Abstract
Monitoring oxygenation in peripheral tissues of preterm babies may be useful in understanding the redistribution of blood flow during hypotension. Hemoglobin flow and venous saturation were measured in the forearm using near infrared spectroscopy with venous occlusion and were used to calculate fractional oxygen extraction, oxygen delivery, and oxygen consumption. Thirty ventilated preterm babies (median birth weight 976 g) were studied; 15 were hypotensive and 15 normotensive. Treatment for hypotension was dopamine alone (median dose 5 µg/kg/min) in eight cases, 4.5% human albumin solution (20 mL/kg) with dopamine in five cases, and only a blood transfusion (20 mL packed cells/kg) in two cases. There was a weak correlation between hemoglobin flow and mean arterial blood pressure (r = 0.40, p = 0.03). In hypotensive compared with normotensive babies, there was a significantly lower median hemoglobin flow (10.2 versus 20.2 µmol/100 mL/min, p = 0.0006), forearm oxygen delivery (37.8 versus 75.2 µmol/100 mL/min, p = 0.0008), and oxygen consumption (11.0 versus 23.9 µmol/100 mL/min, p = 0.006), but the fractional oxygen extraction (0.327 versus 0.306, p = 0.48) and the blood lactate concentration (1.22 versus 1.20 mmol/L, p = 0.44) were similar. Following treatment of hypotension, oxygen delivery (p = 0.02) and oxygen consumption (p = 0.04) increased to 64.2 and 21.7 µmol/100 mL/min, respectively, but fractional oxygen extraction (p = 0.81) and blood lactate concentration (p = 0.94) after treatment were unchanged. VO2 was variable in the forearm of human infants. It reduced when DO2 was low, and there was no evidence of tissue injury or switch to anaerobic metabolism. Measurements of peripheral tissue oxygenation seem to be of some value in understanding the pathophysiologic changes that occur with hypotension.
Similar content being viewed by others
Main
Hypotension in preterm babies may be the result of cardiac dysfunction(1), ductal and intra-atrial shunts(2–4), and hypovolemia. It may result in a redistribution of blood flow to favor the cardiac and the cerebral circulations. A low blood pressure has also been associated with a poor outcome in terms of mortality and morbidity(5–9). The rationale for the therapeutic support of blood pressure is based on the assumption that a low blood pressure represents low systemic blood flow(10,11) and therefore impaired oxygen delivery to the tissues, but because it is tissue oxygen delivery that is critical, systemic blood pressure may not be the most biologically relevant variable to monitor. Because it is a function both of blood flow and systemic vascular resistance, it is possible to have a low blood pressure with normal blood flow or a normal blood pressure with low blood flow, depending on the systemic vascular resistance. Low systemic blood flow is associated with changes in distribution of flow so that perfusion of vital organs such as the brain and the heart is maintained at the expense of flow to peripheral tissues such as skin. Monitoring the oxygen delivery to the peripheral tissues and their oxygen consumption is therefore likely to yield interesting information of potential clinical relevance.
Tissue oxygeneration represents a balance between oxygen delivery (DO2) and oxygen consumption (VO2). Normally, variations in the level of DO2 do not alter VO2, which is delivery independent. However, when DO2 falls beyond a critical point, VO2 becomes delivery dependent, and a further reduction in DO2 results in decreased aerobic metabolism with the production of lactic acid and possible cell injury. This model of the relationship between VO2 and DO2 has been demonstrated in adult humans(12–18) and animals(19–23) but not in preterm human infants. This model assumes a constant VO2, which may not be the case in the peripheral circulation of critically ill newborn infants.
The balance between DO2 and VO2 is represented by the fractional oxygen extraction (FOE). Equation 1 DO2 can be calculated from the hemoglobin flow (Hbflow) and the arterial oxygen saturation (SaO2): Equation 2 Each mol of hemoglobin carries 4 mol of oxygen. Because the amount of dissolved oxygen is insignificant in comparison with that carried by hemoglobin, it can be ignored.
VO2 can be calculated from the Hbflow, SaO2, and the venous oxygen saturation (SvO2): Equation 3 Combining equations 2 and 3 with equation 1, Equation 4 measurements of SaO2 are possible using pulse oximetry. Measurements of peripheral venous saturation and Hbflow in the forearm of neonates can be made using techniques involving near infrared spectroscopy (NIRS) with venous occlusion(24,25). These measurements are simple, involving minimal disturbance of the subject, and repeated measurements are possible(24,25). Measurement of forearm Hbflow, SvO2, and SaO2 allow FOE, DO2, and VO2 in peripheral tissues to be calculated.
