Abstract
We examined the effect of acute systemic blockade of nitric oxide synthesis on blood pressure and renal function in the monogenetically hypertensive TGR(mRen2)27 rat strain. Untreated conscious transgenic rats had significantly(p < 0.01) higher systolic blood pressures (185 ± 9versus 130 ± 5 mm Hg) and urinary albumin excretion (32± 5 versus 6 ± 2 mg/day) than did control animals without evidence of renal insufficiency. Plasma and urinary nitric oxide metabolite levels did not differ between transgenic and control rats. i.v. administration of NG-nitro-L-arginine methyl ester (10 mg/kg) to both groups caused similar elevations in systemic blood pressure(transgenic 25 ± 3 versus control 24 ± 3 mm Hg). NG-Nitro-L-arginine methyl ester induced reductions in whole kidney (1.4 ± 0.2 versus 0.7 ± 0.1 mL/min), and single nephron (23 ± 3 versus 11 ± 2 nL/min) glomerular filtration rates were significantly (p < 0.05) larger in transgenic than in control rats. This greater loss of GFR in transgenic animals was caused by a larger reduction in glomerular ultrafiltration coefficient (1.8 ± 0.2 versus 1.1 ± 0.1 nL·min-1·mm Hg-1, p < 0.05), a larger increase in afferent arteriole resistance (3.4 ± 0.2 versus 1.4 ± 0.1 dyne·s·cm-5, p < 0.05), and a subsequently smaller rise in glomerular transcapillary pressure (10 ± 1 versus 5 ± 1 mm Hg, p < 0.05). These results indicate that the renal microvasculature and glomerular hydraulic conductivity or surface area of transgenic rats are more sensitive to nitric oxide inhibition and are consistent with an important role for nitric oxide in TGR(mRen2)27 kidney function.
Similar content being viewed by others
Main
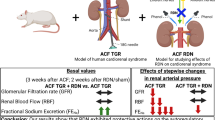
The TGR(mRen2)27 rat strain (TGR) is a new model of genetic hypertension produced by inserting the mouse ren-2 gene complete with flanking control regions into the rat genome(1). These transgenic animals develop high blood pressure early in life with the severity of their hypertension dependent on transgene zygosity. Systolic blood pressures of rats heterozygous for the mouse renin transgene are ≈200 mm Hg, whereas pressures of homozygous animals approach 300 mm Hg.
Although these animals' hypertension clearly relates to the presence of the mouse renin gene, the mechanisms responsible for elevating blood pressure are unclear. Studies of the circulating renin-angiotensin system in TGR have produced conflicting results that vary with age, zygosity, anesthesia, and analytical methods(1–3). Recent evidence suggests that these animals could be a high mouse renin model of hypertension due to the enhanced reaction between mouse renin and rat angiotensinogen(4, 5). Alternatively, the pathogenesis of high blood pressure in TGR could relate to tissue-specific renin-angiotensin systems. Markedly enhanced adrenal cortical transgene expression, elevated adrenocorticosteroid levels, and suppression of hypertension by dexamethasone suggest an important contribution from an adrenal renin-angiotensin system(1, 6). Regardless of the cause of their hypertension, these animals provide a unique opportunity to compare genotype with phenotype. Because phenotypic differences in this strain can be related to the presence or absence of the mouse renin transgene, the physiologic consequences of a specific genetic change can be accurately studied in vivo.
It is generally accepted that the nitric oxide (NO) system plays an important role in the regulation of systemic and renal hemodynamics(7). Dysfunction of this system may be involved in the pathogenesis of hypertension and hypertensive renal disease(8). For example, chronic inhibition of NO synthesis with L-NAME causes severe hypertension and progressive glomerulosclerosis, whereas administration of the NO precursor L-arginine can ameliorate hypertension and correct blunted pressure-natriuresis responses(9, 10). Currently, there is limited and conflicting information about the NO system in TGR, none of which is specific to renal function. Tschudi et al.(11) have reported that vessels isolated from TGR(sex not reported) do not demonstrate increased basal or stimulated NO release. In contrast, injection of the NO synthesis inhibitor NG-monomethyl-L-arginine caused a substantially larger increase in systemic blood pressure in female transgenic than control animals, suggesting increased production of or sensitivity to NO(12, 13). The pressor reaction of female TGR to NO synthesis inhibition is significantly attenuated by pretreatment with lisinopril or losartan(12). This response is contrary to that of normal female rats(12) and implies a unique role for the TGR RAS in this interaction. These results are clouded by studies showing that estrogen is responsible for the enhanced NO activity in female TGR(13). It is therefore not clear if the potential importance of NO in TGR is a sex- or strain-dependent finding. In this investigation, we examined the effect of acute systemic blockade of NO with L-NAME on blood pressure and renal function in anesthetized male TGR.
