Abstract
This investigation determined if a short interval of modest hypothermia (1 h) initiated 30 min after brain ischemia provided neuroprotection. The rationale for the time and duration of brain cooling reflects the likelihood that the implementation of neuroprotective strategies will occur at an interval shortly after ischemia, and that long- term maintenance of normothermia is a cornerstone of neonatal stabilization. Studies were performed in 22 ventilated neonatal mini-swine in a superconducting magnet to obtain 31P magnetic resonance spectra. After a control period all animals underwent 15 min of global brain ischemia and were maintained normothermic for the first 30 min post-ischemia. In one group of 11 swine normothermia was continued. In the other group of 11 swine, modest hypothermia was initiated at 30 min post-ischemia, continued for 1 h and followed by resumption of normothermia. Animals were subsequently weaned from ventilator support, removed from the magnet, and underwent neurobehavioral and histologic assessment at 72 h post-ischemia. Both groups had similar severity of ischemia, as indicated by identical changes in arterial blood pressure and pH, alterations in brain β- nucleotide triphosphate (% of control where control = 100%, 32 ± 28 vs 27 ± 26% for normothermic and hypothermic groups, respectively), and the extent of intraischemic brain acidosis (6.13 ± 0.19 vs 6.14 ± 0.14 for normothermic and hypothermic groups, respectively). In both groups the distribution of stages of encephalopathy were the same: 1 normal and 10 abnormal (4 mild, 2 moderate, and 4 severe) normothermic, and, 3 normal and 8 abnormal (4 mild, 2 moderate, and 2 severe) hypothermic animals. There was no difference in the extent of neuronal injury between groups. We conclude that a 1-h interval of modest hypothermia initiated at 30 min post-ischemia does not confer neuroprotection.
Similar content being viewed by others
Main
Hypoxic-ischemic brain injury in the term and near term newborn remains a condition in which therapy is limited to supportive intensive care. Investigations have increased regarding specific pharmacologic and nonpharmacologic brain-oriented therapies (1). Modest reductions in brain temperature as an interventional therapy continues to show promise for the newborn and multiple studies have demonstrated benefit when modest hypothermia is used for resuscitation immediately after an insult. Modest reduction in body temperature for 12 h after hypoxia-ischemia attenuated the extent of secondary or delayed energy failure occurring between 12–48 h post-insult (2). Using the same model and hypothermic regimen, the delayed rise in lactate peak area ratios occurring 24–48 h after hypoxia-ischemia was reduced (3). Immediate reduction in body temperature after hypoxia-ischemia in both 7 d (6°C for 3 h) and 21 d (2.5°C for 72 h) rat pups resulted in a reduction in the extent of neuronal injury compared with animals maintained normothermic (4, 5). This laboratory has demonstrated both histologic and neurobehavioral benefits from a 2.5°C temperature reduction for 1 h immediately after brain ischemia in neonatal swine (6). However, two investigations of modest temperature reduction for immediate resuscitation of 7-d rat pups undergoing hypoxia-ischemia failed to document benefit at 28-d follow-up (7, 8). In one study, evidence of benefit from modest hypothermia was present when brains were examined at 7 d after hypoxia-ischemia (8), raising the possibility that modest hypothermia may delay the development of permanent injury, and thereby extend the time interval to initiate other potential therapies.
Although the evidence of neuroprotection associated with modest hypothermia immediately after hypoxia-ischemia is encouraging, practical concerns may limit its clinical application. For a resuscitative therapy to be successful for neonates, treatment needs to be effective when initiated at an interval after hypoxia-ischemia or ischemia. This reflects the necessity to establish a diagnosis and stabilize vital functions (airway, ventilation, perfusion pressure, substrate availability). Few studies have examined modest hypothermia for brain resuscitation at an interval after an insult in neonates. Gunn and coworkers (9) demonstrated that a modest reduction in brain temperature via selective head cooling in fetal sheep provided neuroprotection in utero when initiated 1.5 h post-ischemia in fetal sheep. However, modest hypothermia initiated at 6 h after hypoxia-ischemia in 21-d rat pups did not provide neuroprotection (5). Prior studies from this laboratory demonstrated that neuronal damage was decreased by 1 h of immediate post-ischemic modest hypothermia (6), but the extent of histologic benefit was less compared with modest hypothermia used in a protective mode (10). Given the difference between protective and immediate resuscitation with modest hypothermia, and the paucity of available data in neonatal models, our investigation tested the hypothesis that 1 h of post-ischemic modest hypothermia would decrease brain damage when initiated 30 min after ischemia, compared with normothermia during the post-ischemic interval.