If VO2 remains constant, a decrease in DO2 would be expected to result in an increase in FOE. This is a reasonable assumption because we have shown that babies with a low hemoglobin concentration maintain VO2 in peripheral tissues but that the FOE is increased(26). The point at which FOE increases might then identify when delivery to the tissues has become critical and provide an indication for appropriate therapeutic intervention.
We therefore hypothesized that a low blood pressure and low DO2 would be associated with an increased FOE. We also hypothesized that there is a critical value of DO2 at which VO2 becomes delivery dependent. Our third hypothesis followed from the first two: treatment to raise systemic blood pressure during hypotension should result in improved peripheral oxygenation.
METHODS
Subjects. Thirty babies were studied, and their details are given in Table 1. All babies were ventilated preterm babies with birth weights less than 1500 g. Measurements of arterial blood gases, blood lactate, and hemoglobin concentrations were made at the time of the initial NIRS measurements. All had invasive blood pressure monitoring and were not being treated with inotropes at the time of the initial measurement of peripheral Hbflow and venous saturation. The core temperature (rectal) was recorded using a mercury thermometer at least four times hourly and more often if there was concern about the baby by the clinical staff. The skin temperature was measured continuously using a probe (Athena, S&W Medico Teknik, Denmark) on the baby's abdomen positioned over the liver and was recorded at the same time as the rectal temperature. The temperature measured with this probe was also used to control the incubator temperature. No other measurements of peripheral temperature were made.
Two groups of babies were studied. Babies in the first group were normotensive with mean arterial blood pressures above the 10th percentile(6) at the time of the measurement. These babies were studied on one occasion only.
Babies in the second group were all hypotensive at the time of the initial measurement, with blood pressures below the 10th percentile for birth weight and postnatal age(6). This limit was used by clinicians responsible for the care of the baby as the indication for starting treatment for hypotension. A measurement was made when the blood pressure was low and a clinical decision had been made to initiate treatment for hypotension (but before treatment was given). Another set of measurements of peripheral SvO2, SaO2, and Hbflow was made when the blood pressure had become normal (>10th percentile) after the therapeutic intervention. This second measurement was made a median of 3 h after the first (range 1-18 h).
Hypotensive babies received different therapies for their low blood pressure depending on the clinical situation. Eight babies received a continuous dopamine infusion at a median dose of 5 µg/kg/min (range 5-10 µg/kg/min). Five babies received a bolus of 20 mL/kg, 4.5% human albumin solution over 30 min followed by a continuous dopamine infusion, median dose 7.5 µg/kg/min (range 5-10 µg/kg/min). Two babies received only a blood transfusion in the form of 20 mL/kg of packed red blood cells. All the treatments for hypotension succeeded in raising the blood pressure to above the 10th percentile, but the infusions of human albumin solution only produced a transient improvement, and some of the babies receiving dopamine required serial increases in dose to achieve a normal blood pressure.
Outcome was assessed as 1) survival to discharge from the neonatal unit or 2) periventricular hemorrhage (PVH), defined as intraventricular hemorrhage with ventricular dilatation or parenchymal hemorrhage.
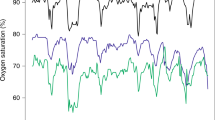
Near infrared spectroscopy: SvO2 measurements. Measurements were made using the Hamamatsu NIRO 500 (Hamamatsu UK Ltd.) and a pulse oximeter (Datex, Finland) in beat to beat mode. SvO2 was measured using a technique that has been described elsewhere in detail(24,26). The monitoring optodes were positioned on the upper forearm, and the interoptode distance was measured using calipers (usually 1.5-2.5 cm). A brief venous occlusion was made with a blood pressure cuff around the upper arm manually inflated to the monitored diastolic pressure(24). SvO2 was measured five times during a 2-min period for each FOE measurement, and the mean value was used. Measurements were made when babies were quiet and at rest. The pulse oximeter optodes were positioned on the same limb. Arterial saturation was recorded every 0.5 s, and the mean arterial saturation at the time of each measurement of venous saturation was used to calculate FOE. Arterial saturations were maintained in the range 88-94% for babies less than 32 wk and greater than 92% for babies more than 32 wk(27).