METHODS
Experiments were performed on eight 6-mo-old male TGR heterozygous for the mouse ren-2 renin gene and eight age-matched Sprague-Dawley Hannover control rats obtained from Moellegaard Breeding Center GmbH, Schoenwalde, Germany. Rats from this strain served as oocyte donors and mates for the development of TGR. Animals were maintained on standard 24% protein rat chow and water ad libitum. The experimental protocol was approved by our institutional animal care committee.
Indirect systolic blood pressure was measured in unanesthetized rats by a tail-cuff method (Narco Biosystems, Houston, TX). Urine was collected from animals kept in metabolism cages for 16 h with free access to water but deprived of food. Blood samples were obtained from the tail vein at the end of collection periods. Plasma sodium and creatinine concentrations and urinary sodium, creatinine, albumin, and NOX (nitrite + nitrate) excretion were determined from these samples.
After the above measurements, the same rats were anesthetized with Inactin(80 mg/kg i.p.) and prepared for renal clearance and micropuncture studies as previously described(14). Isotonic saline containing tritiated inulin (1 mCi/mL) and PAH (0.1 g/dL) was given as a bolus injection(0.5% body weight) followed by continuous infusion at 0.6 mL·h-1·100 g body weight-1. After 30 min of equilibration, a 45-60-min urine collection was performed with a 0.2-mL arterial blood sample obtained at the urine collection midpoint. L-NAME (10 mg/kg i.v. bolus) was then given followed by a 10-min equilibration and a second 45-60-min clearance period with a another 0.2-mL blood sample obtained at the clearance midpoint. Renal vein samples were taken with a 30-gauge needle to determine the extraction ratio for PAH.
Timed (3-5 min) collections of tubular fluid were made in three proximal tubules after blocking their lumens with Sudan black-stained castor oil to determine SNGFR. Three free flow and stop flow pressures were measured in the earliest convolutions of proximal tubules with a 3-7-μm pipette connected to a servonull micropressure system (World Precision Instruments, Sarasota, FL). Stop flow pressure was determined by blocking tubules with Sudan black-stained castor oil contained in a 12-14 μm pipette. Three hydraulic pressures in efferent star vessels were also measured.
RPF was estimated from the clearance of and extraction ratio for PAH. RBF was calculated by dividing RPF by 1 - arterial hematocrit. RVR was calculated as MAP/RBF. PGC was determined indirectly from stop flow pressure + arterial plasma colloid osmotic pressure (IIA). II was calculated using 1.886C + 0.206C2 + 0.005C3 in which C was plasma protein concentration. Glomerular transcapillary hydraulic pressure difference (ΔP) was calculated as PGC - free flow pressure. SNPF was calculated by dividing SNGFR by single nephron filtration fraction. The single nephron filtration fraction was assumed to be equal to whole kidney filtration fraction estimated from GFR/RPF. Maximum mean effective ultrafiltration pressure (PUF) was calculated by subtracting[(IIA - IIE)/2] from ΔP where IIE was II in the efferent arteriole, the protein concentration of which being estimated from the arterial plasma protein concentration divided by 1 - single nefron plasma flow rate. Minimum values of ultrafiltration coefficients(Kf) were determined by dividing SNGFR by PUF. Transcapillary hydraulic pressure was greater than IIE in all experiments indicating filtration pressure disequilibrium. Afferent arteriole resistance (RA, dyne·s·cm-5) was determined using [(MAP - PGC)/SNBFA] × 7.962 × 1010, where afferent single nephron blood flow (SNBFA) was calculated by dividing SNPF by 1 - arterial hematocrit. Efferent arteriole resistance (RE, dyne·s·cm-5) was calculated using [(PGC - PE)/SNBFE] × 7.962 × 1010, where PE was efferent star vessel pressure and efferent single nephron renal blood flow rate (SNBFE) was calculated as SNBFA - SNGFR.
A microcontinuous gradient gel electrophoresis procedure was used for the separation and quantitation of proteins in plasma and urine(14). Tritiated samples of plasma, urine, and tubular fluid were placed in scintillation fluor and counted in a Packard Tri-Carb scintillation counter. Sodium and potassium concentrations were determined by flame photometry. Creatinine and PAH were assayed using previously described methods(14). NOX concentrations in urine and plasma were measured as described by Feld et al.(15). These samples were stored at -4°C for no more than 2 wk before analysis.
