Abstract
The spectrum of clinical presentation of fatty acid oxidation defects (FAOD) continues to expand. One FAOD, L-3-hydroxyacyl-CoA dehydrogenase (LCHAD) deficiency has been associated with liver disease in pregnancies involving a heterozygous mother carrying an affected fetus. Hepatic carnitine palmitoyltransferase (CPT I) deficiency typically presents as a Reye-like syndrome in children between 8 and 18 mo of age. We have investigated a family in which the mother developed liver disease consistent with acute fatty liver of pregnancy (AFLP) and hyperemesis gravidarum in her two successive pregnancies. Neither child nor their mother was found to carry the common LCHAD G1528C mutation. Both children were subsequently shown to have absent activity of CPT I. This is the first report of CPT I deficiency presenting as maternal illness in pregnancy.
Similar content being viewed by others
Main
FAOD are an increasingly recognized group of disorders with diverse clinical presentations (1). One disorder, CPT I deficiency, was first reported in 1981 (2). It is characterized by fasting hypoketotic hypoglycemia, recurrent encephalopathy, and signs of liver disease, including features of Reye Syndrome (2, 3). Early recognition of this and other FAOD is crucial to allow for avoidance of prolonged fasting, causing potentially life threatening hypoglycemia and neurologic sequelae. Recently, the association between LCHAD deficiency and trifunctional protein deficiency (TFP) in infants and unexpected and life threatening maternal liver disease in their mothers late in pregnancy has been described (4, 5). One common mutation, the G1528C in exon 15 of the TFP - subunit, causing a glutamic acid to glutamine substitution (E474Q), has been described in children with LCHAD deficiency and maternal AFLP (6, 7). Additional LCHAD mutations have recently been recognized to be associated with maternal illness in pregnancy (8). We now report two infant siblings with CPT I deficiency whose mother presented with suspected AFLP in the first pregnancy and hyperemesis gravidarum in the subsequent pregnancy.
METHOD
Case report.
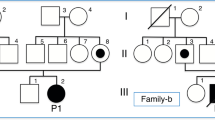
A 19-y-old Inuit female was referred to our tertiary care facility from her remote community in the Canadian Arctic at 33 wk gestation with nausea, vomiting, hypertension, weight loss, and right upper quadrant pain. The father is a healthy 24-y-old Inuit man with no known consanguinity to the mother. Family history is noncontributory. Physical examination in the mother revealed no obvious icterus, and no hepatosplenomegaly or right upper quadrant tenderness. The mother's liver function studies on admission revealed direct hyperbilirubinemia (total 41 μmol/L [normal 3–18]; direct 35 μmol/L (0–7), elevated liver enzymes (AST 124 U/L [normal 0–32]; ALT 110 U/L [normal 0–25]; LDH 708 U/L [normal 63–200]; gamma GT 64 U/L [normal 5–29]), with normal ammonia, PT/PTT, total protein, albumin, serum amylase, platelets [range 212–269 × 109/L], and renal function. Serum creatinine and uric acid levels were at the upper limits of normal at 108 U/L [normal 70–100] and 304 U/L [normal 30–330], respectively. Viral serology was normal. Other investigations included abdominal ultrasound that revealed a “sludge-filled” gallbladder but no distinct calculi and a possible fatty liver. The working diagnosis was acute fatty liver of pregnancy based on a compatible clinical presentation of malaise, nausea, vomiting, abdominal pain in the 3rd trimester, elevated aminotransferases, ultrasound findings, and the exclusion of viral or toxic hepatitis or biliary tract disease (5).
Because of hypertension, persistent vomiting, and the appearance of a prolonged PT (16.3 s; control 12.2 s), labor was induced. A healthy infant girl (patient 1) was born at 34 wk gestation. Growth parameters at birth were weight 2217 g, length 47 cm, head circumference 31 cm, all at the 50th percentile for gestational age. No perinatal problems were encountered except for mild hyperbilirubinemia, which was treated with phototherapy. Mother's illness resolved after delivery with normalization of the biochemical findings, but investigations for a possible fatty acid oxidation defect were initiated in the infant and mother because of the maternal history. The infant was bottle fed initially with a standard cow's milk commercial formula with iron, but was switched at 1 y of age to a commercial cow's milk therapeutic formula Portagen (Mead Johnson) containing approximately 2.7 g medium chain triglycerides (MCT)/100 mL formula, with the total fat content in the formula being 3.2 g/100 mL. She has remained well without any known episodes of hypoglycemia, liver dysfunction, or multisystem involvement.