NIRS hemoglobin flow measurements. NIRS measures changes in total tissue hemoglobin concentration (ΔHbT). Measurements of forearm Hbflow were also made from the NIRS data using a method adapted from that described and validated by de Blasi et al.(25) in adult patients. The method assumes that in a steady state arterial and venous flow are equal. During the initial part of a venous occlusion, hemoglobin accumulates in the tissues owing to cessation of venous flow, and the rate of Hbflow is considered to be equal to the rate of tissue hemoglobin accumulation during the initial part of the occlusion. We measured Hbflow (µmol/100 mL/min) from the slope of a line through the ΔHbT values during the first 2 s of occlusion using a least squares method. The differential path length factor used was 3.59, which is that determined for the adult forearm(28) as path length measurements for the neonatal forearm are not available. The tissue density of neonatal forearm is also not known, and results are therefore presented as µmol/100 mL of tissue/min. Measurements took approximately 10 min to complete.
Forearm arterial resistance. Forearm arterial resistance could also be calculated as = (mean arterial blood pressure - venous pressure)/forearm blood flow. Because blood flow = (Hbflow/Hb), forearm arterial resistance (mm Hg/ml/min) can be calculated as vascular resistance = (blood pressure difference × Hb)/Hbflow. Because the central venous pressure was not measured routinely in the babies studied, this was simplified to vascular resistance = (mean arterial blood pressure × Hb)/Hbflow.
Statistics. Data were analyzed using SPSS for Windows (version 4). The venous saturation and blood flow for each baby was determined as the mean value of five venous occlusions. Data in the two groups of babies were compared using Mann Whitney U tests. Data in the three outcome groups were compared using analysis of variance and Mann Whitney U tests. The relationship between variables was assessed using simple linear regression. Changes within the hypotensive group were assessed using Wilcoxon Rank Sum tests.
Ethical approval for the study was obtained from the local ethics committee, and written parental consent was obtained.
RESULTS
The two groups of babies studied are summarized in Table 1. There were no significant differences between the groups in terms of gestational age or fraction of inspired oxygen (FiO2), but babies who were hypotensive tended to be smaller and were slightly older.
Compared with the normotensive group, the hypotensive infants had significantly lower median Hbflow (p = 0.0006) and forearm DO2 (p = 0.0008) and VO2 (p = 0.006) (see Table 2). Values for these variables in the hypotensive group were only half those of the normotensive group. The FOE of hypotensive babies was not significantly different from that of the normotensive babies (p = 0.48) (see Table 2). The blood lactate concentrations in the normotensive group and in the hypotensive group were not significantly different (p = 0.44) (see Table 2). The median core temperatures of the two groups were similar (p = 0.9), but the median skin temperature (IQR) of the hypotensive group was 0.3°C lower (p = 0.05) than that of the normotensive group (see Table 1). There was no difference in the forearm arterial resistance of the two groups of babies (see Table 2) (p = 0.37).
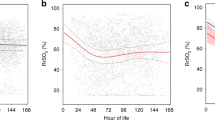
After therapies intended to correct hypotension, there was a significant increase in median Hbflow (IQR) from 10.2 (7.4-16.0) µmol/100 mL/min to 16.6 (15.2-21.6) µmol/100 mL/min (p = 0.02). The median (IQR) FOE after treatment was 0.325 (0.253-0.383), which was not significantly different from the pretreatment value of 0.327 (0.277-0.366) (p = 0.81). After treatment for hypotension, the median (IQR) DO2 increased to 64.2 (57.1-83.4) µmol/100 mL/min (p = 0.01), and the median (IQR) VO2 increased to 21.7 (15.9-26.1) µmol/100 mL/min (p = 0.02) (see Fig. 1). Median (IQR) blood lactate concentration after treatment was 1.22 (0.75-1.75) mmol/L, which was not significantly different from the pretreatment value (p = 0.94).
The median (IQR) forearm arterial resistance after all treatments for hypotension was 4.6 (4.0 to 5.9) mm Hg/ml/min, and this was not significantly different from the pretreatment value (p = 0.51). The mean change (95% CI) was -0.95 (-8.1 to 1.4) mm Hg/ml/min. In those babies who received dopamine, there was also no significant change in vascular resistance [mean change (95% CI) -0.54 (-5.5 to 1.04) mm Hg/ml/min (p = 0.66)].
