Abstract
Cerebral blood flow (CBF) measurement by near infrared spectroscopy (NIRS) using oxyhemoglobin (Hbo2) as a tracer (CBF-Hbo2) needs rapid changes in arterial oxygen saturation (Sao2) which often cannot be achieved in many sick infants. An alternative method based on the same adaptation of the Fick principle using i.v. injection of the dye indocyanine green (ICG) is described (CBF-ICG). Six mechanically ventilated infants (age 26-38 wk, birth weight 0.885-3.730 kg) requiring supplementary oxygen therapy were studied within 72 h of birth. For CBF-ICG measurements, ICG (0.1 mg·kg-1 was injected via an umbilical venous catheter, and blood ICG concentration was measured by an optical umbilical artery catheter and brain ICG concentration was measured by NIRS. For CBF-HbO2 measurements the inspired oxygen concentration was rapidly increased, blood Hbo2 concentration was calculated from Sao2 measured by pulse oximetry, and brain Hbo2 concentration was measured by NIRS. A series of CBF measurements were performed using each method before and after altering the arterial carbon dioxide tension (Paco2). Mean CBF values from repeated measurements by each method at any given Paco2 were used to compare the methods. The SD of single measurements within an individual subject by CBF-ICG was 15%, and by CBF-HbO2, 24%. The relationship between the methods was mean CBF-ICG = (1.13. mean CBF-HbO2) - 2.76 mL·100 g-1·min-1 Hbo2 (r = 0.93, p< 0.001). The mean difference between the methods (CBF-ICG - CBF-Hbo2) was -0.25 mL·100 g-1·min-1 (95% confidence interval 6.30 to -6.80). The methods were in good agreement, and the use of i.v. ICG permitted rapid and repeated CBF measurements in the sickest infants at greatest risk of cerebral injury.
Similar content being viewed by others
Main
The measurement of CBF in sick newborn infants is of considerable interest as abnormal perfusion plays an important role in the development of cerebral injury(1–3). Xenon-133 clearance, positron emission tomography, and NIRS using Hbo2 as a tracer (CBF-Hbo2) have been used for quantitative CBF measurements and provided valuable information(4–6). However, 133Xe and positron emission tomography expose the infant to ionizing radiation, and CBF-Hbo2 requires a rapid change in Sao2, which often cannot be achieved in infants with severe respiratory insufficiency, in whom CBF measurements would probably be of most value.
We describe an alternative method using NIRS with ICG as an intravascular tracer (CBF-ICG), which should allow rapid and repeated measurements of CBF in almost all newborn infants. CBF-ICG is based on the same adaptation of the Fick principle as the validated CBF-Hbo2 method but uses i.v. administration of the dye ICG(4–7). This dye strongly absorbs near infrared light and is rapidly cleared from the body. It has been used for many years in children and adults and shown to be safe(8, 9). In this study we measured CBF values in the same infants using both CBF-ICG and CBF-Hbo2 and compared values.
METHODS
Subjects. Six newborn infants of gestational age range 26-38 wk(median 28 wk) and birth weight 0.885-3.730 kg (median 1.080 kg) were studied at postnatal age 10-60 h (median 25 h). All subjects were receiving intermittent positive pressure ventilation with the fractional inspired oxygen concentration ranging between 33 and 72% (median 60%). No infant had an abnormal cranial ultrasound scan, congenital cardiac disease, or jaundice severe enough to require phototherapy. Written parental consent was obtained for all infants, and the study was approved by the Hammersmith Hospitals Research Ethics Committee.
Theory. NIRS. The principles of NIRS have been described in detail before. Changes in the attenuation of near infrared light are used to calculate changes in the concentration of major near infrared-absorbing compounds in vivo. These include the endogenous compounds Hbo2 and Hb, and the exogenous dye ICG. The absorption coefficients of these compounds are known, allowing concentration changes to be calculated using the modified Beer-Lambert law.