In the subsequent pregnancy mother remained in her home community and had no documented liver disease. She did, however, suffer from hyperemesis gravidarum requiring i.v. fluids at her local nursing station. A healthy male infant (patient 2), whose growth parameters were appropriate for gestational age, was born at 35 wk gestation in the nursing station. Asymptomatic hypoglycemia (plasma glucose 1.1 mmol/L) was documented at 1 h of age, and he was transferred to the local hospital for further care. No medical problems were subsequently recorded, but at 6 wk of age, he was transferred to our intensive care facility with a 2-d history of an upper respiratory infection and apnea. Bronchopneumonia was diagnosed and he required intubation and mechanical ventilation for 3 d. Plasma glucose was 3.3 mmol/L on admission. Because the diagnosis of CPT I deficiency had been confirmed by this time in his sister, we initiated metabolic studies on his blood, urine, and skin fibroblasts. He was placed on the same formula enriched with MCT as his sister. At the time of their last assessment in July 1998, both children, 2 y 5 mo and 1 y 3 mo of age, were well with normal growth and development to date.
Laboratory investigations.
Organic acids in urine were determined by gas chromatography/mass spectrometry (9). Quantitative analysis of plasma acylcarnitine was performed using an established stable isotope dilution gas chromatography/mass spectrometry method (10). The accumulation of β oxidation intermediates was studied by in vitro probing of cultured skin fibroblasts with palmitate or linoleate and subsequent analysis of the resultant acylcarnitines by tandem mass spectrometry as previously described (11, 12). Palmitate oxidation was studied in cultured fibroblasts as described (13). Palmitate oxidation in whole blood samples was performed by a modification of the procedure for cultured fibroblasts (13a). The activities of the acyl-CoA dehydrogenases, enoyl-CoA hydratases (short and long chain), L-3 hydroxyacyl-CoA dehydrogenases (short and long chain), 3 ketothiolases (short, medium, and long chain), CPT I, CPT II, and mitochondrial carnitine/acylcarnitine translocase were assayed in cultured fibroblasts from the first baby according to established protocols (14). CPT I and CPT II activities were assayed in the cultured fibroblasts of the second child. Testing for the common missense G1528C mutation in the LCHAD gene was performed in genomic DNA using established protocols (7).
RESULTS
Plasma amino acids, urine organic acids, and whole blood acylcarnitine profiles were normal in both children. Total and free serum carnitine in patient 1 was 49.2 μmol (normal 24–66) and 41.4 μmol (normal 19–50), respectively. In patient 2 total and free serum carnitine were 28.7 μmol (24–66) and 23.0 μmol (19–50), respectively. In vitro probing of cultured fibroblasts of patient 1 with palmitate and linoleate revealed normal acylcarnitine intermediates. Fibroblast palmitate oxidation was 34% and 14% of control activity in patients 1 and 2, respectively. Palmitate oxidation in whole blood was decreased in both children to 12% and 19% of control activity, respectively. Whole blood palmitate oxidation in the mother was 50% of control activity. Enzymatic analysis in cultured fibroblasts of patient 1 revealed complete absence of CPT I activity but normal activities of the enzymes involved in fatty acid oxidation listed in Methods. Complete CPT I deficiency was also confirmed in the cultured fibroblasts of patient 2. CPT II activity in patient 2 was appreciably lower than CPT II activity in his sib and normal controls. The CPT results are summarized in Table 1, and neither patient nor their mother had the common LCHAD G1528C mutation.
DISCUSSION
We believe that the lower β oxidation of palmitate in cultured fibroblasts and whole blood in these siblings is due to complete deficiency of CPT I. In patient 1 the activities of the other enzymes studied were well within the normal range. The activity of CPT II in patient 2 is indeed lower than CPT II activity in his sister and normal controls, and is in the range of what is found in heterozygotes. This could imply true heterozygosity for CPT II deficiency or could be artifactual due to poor growth of cells in patient 2.