METHODS
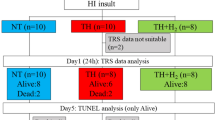
This investigation was approved by the Institutional Review Board for Animal Research at the University of Texas Southwestern Medical Center at Dallas. Details regarding the surgical preparation, physiologic monitoring, MRS, and outcome variables have been previously published (6, 10) and are summarized briefly below. Twenty-two mini-swine were studied in the first 2 wk of life. Animals were aseptically instrumented 24 h before the experiment to place arterial and venous catheters (ketamine and pentobarbital for anesthesia) that were stored in a pouch on the animal's back. On the day of the experiment animals were intubated (thiopental), mechanically ventilated (70% N20 and 30% O2), immobilized (vecuronium), and provided anagelsia (nalbuphine HCl). A rectal temperature probe was inserted, a blood pressure cuff was positioned around the animal's neck, the body was wrapped in a thermal blanket, and then positioned in the bore of a superconducting magnet with the head resting on a 4 × 5 cm double tuned (31P and 1H) surface coil.
After a 90-min stabilization period in the magnet, a 20-min control period was used to obtain baseline data, and was followed by brain ischemia during which a normothermic rectal temperature was maintained. To induce ischemia the neck blood pressure cuff was gradually inflated along with venous hemorrhage over a 20-min interval. The start of brain ischemia was designated when a cuff inflation pressure of 300 mm Hg and a mean arterial pressure of 30 mm Hg had been achieved. Ischemia was maintained for 15 min. At the completion of ischemia all withdrawn blood was reinfused, the neck cuff was deflated, and rectal temperature was maintained normothermic for the first 30 min. For 11 swine (mean ± SD, age 9 ± 4 d, weight 1.72 ± 0.68 kg) normothermia was continued for 90 min, although for the other 11 swine (age 8 ± 4 d, weight 1.67 ± 0.50 kg) modest hypothermia was initiated and continued for 1 h, followed by resumption of normothermia for 30 min. Groups were designated normothermic and hypothermic based on the post-ischemic rectal temperature. Modest hypothermia was achieved by changing the temperature of the circulating water through the thermal blanket and monitoring rectal temperature. After the post-ischemic interval, animals were weaned from the ventilator, extubated, returned to their pens and maintained for 72 h.
Two additional piglets were studied to verify that rectal temperature could be used as an indirect measure of brain temperature during the post-schemic interval. Both animals were acutely instrumented with placement of intravascular catheters—a rectal and a brain temperature probe at a depth of 2 cm beneath the cortical surface. The animals were then wrapped in a thermal blanket and subjected to a 15-min interval of normothermic brain ischemia as described above. After ischemia one animal was maintained with a normothermic rectal temperature for 3 h, and the second animal maintained normothermic for 30 min followed by modest hypothermia for 60 min, and subsequent resumption of normothermia.
Mean arterial blood pressure, heart rate, and rectal temperature were monitored continuously. Arterial blood was sampled for pH, blood gases, hematocrit, and plasma concentrations of glucose and lactic acid during control (in duplicate), at 4 and 12 min of ischemia, and at 5, 30, 60, 90, and 120 min after ischemia. Phosphorus-31 MRS (31P- MRS) of brain were acquired on a Nicolet system (Madison, WI) equipped with a 1.9 Tesla Oxford magnet (Oxford, U.K.) operating at 32.5 MHz for 31P and 80.3 MHz for 1H as described previously (11). Each 31P MR spectrum was acquired over an approximately 7-min duration using a simple pulse acquire sequence (45-μs pulse width, 256-ms acquisition time, 1.5 s interpulse delay, sweep width of 2000 Hz, 4K data points per free induction decay and 256 free induction decay transients per spectrum). Spectra were acquired in duplicate during control, ischemia, and at 30-min intervals during the 120-min post-ischemia period.
At 24, 48, and 72 h after ischemia, a neurobehavioral assessment was performed using an adaptation of the OPS described by Leonov et al. (12) and previously used in this laboratory (6, 10). The OPS evaluates the state of awareness, ambulatory abilities, muscle tone, abnormal movements, presence or absence of hyperventilation and seizures, response to noise, pain, and light, and the ability to feed. Scores were used to categorize each piglet as either normal or with varying degrees of encephalopathy (mild, moderate, severe). Animals were reintubated after assessment at 72 h post-ischemia, or earlier if animals died prematurely. After intubation brains were perfused and fixed in vivo for histologic evaluation. Brains were sectioned in axial orientation, at depths of approximately 5, 10, 15, 20, and 25 mm from the cortical surface, processed, and stained with hematoxylin and eosin. Ischemic neuronal damage was determined by a neuropathologist (D.K.B.) blinded to group assignment. The neuronal histologic score was based on the presence of nuclear pyknosis and karyolysis, and cytoplasmic retraction and eosinophilia. Neuronal morphology in 16 predefined brain regions was scored on a scale of 0 to 4 as follows: 0, normal: 1, scattered isolated ischemic neurons: 2, cluster of ischemic neurons; 3, laminar necrosis: and 4, ischemic changes in almost all or all neurons (photomicrographic examples of the neuronal morphology can be viewed inRef. 6).