Measurement of cerebral blood flow using NIRS. Both CBF-Hbo2 and CBF-ICG are based on the Fick principle, which states that the accumulation (Q) of tracer substance in an organ is equal to the difference between the rate of arrival and the rate of departure of that substance. If a substance is suddenly introduced into the arterial blood, a measurement of the amount accumulated in the organ can be made at a specific time (t) later. When t is less than the transit time through the organ, the tracer will not appear in the venous blood, and if measurements are made in a period shorter than the transit time through the organ, then flow (F) can be calculated as the ratio of tracer accumulated to the quantity of tracer introduced during time t. This quantity is equal to the integral of the arterial concentration of tracer(Pa) at time t (Pa[t]) with respect to time. Thus F =(Q(t)/0∫t(Pa)dt).
For CBF-Hbo2 measurements a change in Hbo2 concentration is used as a tracer(6). When a sudden increase occurs in Sao2, the initial increase in cerebral Hbo2 concentration represents the accumulation of tracer. The quantity introduced is given by the product of the integral of ΔSao2 with respect to time and the arterial total hemoglobin concentration [total Hb]. Thus CBF-Hbo2(mL·100 g-1·min-1) =(K1·Δ[Hbo2])/[total Hb]·∫0t(ΔSao2)dt), where K1 is a constant reflecting the molecular weight of hemoglobin (64 500) and cerebral tissue density (1.05).
When the total cerebral hemoglobin concentration is constant, it may be assumed that the changes in Hbo2 and Hb concentration are equal and opposite. The signal representing the difference between the change in Hbo2 and Hb concentration is thus twice the amplitude of the corresponding signal representing the change in Hbo2 concentration. To improve the signal-to-noise ratio of the NIRS data, the above equation can therefore be modified to: CBF-HbO2 (mL·100 g-1·min-1) = (K1·Δ([Hbo2] -[Hb])/2. [total Hb]·∫0t(ΔSao2)dt).
For CBF-ICG measurements a change in ICG concentration is used as a tracer. When a sudden increase occurs in arterial ICG concentration, the initial increase in cerebral ICG concentration represents the accumulation of tracer. The quantity introduced is given by the integral of the change in arterial blood ICG concentration with respect to time. Thus CBF-ICG (mL·100 g-1·min-1) = (K2·Δ[cerebral blood ICG])/∫0t(Δ[arterial blood ICG]dt), where K2 is a constant reflecting the molecular weight of ICG (925) and cerebral tissue density.
Experimental procedure. Optodes placed biparietally on the head at least 3.5 cm apart allowed changes in cerebral Hbo2 and ICG concentration to be measured every 0.5 s by NIRS (NIRO 500, Hammamatsu, Japan). The optical path length was taken as 4.39 times the interoptode distance(10).
CBF-Hbo2 was measured as described previously(6). Sao2 was measured by a pulse oximeter in the beat to beat mode sited on the right hand. After a period when Hbo2 and Sao2 were stable a sudden transient increase in Sao2 was induced by increasing the inspired oxygen concentration for a few breaths.
For CBF-ICG measurements 0.5 mL of the infants blood was withdrawn and mixed with 0.5 mL (0.1 mg·kg-1) of ICG (Pulsion-green, Pulsion, Munich, Germany) dissolved in water. After a period of 15 s to allow binding of dye to plasma proteins, the solution was injected as a bolus through a 5 F umbilical venous catheter with its tip in the right atrium. Changes in arterial concentration of ICG were measured every 0.5 s using a 4 FG fiberoptic catheter (model IVH 4, Pulsion) positioned in the descending aorta via an umbilical artery. The sample volume of the catheter is of the order of microliters because blood absorbs light at these wavelengths strongly. Correct placement of catheters was confirmed radiologically and by ultrasonography. Their function was checked before making a series of CBF-ICG measurements by an initial test injection of dye.
A series between three and five CBF measurements was made using one method, and then using the other method (paired series). Paco2 was then altered, by changing the ventilator rate or by adding ventilatory dead space. After a minimum stabilization period of 30 min, further paired series of CBF measurements were performed, and the procedure was repeated. The initial method used in each paired series of CBF measurements and the initial direction of Paco2 change were selected randomly.
Heart rate, transcutaneous oxygen, and carbon dioxide tensions were recorded continuously. Mean arterial blood pressure was monitored via an umbilical arterial catheter. Arterial sampling was performed to determine hemoglobin concentration at the beginning of the study, glucose values at the beginning of each paired series of CBF measurements, and blood pH, oxygen(PaO2), and carbon dioxide (Paco2) tensions at the beginning and the end of each paired series.