Relationship between variables. There was a significant correlation between Hbflow and mean arterial blood pressure (r = 0.40, n = 30, p = 0.03) in both groups combined (see Fig. 2) but not in the hypotensive group (n = 15, r = 0.04, p = 0.89) or in the normotensive group (r = -0.05, n = 15, p = 0.87). DO2 correlated with the mean blood pressure (r = 0.38, n = 30, p = 0.04), but VO2 did not (r = 0.27, n = 30, p = 0.14). There was no relationship between peripheral VO2 and gestational age (r = -0.16, n = 30, p = 0.4), birth weight (r = -0.03, n = 30, p = 0.88), postnatal age (r = -0.13, n = 30, p = 0.49, or blood lactate concentration (r = -0.03, n = 27, p = 0.87). There was no correlation between DO2 and blood lactate concentration (r = 0.05, n = 27, p = 0.79).
Outcome. In the hypotensive group, 8 babies survived without any PVH, 2 had PVH, and 5 died. In the normotensive group, 10 babies survived without any PVH, 2 had PVH, and 3 died. No infants had periventricular leukomalacia. The measured variables in each of these outcome groups are summarized in Table 3. Comparisons were made using analysis of variance. VO2, DO2, and Hbflow were not significantly different in babies with PVH and those who died when compared with babies with a normal outcome. Blood lactate concentration measured at the time of the NIRS measurements, however, was significantly higher in babies with PVH (p = 0.01) but not those who died (p = 0.054) when compared with normal survivors. Blood pressure at the time of the NIRS measurements was not significantly lower in babies who died when compared with normal survivors (p = 0.07) or in those with PVH (p = 0.80).
Variability of SvO2 and Hbflow measurements. The variability or peripheral SvO2 and Hbflow measurements was assessed by analyzing the variation in five measurements made from individual venous occlusions in 20 consecutive babies. The mean (SD) value for SvO2 was 61.4% (3.36%), giving an intersubject coefficient of variation of 5.5%. The mean (SD) value for hemoglobin flow measurements was 12.1 (1.98) µmol/100 mL/min, giving an intersubject coefficient of variation of 16.3%.
The variation within an individual was assessed in babies who had repeated measurements of SvO2 and Hbflow. Twenty babies were measured on more than one occasion at time intervals of between 1 and 24 h. The coefficient of variation was assessed for each individual. The mean intraindividual coefficient of variation (range) for SvO2 was 5.6% (3.1-10.1%) and for Hbflow was 17.2% (7.4-31.0%).
In the present study, the intraindividual coefficients of variation were assessed from the five venous occlusions that were used to calculate the result for each patient. The mean coefficient of variation (range) for SvO2 was 6.4% (1.8-12.9%) for hypotensive patients and 3.9% (0.5-9.2%) for normotensive babies. For Hbflow, the mean coefficient of variation (range) was 22.2% (11.1-42.3%) for hypotensive patients and 13.6% (7.8-27.8%) for normotensive babies.
DISCUSSION
This study has shown that peripheral VO2 and DO2 were lower in hypotensive preterm babies when compared with those who were normotensive but that oxygen extraction was similar in both groups. Treatment of the hypotension in the hypotensive groups increased DO2 and VO2 to values comparable with those of normotensive infants but did not alter oxygen extraction. There are several possible explanations for these observations, all depending on the complex nature of oxygen metabolism in the peripheral tissues.
It is possible that VO2 was DO2 dependent in the hypotensive babies. Increasing DO2 in these babies by treating the hypotension therefore increased VO2. However, FOE in the hypotensive babies was not higher when compared with FOE of normotensive babies, and there was no fall in FOE with treatment of hypotension. If DO2 had decreased to a point at which VO2 had become DO2 dependent, then we might have expected to see high values for FOE. It is of course possible that the peripheral tissues of preterm babies are not able to alter oxygen extraction in response to a declining oxygen delivery, but neither higher levels of blood lactate concentration nor tissue injury were associated with low levels of DO2. From consideration of the above we feel that this explanation is unlikely to be correct; the biphasic model for the relationship between DO2 and VO2 is too simplistic to be applied in this situation, and other factors need to be taken into account. One is the local micro-environment. Hemoglobin oxygen affinity plays a part, and this is determined by the nature of the hemoglobin molecule (whether hemoglobin A or hemoglobin F) and its physical environment (especially temperature and pH). Diffusion of oxygen from capillaries to the cell depends on the oxygen tension gradient between erythrocytes and the mitochondria. This is determined by capillary PO2 and other local microcirculatory conditions, such as the position of the cell in relation to intercapillary distances and the surface area of open capillaries(29). The latter can change rapidly, for example in septic shock where arteriovenous shunting occurs and where there is tissue hypoxia despite a high DO2 and a low FOE(17,18).
