Abstract
Echolucent images (EL) of cerebral white matter, seen on cranial ultrasonographic scans of very low birth weight newborns, predict motor and cognitive limitations. We tested the hypothesis that markers of maternal and feto-placental infection were associated with risks of both early (diagnosed at a median age of 7 d) and late (median age = 21 d) EL in a multi-center cohort of 1078 infants <1500 ×g. Maternal infection was indicated by fever, leukocytosis, and receipt of antibiotic; feto-placental inflammation was indicated by the presence of fetal vasculitis (i.e. of the placental chorionic plate or the umbilical cord). The effect of membrane inflammation was also assessed. All analyses were performed separately in infants born within 1 h of membrane rupture (n= 537), or after a longer interval (n= 541), to determine whether infection markers have different effects in infants who are unlikely to have experienced ascending amniotic sac infection as a consequence of membrane rupture. Placental membrane inflammation by itself was not associated with risk of EL at any time. The risks of both early and late EL were substantially increased in infants with fetal vasculitis, but the association with early EL was found only in infants born ≥1 after membrane rupture and who had membrane inflammation (adjusted OR not calculable), whereas the association of fetal vasculitis with late EL was seen only in infants born <1 h after membrane rupture (OR = 10.8;p= 0.05). Maternal receipt of antibiotic in the 24 h just before delivery was associated with late EL only if delivery occurred <1 h after membrane rupture (OR = 6.9;p= 0.01). Indicators of maternal infection and of a fetal inflammatory response are strongly and independently associated with EL, particularly late EL.
Similar content being viewed by others
Main
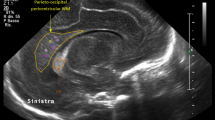
The cranial ultrasound image most clearly associated with histologic evidence of neonatal cerebral white matter damage is an EL in the paraventricular white matter, often identified as periventricular leukomalacia (1). Sonographic expressions of white matter damage predict the motor, cognitive, and perceptual disorders that occur most commonly in infants born near the end of the second trimester (2–7).
Markers of intra-amniotic infection have been linked to premature delivery (8–12), and in very preterm or low birth weight infants to white matter damage (13–20) and cerebral palsy (20–25). If intra-amniotic infection increases the risks of both preterm delivery and white matter damage, then their correlates and consequences might be the same or closely related (26–29). We report here on the relationships of maternal infection and of fetal inflammatory response to white matter lesions.
Several recent findings suggest that the fetal inflammatory response to an intra-amniotic infection may be biologically important, perhaps even more important than the maternal inflammatory response. First, the fetus contributes to the cellular inflammatory response evident in the amniotic fluid (30, 31). Second, funisitis, the most obvious morphologic indicator of a fetal inflammatory response, appears to be better than membrane inflammation in predicting preterm delivery and perinatal death (32), and EL evident within 3 d of birth (13). Third, intra-amniotic infection is accompanied by fetal cytokinemia, that exceeds maternal cytokinemia (33). Fourth, the more severe the histologic inflammatory response, the higher the level of cytokines in the amniotic fluid (34). Fifth, elevated levels of pro-inflammatory cytokines in the amniotic fluid, umbilical cord blood, and early neonatal blood specimens are among the best available predictors of preterm parturition (8, 11, 12), cerebral white matter damage (15, 16, 20), and cerebral palsy (20, 35). Sixth, levels of these cytokines appear to be elevated in the brains of infants who die with histologic evidence of white matter damage (36–38).
Of the 47 infants with an EL in our sample, 17 had their EL identified on the first protocol scan (median age 1 d) or the second (median age 7 d), and 30 had their EL first identified on the third protocol scan (median age 21 d). Because EL present within a short time after delivery might have a risk factor profile that differs from that of EL first evident weeks later (39), we evaluated separately the antecedents of early EL and late EL.
In our prospective multi-center study of very small infants born preterm, we hypothesized a priori that maternal infection was one of the antecedents of EL. To test this particular hypothesis, we related correlates of maternal infection (including fever, leukocytosis, and receipt of antibiotics) to the risk of cerebral white matter EL in a sample of 1048 VLBWI. Placental membrane inflammation was evaluated separately because it appears to have both maternal and fetal contributions (30).
To evaluate the contribution of the fetus to the occurrence of EL, we analyzed how well fetal vasculitis (i.e. vasculitis in the umbilical cord and/or chorionic plate) predicted EL, especially EL first identified weeks after birth. An essential assumption of our analyses is that delivery very shortly after membrane rupture (e.g. within 1 h) does not allow enough time for the fetus to develop a histologically visible inflammatory response to an intra-amniotic infection that follows membrane rupture. Because chorionic plate/umbilical cord vasculitis most likely requires at least several hours after a stimulus to become histologically evident (31, 32, 40, 41), fetal vasculitis in the infant delivered within 1 h of membrane rupture probably antedated membrane rupture.
METHODS
Sample.
A total of 1607 infants were eligible for this study. They were born at one of four participating hospitals between January 1991 and December 1993, weighed 500 to 1500 g at birth, had at least one of three cranial ultrasound scans at times established by the study design, and had information available from medical records about correlates and expressions of maternal infection and about potential confounders (42, 43).