Data analysis. Analyses of CBF data were based on predetermined criteria. CBF-HbO2 measurements were rejected if baseline SaO2 varied >2% in the 10 s before the increase, a change in Sao2 of≥4% was not achieved within 4 s, cerebral ([HbO2] +[Hb])/([HbO2] - [Hb]) changed >30% during the measurement, or if the time delay between the points where SaO2 and cerebral HbO2 start to rise was >4 s.
CBF-ICG measurements were rejected if arterial ICG concentration varied by>0.5 mg·L-1 in the 10 s before the increase, a clear change of 0.1 μmol·L-1 in cerebral ICG concentration and 5 mg·L-1 in arterial ICG concentration was not achieved within 6 s, or if the time delay between the points where arterial and cerebral ICG concentrations start to rise was >4 s.
An integration time of 6 s was used for calculating CBF with both methods. Mean CBF-ICG and mean CBF-HbO2 values at the different Paco2 levels from each of the paired series of measurements were compared by linear regression analysis and then by plotting the difference between a pair of values against their mean as suggested by Bland and Altman(11).
The CBF response to alterations in Paco2 (CBF-CO2 reactivity) was calculated for both methods by linear regression analysis using dummy variables, both before and after logarithmic transformation. Data analysis was repeated using individual data points, which also permitted estimation of the intrasubject SD of individual measurements, through calculation of the root mean square error.
Statistical calculations were performed using both SPSSPC (SPSS Inc., Chicago, IL) and Stata (Stata Corporation, College Station, TX). A p value less than 0.05 was considered significant.
RESULTS
The ranges for the measured variables during the study were heart rate 120-160 min-1, mean arterial blood pressure 31-49 mm Hg, SaO2 85-98%, arterial pH 7.21-7.44, PaO2 7.2-12.2 kPa, Paco2 4.0-6.8 kPa, blood glucose 4.1-9.9 mmol·L-1, and arterial hemoglobin 14.2-16.6 g·dL-1.
Paco2 changed by -0.2 to 0.5 kPa (median 0.3) between the beginning and the end of each of the paired series of CBF measurements. Transcutaneous CO2 tension fluctuation during any of the measured series ranged between 0.3 and 0.5 kPa (median 0.3 kPa).
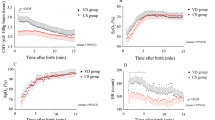
Thirty-five of 78 CBF-HbO2 and 7 of 63 CBF-ICG measurements did not meet the quality criteria. However, at least two determinations of CBF were successful in each series of measurements. A typical CBF-ICG determination is shown in Figure 1. The time interval between CBF measurements in any series using the HbO2 method ranged between 3 and 8 min (median 5 min) and for the ICG method 2-7 min (median 3).
Change in cerebral and arterial ICG concentration after injection into the right atrium. ICG injected as a bolus at time = 0 s. CBF calculated by relating increase in cerebral ICG concentration (Q) to the time integral of arterial concentration(∫0t(Pa)dt) over the first 6 s after appearance of dye in each optical field.
The mean CBF value obtained by repeated measurement by each method at any given Paco2 was used to compare the methods. There was a significant correlation between the two techniques (r = 0.93, p < 0.001) (Fig. 2). The relationship between the methods was mean CBF-ICG = (1.13·mean CBF-HbO2) - 2.76 mL·100 g-1·min-1. Analysis of single paired data gave similar results.
The Bland-Altman plot is shown in Figure 3. The mean difference between the methods was -0.25 mL·100 g-1·min-1 (95% CI 6.30 to -6.80). There was a trend toward lower CBF-HbO2 values compared with CBF-ICG values with increasing CBF (slope = 0.20), but this was not significant.
Bland-Altman plot showing differences between mean CBF-ICG and CBF-Hbo2 values vs their average. Data calculated from mean CBF values from repeated measurements using each method at any given Paco2 level. Six infants each denoted by a unique symbol. The mean difference between the methods (- - -) was -0.25 mL·100 g-1·min-1 (95% CI 6.30 to -6.80).
