Each infant's heart rate was digitally recorded for a total period of 2 h, spanning both 1 h before feeding and extending to 1 h after feeding. For each infant, multiple 150 s, artifact-free recording segments were used to generate power spectra. These segments were all obtained from approximately 1 h before and 1 h after feeding, at times when the infants were noted to be sleeping quietly. Software, developed by Nian-Crae, Inc., was used to generate the power spectrum for each heart rate recording segment. The area under each power spectrum was then calculated for three regions; 0.003–0.03 Hz (very low frequency = VLF), 0.03–0.39 Hz (low frequency = LF), and 0.40–1.00 Hz (high frequency = HF). The sum of VLF + LF + HF was calculated to determine the total spectral power (TP). Furthermore, to express the relative contributions of LF and HF power, the ratio of LF to HF was calculated (LF/HF).
Statistical analysis.
Mean and standard deviations were calculated for demographic data as well as for the spectral power in each region of the power spectrum, LF/HF ratios, and total power. Two-way analyses of variance were used to compare control and symptomatic groups. All statistical analyses were conducted using Statistics for Windows, version 4.5, by Statsoft, Inc. A p value of less than 0.05 was considered to be statistically significant.
RESULTS
A shown in Table 1, the control and symptomatic groups were similar with respect to both birth weight and gestational age. There were also no significant differences in Apgar scores, male to female ratio, incidence of RDS, age at time of study, or weight at time of study.
The spectral power data obtained 1 h before and 1 h after feeding are shown in Table 2. None of the 22 infants suffered bradycardia during the study period. Infants with a history of feeding bradycardia exhibited significantly higher HF power (1.9 ± 1.6 versus 0.7 ± 0.7 (beats/min) (2), and lower LF/HF ratios (18.3 ± 8.9 versus 35.3 ± 25.7) before feeding, than control infants (p < 0.05). HF power was similar before and after feeding in the symptomatic group (1.9 ± 1.6 versus 1.2 ± 1.3 (beats/min) (2). The two groups exhibited no significant differences in the VLF and LF regions of their power spectra, and no significant differences were identified in TP. After feeding, HF power, and the LF/HF ratio were similar in both the control and symptomatic groups. However, in the control group, infants exhibited significantly lower HF power (0.7 + 0.7 versus 1.0 + 0.6 (beats/min) (2) and higher LF/HF ratios (35.3 ± 25.7 versus 24.5 ± 18.0) before feeding, than after (p < 0.05).
DISCUSSION
Spectral analysis has recently become a useful tool in the study of heart rate variability, and has been used to establish correlations between the fluctuations in instantaneous heart rate and autonomic function. Studies have demonstrated, for example, that life-threatening arrhythmic events are predicted by a reduction in heart rate variability in both adults (23) and infants (2, 6). Analysis of beat-to-beat heart rate variability and of the changes in IHR in response to the Valsalva maneuver, have been used to investigate parasympathetic function in the pediatric population (24).
Autonomic nervous system dysfunction has been hypothesized as a contributor to sudden infant death syndrome (SIDS) (1). Perticone et al. demonstrated a correlation between prolongation of the QT interval, decreased heart rate variability, and subsequent SIDS (2). A decrease in heart rate variability was also identified in infants considered to be at increased risk for SIDS. SIDS research has also generated several reports on the application of spectral analysis to infants; however, the results have been conflicting. Kluge et al. (5) and Schechtman et al. (6) reported that the degree of respiratory sinus arrhythmia, measured by the high frequency region of the power spectrum, is decreased in SIDS victims. The significant overlap between the two groups, however, precluded the use of these data as a predictive tool. A decrease in high frequency variability was also reported by Chauchemez et al. (7). On the other hand, Gordon et al. demonstrated an elevation of low frequency power in SIDS victims, compared with controls (25).
Several studies have explored the use of spectral analysis to assess autonomic development in the pediatric population (12–18). In adults, this technique has been used to study patients with either cardiac or autonomic disorders (26–28). There is only scant data relating autonomic function, swallowing, and heart rate. Gandevia and McCloskey reported their observations on the changes in heart rate that accompany swallowing (24). They also described reflex bradycardia occurring in response to diving, nasopharyngeal stimulation, and ocular pressure. This reflex is modified by respiration and swallowing. Palmer described that vaso-vagal reflexes, initiated by swallowing, can influence cardiac rhythm (29). Dangerous arrhythmias were also reported to result from belching, retching, swallowing, and gastric distention.
Many healthy preterm and full-term infants can experience bradycardia during feeding, despite the absence of gastroesophageal reflux. The nature of the autonomic nervous system's contribution to feeding bradycardia, however, remains unclear. Reflex bradycardia, during swallowing or nasopharyngeal stimulation, is known to be triggered by an increase in parasympathetic activity. This study sought to establish whether differences in baseline autonomic activity, could be responsible for predisposing certain infants to bradycardia during feeding.