We excluded 11 infants because we lacked information about the number of hours between membrane rupture and delivery, 20 infants who were missing information about confounders, and another 452 infants because their placenta was not available for examination. An additional 46 infants were excluded because they had an echodensity in the cerebral white matter, but lacked a later ultrasound scan to establish that the density either disappeared (so they could be considered noncases) or became an EL (so that they could be considered cases). A total of 1078 infants and their 944 mothers constituted the population for this set of analyses. Demographic characteristics of excluded and included infants were similar.
The gestational age estimate was based on the following hierarchy: fetal ultrasound scan estimate obtained before the end of the 13th wk of gestation (30%), dates in the prenatal record or from maternal interview usually within 48 h of delivery (69%), and from the neonatologist's examination in the delivery room (1%). The gestational age assigned to each infant refers to completed weeks.
Cranial ultrasound scans.
Protocol scans were obtained once during the first 4 postnatal d (median d 1), once between postnatal d 5 and 14 (median d 7), and once between d 15 and 60 (median d 21). The first protocol cranial ultrasound set of scans was available for 1016 infants, the second for 922, and the third for 791. Of the six infants who had a third scan but did not have an earlier scan, none had an EL. Fully 28 of the 30 infants with a late EL had all three protocol scans. Of the other two infants with a late EL, one missed the first protocol scan and one missed the second. Thus, only one infant classified as having a late scan might, instead, have had her EL classified as an early EL had an El been identified on the second protocol scan.
Manuals were created to standardize the scanning procedure and the interpretation of scans. The six standard coronal views were those recommended by Teele and Share (44). The five sagittal views included the midline, each lateral ventricle, and lateral to each lateral ventricle.
Each set of scans was read independently by two sonologists who had no knowledge about the mother or infant. An EL was defined as a hypoechoic (or echopoor) zone of any size anywhere in the cerebral white matter. If either reader identified an EL anywhere in the cerebral white matter, then the scans were presented to a consensus committee. Nine sonologists rotated among the consensus committees. All consensus committees consisted of a minimum of three sonologists (each from a different institution) reading together. All members of each consensus committee had to agree about the presence, size, and location of all ELs. They did so for 92% of the sets of scan they read. When they could not agree, we accepted the majority decision of a larger consensus group (consisting of the three or four readers who disagreed plus the three or four readers from another consensus committee). The overall agreement between individual readers and consensus committees was 85%, with a kappa of 0.46.
Clinical indicators of infection.
Trained research assistants reviewed hospital delivery service records including medication sheets, physicians' orders, and physicians' and nurses' notes for information about the clinical indicators of infection apparent during the interval bounded by 24 h before and 24 h after delivery.
Fever was defined as a body temperature more than 38°C or 100.4° F, and leukocytosis as a white blood cell count of more than 20,000/mL, approximately the top quintile. Women were classified as having received an antibiotic if they did so during the 24 h preceding delivery. Antibiotic receipt was coded categorically as a single yes/no variable because prophylactic or therapeutic purpose was often not recorded, and the available information was insufficient to allocate antibiotic use to either a prophylactic or therapeutic category.
Placental pathology.
At all four institutions, placentas of infants weighing 1500 g were examined according to the study protocol. Samples obtained for histologic examination included cross-sections of the umbilical cord taken from both the placental and fetal ends, a full thickness section (i.e. from chorionic plate to decidual floor) of the placenta near the cord insertion, a full thickness section taken half-way between cord insertion and margin, and a membrane roll with the margin attached or included as a separate piece. Tissue was fixed in 10% formalin, embedded in paraffin, and histologic sections were stained with hematoxylin and eosin. For this study, groups of slides were read systematically.
Membrane inflammation was defined as polymorphonuclear leukocytes in the subchorion, chorion, or amnion (39). Fetal vasculitis was defined as polymorphonuclear leukocytes in the vessel wall located in the chorionic plate of the placenta or in the umbilical cord. Two summary variables (membrane inflammation and fetal vasculitis) in place of the five available (subchorionitis, chorionitis, chorioamnionitis, chorionic plate vasculitis, and umbilical vasculitis) simplifies the analytic task and is based on observations in this sample. Because the risk of EL did not differ whether the inflammation involved the subchorion, chorion, or both chorion and amnion, we classified membrane inflammation as a yes/no variable. Similarly, the odds ratios for developing EL were similar whether we classified infants by the presence/absence of chorionic plate vasculitis or umbilical vasculitis.
Analyses.
One set of analyses had as the cases all infants who developed EL. Grouping the infants whose EL was first identified on the first or second scan (usually by the 7th to 10th d) as “early” EL allowed these 17 infants to be somewhat comparable to the de Vries et al. criterion for an antenatal lesion (39). We evaluated these infants with early EL separately from infants whose EL was identified later (Table 1). Only 1 of the 30 infants with late EL did not have the second protocol scan, and so might have had an unidentified early EL rather than late EL.
Among all infants for whom histologic examination of the placenta was possible, the longer the interval between membrane rupture and delivery, the higher the rate of membrane inflammation (Table 2). In the Brigham and Women's Hospital component of this sample, the longer the interval between membrane rupture and delivery, the higher the rate of ureaplasma recovery from the placenta (41). To separate infants whose inflammatory response most probably preceded membrane rupture from those in whom it probably followed membrane rupture, we chose a 1 h interval between membrane rupture and delivery (Tables 3, 5, and 6). Although short, this interval allowed inclusion of infants exposed to labor and delivered vaginally. A shorter interval between membrane rupture would have limited the subsample to abdominal deliveries. The choice of 1 h was made before data analysis, and in no way reflects an effort to optimize any goal other than avoiding bias (45).