The relationship between mean CBF-ICG and Paco2 for each infant is shown in Figure 4. The overall CBF-CO2 reactivity for the six infants using CBF-ICG was 4.59 mL·100 g-1·min-1·kPa-1 (95% CI 1.95-7.23), and for CBF-HbO2 3.94 mL·100 g-1·min-1·kPa-1 (95% CI 1.08-6.80). The CBF-CO2 reactivities expressed percentually were 31.0%·kPa-1 (95% CI 19.8-42.2) and 21.0%·kPa-1(95% CI 6.0-36.0), respectively.
Analysis of individual data did not show any significant differences from the calculations employing mean data. However, this analysis allowed the additional calculation of the root mean square error of individual data, which showed that single CBF-ICG measurements were distributed with a SD of 15%, and CBF-HbO2, 24%.
DISCUSSION
This study demonstrated that CBF can be measured using ICG. ICG has been used in clinical practice for many years in both term and preterm infants without reports of significant toxic effects. As very small quantities of ICG are required some 50 estimations of CBF can be performed before the maximum permitted dose is reached. A much higher proportion of determinations was successful with CBF-ICG than with CBF-HbO2. Using CBF-ICG it is also possible to make CBF measurements in infants with severe respiratory impairment.
CBF-ICG gives similar results to CBF-HbO2, which has previously been shown to give comparable results to those obtained using 133Xe clearance(4, 7). The CBF values obtained in this study are similar to those previously obtained with 133Xe clearance and positron emission tomography(4, 5). There was also a trend toward slightly lower values with increasing flow rates using CBF-HbO2, similar to that seen in one study comparing CBF-HbO2 with 133Xe clearance(4).
NIRS measurements of CBF are made within 10-20 s and easily repeatable. Thus, unlike most other techniques, its usual practice is to make multiple measures for every clinical estimation. Consequently this study was designed to test repeated CBF measures and the statistical analysis performed of mean data. However, when individual data were analyzed, similar results were obtained, and this analysis additionally allowed the calculation of the SD of an individual CBF measurement by either technique. For CBF-ICG this was 15%, much lower than for CBF-HbO2. A significant proportion of intrasubject variance may be attributed to alterations in Paco2, as despite close attention to experimental protocols Paco2 varied by a median of 0.3 kPa, which could be expected to change CBF by about 10%.
Both NIRS techniques consistently demonstrated an appropriate physiologic response to changes in Paco2. Logarithmic transformation of mean CBF values was performed for determination of percentual CBF-CO2 reactivity, thus assuming a log-linear relation between CBF and Paco2. Dummy variables were used to account for interindividual variation in CBF and thus the estimated regression coefficient depended only on intraindividual variance.
The CBF-ICG and CBF-HbO2 methods share certain assumptions. First the period of measurement (t) must be less than the cerebral transit time. Although the cerebral transit time was not measured in this study, an previous study using labeled erythrocytes estimated a mean value of 8 s(12).
Second, during measurement CBF and cerebral hemoglobin concentration must remain constant, and for CBF-HbO2 the cerebral oxygen extraction must also remain constant. Studies in animals and human subjects have shown that CBF and oxygen extraction do not change significantly within the PaO2 range of 6 to 13 kPa(13, 14). There are no data to suggest that ICG causes cerebral vasoconstriction or vasodilation, and ICG has been used for cardiovascular measurements for many years(8, 9).
There have been concerns that hyperoxia induced during CBF-HbO2 measurements may alter cerebral hemodynamics. NIRS allows quantification of cerebral hemoglobin concentration from observation of the sum of [HbO2] and [Hb] signals, thus CBF-HbO2 measurements in which there was a change in [HbO2] + [Hb], suggesting a vasoactive effect can be excluded from analyses. However, this was not observed in the present study.
Large right to left shunts pose a theoretical problem with both methods. The measured arterial concentration of tracer may not accurately reflect the concentration in the cerebral blood supply. In the case of right to left shunting through a patent ductus arteriosus for example, the oxygen saturation in the right and left carotid arteries may be different because of variable contribution by deoxygenated blood shunted through the patent ductus arteriosus, which is positioned between the two. Sao2 measured on the right hand may then be used as a surrogate measure for monitoring the Sao2 in the right carotid but not the left carotid. Shunting through a patent ductus arteriosus is assumed to be small if the Sao2 on the right hand and foot are similar.