Changes in the cerebral energy metabolites NTP, PCr, and Pi were quantitated by comparison of 31P-MRS peak heights measured during and after ischemia with respect to baseline values at control, and expressed as a percent of control. Intracellular pH was calculated from the chemical shift of the Pi peak relative to PCr, as outlined previously (13). A repeated measures analysis of variance was used to compare brain metabolic and systemic variables of the normothermic and modestly hypothermic groups. If significance was achieved using a liberal value for time and interaction effects (p< 0.1), then a Bonferroni-adjusted multiple comparisons were used to localize significant group-time interaction (p< 0.0016) and time effects (p< 0.0018–0.0024, depending on the number of comparisons). Comparison of OPS between groups was performed using a one-sided exact linear-by-linear test. Neuronal histologic scores were compared between groups by a one-sided Mann-Whitney test. All results are mean ± SD.
RESULTS
Figure 1 shows the relationship between rectal and brain temperature during the post-ischemic interval. Brain temperature at a depth of 2 cm beneath the cortical surface was almost identical to rectal temperature before ischemia, and intraischemic brain temperature decreased in both animals even though rectal temperature was maintained normothermic. After ischemia, maintenance of a normothermic rectal temperature was associated with a rapid increase in brain temperature to within 0.75°C of the body temperature. In the animal undergoing post-ischemic modest hypothermia, brain temperature reapproximated rectal temperature during the initial normothermic recirculation, and then mirrored rectal temperature as the latter was reduced during hypothermia. As rectal temperature was raised after modest hypothermia, brain temperature increased, but there appears to be a lag in the change in brain relative to rectal temperature. Despite the latter, the results support the use of rectal temperature as an indirect measure of brain temperature during the post-ischemic interval.
The relationship between rectal and brain temperature in two newborn swine. In the top panel rectal temperature of the first animal was maintained constant during control (C), ischemia (Isc), and post-ischemia (Post-Isc). In the bottom panel rectal temperature of a second animal was lowered 30 min into the post-ischemic period and maintained hypothermic for 1 h. This interval is demarcated by a box labeled hypothermia.
Rectal temperatures were the same in the normothermic and hypothermic groups during control and ischemia (Fig. 2). Distinct rectal temperatures occurred between groups after 30 min of normothermic post-ischemic conditions and were maintained for 1 h (p< 0.001). Although rewarming was commenced at 153 min, rectal temperature remained lower until 180 min, resulting in a total duration of post-ischemic hypothermia equal to 90 min. Changes in MABP during and after ischemia were the same between groups, and both groups had a lower MABP over the last 90 min of the post-ischemic interval compared with control values. There were significant but similar time effects for heart rate in each group. For normothermic and hypothermic groups, respectively, heart rate at control was 228 ± 47 and 253 ± 32 bpm, increased during ischemia in each group to 287 ± 13 and 281 ± 33 bpm (p< 0.0001 versus control), and fell to 194 ± 25 and 168 ± 17 bpm at the completion of the post-ischemic interval (p< 0.0001 versus control). Arterial pH was the same between groups, and values at the completion of post-ischemia did not differ from baseline values at control. There were no differences between groups in arterial O2 tension throughout the study. Experiments were conducted under normocapnic conditions (PaCO2 at control, 4.7 ± 0.3 and 4.7 ± 0.5 kPa for normothermic and hypothermic, respectively) and was maintained constant during the study. Arterial plasma glucose concentration was the same between groups at control (5.6 ± 0.9 and 5.3 ± 0.9 mM for normothermic and hypothermic, respectively), increased to the same amount during ischemia (20.4 ± 8.7 and 18.2 ± 8.9 mM, respectively) and returned to control values by the completion of the post-ischemic interval. Similarly there were no differences between groups in arterial plasma lactate concentration; baseline values were 1.1 ± 0.2 and 1.0 ± 0.2 mM for normothermic and hypothermic groups, respectively, rose by 5 mM during ischemia in each group, and returned to baseline values by the completion of the post-ischemic period.
Results are plotted during control (C), ischemia (Isc), and following ischemia (Post-Isc) for normothermic (solid symbols) and modestly hypothermic (open symbols) animals. Distinct rectal temperatures occurred between groups after 30 min of normothermic recirculation and persisted over 90 min. Mean arterial pressure and arterial pH were the same between groups throughout the study.