A similar pattern of results with a normal FOE and a low DO2 and VO2 has been reported in other clinical circumstances in sick individuals with acute respiratory distress syndrome(12–14,30) and in animal models of endotoxinemia(17,18,22,23,31). In our patients, blood lactate concentrations were not elevated despite low values of DO2, and we feel that similar mechanisms are unlikely to be relevant to this situation.
Another possible explanation relates to a change in local temperature. When hypotension caused peripheral vasoconstriction and decreased perfusion, local tissue temperature might have been expected to drop with a consequent fall in metabolic rate. Because of this, the decreased DO2 may still have been sufficient for tissue needs without true tissue hypoxia. It is also possible that vasoconstriction caused a decreased flow through some capillary beds and an increase in arteriovenous shunting, resulting in a low oxygen extraction despite the low DO2, as described above. Whether there was cellular hypoxia would depend on the balance between DO2 and VO2 for each tissue bed. The results of this investigation represented the balance of tissue oxygenation for several tissue beds, which may have been different because of varying local conditions. In this study, the only measurement of skin temperature was from the abdomen as a continuous guide to control the incubator temperature, and this measurement would be expected to be closer to core than to peripheral temperature. The abdominal temperature was an average of 0.3°C less in hypotensive than normotensive infants, but this difference was not significant. The rectal temperatures of all the babies were similar. The temperature of the limb would have been a useful measurement in trying to understand the sequence of physiologic changes, but this was a clinical observation study, and this measurement is not routinely made. One important conclusion is that it should be in future work. There are other ways for the peripheral tissues to economize on oxidative metabolism. One is by decreasing movements; another is by limiting growth. These speculations would need to be studied in more detail.
A final possible explanation is that reduced peripheral VO2, which was associated with hypotension, may have been determined by endocrine mediators, for example catecholamines or corticosteroids, with the reduction in DO2 following the reduction in VO2. This last explanation would account for the observation that oxygen extraction and blood lactate concentration were not raised during hypotension. The exact link between metabolism, vascular tone, and local temperature in peripheral tissues remains to be elucidated.
It is unlikely that the observations reported here were subject to serious methodologic artifact. The measurements of venous saturation and Hbflow in the forearm have been validated in infants and adults(24,25,32). The intrasubject coefficients of variation for forearm venous saturation and Hbflow were 5% and 15%, respectively, but these intraindividual variations reflect not only the variation related to measurement but also the variation related to biologic variability. There were sufficiently large differences between the values of Hbflow in the hypotensive babies compared with the normotensive group to lead us to the view that these observed changes were biologically valid.
Blood lactate concentrations were similar in normotensive and hypotensive babies and did not change after treatment for hypotension. Lactate concentration may be useful for distinguishing whether DO2 is adequate for the tissue's demands. It has been used in critically sick adults(33–35) and neonates(36,37) to predict outcome and represents the consequence of inadequate DO2 to meet demand(38). In this present study, however, the blood lactate concentrations of hypotensive babies were not higher than that of normotensive babies, and there was no change in lactate concentration after treatment for hypotension, adding weight to the view that the low peripheral DO2 was adequate for tissue demands in the presence of the low peripheral VO2 in these infants.
Blood lactate concentrations do not, however, necessarily relate to the current state of tissue oxygenation. Blood lactate concentration is sometimes high at birth, probably because of preceding tissue hypoxia, and normally falls rapidly within the first 12 h after birth(37). In addition, low blood flow to some vascular beds may result in a build up of lactate within the tissues, but this would not be reflected by an increase in blood lactate concentration until the blood flow returned to normal and the excess lactate was washed out of the tissues. An association between an adverse outcome and a failure to fall (or a rise) in blood lactate has been shown by others(36,37,39). This present study also showed an association between hyperlactatemia and an adverse outcome: hyperlactatemia was more strongly associated with death and PVH than was a low blood pressure. There may be several reasons for the association between hyperlactatemia and PVH. Serious PVH may follow cerebral ischemia, which is likely to be associated with generally impaired perfusion, causing hyperlactatemia. Alternatively, the cardiovascular instability produced by a significant PVH may compromise adequate oxygenation in other tissues. Decreased VO2, DO2, and Hbflow were not associated with death or morbidity, and similar findings have been reported in adult subjects(40).