Results are means ± SE. Data obtained from an individual animal during micropuncture experiments were averaged, and this single average represented that animal. Differences within groups were analyzed by two-tailed paired t tests. Differences between groups were analyzed by ANOVA with the Scheffe post hoc test. Differences were considered significant when p < 0.05.
RESULTS
Data from conscious animals are displayed in Table 1. Awake systolic blood pressure of TGR was significantly greater than that of control rats. Body and kidney weights were similar in both groups. There were no differences in plasma sodium, creatinine, or NOX concentrations between TGR and control animals. Urine volume, urinary sodium, and NOX excretion as well as endogenous creatinine clearance did not differ between groups. TGR had significantly higher urinary albumin excretion than did control rats.
Results of clearance experiments are shown in Table 2 and Figure 1. Consistent with their awake systolic blood pressure, anesthetized TGR had significantly higher MAP than did control animals. L-NAME increased MAP in both groups. The absolute (25 ± 3versus 24 ± 3 mm Hg) and relative magnitude of L-NAME-induced MAP increase did not differ between TGR and control rats. Urine flow rate and sodium excretion were significantly higher in TGR than in control animals at baseline. L-NAME significantly increased urine flow and sodium excretion in both groups; urine potassium excretion was unaffected. GFR and RBF fell in response to L-NAME associated with a significant rise in FF in both TGR (0.30± 0.02 versus 0.36 ± 0.02, p < 0.05) and control rats (0.28 ± 0.02 versus 0.36 ± 0.03,p < 0.05). Absolute (1.4 ± 0.2 versus 0.7± 0.1 mL/min, p < 0.05) and percent reductions in GFR produced by L-NAME were significantly greater in TGR than in control animals. Absolute (11.1 ± 2 versus 9.1 ± 2 mL/min) and percent reductions in RBF did not differ between groups. Before L-NAME, RVR was significantly higher in TGR than in control rats. L-NAME increased RVR more in TGR than control animals (10.6 ± 1.4 versus 5.7 ± 0.8 mm Hg/mL/min, p < 0.05). Treatment with L-NAME significantly reduced plasma NOX and did not alter urinary NOX excretion in both groups.
Table 3 and Figure 2 summarize glomerular hemodynamic data. Before L-NAME administration, RA was higher in TGR than in control rats; otherwise, no significant differences in single nephron function were detected between the two groups. After L-NAME, significant declines in SNGFR, SNPF, and Kf occurred in both groups. TGR experienced greater absolute (23 ± 3 versus 11± 2 nL/min, p < 0.05) and percent reductions in SNGFR than control animals. Absolute (90 ± 9 versus 67 ± 7 nL/min) and relative reductions in SNPF did not differ between groups. Absolute (1.8 ± 0.2 versus 1.1 ± 0.1 nL·min-1·mm Hg-1, p < 0.05) and percent reductions in Kf produced by L-NAME were significantly greater in TGR than in control rats. PGC, ΔP,RA, and RE rose significantly in response to L-NAME in both TGR and control rats. Increases in ΔP (10 ± 1versus 5 ± 1 mm Hg, p < 0.05) and RA (3.4 ± 0.2 versus 1.4 ± 0.1 dyne·s·cm-5, p < 0.05) were greater in TGR than in control rats.
DISCUSSION
Consistent with earlier studies, we found that conscious TGR have severe hypertension and pathologic proteinuria without evidence of renal insufficiency(14). Plasma and urine NOX levels did not differ between conscious or anesthetized control and transgenic rats, suggesting similar rates of endogenous NO production. We are aware that diet and proximal tubule reabsorption can alter urinary NOX excretion independent of changes in NO production(16, 17). Although we cannot prove that their dietary nitrate intakes were identical, transgenic and control rats ingested the same diets and had similar body weights. In addition, the fact that NO synthase inhibitors reduced serum NOX levels and prevented the expected rise in urinary NOX excretion in response to an acute increase in arterial blood pressure in this and other studies despite increasing urine flow and sodium excretion suggests that NOX excretion can be used as a measure of NO production and that L-NAME decreased endogenous NO formation in this study(9, 16, 18, 19). This interpretation is controversial(17).