This case report illustrates that fatty acid oxidation disorders other than LCHAD deficiency can lead to maternal complications in pregnancy, and that there is a wider range of clinical presentations of CPT I deficiency than has previously been recognized. CPT I deficiency usually presents after prolonged fasting or during intercurrent illnesses between 8 and 18 mo of age with fasting hypoketotic hypoglycemia, seizures, hepatomegaly and liver dysfunction (2, 3). Classically hypoketotic hypoglycemia without dicarboxylic aciduria with a high or high-normal plasma carnitine level and a normal acylcarnitine profile distinguishes this disorder from all other fatty acid oxidation defects (15). Although one infant with CPT I deficiency has been previously reported as presenting in the neonatal period, early presentation is most unusual (11).
In our patients, maternal illness was present in both affected pregnancies and led to further investigations in the offspring. The first pregnancy was complicated by suspected acute fatty liver of pregnancy, and the second by hyperemesis gravidarum. Both of these maternal complications have not previously been associated with CPT I deficiency in the offspring. It is now well recognized that a woman carrying a fetus with LCHAD or TFP deficiency is at risk for AFLP and that recurrences have been reported in subsequent pregnancies. This is, however, the first report of CPT I deficiency presenting in pregnancy with maternal illness and expands the list of FAOD that may present in pregnancy. Urine organic acid screening, acylcarnitine profiles, and serum carnitine are most often normal in CPT I deficiency. Thus we propose that other general screening tests for FAOD, including acylcarnitine analysis in blood by tandem mass spectrometry and palmitate oxidation in whole blood or intact cells (lymphocytes/fibroblasts), should be pursued in babies and their mothers with unexplained AFLP, HELLP (hemolysis, elevated liver enzymes, low platelets) syndrome or hyperemesis gravidarum. Definitive diagnosis of CPT I deficiency requires enzymatic confirmation as performed here. DNA analysis to determine the mutations causing CPT I and CPT II deficiency is in progress.
It has been postulated that the development of AFLP results from exceeding the capacity for β oxidation in maternal liver mitochondria during the third trimester. Decreased mitochondrial β oxidation of fatty acids has been described in pregnancy and it has been shown in mice that maternal serum levels of FFA increase throughout pregnancy peaking toward the end of the third trimester (16). Thus any underlying genetic error that decreases the metabolism of long chain fats in the fetus and produces abnormal fatty acid metabolites that enter the maternal circulation may be toxic to the maternal liver mitochondrial β oxidation and lead to acute fatty liver of pregnancy. This case report illustrates that CPT I deficiency in the fetus may also lead to hepatocellular damage or hyperemesis gravidarum in the mother and that the spectrum of disorders of the fetus causing maternal liver disease in pregnancy is indeed wider than has previously been appreciated.
Abbreviations
- FAOD:
-
fatty acid oxidation defects
- CPT:
-
carnitine palmitoyltransferase
- LCHAD:
-
L-3-hydroxyacyl-CoA dehydrogenase
- TFP:
-
trifunctional protein
- AFLP:
-
acute fatty liver of pregnancy
- HELLP:
-
hemolysis, elevated liver enzymes low platelets
References
Hale DE, Bennet MJ 1992 Fatty acid oxidation disorders: A new class of metabolic diseases. J Pediatr 121: 1–11.
Bourgneres P-F, Saudubray J-M, Marsac C, Bernard O, Odievre M, Girard J 1981 Fasting hypoglycemia resulting from carnitine palmitoyl transferase deficiency. J Pediatr 98: 742–746.
Haworth JC, Demaugre F, Booth FA, Dilling LA, Moroz SP, Seshia SS, Seargeant LE, Coates PM 1992 Atypical features of the hepatic form of carnitine palmitoyltransferase deficiency in a Hutterite family. J Pediatr 121: 553–557.
Wilcken B, Leung K-C, Hammond J, Kamath R, Leonard JV 1993 Pregnancy and fetal long-chain 3-hydroxyacyl coenzyme A dehydrogenase deficiency. Lancet 341: 407–408.
Treem WR, Shoup ME, Hale DE, Bennett MJ, Rinaldo P, Millington DS, Stanley CA, Riely CA, Hyams JS 1996 Acute fatty liver of pregnancy, hemolysis, elevated liver enzymes, and low platelets syndrome, and long chain 3-hydroxyacyl-coenzyme A dehydrogenase deficiency. Am J Gastroenterol 91: 2293–2300.
Sims HF, Brackett JC, Powell CK, Treem WR, Hale DE, Bennett MJ, Gibson B, Shapiro S, Strauss AW 1995 The molecular basis of pediatric long chain 3-hydroxyacyl-CoA dehydrogenase deficiency associated with maternal acute fatty liver of pregnancy. Proc Natl Acad Sci USA 92: 841–845.