In generalized form, the main null hypothesis we tested is that the risk of an EL in the cerebral white matter of VLBWI is not associated with indicators and correlates of maternal infection just before and during delivery (including elevated temperature, elevated white blood cell count, maternal receipt of antibiotic, placental membrane inflammation, and fetal vasculitis).
All multivariate analyses were stratified according to the interval between membrane rupture and delivery (<1 h, ≥1 h). The relationships among variables were evaluated in univariate analyses, and in different strata defined by the presence, or level, of potential confounders. We adjusted for potential confounders simultaneously in logistic regression models.
The contributions of membrane inflammation and fetal vasculitis to EL risk were highly correlated (54% of placentas with membrane inflammation also had fetal vasculitis, but 99% of placentas with fetal vasculitis had membrane inflammation). Therefore, we first evaluated the contribution of membrane inflammation to EL risk in logistic regression models that included potential confounders and all the indicators of infection except fetal vasculitis. Then, to assess fetal vasculitis, we created similar logistic regression models restricted to the sample of infants with inflamed placental membranes (Table 5). This analytic strategy applies a time-oriented modeling of risk (46, 47) that assumes that in the course of gestational intra-amniotic infection membrane inflammation alone tends to precede fetal vasculitis (32, 34, 40).
We also evaluated other analytic strategies. For example, we created logistic regression models that had variables for membrane inflammation and fetal vasculitis, individually and in combinations, as well as models that had interaction terms for the interval between membrane rupture and delivery and each of the variables that appeared to have greater influence in some subgroups. Regardless of the analytic approach, the findings were robust and supported the view that the risk of both early and late EL was discriminated much better by fetal vasculitis than by membrane inflammation.
We have suggested that intraventricular hemorrhage might be an intervening/contributory event leading from antenatal exposures and characteristics to EL occurrence (28). In addition, postnatal phenomena may also be mediators or add to EL risk. We carried out additional analyses with postnatal characteristics to see if they functioned as intermediaries.
RESULTS
Characteristics of infants classified by the protocol scan thatfirst identified EL (
Table 1).
Our main objective in preparing Table 1 was to see if our data supported joining or separating infants who developed their EL at different postnatal ages. Only eight infants had EL identified on the first cranial ultrasound scan (median age1 d), and another nine had the EL first identified on the second protocol scan (median age 7 d). The remaining 30 of the 47 infants with EL had the lesion first identified on the last protocol scan (median age 21 d).
The small numbers in the first two groups severely limit inferences. We combined the 17 infants with an EL first identified on either the first or second protocol scan into one early EL group to achieve the closest approximation possible to the de Vries et al. criterion (39) for antenatal onset of white matter damage (i.e. a cyst evident before 7 d).
The 47 EL infants differed considerably from the 1031 infants who did not develop an echolucency. Those who developed an EL were gestationally younger, less likely to be growth retarded (i.e. have a birth weight Z score <−2), and have a mother with pregnancy-induced hypertension. They were more likely to be born to a woman who had leukocytosis, received an antibiotic, and had inflammation of the placenta membranes. They were also more likely to have had fetal vasculitis, hypothyroxinemia, intraventricular hemorrhage, and to have been placed on a mechanical ventilator.
Compared with infants who developed a late EL, those who had an early EL tended to be gestationally older, and were more likely to be growth retarded, delivered abdominally, and have a mother who had pregnancy-induced hypertension, a fever during the 24 h before or after delivery, and received antenatal corticosteroid. They were also less likely to be a singleton, exposed antenatally to an antibiotic, and to develop hypocarbia.
Interval between membrane rupture and delivery (
Table 2).
Fever and leukocytosis were more frequent among mothers who delivered more than 24 h after membrane rupture than among those who delivered sooner. Several other indicators of infection, including antibiotic receipt and inflammation of placental membranes, as well as fetal vasculitis, increased in prevalence as the interval between membrane rupture and delivery increased. However, fetal growth retardation and pregnancy-induced hypertension decreased in prevalence with increasing interval between membrane rupture and delivery. EL occurred in approximately 4–5% of infants, regardless of the interval between membrane rupture and delivery.
EL in infants with neither, one, or both indicators of placentalinflammation (
Table 3).
Among infants born within 1 h of membrane rupture, early EL was present in 1–2% regardless of the presence of membrane inflammation or fetal vasculitis. Late EL was present in 1% if fetal vasculitis was absent and in 9% if fetal vasculitis was present.
Infants born more than 1 h after membrane rupture had an EL frequency that did not appear to be influenced by the presence of membrane inflammation or fetal vasculitis. Among later-delivered infants without fetal vasculitis, however, the risk of late EL was four times greater than in those delivered within 1 h after membrane rupture (data not shown).
Potential confounders (Table4).
Gestational age, birth weight Z score (a measure of fetal growth), and pregnancy-induced hypertension were associated (positively or negatively) with fetal vasculitis and maternal antibiotic (Table 4) and both early and late EL (Table 1). As such, they are potential confounders of the associations between fetal vasculitis and EL risk, and between mother's receiving an antibiotic and EL risk. Maternal receipt of an antenatal dose of corticosteroid was also a potential confounder for late, but not early, EL.
Multivariate analyses of antenatal variables (Table5).
When we adjusted for potential confounders and the other variables displayed in Table 5, we found that a parsimonious model without variables for birth weight Z score and pregnancy-induced hypertension did just as well as the larger multivariate model.
