Abstract
The aim of this study was to determine whether there is a relationship between changes in PR-RR correlation of the fetal ECG and progressive changes in fetal acid-base status and blood pressure (BP) during repeated umbilical occlusion. Chronically instrumented fetal sheep at 126.8 ± 0.6 d (mean± SEM) were randomized to receive 1 min of total umbilical cord occlusion either every 5 min for 4 h (1:5 group; n = 8), or every 2.5 min until BP fell <2.7 kPa (20 mm Hg) on two successive occlusions (1:2.5 group; n = 8). The PR-RR correlation was determined in 5- or 2.5-min intervals. Umbilical cord occlusion caused variable decelerations with initial sustained hypertension. In the 1:5 group BP remained elevated throughout, and there was little change in acid-base status (pH = 7.34 ± 0.07, base deficit = 1.3 ± 3.9 after 4 h). In contrast, after the third occlusion the 1:2.5 group showed progressive hypotension during occlusions, and severe progressive metabolic acidemia (pH 6.92 ± 0.1, base deficit 17.0 ± 4.7 mmol/L after the last occlusion). In both groups, the PR-RR relationship switched from positive to negative with the onset of occlusions, then reverted to positive after a variable interval. In the 1:2.5 group later reversion of the PR-RR to positive was associated with earlier and more prolonged hypotension during the middle and end of the occlusion series (p < 0.001). We conclude that the initial switch to a negative PR-RR relationship during repetitive umbilical occlusion was due to a reflex-mediated response unrelated to fetal acidosis or hypotension. Both stable well compensated fetuses and severely hypoxic, hypotensive fetuses subsequently showed a positive PR-RR correlation.
Similar content being viewed by others
Main
Although electronic fetal monitoring has been associated with a significant reduction in fetal mortality(1) and postasphyxial seizures(2), the positive predictive value of changes in the fetal heart rate pattern remains low(3). Thus a number of possible approaches to improving the sensitivity and specificity of fetal monitoring have been proposed. One suggestion is that relative changes in the PR and RR intervals of the fetal ECG may help to discriminate patterns of fetal heart rate changes during labor(4,5). The PR interval reflects the atrioventricular conduction time and is usually positively related to the RR interval duration, i.e. as the RR interval lengthens during bradycardia, the PR interval also lengthens; however, in some circumstances a paradoxical shortening of the PR interval may be seen (i.e. a negative relationship). Some human observational studies have reported that a change from a positive to a negative correlation was associated with fetal acidemia at birth(5), whereas others have not(6). Although, experimentally, single brief episodes of hypoxia(7) and prolonged continuous hypoxia(8) have been associated with a negative switch, these paradigms cannot be used to resolve this controversy as neither reflects the typical pattern of normal labor.
We have recently characterized the effects of recurrent umbilical cord occlusions in fetal sheep repeated at rates consistent with active labor(9). One-minute occlusions repeated every 2.5 min were associated with severe variable decelerations and progressive fetal metabolic acidemia and hypotension(9), with corresponding cerebral compromise(10). In pilot studies we found that if the frequency of occlusions was reduced to every 5 min, variable fetal heart rate decelerations still occurred, but no significant changes in fetal blood pressure or acid-base status were seen even after more than 4 h of occlusions(9).
The aim of this study was to determine whether there is a relationship between changes in the PR-RR relationship and fetal acid-base status and MAP during recurrent 1-min umbilical cord occlusions repeated either every 5 or every 2.5 min, in chronically instrumented late gestation fetal sheep.
METHODS
Surgical procedures. Operations were performed in Romney/Suffolk sheep under halothane anesthesia (2%) using sterile techniques, as previously described(9,11). Briefly, in 16 fetal sheep, polyvinyl catheters were inserted into the right and left brachial artery and in the amniotic cavity. An inflatable occluder cuff (In Vivo Metric, Healdsburg, CA) was placed around the umbilical cord. ECG electrodes (Cooner wire AS633-3SSF) were placed s.c., one over the apex of the heart and one on the right shoulder. The maternal long saphenous vein was catheterized. After surgery, ewes were housed in a cage at constant temperature (16°C) and humidity (50%), with free access to water and hay, supplemented with sheep nuts and alfalfa. Gentamicin (80 mg, intraamniotically) was administered to the fetuses daily throughout the experiments. After completion of the studies, animals were killed by an overdose of pentobarbital i.v. Studies were approved by the Animal Ethics Committee of the University of Auckland.