Ijlst L, Ruiter JPN, Hoovers JMN, Jakobs ME, Wanders RJA 1996 Common missense mutation G1528C in long-chain 3-hydroxyacyl-CoA dehydrogenase deficiency characterization and expression of the mutant protein, mutation analysis on genomic DNA and chromosomal localization of the mitochondrial trifunctional protein-subunit gene. J Clin Invest 98: 1028–1033.
Isaacs JD JR, Sims HF, Powell CK, Bennet MJ, Hale DE, Treem WR, Strauss AW 1996 Maternal acute fatty liver of pregnancy associated with fetal trifunctional protein deficiency: molecular characterization of a novel mutant allele. Pediatr Res 40: 393–398.
Goodman SI, Markey SP, eds. 1981 Diagnosis of organic acidemias by gas chromatography - mass spectrometry. Alan R Liss, New York, 105–114.
Costa CG, Struys EA, Bootsma A, ten Brink HJ, Dorland L, Tavares de Almeida I, Duran M, Jakobs C 1997 Quantitative analysis of plasma acylcarnitines using gas chromatography chemical ionization mass fragmentography. J Lipid Res 38: 173–181.
Roe CR, Coates PM 1995 Mitochondrial fatty acid oxidation disorders. In: Scriver CR, Beaudet AL, Sly WS, Valle D (eds) The Metabolic and Molecular Bases of Inherited Disease, 7th Ed. McGraw-Hill, New York, 1501–1533.
Nada MA, Rhead WJ, Sprecher H, Schulz H, Roe CR 1995 Evidence for intermediate channeling in mitochondrial β-oxidation. J Biol Chem 270: 530–535.
Moon A, Rhead WJ 1987 Complementation analysis of fatty acid oxidation disorders. J Clin Invest 79: 59–64.
Seargeant LE, Balachandra K, Mallory C, Dilling LA, Greenberg CR 1999 A simple screening test for fatty acid oxidation defects using whole-blood palmitate oxidation. J Inherit Metab Dis 22: 740–746.
Wanders RJA, Ijlst L, Poggi F, Bonnefont JP, Munnich A, Brivet M, Rabjer D, Saudubray JM 1992 Human trifunctional protein deficiency: a new disorder of mitochondrial fatty acid β-oxidation. Biochem Biophys Res Commun 188: 1139–1145.
Stanley CA, Sunaryo F, Hale DE, Bonnefont J-P, Demaugre F, Saudubray JM 1992 Elevated plasma carnitine in the hepatic form of carnitine palmitoyltransferase-1 deficiency. J Inherit Metab Dis 15: 785–789.
Grimbert S, Fromenty B, Fisch C, Letteron P, Berson A, Durand-Schneider AM, Feldmann G, Pessayre D 1993 Decreased mitochondrial oxidation of fatty acids in pregnant mice: possible relevance to the development of acute fatty liver of pregnancy. Hepatology 17: 628–637.
Acknowledgements
The authors thank Louise A. Dilling, Metabolic Coordinator, for dedicated assistance and Dr. James C. Haworth for helpful comments.
Author information
Authors and Affiliations
Additional information
Supported by the Children's Hospital Foundation of Manitoba.
Rights and permissions
About this article
Cite this article
Innes, A., Seargeant, L., Balachandra, K. et al. Hepatic Carnitine Palmitoyltransferase I Deficiency Presenting as Maternal Illness in Pregnancy. Pediatr Res 47, 43 (2000). https://doi.org/10.1203/00006450-200001000-00010
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200001000-00010
This article is cited by
-
Comparison of maternal and neonatal outcomes between acute fatty liver of pregnancy and hemolysis, elevated liver enzymes and low platelets syndrome: a retrospective cohort study
BMC Pregnancy and Childbirth (2021)
-
Analysis of clinical characteristics and genetic testing in patients with acute fatty liver of pregnancy: a retrospective study
BMC Pregnancy and Childbirth (2021)
-
Disorders of mitochondrial long-chain fatty acid oxidation and the carnitine shuttle
Reviews in Endocrine and Metabolic Disorders (2018)
-
Impact of pregnancy on inborn errors of metabolism
Reviews in Endocrine and Metabolic Disorders (2018)
-
Acute Fatty Liver Disease of Pregnancy: Updates in Pathogenesis, Diagnosis, and Management
American Journal of Gastroenterology (2017)