In addition to physiologic variables, 31P-MR spectra were acquired to assess the severity of brain ischemia between the two groups. High energy metabolite ratios were the same for both groups at control (PCr/β-NTP; 1.60 ± 0.22 and 1.53 ± 0.20, Pi/β-NTP; 1.34 ± 0.11 and 1.29 ± 0.19, for normothermic and hypothermic, respectively). Both groups developed the same extent of intraischemic brain acidosis, which persisted over the first 15 min of the post-ischemic period (Fig. 3). Intracellular pH was the same as control values by 30 min after ischemia, and did not differ between groups at any time. The extent of intraischemic brain energy failure was also similar between groups as indicated by the reduction in β-NTP and the increase in Pi relative to control. Both groups did not differ in the extent of recovery in β-NTP and decrease in Pi during the post-ischemia interval. Changes in PCr paralleled the alterations in β-NTP during and after ischemia and did not differ between groups (not shown).
Results and group designations are plotted as in Figure 2. SDs for β-NTP and Pi at control represent the SD of the percent difference between duplicate spectra acquired during control. There were no differences between groups for intracellular pH, β-NTP, and Pi.
During the 72 h follow-up after ischemia, surviving animals had stable physiologic measurements and there were no differences between groups in MABP, arterial pH, blood gases, and plasma concentrations of glucose and lactate. Classification of the maximal OPS score for each animal (Table 1) indicated that there were no differences between groups in the number and distribution of normal and encephalopathic animals. Seven animals died before the 72 h follow-up. Four deaths occurred in the normothermic group (three severe and one moderate encephalopathy) on the first day after ischemia. Three deaths occurred in the hypothermic group (two severe and one moderate encephalopathy), all on the second day after ischemia. In each region of brain more than 70% of animals had evidence of neuronal injury. Exceptions were the medulla (no injury in either group) and the pons (one normothermic and two hypothermic animals with injury). There were no differences between groups in the extent of neuronal injury for the 16 regions surveyed (Fig. 4). Results for the neocortex at a depth of 10 mm beneath the cortical surface, cerebellum and midbrain (data not shown) are similar to the results in Figure 4.
The results represent histologic grades of frontal, parietal, temporal, and occipital cortex at a depth of 5 mm beneath the cortical surface within an axial section (top) and selected subcortical structures (bottom). Solid and open symbols represent normothermic and modestly hypothermic groups, respectively, and each symbol represents a different animal. Group comparisons are indicated by the p values.
DISCUSSION
This investigation demonstrated that a 1-h interval of modest hypothermia initiated 30 min after normothermic ischemia does not provide neuroprotection. This conclusion is based on two different outcome variables, the extent of histologic neuronal injury and neuro-behavioral assessment. These experiments used a well-established model of brain ischemia in which neuronal damage is global and was evident in more than 70% of the animals in each group. The extent of ischemic neuronal alterations ranged from isolated ischemic neurons to extensive ischemic changes in all neurons surveyed. Previous studies in this laboratory have indicated that neuronal damage can be attenuated in this model by interventions using hypothermia (6, 10). 31P-MR spectroscopy was used to assess the severity of brain ischemia and demonstrated that the degree of energy failure and brain acidosis both during and after the ischemic interval was similar between normothermic and hypothermic groups. In addition, systemic physiologic and biochemical variables were comparably affected by the ischemic insult in both groups. The only difference was the rectal temperature which by design was significantly lower in the hypothermic group from 30 to 90 min after brain ischemia. Our preliminary results verified that brain temperature in the hypothermic group was likely to be approximately 2°C lower than the normothermic group during the interval of post-ischemic hypothermia.
As in our prior investigation (6) a 1-h interval of modest hypothermia was examined in the post-ischemic period. The rationale for a relatively short exposure to a reduction in body temperature are the well-known potential adverse effects of a cold stress in neonates. These include derangements in cardiopulmonary function with resultant reductions in arterial O2 tension (14), and metabolic alterations such as lactic acidosis and hypoglycemia (15, 16). Other well documented adverse effects of cold exposure such as hematologic abnormalities (17) and immunologic dysfunction (18) have been readily demonstrated in older patients. Therapies that could provide neuroprotection and simultaneously minimize exposure to potential hazards associated with the treatment would be more attractive for evaluation in Neonatal Intensive Care Units.