Recordings. Fetal arterial blood pressure (corrected for amniotic pressure), and the fetal ECG were measured continuously, saved to disks using customized Labview programs (National Instruments, Austin, TX), and later transferred to CD-ROM storage media. The blood pressure signal was collected at 64 Hz and low pass filtered at 30 Hz. The raw ECG was analog-filtered between 0.05 and 80 Hz and digitized at 512 Hz. Measurements started at least 12 h before the experiment and were continued for at least 24 h after the end of occlusions.
Experimental procedures. Experiments were started 3-5 d after surgery, at a gestational age of 126.3 ± 2.6 d (term is 147 d). After a baseline period of at least 12 h, fetuses were randomized to one of two groups, the 1:5 group (repeated total umbilical cord occlusion for 1 min out of every 5 min, n = 8) or the 1:2.5 group (repeated total umbilical cord occlusion for 1 min out of every 2.5 min, n = 8). The cardiovascular and cerebral responses of three fetuses in the 1:2.5 group have previously been reported(9,10). Umbilical cord occlusion was performed by inflating the cuff with sterile saline, and then deflating it after 1 min. This procedure was repeated for up to 4 h, or until the fetal mean arterial blood pressure had fallen below 2.7 kPa (20 mm Hg) during two successive occlusions, or the fetal blood pressure failed to recover to baseline levels when the next occlusion was due.
Fetal arterial blood gas analysis and measurements of glucose and lactate levels were performed immediately before the first occlusion, after every sixth occlusions (i.e. every 30 min in the 1:5 group and every 15 min in the 1:2.5 group), every hour for the 4 after the last occlusion, and daily thereafter.
Data analysis and statistics. Off line analysis of the raw MAP and ECG data were performed using customized Labview programs (National Instruments, Austin, TX). One-second averages of MAP were calculated for each fetus; these data were used to derive the baseline MAP before and after occlusions, the maximum MAP during each occlusion, the minimum MAP at the end of each occlusion, and the mean interocclusion MAP.
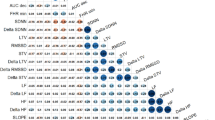
The ECG wave form was averaged with respect to the S wave at 5-s intervals, and the PR and RR intervals for each averaged wave form were calculated. The raw ECG data for each averaged wave form were visually assessed to identify P wave shape changes and to verify software identification of the P and R waves. Pearson's correlation coefficient(Excel; Microsoft, Seattle, WA) for the PR and RR intervals was calculated every 5 min for 4 h preceding the occlusions, for 24 h after the occlusions, and for the 4 h during the occlusions in the 1:5 group. Correlation coefficients were calculated every 2.5 min during occlusions in the 1:2.5 group. Examples of PR and RR data which result in positive and negative correlations are shown in Figure 1.
Examples of a positive (left panels) and a negative relationship (right panels) between the PR and RR intervals measured from averaged fetal ECG complexes. The top panels show 1-h plots of the PR and RR intervals; the corresponding correlation coefficients, calculated in 5-min blocks, are shown in the bottom panels.
For statistical analysis of metabolic, cardiovascular, and PR-RR correlations, groups were compared using ANOVA, with time as a repeated measure. Between group comparisons were made by the MWU, and within group comparisons were made with the Wilcoxon matched pairs test. χ2 analysis was used to evaluate discrete variables.
RESULTS
Repeated umbilical cord occlusions were performed on eight fetuses in each experimental protocol group. In two cases in the 1:2.5 group, ECG recordings were available only for the first 90 min of occlusions due to technical problems. The MAP, acid-based changes, and PR-RR correlation coefficients for the 1:5 and 1:2.5 groups are shown in Figures 2 and 3, respectively. All fetuses survived to the end of the experiment.
The time sequence of changes in MAP(i), pH and BD (ii), and PR-RR correlation coefficient(derived from 5-min intervals; iii) in the 1:5 occlusion group. MAP is presented as the maximum and minimum blood pressure during each occlusion, and the mean pressure for the interval between occlusions. Note the sustained rise in MAP during occlusions; although there is a small fall in MAP during occlusions the minimum pressure never falls below preocclusion levels. There is a small fall in pH, which stabilizes despite ongoing occlusions. The PR-RR correlation becomes negative at the start of occlusions, but rapidly reverts to a positive correlation.
The time sequence of changes in MAP (i), pH and BD (ii), and PR-RR correlation coefficient (iii) for subgroups A (left panels) and B (right panels) in the 1:2.5 occlusion group. In contrast to the 1:5 group, after the first three occlusions, the MAP during occlusions progressively fell, with an associated severe metabolic acidosis. As the individual experiments were of unequal duration, the average data during occlusions are presented in three separate intervals: the first 30 min, the middle 30 min (median ± 15 min), and the final 30 min of occlusions. The PR-RR correlation during occlusions was calculated from 2.5-min intervals. MAP is presented as the maximum and minimum blood pressure during each occlusion, and the mean pressure for the interval between occlusions. Subgroup A shows a continued negative correlation during the middle 30-min period of occlusions, but reverted to positive by the final 30 min. In contrast subgroup B shows early reversion within the first 30 min; this group tended to show variable PR-RR correlation in the last 30 min. Early reversion, as in subgroup B, was associated with significantly slower development of hypotension during occlusions. p < 0.001 for min MAP, subgroup A versus subgroup B, repeated measures ANOVA.