Of the 17 infants with early EL, 9 were born <1 h after membrane rupture, and 8 were born ≥1 h after membrane rupture. With such small numbers of cases, the odds ratios tend to have wide confidence intervals, and the p values tend to be high (Table 5 A). Thus, neither the odds ratio of 3.4 (p= 0.09) for maternal receipt of antibiotic in the <1 h stratum, nor the 4.2 (p= 0.21) odds ratio for membrane inflammation in the ≥1 h stratum is statistically significant.
Among the 353 infants whose placenta had membrane inflammation and who were delivered more than 1 h after membrane rupture, all 7 infants with early EL had fetal vasculitis. Thus, an odds ratio for early EL could not be calculated. One of these infants was born 42 h after membrane rupture, and four were born more than 22 d after membrane rupture.
Of the 30 infants with late EL, 12 were born <1 h after membrane rupture, and 18 were born ≥1 h after membrane rupture (Table 5 B). In the <1 h stratum, maternal receipt of antibiotic has an odds ratio for late EL of 6.9 (p= 0.02). In this stratum, fetal vasculitis had a late EL odds ratio of 10.8 (p= 0.05).
Potential postnatal intermediaries between antenatal variables andEL risk (Table6).
To see if postnatal variables account for the relationship between EL risk and either maternal receipt of antibiotic or fetal vasculitis, we added individual postnatal variables one by one to the models in Table 5. With the addition of a variable for intraventricular hemorrhage, the early EL odds ratio for maternal antibiotic in the <1 h stratum fell from 3.4 to 2.5. The addition of other postnatal variables had smaller effects. Mean arterial blood pressure in the lowest or highest quartile, and mechanical ventilation, increased the point estimate slightly.
The point estimate of the late EL odds ratio associated with maternal receipt of antibiotic in the <1 h stratum was 6.9, but fell to 6.1 with the addition of a variable for intraventricular hemorrhage to the multivariate model. This drop of 12% was the only decrease seen with the addition of individual postnatal variables. For the other four postnatal variables, the point estimate increased between 33 and 64%.
The odds ratio of 10.8 for late EL associated with fetal vasculitis in the <1 h stratum of infants with membrane inflammation fell by 14% to 9.3 with the addition of intraventricular hemorrhage to the model.
DISCUSSION
The risk profiles for early and late EL, although probably not identical, each include fetal vasculitis and maternal antibiotic. Thus both fetal and maternal factors might be important contributors to EL occurrence in the very low birth weight newborn.
Fetal vasculitis.
Some intra-amniotic infections are thought to begin with membrane inflammation near the cervical os (presumably the area most accessible to bacterial organisms from the exterior) (40). The more severe the histologic response to the intra-amniotic infection, the more intense is the proinflammatory cytokine cascade (34), which appears to occur much more in the fetus than in the mother (33). In our sample, except for two infants, fetal vasculitis occurred only when the placenta membranes were inflamed.
Why should fetal vasculitis be associated with early EL among infants born ≥1 h after membrane rupture, and with late EL among infants born <1 h after membrane rupture? One difference could be the intensity of the exposure, with early EL following a more intense fetal vasculitis than late EL. For example, early EL infants who develop fetal vasculitis after prolonged membrane rupture were probably more likely than late EL infants to be exposed to (the consequences of) a maternal intra-amniotic infection that was so severe as to prompt rapid evacuation of the uterus. However, late EL infants who developed fetal vasculitis when the membranes were intact were probably exposed to (the consequences of) a considerably less intense/virulent intra-amniotic infection. The more intense the chorioamnionitis, the higher the levels of pro-inflammatory cytokines in the amniotic fluid (34). In this light, we might postulate that high blood levels of fetal cytokines result in early EL and that lower levels result in late EL because more time is needed to make their effects on developing white matter evident. Differences in pre- and postmembrane rupture infections might also reflect characteristics of the inciting organism (e.g. virulence) (48).
A second difference might be the duration of the infection. Because the fetal cytokinemia in prerupture intra-amniotic infection can be present days before the onset of spontaneous preterm parturition (11, 12), differences in the duration of fetal cytokinemia do not seem an attractive explanation for differences between early and late EL.
Several criteria for causal inferences (49) lead us to view fetal vasculitis as a link in the causal chain leading to both early and late EL. Our finding that EL is associated with fetal vasculitis, but not with membrane inflammation, supports the specificity criterion. The consistency criterion is defined by the number, diversity, rigor, and severity of tests of association. This criterion is satisfied by the plethora of studies associating an infection/inflammatory response outside the central nervous system with white matter damage, as well as with motor and cognitive limitations (50). In addition, funisitis has previously been shown to predict very early EL (13). Prolonged rupture of membranes, but without documented infection, has been significantly associated with cerebral palsy risk in preterm infants (23, 51), as has prelabor, preterm membrane rupture (52). In our sample, the longer the interval between membrane rupture and delivery, the higher the unadjusted frequency of late EL (Table 2). The coherence criterion is satisfied by the wealth of data linking a fetal cytokine cascade with intra-amniotic infection (53), cerebral white matter damage (15, 16, 20), and cerebral palsy (20, 35). In addition, levels of these cytokines appear to be elevated in the brains of infants who die with histologic evidence of white matter damage (36–38).