In the case of CBF-ICG measurement with a large right to left ductal shunt, the arterial ICG signal measured via a catheter in the descending aorta may be anticipated to demonstrate a large early rise in the ICG signal, before the arrival of blood that has been through the pulmonary circulation and the left side of the heart. Theoretically this would lead to an overestimation of the quantity of ICG introduced into the cerebral circulation during a CBF measurement, and an underestimation of CBF. Such changes were not seen in any of the subjects.
Arterial injection of ICG into the cardiopulmonary bypass circuit proximal to its insertion into the aorta in humans(15), and into the carotid artery in animals(16), has been used to measure CBF. However, this is the first study to inject the dye into the central venous circulation. An advantage of this method is that the dye is injected through a catheter that is easy to place, and which is often inserted for clinical purposes. A practical problem relates to the need for insertion of a catheter specifically for measurement of arterial ICG concentration. This difficulty may be overcome by the use of a lumened, dual purpose indwelling catheter, that also permits blood sampling and blood pressure monitoring, which is currently being evaluated, or possibly by the use of a device similar to a pulse oximeter that detects ICG (M. Wolff, personal communication). However, no complications due to the ICG measurement catheter were observed.
Important information in addition to CBF measurements may be possible using ICG. CBV can be measured by relating brain and arterial ICG concentrations in a manner analogous to that using Hbo2(17). Repeated plasma volume estimations by the dye dilution method should also be possible without the need for blood sampling, as the quantity of ICG injected is known, and the arterial concentration is measured in situ. ICG has been used previously to measure plasma volume, but only a limited number of measurements could be performed due to the need for repeated blood sampling(18). Fluid management in sick infants may thus be considerably improved.
Abnormalities of CBF are important in the pathogenesis of cerebral ischemia and hemorrhage, which are the commonest causes of permanent neurodevelopmental disability in infants who need intensive care. The new method described here should allow measurements of CBF in most newborn infants, including those with severe respiratory insufficiency who are at high risk of brain injury. As repeated measurements can be performed rapidly, this technique could considerably improve the investigation of cerebral perfusion, and in particular the role of short-term transients in CBF in the pathogenesis of brain injury.
Abbreviations
- CBF:
-
cerebral blood flow
- Hb:
-
deoxyhemoglobin
- Hbo2:
-
oxyhemoglobin
- ICG:
-
indocyanine green
- CBF-ICG:
-
CBF measured using ICG
- CBF-Hbo2:
-
CBF measured using Hbo2
- CI:
-
confidence interval
- NIRS:
-
near infrared spectroscopy
- Paco2:
-
arterial carbon dioxide tension
- Sao2:
-
arterial oxygen saturation
References
Pape KE, Wigglesworth JS 1979 Haemorrhage, Ischaemia and the Perinatal Brain. Heinemann, London, pp 100–133
Volpe JJ, ed 1994 Hypoxic-ischemic encephalopathy: neuropathology and pathogenesis. In: Neurology of the Newborn. WB Saunders, Philadelphia, pp 279–313
Volpe JJ, ed 1994 Intracranial hemorrhage: germinal matrix-intraventricular hemorrhage. In: Neurology of the Newborn. WB Saunders, Philadelphia, pp 403–463
Skov L, Pryds O, Greisen G 1991 Estimating cerebral blood flow in newborn infants: comparison of near infrared spectroscopy and133 xenon clearance. Pediatr Res 30: 570–573
Volpe JJ, Herscovitch P, Perlman JM, Raichle ME 1983 Positron emission tomography in the newborn: extensive impairment of regional cerebral blood flow with intraventricular hemorrhage and hemorrhagic intracerebral involvement. Pediatrics 72: 589–601