1:5 Group. All fetuses tolerated 4 h or occlusions without hypotension or significant metabolic acidosis (Fig. 2). The interocclusion MAP rose from a preocclusion baseline mean of 5.8 ± 0.74 kPa to 7.6 ± 0.28 kPa after the first occlusion (p< 0.002, MWU); MAP between occlusions did not change significantly over the rest of the occlusion series. MAP rose with each occlusion and did not fall below the preocclusion baseline. As shown in Figure 2, a small metabolic acidosis developed during the first 30 min of occlusions; arterial pH fell from 7.41 ± 0.01 to 7.35 ± 0.05, whereas BD rose from -3.5 ± 2.2 mmol/L to 0.08± 3.2 mmol/L. Thereafter acid-base status remained stable, and the pH(7.34 ± 0.07) and BD (1.3 ± 3.9) at the end of the occlusions were not significantly different from the 30-min values. Lactate rose from a baseline of 1.1 ± 0.1 mmol/L before occlusions to 2.3 ± 0.4 mmol/L at 30 min (p < 0.01, Wilcoxon), and 4.5 ± 1.3 mmol/L at the last occlusion (NS, compared with 30 min).
The PR-RR correlation coefficient was positive during the baseline period and became negative with the first occlusion in all animals. In seven of the eight animals, despite continuing occlusions, the correlation coefficient reverted to positive after a variable period of time (median 40 min, range 5-130 min). In the eighth fetus the correlation remained negative for the duration of the occlusion series, but immediately became positive once the experiment ended. This fetus had the least acid-base changes of the entire group (after 4 h of occlusions; pH 7.42, BD 4.3 mmol/L, lactate 1.4 mmol/L). The PR-RR correlation was positive in all fetuses throughout the 24-h recovery period.
1:2.5 Group. In contrast to the 1:5 group, fetuses in the 1:2.5 group became progressively hypotensive and acidotic and the experiments were terminated after a mean of 74 ± 15 occlusions. As the individual experiments were of unequal duration, the average data have been presented for three intervals in Figure 3; the first 30 min, the middle 30 min (defined as the median ± 15 min), and the final 30 min of occlusions. The 1:2.5 group were then, post hoc, further divided into two subgroups (A, n = 5 and B, n = 3) on the basis of their PR-RR correlation pattern as described below. After the third occlusion, all fetuses developed a marked biphasic blood pressure response to successive occlusions, with initial hypertension followed by a fall in MAP reaching a nadir a few seconds after release of the occluder. The hypotension became greater with successive occlusions, until studies were stopped when MAP fell below 2.7 kPa for two successive occlusions.
The overall pattern of PR RR changes was similar to that of the 1:5 group, with an immediate switch to negative with the onset of occlusions followed by reversion to positive. Two patterns of timing of the reversion to positive were seen. In five fetuses the correlation remained almost entirely negative for an extended period (121 ± 46 min), including the first and middle 30 min before reverting to positive in the last 30 min (subgroup A). In the three other fetuses the correlation was negative for a much shorter period(31 ± 8 min, p = 0.06, MWU) and had reverted to positive by the middle 30 min (subgroup B). In this group, the positive correlation tended to weaken during the last 30 min. In the recovery period after the occlusions all fetuses showed a negative PR-RR correlation for some hours(5.3 ± 2.3 h in subgroup A (range 3-10) and 9.0 ± 4.5 h (range 4-18) in B; NS) before returning to a predominantly positive relationship.