The lack of neuroprotection associated with the current protocol is in marked contrast to the generally positive results when modest hypothermia is implemented either during or immediately after an hypoxic-ischemic interval. However, these observations are not in conflict with reports in adult animals. For example, a beneficial effect of 3 h of post-ischemic hypothermia in adult rats was demonstrated when brain cooling was initiated 5 min into the recirculation period but was not detectable when cooling was delayed to 30 min after ischemia (19). Similarly in adult dogs undergoing cardiac arrest due to ventricular fibrillation, a delay of 15 min in initiation of cooling after reperfusion resulted in greater histologic damage and worse neurologic deficit scores, compared with animals undergoing mild, resuscitative brain hypothermia concurrent with reperfusion (20). However, results from adult studies should not be extroplated or used to predict findings for neonates due to the potential confounding effect of brain maturation. For example, it has long been recognized that the newborn is more resistant to anoxia and ischemia compared with adults of the same species (21), and reduced cerebral energy requirements of the newborn account for much of this difference (22). We have used 31P-MR spectroscopy to establish that mini-swine have similar maturational increases in cerebral energy utilization rate during the first month of life (23). In adults hypoxic-ischemic brain damage is worsened by hyperglycemia and has been attributed to excess brain lactate production (24, 25). In contrast, Vannucci and coworkers (26, 27) demonstrated that hyperglycemia in the immature rat does not increase the extent of hypoxic-ischemic brain damage. The latter reflects the lack of differences in the extent of depletion in high energy phosphate reserves and accumulation of brain lactate in glucose-supplemented versus saline-infused 7-d-old rat pups. Complementing the latter observations, we demonstrated that rates of brain lactate formation were not as strongly accelerated by increasing blood glucose compared with older mini-swine (28). Furthermore, maturation may affect the time course of pathophysiologic changes immediately after ischemia. For example, more severe intraischemic brain acidosis decreases post-ischemic lactate and acid clearance (29); due to confounding systemic hyperglycemia that occurs commonly in adults, brain lacticacidosis may be both more severe and prolonged in adults compared with newborns. In addition, the extent of post-ischemic uncoupling between brain acid and lactate clearance increases with advancing age (29). Similar careful comparisons of the effect of maturation on other components in the cascade culminating in brain injury, such as the release/clearance of excitotoxins, oxidative injury, etc., have not been performed. For the available observations discussed above the direction of effect would benefit the newborn. Given that hypothermia may further favorably alter events in the immediate post-ischemic interval (e.g. reduce lactate production, clearance of excitotoxins), it seemed reasonable to postulate for the newborn that a short 30-min delay before initiating modest hypothermia may still provide neuroprotection.
Studies in adult animals have also demonstrated that the duration of the therapeutic window can be lengthened if the interval of post-ischemic brain cooling is increased. In adult rats undergoing transient cerebral ischemia, different durations of modest hypothermia initiated at 2 h after ischemia were examined for the effect on the hippocampal CA1 region (30). Thirty min of hypothermia was not effective in providing neuroprotection, 3.5 h of hypothermia decreased neuronal damage by only 10%, and 5 h of hypothermia resulted in marked neuronal protection. In adult gerbils the extent of histologic damage in the CA1 region after 5 min of global ischemia was markedly decreased when brain cooling (32°C) initiated at 1 h post-ischemia was extended from 12 h (85% of neurons damaged) to 24 h [10% of neurons damaged (31)].
There is limited information in the perinatal period regarding the duration of the therapeutic window. Sirimanne et al. (5) studied 21-d rat pups subjected to 15 min of hypoxia-ischemia and manipulated body temperature during either the first 6 h and/or between 6–72 h after the insult. The extent of cortical infarction and striatal damage was reduced only when hypothermia (a decrease in body temperature from 37.9 to 35.5°C) was extended over the entire 72 h after hypoxia-ischemia. In contrast, Gunn et al. (9) demonstrated that selective head cooling in fetal sheep initiated at 90 min after global brain ischemia and continued for 72 h reduced secondary cortical cytotoxic edema, preserved greater residual EEG activity, and decreased the extent of cortical infarction and neuronal loss. The same investigators have extended these observations by initiating selective hypothermia at 5.5 h after reperfusion and continuing treatment until 72 h, and demonstrated qualitatively similar beneficial effects as above but with less neuroprotection (32). An important distinction between studies performed in utero and postnatally is that the degree of brain cooling during the ischemic interval is potentially markedly different. In the reports of Gunn et al. (9, 32), extradural temperature did not change during ischemia performed in utero, and presumably reflects similar temperature of the brain and amniotic fluid cavity. In contrast, in our study intraischemic brain temperature decreased approximately 3°C (Fig. 1) because experiments were conducted at room temperature creating a temperature gradient from the brain to the ambient environment, at a time when O2 uptake and heat production were reduced. Sirimanne et al. (5) studied hypoxia-ischemia postnatally at an environmental temperature of 34°C with high humidity, conditions that should minimize intraischemic temperature reduction (measurements were not reported). The magnitude of intraischemic temperature decrease could be expected to influence the final outcome of any experimental paradigm. Despite this, the favorable outcome of fetal lambs treated with delayed hypothermia post-ischemia may have been facilitated by the duration of the therapy and the enhanced ischemic resistance characteristic of the immature (21). Whether the pathogenesis of ischemic brain damage in the fetus is identical to the neonate with respect to the contributions of different pathways (e.g. excitotoxins, oxidative injury, apoptosis, etc.) is unknown. Clearly some processes such as the neurotoxicity of glutamate depend markedly on the stage of brain development (33).