The measurements made using these techniques represent oxygenation in the tissues of the forearm. The peripheral tissues of the upper forearm were chosen because it is likely that changes in the extremities precede changes in more central organs(41). Changes in peripheral oxygen tension have been shown to precede other indicators of shock in animal models(42) and in critically ill adults(43). There are other advantages: the site of monitoring can be easily standardized and it is a part of the body that is readily accessible in all patients.
This study, like that of others(2), has shown a weak relationship between systemic arterial blood pressure and peripheral blood flow. A possible reason for this is that babies with high peripheral vascular resistance may have a normal blood pressure but a low blood flow to the peripheries. A normal blood pressure does not necessarily imply adequate tissue perfusion. One possible consequence of hypotension is to produce an increase in peripheral vascular resistance to allow redistribution of blood flow to central organs. In this study, however, the vascular resistance was not increased in the hypotensive babies, but this does not exclude redistribution of the cardiac output during hypotension, as there may have been vasodilation in other tissues.
When hypotension was treated, VO2 increased significantly. There are several possible explanations. First, DO2 may have increased above the critical point so that VO2 also increased because it was no longer delivery dependent. Alternatively, because the treatment for hypotension consisted mainly of treatment with catecholamines (dopamine infusions, none of the babies received dobutamine), which are known to stimulate metabolic activity particularly within muscle tissue(44,45), the changes seen may have been the result of an increase in oxygen consumption as the primary event. This may then have been followed by an increase in DO2. Another effect of the treatment with dopamine might have been expected to be an increase in systemic vascular resistance through peripheral vasoconstriction. This was not, however, seen in this study, probably because the dose of dopamine (median 5 µg/kg/min) was fairly low, and peripheral vasoconstriction is likely to occur at higher dopamine dosages.
The main difference between the oxygenation of peripheral tissue, investigated in this study, and vital central organs (e.g. brain and myocardium) is the ability for vasoconstriction at the peripheries. In central organs, we would expect a fall in DO2 to be compensated by increased FOE and constant VO2. In a separate study investigating the effect of a low hemoglobin concentration in otherwise healthy preterm infants, we found that peripheral FOE increased in some infants with symptoms attributed to anemia but not in those with normal hemoglobin concentrations(26). The main difference between that situation and the present study was that DO2 is likely to have decreased more acutely in hypotensive babies than those with anemia. The anemic infants were well perfused and peripheral temperature was maintained, whereas in the hypotensive babies, not only was DO2 low but also blood flow to the forearm was lower.
Further study is required to determine the precise mechanism for low peripheral oxygen consumption and delivery in preterm babies, the implications of these observations in terms of outcome, and the sequence of events. Changes in DO2 and VO2 with treatment for hypotension also need to be further investigated to determine when interventions are appropriate and which interventions are most effective at improving outcome. Finally, measurements of cerebral VO2 and DO2 are also possible using NIRS(46), and the relationship between these measurements and peripheral oxygenation may also be clinically relevant.




Abbreviations
- Hbflow :
-
hemoglobin flow
- PVH :
-
periventricular hemorrhage
- NIRS :
-
near infrared spectroscopy
- DO 2 :
-
oxygen delivery
- VO 2 :
-
oxygen consumption
- FOE :
-
fractional oxygen extraction
- SaO 2 :
-
arterial oxygen saturation
- SvO 2 :
-
venous oxygen saturation
- FiO 2 :
-
fraction of inspired oxygen concentration
References
Gill AB, Weindling AM 1993 Cardiac function in the shocked very low birthweight infant. Arch Dis Child 68: 17–21.
Kluckow M, Evans N 1996 Relationship between blood pressure and cardiac output in preterm infants requiring mechanical ventilation. J Pediatr 129: 506–512.
Evans N, Iyer P 1994 Assessment of ductus arteriosus shunt in preterm infants supported by mechanical ventilation: effects of interarterial shunting. J Pediatr 125: 778–785.
Evans N, Iyer P 1994 Incompetence of the foramen ovale in preterm infants supported by mechanical ventilation. J Pediatr 125: 786–792.
Miall-Allen VM, De Vries LS, Whitelaw AGL 1987 Mean arterial blood pressure and neonatal cerebral lesions. Arch Dis Child 62: 1068–1069.
Watkins AMC, West CR, Cooke RWI 1989 Blood pressure and cerebral haemorrhage and ischaemia in very low birthweight infants. Early Hum Dev 19: 103–110.