The systemic, whole kidney, and glomerular hemodynamic responses of transgenic and control rats to L-NAME were qualitatively similar and consistent with the previously described actions of this drug in normal anesthetized animals(7, 8). Unlike female TGR in which NO synthesis inhibition caused a significantly greater blood pressure elevation compared with female control rats(11), L-NAME-induced pressure elevations did not differ between transgenic and control animals, supporting the modulating effect of estrogen in this strain. Current evidence indicates that estrogen can promote vasodilation by inducing endothelial NO synthase and stimulating NO production(20). Increased urine flow rate and sodium excretion caused by L-NAME most likely represent a pressure-diuresis-natriuresis response; however, a direct effect on tubule reabsorption cannot be excluded(21, 22). Nitric oxide inhibition causes an exaggerated diuresis-natriuresis in SHR but not their normotensive WKY counterparts(21). This response is independent of changes in renal perfusion pressure but appears to require intact renal innervation(22). Whether TGR react in a comparable fashion is unknown.
Although GFR decreased in both groups after L-NAME, its reduction was significantly greater in transgenic rats because of their proportionately lower Kf and ΔP. This finding implies a greater dependence on NO in TGR renal function, but our results do not allow differentiation between increased production of and sensitivity to this molecule or between primary differences in kidney function and secondary alterations caused by hypertension. Moriguchi et al.(12) have proposed that NO compensates for RAS overactivity in this strain. In animals with activated RAS, NO preserves normal glomerular hemodynamics by antagonizing angiotensin II-induced vasoconstriction and mesangial cell contraction(23–25). Growing evidence points to overactivity of the intrarenal RAS in TGR. For example, use of angiotensin-converting enzyme inhibitors or angiotensin II receptor antagonists in TGR corrects their blunted pressure-diuresis-natriuresis response(18, 26, 27), markedly attenuates their heightened tubuloglomerular feedback mechanism(28) and, at a dose too low to affect systemic blood pressure, reduces their glomerulosclerosis and protein-uria(29). Taken together, this functional information suggests intrarenal RAS activation in TGR, an environment that should benefit from the moderating influence of NO.
However, conclusions about the TGR(mRen2)27 renin-angiotensin and nitric oxide systems should be made cautiously. Although kidney angiotensin II levels have been reported 3-fold higher in 6-wk-old homozygous TGR compared with age-matched normotensive Sprague-Dawley control rats(2), another study of rats at 16 wk of age found no significant difference between homozygous TGR and control rats and that the renal angiotensin II content of heterozygous TGR rats was significantly reduced(3). In addition, current evidence indicates that the beneficial hemodynamic effects of NO manifest only when angiotensin II levels are acutely but not chronically elevated(30).
To our knowledge, only one other report has addressed the consequences of NO synthesis inhibition on whole kidney and single nephron function in a genetically hypertensive rat strain. Ono et al.(31) reported that long-term treatment of SHR with oral L-NAME caused significant elevations in MAP and RVR together with significant declines in GFR and effective RPF. These changes in whole kidney function were associated with significant increases in ΔP, RA, and RE as well as marked reductions in Kf and SNPF. Although their results are similar to those of the current study and demonstrate an important protective role for NO in the hypertensive kidney, both the severe L-NAME-induced structural damage and the lack of normotensive control strain experiments make a definitive comparison difficult.
These investigators also noted preferential L-NAME-induced preglomerular vasoconstriction in SHR that limited the development of glomerular hypertension at the expense of glomerular ischemia(31). This finding is consistent with studies in isolated perfused hydronephrotic SHR kidneys, showing that afferent arteriole myogenic constriction is intact but shifted to higher renal perfusion pressures in SHR and that an enhanced effect of NO on afferent arterioles is responsible for this resetting(32). Increased TGR afferent arteriole sensitivity to NO blockade was also demonstrated in the present study. It is of interest in this regard that glomerulosclerosis in older SHR appears to be caused by ischemia and not barotrauma(33, 34). Hypertensive renal injury in these animals could therefore possibly relate to age-dependent loss of NO production or responsiveness in preglomerular vasculature. We have previously shown that the functional and histologic evolution of kidney damage in TGR resembles that in SHR at least through 8 mo of age(14). Whether similarities in NO dependence between these two genetically hypertensive rat strains represent a shared primary vascular defect or hypertension-induced vascular injury is not known.
In summary, acute systemic NO synthesis inhibition causes a proportionately greater reduction of GFR in TGR than in control rats despite comparable changes in systemic blood pressure. Enhanced afferent arteriole vasoconstriction and Kf reduction are responsible for this difference. Additional studies employing intrarenal NO and angiotensin II blockers that do not alter systemic hemodynamics are needed to clarify the interaction between kidney renin-angiotensin and NO systems in these animals. Nevertheless, our results support an important role for NO in TGR renal function.