The lack of neuroprotection observed in our study using 1 h of modest hypothermia initiated 30 min after global brain ischemia is consistent with the accumulating data that long intervals of brain cooling are necessary to achieve neurologic benefit when implemented after a brain insult. This implies that ischemic and hypoxic-ischemic injury are ongoing processes involving deleterious mechanisms that are active during the post-ischemic period. These processes remain poorly understood, are not well integrated, and manifest at some interval between primary energy failure (the acute ischemic or hypoxic-ischemic event) and delayed or secondary energy failure. The latter is characterized by reductions in PCr and NTP, increases in Pi, and absence of brain acidosis beginning at 12 h and reaching minimal values of NTP at 24–48 h post-acute insult (34). When delayed hypothermia is neuroprotective, the mechanisms by which this occurs are not firmly established. Modest hypothermia initiated after a short post-ischemic delay may affect processes interdigitated with primary energy failure such as shortening the interval to restore phosphorylated metabolites, decreasing the duration of brain acidosis, more rapid clearance of excitatory neurotransmitters from the extracellular fluid, and attenuation of nitric oxide production (35). Modest hypothermia initiated at longer intervals after ischemia (i.e. hours) presumably would affect processes involved in the development of secondary energy failure. These processes are speculative at present but may involve trigger mechanisms for apoptosis (36), secondary release of excitotoxins (37), and impairment of protein synthesis. In newborn piglets under well-controlled laboratory conditions, modest hypothermia initiated immediately after hypoxia-ischemia and continued for 12 h attenuated the extent of secondary energy failure (2). Initiating brain cooling immediately after hypoxia-ischemia may obviate the need for a prolonged interval of hypothermia, as demonstrated by Bona et al. (38). These investigators demonstrated neuropathologic brain protection at 6 wk after a 6-h interval of hypothermia initiated immediately after hypoxia-ischemia. Even shorter intervals of immediate post-insult hypothermia (3 h) have been demonstrated to delay the development of brain injury (8), and potentially offer an extended therapeutic window to initiate other therapies with possible synergistic effects with brain cooling (39). However, in clinical practice immediate brain cooling after hypoxia-ischemia will be unlikely, and management trials will need to evaluate the impact of some delay between the insult and therapy. Given the demonstration of essentially normal 31P-MRS on d 1 of life in term asphyxiated infants and subsequent cerebral energy failure during the next few days (40), it seems likely that prolonged periods of brain cooling (2–3 d) will need to be tested in clinical trials.
Abbreviations
- MABP:
-
mean arterial blood pressure
- MRS:
-
magnetic resonance spectroscopy
- NTP:
-
nucleotide triphosphate
- OPS:
-
overall performance score
- PCr:
-
phosphocreatine
- Pi:
-
inorganic phosphorus
References
Vannucci RC, Perlman JM 1997 Interventions for perinatal hypoxic-ischemic encephalopathy. Pediatrics 100: 1–11.
Thoresen M, Penrice J, Lorek A, Cady EB, Wylezinska M, Kirkbride V, Cooper CE, Brown GC, Edwards AD, Wyatt JS, Reynolds EOR 1995 Mild hypothermia after severe transient hypoxia-ischemia ameliorates delayed cerebral energy failure in the newborn piglet. Pediatr Res 37: 667–670.
Amess PN, Penrice J, Cady EB, Lorek A, Wylezinska M, Cooper CE, D'Souza P, Tyszczuk L, Thoresen M, Edwards AD, Wyatt JS, Reynolds EOR 1997 Mild hypothermia after severe transient hypoxia-ischemia reduces the delayed rise in cerebral lactate in the newborn piglet. Pediatr Res 41: 803–808.
Thoresen M, Bågenholm R, Loberg EM, Apricena F, Kjellmer I 1996 Posthypoxic cooling of neonatal rats provides protection against brain injury. Arch Dis Child 74: F3–F9
Sirimanne ES, Blumberg RM, Bossano D, Gunning M, Edwards AD, Gluckman PD, Williams CE 1996 The effect of prolonged modification of cerebral temperature on outcome after hypoxic-ischemic brain injury in the infant rat. Pediatr Res 39: 591–597.