Our failure to find a significant association between membrane rupture and EL is not entirely unexpected, in light of reports that in VLBWI histologic chorioamnionitis was not associated with cerebral palsy (25), and that an association between clinical chorioamnionitis and cerebral palsy was seen only under selected conditions (24). All of these findings are in keeping with the hypothesis that the fetal inflammatory response, and not the intra-amniotic infection, damages the fetal brain.
Maternal antibiotic.
Maternal antibiotic receipt has been associated with cerebral palsy in VLBWI (25), but does not appear to have been identified previously as an antecedent of white matter damage. In our study, the risks of both early and late EL are increased among infants whose mothers received an antibiotic, but only if birth occurred within 1 h of membrane rupture. The EL/antibiotic association is compatible with two possibilities.
A likely possibility is that the antibiotic serves merely as a marker of the infection for which it was presumably administered. Antibiotic receipt conveyed risk information even when we included in our analyses variables about maternal fever, leukocytosis, membrane inflammation, and fetal vasculitis. This raises the possibility that maternal receipt of antibiotic is evidence of an infection not otherwise apparent on review of medical records or by examination of the placenta. This possibility appears tenable in light of observations that maternal (extra-uterine) infections have been associated with an increased risk of histologically defined white matter damage (54, 55), neurologic abnormality at 1 year of age (25, 56), and mental retardation (57).
Another possibility is that the antibiotic itself damages developing white matter (58), perhaps via antimetabolite (59) or cytokine-enhancing properties (60, 61). A rapidly maturing cell line, such as the OA-2 precursor of oligodendrocytes, might pass through a stage that is especially vulnerable (62), perhaps to antibiotic exposure.
Why should the association between EL risk and antibiotic be seen only in those born within 1 h of membrane rupture? One explanation is that antibiotic given to many women who gave birth more than 1 h after membrane rupture (especially if the placenta had minimal membrane inflammation) should be viewed as prophylactic, because membrane rupture is widely viewed as predisposing the fetus to infection (63). Other explanations postulate that antibiotic administered therapeutically to a woman with “prolonged” rupture of membranes is given too late, or for too short a time, to reverse the accompanying fetal inflammatory response, or to adversely affect the fetal brain.
Early versus late EL.
We found that both early and late EL are associated with both maternal antibiotic receipt and fetal vasculitis. Perhaps, then, early and late EL are more alike than they are different. In Table 1, however, differences are sufficient to suggest that the two entities are heterogeneous.
Postnatal variables.
We have suggested that some correlates of intra-amniotic infection contribute to cerebral white matter damage, in part, by increasing the risk of intraventricular hemorrhage (28). Indeed, fetal vasculitis does predict intraventricular hemorrhage in this sample of VLBWI (43). The addition of an intraventricular hemorrhage variable to the model of EL risk, however, scarcely diminished the apparent contributions of the variables for maternal antibiotic receipt and fetal vasculitis. The addition of variables conveying information about blood pressure, hypocarbia, and mechanical ventilation had even less effect on the point estimates of EL risk associated with either maternal antibiotic or fetal vasculitis. These findings suggest that intraventricular hemorrhage and the other postnatal variables we evaluated are not major intermediaries between antenatal indicators of infection/inflammation and the occurrence of EL.
Bias.
Defining samples by birth weight rather than gestational age overrepresents growth retarded infants at older gestational ages (64). The < 1 h subsample has an even greater over-representation of growth retarded/restricted infants and infants born to mothers who had pregnancy-induced hypertension. These characteristics tend to be associated with each other (65). They are also sometimes associated with reduced risk of intracranial hemorrhage, white matter damage, and cerebral palsy in the very preterm (39, 66–69). Adjustment for both fetal growth retardation and pregnancy-induced hypertension, however, had no effect on EL risk. Nevertheless, the distortion that results from overrepresentation of some groups could have distorted our perception of antecedent-associated risks.
Information bias (nonrandom missingness) (70) might also have contributed to some of our findings. We limited some of our analyses to infants who had every one of the variables in the multivariate models. Because the absence of information about some of these variables was not random, some bias might have occurred. Incorporating variables for the presence/absence of some of these variables, however, did not appreciably change our main findings.
This study's limited power, which is evident in the wide confidence intervals in Tables 5 and 6, is a consequence of having small numbers of infants with early and late EL, and our dichotomizing the sample by the interval between membrane rupture and delivery.
Implication.
Our finding that both fetal vasculitis and maternal antibiotic are associated with EL, whether first evident days or weeks later is compatible with three hypotheses. First, antenatal phenomena have late occurring (apparently delayed) consequences in those born preterm. Second, a fetal inflammatory response contributes to cerebral white matter damage. Third, an infection in the mother damages the fetus's brain without resulting in a fetal brain infection.
The major implication of our findings is that strategies to eliminate intra-amniotic, and perhaps other infections before membrane rupture (and perhaps considerably earlier in pregnancy) (29, 71) might reduce the risk of both early and late EL, and thereby the risk of motor, cognitive, and perceptual disabilities overrepresented among those born near the end of the second trimester.