Abbreviations
- TGR:
-
TGR(mRen2)27 rats
- NO:
-
nitric oxide
- L-NAME:
-
NG-nitro-L-arginine methyl ester
- NOX:
-
nitric oxide oxidation products
- RAS:
-
renin-angiotensin system
- SHR:
-
spontaneously hypertensive rats
- PAH:
-
p-aminohippuric acid
- SNGFR:
-
single nephron GFR
- RBF:
-
renal blood flow
- RPF:
-
renal plasma flow
- RVR:
-
renal vascular resistance
- MAP:
-
mean arterial pressure
- SNBF:
-
single nephron blood flow
- SNPF:
-
single nephron plasma flow
- PGC:
-
glomerular capillary hydraulic pressure
- PUF:
-
ultrafiltration pressure
- R A:
-
afferent arteriole resistance
- R E:
-
efferent artriole resistance
References
Langheinrich M, Lee M, Bohm M, Pinto Y, Ganten D, Pau M 1996 The hypertensive Ren-2 transgenic rat TGR(mRen2)27 in hypertension research. Am J Hypertens 9: 506–512.
Campbell D, Rong P, Kladis A, Rees B, Ganten D, Skinner S 1995 Angiotensin and bradykinin peptides in the TGR(mRen2)27 rat. Hypertension 25: 1014–1020.
Lee M, Bohm M, Kim S, Bachmann S, Bachmann J, Bader M, Ganten D 1995 Differential gene expression of renin and angiotensinogen in the TGR(mRen2)27 transgenic rat. Hypertension 25: 570–580.
Tokita Y, Francossenz R, Reimann E, Mulrow P 1994 Hypertension in the transgenic rat TGR(mRen2)27 may be due to enhanced kinetics of the reaction between mouse renin and rat angiotensinogen. Hypertension 23: 422–427.
Veniant M, Whitworth C, Menard J, Sharp M, Gonzales M, Bruneval P, Mullins J 1995 Developmental studies demonstrate age-dependent elevation of renin activity in TGR(mRen2)27 rats. Am J Hypertens 8: 1167–1176.
Djavidani B, Sander M, Kreutz R, Zeh K, Bader M, Mellon S, Vecsei P, Peters J, Ganten D 1995 Chronic dexamethasone treatment suppresses hypertension development in the transgenic rat TGR(mRen2)27. J Hypertens 13: 637–645.
Rau L, Baylis C 1995 Glomerular actions of nitric oxide. Kidney Int 48: 20–32.
Lahera V, Navarro-Cid J, Cachofeiro V, Garcia-Estan J, Ruilope L 1997 Nitric oxide, the kidney and hypertension. Am J Hypertens 10: 129–140.
Ikenaga H, Suzuki H, Ishii N, Itoh H, Saruta T 1993 Role of NO on pressure-natriuresis in Wistar-Kyoto and spontaneously hypertensive rats. Kidney Int 43: 205–211.
Patel A, Layne S, Watts D, Kirchner K 1993 L-arginine administration normalizes pressure natriuresis in hypertensive Dahl rats. Hypertension 22: 863–869.
Tschudi M, Noll G, Arnet U, Novosel D, Ganten D, Luscher T 1994 Alterations in coronary artery vascular reactivity of hypertensive ren-2 transgenic rats. Circulation 89: 2780–2786.
Moriguchi A, Brosnihan K, Kumagai H, Ganten D, Ferrario C 1994 Mechanisms of hypertension in transgenic rats expressing the mouse Ren-2 gene. Am J Physiol 266:R1273–R1279.
Brosnihan K, Moriguchi A, Nakamoto H, Dean R, Ganten D, Ferrario C 1994 Estrogen augments the contribution of nitric oxide to blood pressure regulation in transgenic hypertensive rats expressing the mouse ren-2 gene. Am J Hypertens 7: 576–582.
Springate J, Feld L, Ganten D 1994 Renal function in hypertensive rats transgenic for mouse renin gene. Am J Physiol 266:F731–F737.
Feld L, Cachero S, Ellis E, Dedeoglu O, Ueda Y, Leonard C, Letizia R, Mallon V, Van Liew J 1995 Resistance to glomerular injury in the diabetic biobreeding rat. Exp Physiol 80: 991–1000.