Edwards AD, Wyatt JS, Richardson C, Delpy DT, Cope M, Reynolds EOR 1988 Cotside measurement of cerebral blood flow in ill newborn infants by near infrared spectroscopy. Lancet 2: 770–771
Bucher HU, Edwards AD, Lipp AE, Duc G 1993 Comparison between near infrared spectroscopy and 133xenon clearance for estimation of cerebral blood flow in critically ill preterm infants. Pediatr Res 33: 56–60
Niggemann EH, Ma PT, Sunnergreen KP, Winniford MD, Hillis LD 1987 Detection of intracardiac left-to-right shunting in adults: a prospective analysis of the variability of the standard indocyanine green technique in patients without shunting. Am J Cardiol 60: 355–357
Anderson PA, Bowyer KW, Jones RH 1984 Effects of age on radionuclide angiographic detection and quantitation of left-to-right shunts. Am J Cardiol 53: 879–883
Wyatt JS, Cope M, Delpy DT, van der Zee P, Arridge SR, Edwards AD, Reynolds EOR 1990 Measurement of optical pathlength for cerebral near infrared spectroscopy in newborn infants. Dev Neurosci 12: 140–144
Bland JM, Altman DG 1986 Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1: 307–310
Arnot RN, Glass HI, Clark JC 1970 Methods of measurement of cerebral blood flow in the newborn infant using cyclotron-produced isotopes. Radioaktive Isotope in Klinik und Forcshung 9: 60–74
Siesjo BK 1978 Brain Energy Metabolism. Wiley, Chichester, pp 422–426
Kogure K, Scheinberg P, Reinmuth OM, Fujishima M, Busto R 1970 Mechanism of cerebral vasodilatation in hypoxia. J Appl Physiol 29: 223–229
Roberts I, Fallon P, Kirkham FJ, Lloyd-Thomas A, Cooper C, Maynard R, Elliot M, Edwards AD 1993 Estimation of cerebral blood flow with near infrared spectroscopy and indocyanine green. Lancet 342: 1425
Colacino JM, Grubb B, Jobsis FF 1981 Infra-red method for cerebral blood flow: comparison with 133Xenon clearance. Neurol Res 3: 17–31
Wyatt JS, Cope M, Delpy DT, Richardson C, Edwards AD, Wray SC, Reynolds EOR 1990 Quantitation of cerebral blood volume in newborn infants by near infrared spectroscopy. J Appl Physiol 68: 1086–1091
Anthony MY, Goodall SR, Papouli M, Levene MI 1992 Measurement of plasma volume in neonates. Arch Dis Child 67: 36–40
Acknowledgements
The authors thank the staff of the Neonatal Units at Hammersmith Hospital and Queen Charlotte's and Chelsea Hospital, Dr. C. Cooper for providing the absorption coefficients for ICG, Dr. O. Pryds for statistical advice. We also thank Hammamatsu Photonics and Pulsion Medizintechnik.
Author information
Authors and Affiliations
Additional information
Supported by the British Heart Foundation (J.P., I.R.).
Rights and permissions
About this article
Cite this article
Patel, J., Marks, K., Roberts, I. et al. Measurement of Cerebral Blood Flow in Newborn Infants Using Near Infrared Spectroscopy with Indocyanine Green. Pediatr Res 43, 34–39 (1998). https://doi.org/10.1203/00006450-199801000-00006
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199801000-00006
This article is cited by
-
Quantitative regional cerebral blood flow measurement using near-infrared spectroscopy and indocyanine green in patients undergoing superficial temporal to middle cerebral artery bypass for moyamoya disease: a novel method using a frequency filter
Journal of Clinical Monitoring and Computing (2023)
-
Brain Oximetry and the Quest for Quantified Metabolic Rate: Applications Using MRI and Near-Infrared Spectroscopy
Applied Magnetic Resonance (2021)
-
Preservation of the metabolic rate of oxygen in preterm infants during indomethacin therapy for closure of the ductus arteriosus
Pediatric Research (2013)
-
Near-Infrared Spectroscopy Assessment of Cerebral Oxygen Metabolism in the Developing Premature Brain
Journal of Cerebral Blood Flow & Metabolism (2012)
-
Measurement of Cerebral Oxidative Metabolism with Near-Infrared Spectroscopy: A Validation Study
Journal of Cerebral Blood Flow & Metabolism (2006)