The infants' state of arousal, during data collection, was taken into consideration as a potential confounder of our heart rate data. Sleep states in the infant can be divided into six categories: quiet sleep, active sleep, drowsiness, quiet wakefulness, and active wakefulness. In quiet sleep, the infant is fully at rest, with regular respirations and generally absent body movements. In active sleep, on the other hand, there tend to be irregular respirations and a variety of body movements. Because heart rates can differ during times of sleep versus waking, as well as during different sleep states (3, 12, 30), the recording segments analyzed were obtained from periods when the infants were noted, by direct observation, to be sleeping quietly.
One hour before feeding, infants who only suffered from feeding bradycardias exhibited significantly increased power in the high frequency (parasympathetic) region of the power spectrum compared with asymptomatic controls. Furthermore, before feeding, the ratio of LF power to HF power (LF/HF) was significantly lower in infants with feeding bradycardia. This result confirms that the relative contribution made to overall autonomic activity by the parasympathetic nervous system is greater in symptomatic infants. The increase in baseline parasympathetic activity, when compounded by additional vagal stimulation during swallowing, may be the cause of feeding bradycardia in this group of infants. No significant differences were identified in the VLF or HF regions of the power spectrum.
Heart rate variability was also analyzed 1 h after feeding. It is known that in the post-prandial period, the CNS and the intestinal intrinsic nervous system both serve to modulate intestinal motility. An increase in parasympathetic activity leads to an increase in gastrointestinal motility (31). In control infants, the increase in HF power and the drop in the LH/HF ratio, relative to the baseline documented before feeding, may be a reflection of such an increase in parasympathetic activity.
There were no significant differences, after feeding, between VLF, LF, and HF power in the two groups of infants. Thus, in infants experiencing feeding bradycardia, no additional parasympathetic influence was reflected in the heart rate variability power spectra obtained during the post-prandial period. There were also no significant differences identified in total spectral power. It is also possible that an elevation in post-prandial parasympathetic activity may have been present in the bradycardia group, but had subsided by the study period 1 h after feeding. Clinical EKGs were not obtained on our group of infants. EKG data, and assessment of QT intervals, as a further characterization of autonomic stability, would be an interesting addition to future work.
Further work is also needed to determine the underlying physiology responsible for the differences in autonomic activity observed between these two groups of infants. The results of this study indicate that elevations in baseline parasympathetic activity may contribute to the development of feeding bradycardias. A study of how heart rate variability changes during the feeding of these infants may help clarify the etiology of these symptoms. In the future, a better understanding of the physiology responsible for feeding bradycardias, may help guide the development of therapy and monitoring strategies.
Abbreviations
- BW:
-
birth weight
- HF:
-
high frequency (0.4–1.00 Hz)
- IHR:
-
instantaneous heart rate
- LF:
-
low frequency (0.3–0.39 Hz)
- SIDS:
-
sudden infant death syndrome
- TP:
-
total power
- VLF:
-
very low frequency (0.003–0.03 Hz)
References
Matthews TG 1992 The autonomic nervous system - a role in sudden infant death syndrome. Arch Dis Child May 67: 654–656.
Perticone F, Ceravolo R, Maio R, Cosco C 1990 Heart rate variability and sudden infant death syndrome. PACE 13(12 part II): 2096–2099.
Harper RM, Leake B 1978 Polygraphic studies of normal infants and infants at risk for sudden infant death syndrome; heart rate variability as a function of sleep state. Pediatr Res 12: 780–785.
Schechtman VL, Raetz SL, Harper RM 1992 Dynamic analysis of cardiac R-R interval in normal infants and in infants who subsequently succumbed to the sudden infant death syndrome. Pediatr Res 31: 606–612.
Kluge KA, Harper RM, Schetman VL 1988 Spectral analysis assessment of respiratory sinus rhythm in normal infants and infants of SIDS. Pediatr Res 24: 677–682.
Schechtman VL, Harper RM, Kluge KA, Wilson AJ, Hoffman HJ, Southall DP 1988 Cardiac and respiratory patterns in normal infants and victims of sudden infant death syndrome. Sleep 11: 413–424.
Chauchemez B, Peirano P, Samson-Dolfus D 1989 Decreased vagal tone in SIDS victims. IEEE Eng Med Biol Society, 11th Annual International Conference, 321–322.
Harper RM, Leake B, Hodgeman JE, Hoppenbrowers T 1982 Developmental patterns of heart rate variability during sleep and waking in normal infants and infants at risk for the sudden infant death syndrome. Sleep 5: 28–38.
Leistner HL, Haddad GG, Epstein RA, Lai TL, Epstein MAF, Mellins RB 1980 Heart rate variability during sleep in aborted sudden infant death syndrome. J Pediatr 97: 51–55.