Bada H, Sheldon B, Perry EH, Arheart KL, Ray JD, Pourcyrous M, Magill HL, Runyan W, Somes GW, Clark FC 1990 Mean arterial blood pressure changes in premature infants and those at risk for intraventricular haemorrhage. J Pediatr 117: 607–614.
Fujimara M, Salisbury DM, Robinson RO, Howat P, Emerson PM, Keeling JW, Tizard JPM 1979 Clinical events relating to intraventricular haemorrhage in the newborn. Arch Dis Child 54: 409–414.
Szymonowicz W, Yu VYH, Wilson FE 1984 Antecedents of periventricular haemorrhage in infants weighing 1250 g or less at birth. Arch Dis Child 59: 13–17.
Miall-Allen VM, Whitelaw AGL 1989 Response to dopamine and dobutamine in the preterm infant less than 30 wk gestation. Crit Care Med 17: 1166–1169.
Report of a joint working group of the British Association of Perinatal Medicine and the research unit of the Royal College of Physicians: 1992 development of audit measures and guidelines for good practice in the management of neonatal respiratory distress syndrome. Arch Dis Child 67: 1221–1227.
Powers SR, Mannal R, Neclerio M 1973 Physiologic consequences of positive end expiratory pressure (PEEP) ventilation. Ann Surg 178: 265–271.
Danek SJ, Lynch JP, Weg JG 1980 The dependence of oxygen uptake on oxygen delivery in the adult respiratory distress syndrome. Am Rev Respir Dis 122: 387–395.
Mohsenifar Z, Goldbach P, Tashkin DP 1983 Relationship between O2 delivery and O2 consumption in the adult respiratory distress syndrome. Chest 84: 267–271.
Shibutani K, Komatsu T, Kubal K 1983 Critical level of oxygen delivery in anaesthetized man. Crit Care Med 11: 640–643.
Kruse JA, Haupt MT, Puri VK, Carlson RW 1990 Lactate levels as predictors of the relationship between oxygen delivery and consumption in ARDS. Chest 98: 959–962.
Astiz ME, Rackow EC, Falk JL 1987 Oxygen delivery and consumption in patients with hyperdynamic septic shock. Crit Care Med 15: 26–28.
Wolf YG, Cotev S, Perel A 1987 Dependence of oxygen consumption on cardiac output in sepsis. Crit Care Med 15: 198–203.
Cain SM 1965 Appearance of excess lactate in anaesthetised dogs during anaemic and hypoxic hypoxia. Am J Physiol 209: 604–610.
Cain SM 1977 Oxygen delivery and uptake in dogs during anaemia and hypoxic hypoxia. J Appl Physiol 42: 228–234.
Adams RP, Dielman LA, Cain SM 1982 A critical value for oxygen transport in the rat. J Appl Physiol 53: 660–664.
Nelson DP, Beyer C, Samsel RW 1987 Pathological supply dependence of oxygen uptake during bacteraemia in dogs. J Appl Physiol 63: 1487–1492.
Nelson DP, Samsel RW, Wood LDH 1988 Pathological supply dependence of systemic and intestinal O2 uptake during endotoxaemia. J Apply Physiol 64: 2410–2419.
Yoxall CW, Weindling AM 1996 The measurement of peripheral venous oxyhemoglobin saturation in newborn infants by near infrared spectroscopy with venous occlusion. Pediatr Res 39: 1103–1106.
De Blasi RA, Ferrari M, Natali A, Conti G, Mega A, Gasparetto A 1994 Noninvasive measurement of forearm blood flow and oxygen consumption by near-infrared spectroscopy. J Appl Physiol 76: 1388–1393.
Wardle SP, Crawley E, Yoxall CW, Weindling AM 1998 Peripheral oxygenation and anaemia in preterm babies. Pediatr Res 44: 125–131.
Cochran DP, Shaw NJ 1995 The use of pulse oximetry in the prevention of hyperoxaemia in preterm infants. Eur J Pediatr 154: 222–224.
van der Zee P, Cope M, Arridge SR, Essenpreis M, Potter LA, Edwards Ad, Wyatt JS, McCormick DC, Roth SC, Reynolds EOR 1992 Experimentally measured optical pathlengths for the adult's head, calf and forearm and the head of the newborn infant as a function of optode spacing. Adv Exp Med Biol 316: 143–153.