Laptook AR, Corbett RJT, Sterett R, Burns DK, Tollefsbol G, Garcia D 1994 Modest hypothermia provides partial neuroprotection for ischemic neonatal brain. Pediatr Res 35: 436–442.
Yager J, Towfighi J, Vannucci RC 1993 Influence of mild hypothermia on hypoxic-ischemic brain damage in the immature rat. Pediatr Res 34: 525–529.
Trescher WH, Ishiwa S, Johnston MV 1997 Brief post-hypoxic-ischemic hypothermia markedly delays neonatal brain injury. Brain Dev 19: 326–338.
Gunn AJ, Gunn TR, de Haan HH, Williams CE, Gluckman PD 1997 Dramatic neuronal rescue with prolonged selective head cooling after ischemia in fetal lambs. J Clin Invest 99: 248–256.
Laptook AR, Corbett RJT, Sterett R, Burns DK, Garcia D, Tollefsbol G 1997 Modest hypothermia provides partial neuroprotection when used for immediate resuscitation after brain ischemia. Pediatr Res 42: 17–23.
Laptook AR, Corbett RJT, Burns D, Sterett R 1995 Neonatal ischemic neuroprotection by modest hypothermia is associated with attenuated brain acidosis. Stroke 26: 1240–1246.
Leonov Y, Sterz F, Safar P, Radovsky A, Oku K, Tisherman S, Stezoski SW 1990 Mild cerebral hypothermia during and after cardiac arrest improves neurologic outcome in dogs. J Cereb Blood Flow Metab 10: 57–70.
Corbett RJT, Laptook AR, Nunnally RL 1987 The use of the chemical shift of the phosphomonoester P-31 magnetic resonance peak for the determination of intracellular pH in the brains of neonates. Neurology 37: 1771–1779.
Stephenson JM, Du JN, Oliver TK 1970 The effect of cooling on blood gas tension in newborn infants. J Pediatr 76: 848–852.
Gandy GM, Adamsons K, Cunningham N, Silverman WA, James LS 1964 Thermal environment and acid-base homeostasis in human infants during the first few hours of life. J Clin Invest 43: 751–758.
Cornblath M, Schwartz R 1976 Hypoglycemia associated with neonatal cold injury, In: Schaffer AJ, Markowitz M (eds), Disorders of Carbohydrate Metabolism in Infancy. WB Saunders, Philadelphia, 166–67.
Rohrer MJ, Natale AM 1992 Effect of hypothermia on the coagulation cascade. Crit Care Med 20: 1402–1405.
van Oss CJ, Absolom DR, Moore LL, Park BH, Humbert JR 1980 Effect of temperature on the chemotaxis, phagocytic engulfment, digestion and O2 consumption of human polymorphonuclear leukocytes. J Reticuloendothel Soc 27: 561–565.
Busto R, Dietrich WD, Globus MYT, Ginsberg MD 1989 Postischemic moderate hypothermia inhibits CA1 hippocampal ischemic neuronal injury. Neurosci Lett 101: 229–304.
Kuboyama K, Safar P, Radovsky A, Tisherman SA, Stezoski SW, Alexander H 1993 Delay in cooling negates the beneficial effect of mild resuscitative cerebral hypothermia after cardiac arrest in dogs: a prospective, randomized study. Crit Care Med 21: 1348–1358.
Fazekas JF, Alexander AD, Himwich HE 1941 Tolerance of the newborn to anoxia. Am J Physiol 134: 281–287.
Duffy TE, Kokle SJ, Vannucci RC 1975 Carbohydrate and energy metabolism in perinatal rat: relation to survival in anoxia. J Neurochem 24: 271–276.
Corbett RJT, Laptook AR, Garcia D, Ruley J 1993 Energy reserves and utilization rates in developing brain measured in vivo by 31P and 1H nuclear magnetic resonance spectroscopy. J Cereb Blood Flow Metabol 13: 235–246.
Pulsinelli WA, Waldman S, Rawlinson D, Plum F 1982 Moderate hyperglycemia augments ischemic brain damage: A neuropathologic study in the rat. Neurology 32: 1239–1246.
Siesjo BK 1985 Acid-base homeostasis in the brain: physiology, chemistry and neurochemical pathology. Prog Brain Res 63: 121–154.
Vannucci RC, Vasta F, Vannucci SJ 1987 Cerebral metabolic responses of hyperglycemic immature rats to hypoxia-ischemia. Pediatr Res 21: 524–529.