Boger R, Bode-Boger S, Gerecke U, Gutzki F, Tsikas D, Frolich J 1996 Urinary NO3- excretion as an indicator of nitric oxide formation in vivo during oral administration of L-arginine or L-NAME in rats. Clin Exp Pharmacol Physiol 23: 11–15.
Suto T, Losonczy G, Qiu C, Hill C, Samsell L, Ruby J, Charon N, Venuto R, Baylis C 1995 Acute changes in urinary excretion of nitrite + nitrate do not necessarily predict renal vascular NO production. Kidney Int 48: 1272–1277.
Springate J, Van Liew J, Ganten D 1997 Enalapril and pressure-natriuresis in hypertensive rats transgenic for mouse renin gene. Kidney Blood Press Res 20: 1–5.
Suzuki H, Ikenaga H, Hishikawa K, Nikaki T, Kato R, Saruta T 1992 Increases in NO2-/NO3- excretion in the urine as an indicator of the release of endothelium-derived relaxing factor during elevation of blood pressure. Clin Sci 82: 631–634.
Farhat M, Lavigne M, Ramwell P 1996 The vascular protective effects of estrogen. FASEB J 10: 615–624.
Khraibi A 1996 Inhibition of nitric oxide causes exaggerated natriuresis in spontaneously hypertensive rats. Am J Physiol 266:F762–F766.
Khraibi A 1995 Role of renal nerves in natriuresis of L-NAME infusion in SHR and WKY rats. Am J Physiol 269:F17–F21.
Baylis C, Harvey J, Engels K 1994 Acute nitric oxide blockade amplifies the renal vasoconstrictor actions of angiotensin II. J Am Soc Nephrol 5: 211–214.
DeNicola L, Blantz R, Gabbai F 1992 Nitric oxide and angiotensin II. J Clin Invest 89: 1248–1256.
Sigmon D, Newman J, Beierwaltes W 1994 Angiotensin II: endothelium-derived nitric oxide interaction in conscious rats. J Am Soc Nephrol 4: 1675–1682.
Gross V, Lippoldt A, Schneider W, Luft F 1995 Effect of captopril and angiotensin II receptor blockade on pressure-natriuresis in transgenic TGR(mRen2)27 rats. Hypertension 26: 471–479.
Lippoldt A, Gross V, Bohlender J, Ganten U, Luft F 1996 Lifelong angiotensin-converting enzyme inhibition, pressure natriuresis and renin-angiotensin system gene expression in transgenic (mRen2) rats. J Am Soc Nephrol 7: 2119–2129.
Mitchell K, Mullins J 1995 Ang II dependence of tubuloglomerular feedback responsiveness in hypertensive ren-2 transgenic rats. Am J Physiol 268:F821–F828.
Bohm M, Lee M, Kreutz R, Kim S, Schinke M, Djavidani B, Wagner J, Kaling M, Wienen W, Bader M, Ganten D 1995 Angiotensin II receptor blockade in TGR(mRen2)27: effects on renin-angiotensin system gene expression and cardiovascular functions. J Hypertens 13: 891–899.
Deng X, Welch W, Wilcox C 1996 Role of nitric oxide in short-term and prolonged effects of angiotensin II on renal hemodynamics. Hypertension 27: 1173–1179.
Ono H, Ono Y, Frolich E 1995 Nitric oxide synthase inhibition in spontaneously hypertensive rats. Hypertension 26: 249–255.
Hayashi K, Suzuki H, Saruta T 1995 Nitric oxide modulates but does not impair myogenic vasoconstriction of the afferent arteriole in spontaneously hypertensive rats. Hypertension 25: 1212–1219.
Feld L, Zamlauski-Tucker M, Springate J, Van Liew J 1995 Single nephron hemodynamics in spontaneously hypertensive rats. Proc Soc Exp Biol Med 269: 185–189.
Komatsu K, Frolich E, Ono H, Ono Y, Numabe A, Willis G 1995 Glomerular dynamics and morphology of aged spontaneously hypertensive rats. Hypertension 25: 207–213.
Acknowledgements
The authors thank Susan Bemben, Sherry Davies, and Nancy Manz for their excellent technical assistance.
Author information
Authors and Affiliations
Additional information
Supported by a grant-in-aid from the American Heart Association.
Rights and permissions
About this article
Cite this article
Dedeoglu, I., Springate, J. Effect of Nitric Oxide Inhibition on Blood Pressure and Renal Function in TGR(mRen2)27 Rats. Pediatr Res 43, 203–208 (1998). https://doi.org/10.1203/00006450-199802000-00008
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199802000-00008