Kontos HA, Levasseur JE, Richardson DW 1967 Comparative circulatory responses to systemic hypoxia in man and in unanaesthetized dog. J Appl Physiol 23: 381–386.
Rhodes GR, Newell JC, Shah D 1978 Increased oxygen consumption accompanying increased oxygen delivery with hypertonic mannitol in adult respiratory distress syndrome. Surgery 84: 490–497.
Kaufman BS, Rackow EC, Falk JL 1984 The relationship between oxygen delivery and consumption during fluid resuscitation of hypovolemic and septic shock. Chest 85: 336–340.
Yoxall CW Weindling AM 1997 Measurement of venous oxyhaemoglobin saturation in the adult human forearm by near infrared spectroscopy with venous occlusion. Med Biol Eng Comput 35: 331–336.
Cady LD, Weil MH, Afifi AA, Michaels SF, Liu VY, Shubin H 1973 Quantitation of severity of critical illness with special reference to blood lactate. Crit Care Med 1: 75–80.
Broder G, Weil MH 1964 Excess lactate: an index of reversibility of shock in human patients. Science 143: 1457–1459.
Kruse JA, Zaidi SAJ, Carlson RW 1987 Significance of blood lactate levels in critically ill patients with liver disease. Am J Med 83: 77–82.
Deshpande SA, Ward Platt MP 1997 Association between blood lactate and acid-based status and mortality in ventilated babies. Arch Dis Child 76:F15–F20.
Yoxall CW, Weindling AM 1996 Blood lactate concentrations in sick neonates: normal range and prognostic significance of hyperlactataemia. Pediatr Res 40: 557
Kruse JA, Carlson RW 1991 Use of vasoactive drugs to support oxygen transport in sepsis. Crit Care Med 19: 144–146.
Grayck EN, Meliones JN, Kern FH, Hansell DR, Ungerleider RM, Greeley WJ 1995 Elevated serum lactate correlative with intracranial haemorrhage in neonates treated with extracorporial life support. Pediatrics 96: 914–917.
Bernardin G, Pradier C, Tiger F, Deloffre F, Mattei M 1996 Blood pressure and arterial lactate level are early indicators of short-term survival in human septic shock. Int Care Med 22: 17–25.
Cohn HE 1974 Cardiovascular responses to hypoxaemia and acidaemia in fetal lambs. Am J Obstet Gynecol 120: 817–820.
Niinikoski J, Haikola L 1978 Skeletal muscle PO2: indicator of peripheral tissue perfusion in haemorrhagic shock. Adv Exp Med Biol 94: 85–92.
Beerthuizen GUM, Goris RJA, Kreuzer FJA 1989 Skeletal muscle PO2 during imminent shock. Arch Emerg Med 6: 72–82.
Jackson LK, Key BM, Cain SM 1982 Total and hindlimb O2 uptake and blood flow in hypoxic dogs given dopamine. Crit Med 10: 327–330.
Green NM 1961 Effect of epinephrine on lactate, pyruvate and excess lactate production in normal human subjects. J Lab Clin Med 58: 682–686.
Yoxall CW, Weindling AM 1998 Measurement of cerebral oxygen consumption (CVO2) in the human neonate using near infrared spectroscopy: cerebral oxygen consumption increases with advancing gestational age. Pediatr Res 42: 283–290.
Author information
Authors and Affiliations
Additional information
Supported by the Newborn Appeal (Liverpool Women's Hospital) and the National Health Service North West Regional Research and Development Fund.
Rights and permissions
About this article
Cite this article
Wardle, S., Yoxall, C. & Weindling, A. Peripheral Oxygenation in Hypotensive Preterm Babies. Pediatr Res 45, 343–349 (1999). https://doi.org/10.1203/00006450-199903000-00009
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199903000-00009
This article is cited by
-
Evaluation of urine output, lactate levels and lactate clearance in the transitional period in very low birth weight preterm infants
European Journal of Pediatrics (2021)
-
How to assess hemodynamic status in very preterm newborns in the first week of life?
Journal of Perinatology (2017)
-
Day 1 serum lactate values in preterm infants less than 32 weeks gestation
European Journal of Pediatrics (2010)
-
Bedside detection of low systemic flow in the very low birth weight infant on day 1 of life
European Journal of Pediatrics (2009)
-
Foot Pulse Oximeter Perfusion Index Correlates with Calf Muscle Perfusion Measured by Near-Infrared Spectroscopy in Healthy Neonates
Journal of Perinatology (2005)