Abbreviations
- EL:
-
echolucency in cerebral white matter
- OR:
-
odds ratio
- VLBWI:
-
very low birth weight infants
References
Paneth N, Rudelli R, Kazam E, Monte W 1994 Brain Damage in the Preterm Newborn. Mac Keith Press, London
Aziz K, Vickar DB, Sauve RS, Etches PC, Pain KS, Robertson CMT 1995 Province-based study of neurologic disability of children weighing 500 through 1249 grams at birth in relation to neonatal cerebral ultrasound findings. Pediatrics 95: 837–844
Pinto-Martin JA, Riolo S, Cnaan A, Holzman C, Susser MW, Paneth N 1995 Cranial ultrasound prediction of disabling and nondisabling cerebral palsy at age two in a low birth weight population. Pediatrics 95: 249–254
Whitaker AH, Feldman JF, Van Rossem R, Schonfeld IS, Pinto-Martin JA, Torre C, Blumenthal SR, Paneth NS 1996 Neonatal cranial ultrasound abnormalities in low birth weight infants: relation to cognitive outcomes at six years of age. Pediatrics 98: 719–729
Whitaker AH, Van Rossem R, Feldman JF, Schonfeld IS, Pinto-Martin JA, Torre C, Shaffer D, Paneth NS 1997 Psychiatric outcomes in low birth weight children at age 6 years: relation to neonatal cranial ultrasound abnormalities. Arch Gen Psychiat 54: 847–856
Murphy DJ, Hope PL, Johnson A 1995 Ultrasound findings and clinical antecedents of cerebral palsy in very preterm infants. Arch Dis Child 74:F105–109
Murphy DJ, Hope PL, Johnson A 1997 Neonatal risk factors for cerebral palsy in very preterm babies: case-control study. Br Med J 314: 404–408
Gomez R, Ghezzi F, Romero R, Munoz H, Tolosa J, Rojas I 1995 Premature labor and intra-amniotic infection: clinical aspects and role of the cytokines in diagnosis and pathophysiology. Clin Perinatol 22: 281–342
Martius J, Roos T 1996 The role of urogenital tract infections in the etiology of preterm birth. Arch Gynecol Obstet 258: 1–19
Goldenberg RL, Thom E, Moawad AH, Johnson F, Roberts JH, Caritis SN 1996 The preterm prediction study: fetal fibronectin, bacterial vaginosis and peripartum infection. Am J Obstet Gynecol 87: 656–660
Romero R, Gomez R, Ghezzi F, Yoon BH, Mazor M, Edwin SS, Berry SM 1998 A fetal systemic inflammatory response is followed by the spontaneous onset of preterm parturition. Am J Obstet Gynecol 179: 186–193
Gomez R, Ghezzi F, Romero R, Yoon BH, Mazor M, Berry SM 1997 Two thirds of human fetuses with microbial invasion of the amniotic cavity have a detectable systemic cytokine response before birth. Am J Obstet Gynecol 176: 514–32
Bejar R, Wozniak P, Allard M, Benirschke K, Vaucher Y, Coen R, Berry C, Schragg P, Villegas I, Resnik R 1988 Antenatal origin of neurologic damage in newborn infants. Am J Obstet Gynecol 159: 357–363
Verma U, Tejani N, Klein S, Reale MR, Beneck D, Jeanty M 1997 Obstetric antecedents of intraventricular hemorrhage and periventricular leukomalacia in the low-birth-weight neonate. Am J Obstet Gynecol 176: 275–281
Yoon BH, Romero R, Yang SH, Jun JK, Kim IO, Choi JH, Syn HC 1996 Interleukin-6 concentrations in umbilical cord plasma are elevated in neonates with white matter lesions associated with periventricular leukomalacia. Am J Obstet Gynecol 174: 1433–1440
Figueroa R, Martinez E, Sehgal P, Garry D, Patel K, Verma U, Visintainer P, Reale M, Klein S, Tejani N 1996 Elevated amniotic fluid interleukin-6 predicts neonatal periventricular leukomalacia and intraventricular hemorrhage. Am J Obstet Gynecol 174: 330
Roland EH, Magee JF, Rodriguez E, Lupton BA, Hill A 1996 Placental abnormalities: Insights into pathogenesis of cystic periventricular leukomalacia. Ann Neurol 40: 3213
Perlman JM, Risser R, Broyles RS 1996 Bilateral cystic periventricular leukomalacia in the premature infant: associated risk factors. Pediatrics 97: 822–827
Zupan V, Gonzalez P, Lacaze-Masmonteil T 1996 Periventricular leukomalacia: risk factors revisited. Dev Med Child Neurol 38: 1061–1067
Yoon BH, Jun JK, Romero R, Park KH, Gomez R, Choi JH, Kim IO 1997 Amniotic fluid inflammatory cytokines (interleukin-6, interleukin-1β, and tumor necrosis factor-α), neonatal brain white matter lesions, and cerebral palsy. Am J Obstet Gynecol 177: 19–26
Nelson KB, Ellenberg JH 1984 Obstetric complications as risk factors for cerebral palsy or seizure disorder. JAMA 251: 1843–1848
Cooke RWI 1990 Cerebral palsy in very low birth weight infants. Arch Dis Child 65: 201–206
Murphy DJ, Sellers S, Mackenzie IZ, Yudkin PL, Johnson AM 1995 Case-control study of antenatal and intrapartum risk factors for cerebral palsy in very preterm singleton babies. Lancet 2: 1449–1454
Grether JK, Nelson K, Emery S III, Cummins SK 1996 Prenatal and perinatal factors and cerebral palsy in very low birth weight infants. J Pediatr 128: 407–414