Voorhies TM, Rawlinson D, Vannucci RC 1986 Glucose and perinatal hypoxic-ischemic brain damage in the rat. Neurology 36: 1115–1118.
Corbett RJT, Laptook AR, Ruley JI, Garcia D 1991 The effect of age on glucose-modulated cerebral agonal glycolytic rates measured in vivo by 1H NMR spectroscopy. Pediatr Res 30: 579–586.
Corbett R, Laptook A, Kim B, Tollefsbol G, Silmon S, Garcia D 1999 Maturational changes in cerebral lactate and acid clearance following ischemia measured in vivo using magnetic resonance spectroscopy and microdialysis. Dev Brain Res 113: 37–46.
Coimbra C, Wieloch T 1994 Moderate hypothermia mitigates neuronal damage in the rat brain when initiated several hours following transient cerebral ischemia. Acta Neuropathol 87: 325–331.
Colbourne F, Corbett D 1994 Delayed and prolonged post-ischemic hypothermia is neuroprotective in the gerbil. Brain Res 654: 265–272.
Gunn AJ, Gunn TR, Gunning MI, Williams CE, Gluckman PD 1998 Neuroprotection with prolonged head cooling started before postischemic seizures in fetal sheep. Pediatrics 102: 1098–1106.
Marks JD, Friedman JE, Haddad GG 1996 Vulnerability of CA1 neurons to glutamate is developmentally regulated. Dev Brain Res 97: 194–206.
Lorek A, Takei Y, Cady EB, Wyatt JS, Penrice J, Edwards AD, Peebles D, Wylezinska M, Owen-Reece H, Kirkbride V, Cooper CE, Aldridge RF, Roth SC, Brown G, Delpy DT, Reynolds EOR 1994 Delayed (“secondary”) cerebral energy failure after acute hypoxia-ischemia in the newborn piglet: continuous 48-hour studies by phosphorus magnetic resonance spectroscopy. Pediatr Res 36: 699–706.
Thoresen M, Satas S, Puka-Sundvall M, Whitelaw A, Hallstrom A, Loberg EM, Ungerstedt U, Steen PA, Hagberg H 1997 Post-hypoxic hypothermia reduces cerebrocortical release of NO and excitotoxins. Neuroreport 8: 3359–3362.
Mehmet H, Yue X, Squier MV, Lorek A, Cady E, Penrice J, Sarraf C, Wylezinska M, Kirkbride V, Cooper C, Brown GC, Wyatt JS, Reynolds EOR, Edwards AD 1994 Increased apoptosis in the cingulate sulcus of newborn piglets following transient hypoxia-ischemia is related to the degree of high energy phosphate depletion during the insult. Neuroscience Lett 181: 121–125.
Tan WKM, Williams CE, During MJ, Mallard CE, Gunning MI, Gunn AJ, Gluckman PD 1996 Accumulation of cytotoxins during the development of seizures and edema after hypoxic-ischemic injury in late gestation fetal sheep. Pediatr Res 39: 791–797.
Bona E, Hagberg H, Løberg EM, Bågenholm R, Thoresen M 1998 Protective effects of moderate hypothermia after neonatal hypoxia-ischemia: : short-and long-term outcome. Pediatr Res 43: 738–745.
Yager JW, Armstrong E 1998 The effect of brief post-hypoxia hypothermia in combination with neuroprotective agents on hypoxic-ischemia brain damage in the immature rat. Pediatr Res 43: 325A
Hope PL, Cady EB, Tofts PS, Hamilton PA, de L Costello AM, Delpy DT, Chu A, Reynolds EOR, Wilkie DR 1984 Cerebral energy metabolism studied with phosphorus NMR spectroscopy in normal and birth-asphyxiated infants. Lancet 2: 366–369.
Author information
Authors and Affiliations
Additional information
Supported by the United Cerebral Palsy Research and Education Foundation, Inc., the Southwestern Biomedical Magnetic Resonance Facility, National Institutes of Health Grant P41-RR02584 and the Department of Pediatrics, UT-Southwestern Medical Center at Dallas.
Rights and permissions
About this article
Cite this article
Laptook, A., Corbett, R., Burns, D. et al. A Limited Interval of Delayed Modest Hypothermia for Ischemic Brain Resuscitation Is Not Beneficial in Neonatal Swine. Pediatr Res 46, 383 (1999). https://doi.org/10.1203/00006450-199910000-00005
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199910000-00005
This article is cited by
-
Therapeutic hypothermia translates from ancient history in to practice
Pediatric Research (2017)
-
Comparison of Three Hypothermic Target Temperatures for the Treatment of Hypoxic Ischemia: mRNA Level Responses of Eight Genes in the Piglet Brain
Translational Stroke Research (2013)