Schetman VL, Harper RM, Kluge KA, Wilson AJ, Hoffman HJ, Southall DP 1989 Heart rate variation in normal infants and victims of the sudden infant death syndrome. Early Hum Dev 19: 167–181.
Kochiadalis GE, Kanoupakis EM, Igoumendis NE, Marketou ME, Solomou MC, Vardas PE 1998 Spectral analysis of heart rate variability during tilt-table testing in patients with vasovagal syncope. Int J Cardiol 1:64(2): 185–194.
Nungent ST, Finley JP 1989 Heart rate variability in infants as a function of sleep state. IEEE Eng Med Biol Society, 11th Annual International Conference, 319–320.
Chatow U, Davidson S, Reichman BL, Akselrod S 1995 Development and maturation of the autonomic nervous system in premature and full-term infants using spectral analysis of heart rate fluctuation. Pediatr Res 37: 294–301.
Baldzer K, Dykes FD, Jones SA, Brogan M, Carrigan TA, Giddens DP 1989 Heart rate variability analysis in full term infants: spectral indices for the study of neonatal cardiorespiratory control. Pediatr Res 26: 188–195.
Gordon D, Herrera VL, McAlpine L, Cohen RJ, Akselrod S, Lang P, Norwood WI 1988 Heart rate spectral analysis: a noninvasive probe of cardiovascular regulation in critically ill children with heart disease. Pediatr Cardiol 9: 69–77.
Karin J, Hirsch M, Akselrod S 1993 An estimate of fetal autonomic state by spectral analysis of fetal heart rate fluctuations. Pediatr Res 34: 134–138.
Finley JP, Nungent ST, Hellenbrand W 1987 Heart rate variability in children, spectral analysis of developmental changes between 5 and 25 years. Can J Physiol Pharmacol 65: 2048–2052.
Oberlander TF, Grunau ER, Pitfield S, Whitfield MF, Saul JP 1999 The developmental character of autonomic responses to an acute noxios event in 4- and 8-month-old healthy infants. Pediatr Res 45: 519–525.
England SJ, Miller MJ, Martin RJ 1991 Unique issues in neonatal respiratory control. In: Dempsey JA, Pack AI (eds) Regulation of Breathing, 2nd Ed. Marcel Dekker, Inc, New York, 797–827.
Akselrod S, Gordon D, Ubel FA, Shannon DC, Barger AC, Cohen RJ 1981 Power spectrum analysis of heart rate fluctuation: a quantitative probe of beat-to-beat cardiovascular control. Science 213: 220–222.
Pomeranz B, Macaulay RJB, Caudil MA, Kutz I, Adam D, Gordon D 1985 Assessment of autonomic function in humans by heart rate spectral analysis. Am J Physiol 248: H151–H153.
Akselrod S, Gordon D, Madwed JB 1985 Hemodynamic regulation investigated by spectral analysis. Am J Physiol 249: H867–H875.
Malik M, Camm AJ 1990 Heart rate variability. Clin Cardiol 13: 570–576.
Gandevia SC, McCloskey DI 1978 Reflex bradycardia occurring in response to diving, nasopharyngeal stimulation, ocular pressure, and its modification by respiration and swallowing. Am J Physiol 276: 383–394.
Gordon D, Cohen RJ, Kelly D, Akselrod S, Shannon DC 1984 Sudden infant death syndrome: abnormalities in short term fluctuations in heart rate and respiratory activity. Pediatr Res 18: 921–926.
Akselrod S 1988 Spectral analysis of fluctuations in cardiovascular parameters: a quantitative tool for the investigation of autonomic control. Trends Pharmacol Sci 9: 6–9.
Appel ML, Berger RD, Saul JP, Smith JM, Cohen RJ 1989 Beat to beat variability in cardiovascular variables: noise or music?. J Am Coll Cardiol 14: 1139–1148.
Kamath MV, Fallen EL 1993 Power spectral analysis of heart rate variability: a noninvasive signature of cardiac autonomic function. Crit Rev Biomed Eng 21: 245–311.
Palmer ED 1976 The abnormal upper gastrointestinal vasovagal reflexes that affect the heart. Am J Gastroenterol 66: 513–522.
Finley JP, Nugent ST 1995 Heart rate variability in infants, children and young adults. J Auton Nerv Syst 55: 103–108.
Spiro HM 1993 Motility of the small intestine. In: Clinical Gastroenterology, 4th Ed. McGraw-Hill, Inc, New York, 352
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Veerappan, S., Rosen, H., Craelius, W. et al. Spectral Analysis of Heart Rate Variability in Premature Infants with Feeding Bradycardia. Pediatr Res 47, 659–662 (2000). https://doi.org/10.1203/00006450-200005000-00017
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200005000-00017
This article is cited by
-
Heart and respiration rate changes in the neonate during electroencephalographic seizure
Medical and Biological Engineering and Computing (2006)
-
Birth prematurity determines prolonged autonomic nervous system immaturity
Clinical Autonomic Research (2004)