O'Shea TM, Klinepeter KL, Meis PJ, Dillard RG 1998 Intrauterine infection and the risk of cerebral palsy in very low birth weight infants. Paediat Perinat Epidemiol 12: 72–83
Adinolfi M 1993 Infectious diseases in pregnancy, cytokines and neurological impairment: an hypothesis. Dev Med Child Neurol 35: 549–553
Leviton A 1993 Preterm birth and cerebral palsy. Dev Med Child Neurol 35: 553–558
Dammann O, Leviton A 1997 Maternal intrauterine infection, cytokines, and brain damage in the preterm newborn. Pediatr Res 42: 1–8
Dammann O, Leviton A 1997 Does prepregnancy bacterial vaginosis increase a mother's risk of having a preterm infant with cerebral palsy?. Dev Med Child Neurol 39: 836–840
Sampson JE, THeve RP, Blatman RN, Shipp TD, Bianchi DW, Ward BE, Jack RM 1997 Fetal origin of amniotic fluid polymorphonuclear leukocytes. Am J Obstet Gynecol 176: 77–81
Eschenbach DA 1997 Maternal infection and cerebral palsy in infants of normal birth weight. JAMA 278: 207–211
van Hoeven KH, Anyaegbunam A, Hochster H, Whitty JE, Distant J, Crawford D, Factor SM 1996 Clinical significance of increasing histologic severity of acute inflammation in the fetal membranes and umbilical cord. Pediatr Pathol Lab Med 16: 731–744
Salafia C, Sherer DM, Spong CY, Lencki S, Eblinton GS, Parkash V, Marley E, Lage JM 1997 Fetal but not maternal serum cytokine levels correlate with histologic acute placental-inflammation. Am J Perinatol 14: 419–422
Negishi H, Yamada H, Mikuni M, Kishida T, Okuyama K, Sagawa T, Makinoda S, Fujimoto S 1996 Correlation between cytokine levels of amniotic fluid and histological chorioamnionitis in preterm delivery. J Perinat Med 24: 633–639
Nelson KB, Dambrosia JM, Phillips TM, Grether JK 1998 Neonatal cytokines and coagulation factors in children with cerebral palsy. Ann Neurol 44: 665–675
Deguchi K, Mizuguchi M, Takashima S 1996 Immunohistochemical expression of tumor necrosis factor alpha in neonatal leukomalacia. Pediatr Neurol 14: 13–16
Deguchi K, Oguchi K, Takashima S 1997 Characteristic neuropathology of leukomalacia in extremely low birth weight infants. Pediatr Neurol 16: 296–300
Yoon BH, Romero R, Kim CJ, Koo JN, Choe G, Syn HC 1997 High expression of tumor necrosis factor-α and interleukin-6 in periventricular leukomalacia. Am J Obstet Gynecol 177: 406–411
de Vries LS, Eken P, Groenendaal F, Rademaker KJ, Hoogervorst B, Bruinse HW 1998 Antenatal onset of haemorrhagic and/or ischaemic lesions in preterm infants: prevalence and associated obstetric variables. Arch Dis Child Fetal Neonatal Ed 78:F51–56
Benirschke K, Kaufmann P 1995 Pathology of the human placenta. Third edition. New York: Springer-Verlag
Kundsin RB, Leviton A, Allred EN, Poulin SA 1996 Ureaplasma urealyticum infection of the placenta in pregnancies that ended prematurely. Obstet Gynecol 87: 122–127
Leviton A, Paneth N, Susser M, Reuss ML, Allred EN, Kuban K, Sanocka U, Hegyi T, Hiatt M, Shahrivar F 1997 Maternal receipt of magnesium sulfate does not seem to reduce the risk of neonatal white matter damage. Pediatrics 99: E2
The Developmental Epidemiology Network Investigators. 1998 The correlation between placental pathology and intraventricular hemorrhage in the preterm newborn. Pediatr Res 43: 15–19
Teele R, Share J 1991 Ultrasonography of Infants and Children. Philadelphia: WB Saunders pp 1–5
Altman DG, Lausen B, Sauerbrei W, Schumacher M 1994 Dangers of using “optimal” cutpoints in the evaluation of prognostic factors. J Nat Canc Inst 86: 829–835
Leviton A, Pagano M, Kuban KCK, Krishnamoorthy KS, Sullivan KF, Allred EN 1991 The epidemiology of germinal matrix hemorrhage during the first half-day of life. Dev Med Child Neurol 33: 138–145
Leviton A, Kuban KC, Pagano M, Allred EN, VanMarter L 1993 Antenatal corticosteroids appear to reduce the risk of postnatal germinal matrix hemorrhage in intubated low birth weight newborns. Pediatrics 91: 1083–1088
Reisenberger K, Egarter C, Knofler M, Schiebel I, Gregor H, Hirschl AM, Heinze G, Husslein P 1998 Cytokine and prostaglandin production by amnion cells in response to the addition of different bacteria. Am J Obstet Gynecol 178: 50–53
Susser M 1991 What is a cause and how do we know one? A grammar for pragmatic epidemiology. Am J Epidemiol 133: 635–648
Dammann O, Leviton A 1998 Infection remote from the brain, neonatal white matter damage, and cerebral palsy in the preterm infant. Semin Pediatr Neurol 5: 190–201
Spinello A, Capuzzo E, Orcesi S, Stronati M, Di Mario M, Fazzi E 1997 Antenatal and delivery risk factors simultaneously associated with neonatal death and cerebral palsy in preterm infants. Early Hum Dev 48: 81–91
Dammann O, Allred EN, Veelken N 1998 Increased risk of spastic diplegia among very low birth weight children after preterm labor or prelabor rupture of membranes. J Pediatr 132: 531–535
Mazor M, Cohen J, Roberto R, Ghezzi F, Tolosa JE, Gomez R 1995 Cytokines and preterm labor. Fetal Maternal Med Rev 7: 207–233
Gilles FH, Leviton A, Dooling EC 1983 Developing Human Brain: Growth and Epidemiologic Neuropathology. John Wright-PSG Publishing Co., Boston, pp 304–315
Leviton A, Gilles FH 1984 Acquired perinatal leukoencephalopathy. Ann Neurol 16: 1–8
Niswander KR, Gordon MR, Berendes HW, Hardy JB, Blanc WA, Jackson EC, Clifford SH, Lipsitt LP, Douglas RG, Shapiro S, Drage HS, Weiss W 1972 The Women and Their Pregnancies. DHEW Publication No. (NIH 73:379), Bethesda, MD, pp 252–256
Broman S, Nichols PL, Shaughnessy P, Kennedy W 1987 Retardation in Young Children. Lawrence Erlbaum Associates, Hillsdale NJ, pp 208
Hodges GR, Watanabe I 1980 Chemical injury of the spinal cord of the rabbit after intracisternal injection of gentamicin: an ultrastructural study. J Neuropathol Exp Neurol 39: 452–475
Cullen MJ, Webster HD 1989 Inhibition of protein synthesis during CNS myelination produces focal accumulations of membrane vesicles in oligodendrocytes. J Neurocytol 18: 763–774
Tufano MA, de l'Ero GC, Ianniello R, Baroni A, Galdiero F 1992 Antimicrobial agents induce monocytes to release IL-1 alpha, IL-6, and TNF, and induce lymphocytes to release IL-4 and TNF gamma. Immunopharmacol Immunotoxicol 14: 769–782
Prins JM, Kuijper EJ, Mevissen LCM, Speelman P, van Deventer SJH 1995 Release of tumor necrosis factor alpha and interleukin-6 during antibiotic killing of Escherichia coli in whole blood: influence of antibiotic class, antibiotic concentration, and presence of septic serum. Infect Immun 63: 2236–2242
Oka A, Belliveau MJ, Rosenberg PA, Volpe J 1993 Vulnerability of oligodendroglia to glutamate: Pharmacology, mechanisms, and prevention. J Neurosci 13: 1441–1453
Egarter C, Leitich H, Karas H, Wieser F, Husslein P, Kaider A, Schemper M 1996 Antibiotic treatment in preterm premature rupture of membranes and neonatal morbidity: a metaanalysis. Am J Obstet Gynecol 174: 589–597
Arnold CC, Kramer MS, Hobbs CA, McLean FH, Usher RH 1991 Very low birth weight: a problematic cohort for epidemiologic studies of very small or immature neonates. Am J Epidemiol 134: 604–613
Misra DP 1996 The effect of the pregnancy-induced hypertension on fetal growth: a review of the literature. Paed Perinat Epidemiol 10: 244–263
McCarton CM, Wallace IF, Divon M, Vaughan HG Jr 1996 Cognitive and neurologic development of the premature, small for gestational age infant through age 6: comparison by birth weight and gestational age. Pediatrics 98: 1167–1178
Churchill D, Perry IJ, Beevers DG 1997 Ambulatory blood pressure in pregnancy and fetal growth. Lancet 2: 7–10
Collins M, Paneth N 1998 Preeclampsia and cerebral palsy: are they related?. Dev Med Child Neurol 40: 207–211
Spinello A, Capuzzo E, Cavallini Stronati M, De Santolo A, Fazzi E 1998 Preeclampsia, prematurity and infant cerebral palsy. Eur J Obstet Gynecol 77: 151–155
Park T 1998 An approach to categorical data with nonignorable nonresponse. Biometrics 54: 1579–1590
Goldenberg RL, Andrews WW 1996 Intrauterine infection and why preterm prevention programs have failed. Am J Public Health 86: 781–783
Acknowledgements
The authors thank the women who not only agreed to be interviewed for this study, but also allowed data to be collected from their babies' charts. The authors express their appreciation to their colleagues who contributed to the success of this project.
Author information
Authors and Affiliations
Consortia
Additional information
Supported by the National Institute of Neurologic Disorders and Stroke (NS 27306) and from a grant provided by United Cerebral Palsy Research and Education Foundation (R-712–96).
Rights and permissions
About this article
Cite this article
Leviton, A., Paneth, N., Reuss, M. et al. Maternal Infection, Fetal Inflammatory Response, and Brain Damage in Very Low Birth Weight Infants. Pediatr Res 46, 566 (1999). https://doi.org/10.1203/00006450-199911000-00013
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199911000-00013
This article is cited by
-
A systematic review of immune-based interventions for perinatal neuroprotection: closing the gap between animal studies and human trials
Journal of Neuroinflammation (2023)
-
Four major patterns of placental injury: a stepwise guide for understanding and implementing the 2016 Amsterdam consensus
Modern Pathology (2021)
-
Neurocognitive function of 10-year-old multiples born less than 28 weeks of gestational age
Journal of Perinatology (2019)
-
Early life antecedents of positive child health among 10-year-old children born extremely preterm
Pediatric Research (2019)
-
Placental programming of neuropsychiatric disease
Pediatric Research (2019)