The number of occlusions was the same in the two groups, 77 ± 17 occlusions in subgroup A (range 58-90) and 72 ± 16 occlusions in subgroup B (range 59-90). The subgroups developed a similarly severe metabolic acidosis, as shown in Figure 3,A(ii) and B(ii), with lactate levels rising to 14.3± 3.5 in subgroup A and 14.9 ± 1.5 in subgroup B after the last occlusion (NS). There were no significant differences between subgroups. Although statistical comparisons between the subgroups must be limited by the small numbers in each group (five and three), there were some significant differences in the blood pressure response (Fig. 3,A(i) and B(i)). The average interocclusion MAP in the first 30 min was higher in subgroup A than in subgroup B (9.20 ± 0.16 versus 8.6± 0.12 kPa, two-way ANOVA, p < 0.001). In the mid 30 min the minimum pressure in subgroup A fell progressively, whereas it remained stable in subgroup B (mean A 5.3 ± 0.05 kPa, mean B 6.1 ± 0.04 kPa, p < 0.0001, two-way ANOVA). In the last 30 min the minimum pressure was consistently lower in subgroup A (mean A 3.2 ± 0.12 kPa and mean B 3.9 ± 0.27 kPa over 30 min, p < 0.0001, two-way ANOVA). Finally, there was a much steeper fall in minimum MAP in subgroup B (1.2 kPa per 30 min in A and 3.1 kPa per 30 min in B, p< 0.0001, two-way ANOVA). Consistent with this, the time taken to revert to a positive PR-RR correlation showed a strong trend to a relationship with the rate of fall of minimum MAP between 45 and 15 min before the last occlusion (Spearman's r = -0.82, p = 0.058).
Changes in P wave shape. Second degree heart block was noted during or immediately after a number of occlusions in three of eight fetuses in the 1:5 group and four of eight fetuses in the 1:2.5 group (two in subgroup A and two in B). An example is shown in Figure 4. When heart block occurred, it was seen only in the first few occlusions of five of these seven fetuses (median 1, range 1-16). Heart block was more common in occlusions where the RR interval rose above 857 ms (fetal heart rate < 70 beats/min,Table 1). In addition, P wave shape changes, or even disappearance of the P wave during occlusions were noted in a number of fetuses (four in the 1:5 group and five in the 1:2.5 group,Fig. 5). Small P waves prevented accurate automated P wave detection and bifid P waves often resulted in rapid changes in PR interval as the P wave detector oscillated between the two peaks, depending which was temporarily the largest. These shape changes were not related to hypotension or acidosis, nor to RR interval.
DISCUSSION
This is the first systematic evaluation of the evolution of PR-RR relationship during repeated episodes of brief asphyxia. We found that a change in the PR-RR correlation from positive to negative was not associated with fetal hypotension and acidosis but rather with the onset of occlusions. These data are consistent with the clinical observational study of Luzietti et al.(6), who recently reported that a negative PR-RR relationship occurred with all decelerations of more than 40 beats/min. The immediate switch suggests that this paradoxical PR shortening with the onset of occlusions is likely to be associated with reflex cardiac stimulation in response to acute hypoxia.
The precise mechanism involved in this immediate change is unknown but, we speculate, is unlikely to be a baroreceptor reflex as the fall in fetal heart rate occurred before the MAP rose(12). Although sympathetic stimulation is known to shorten atrioventricular conduction time(9,12), autonomic sympathetic activity is also unlikely to be involved. Studies of chemical sympathectomy suggest that it has limited effects on fetal heart rate during asphyxia and that its major contribution is to mediate peripheral vasoconstriction(13). Finally, circulating catecholamines are unlikely to significantly contribute to the initial switch in view of the known time course of their rise during repeated occlusions(14), although it is possible that this slow but very large rise may contribute to later changes. This would be consistent with findings from a human observational study in which the PR interval varied inversely with umbilical cord vein adrenaline concentration at delivery(4). We belive that it is most likely that carotid chemoreflexes play a central role in the initial rapid PR changes. The initial fall in FHR during hypoxia has been shown to be mediated principally by the carotid chemoreceptor afferent limb(15,16). During asphyxia carotid sinus nerve denervation delays the onset of bradycardia(17). To date, however, the effect of chemoreceptors on the fetal PR-RR relationship has not been directly tested.
The PR-RR correlation pattern during occlusions was similar in the 1:5 min group and 1:2.5 min groups despite their contrasting cardiovascular and metabolic states and it would be impossible to distinguish between the 1:5 group and the 1:2.5 groups on this basis alone. Both groups developed a negative correlation with the onset of occlusions but then we identified early and late patterns of a return to a positive correlation. In both the 1:5 group and the 1:2.5 subgroup B the correlation changed back to positive early, whereas in the 1:2.5 subgroup A it remained negative for much longer, becoming positive only in the last 30 min. Although this was a post hoc analysis and the numbers were limited, it is interesting to speculate on the possible mechanisms for this difference. The greater persistence of a negative correlation appeared to be associated with greater changes in cardiovascular and metabolic state, whereas the return to a positive correlation in the 1:5 group and in subgroup B accompanied periods of stability in these measures. We hypothesize that greater persistence of a negative correlation in the 1:2.5 subgroup A reflected relative cardiovascular instability and possibly higher sympathetic stimulation(4).
The eventual change back to a positive PR-RR correlation in the last 30 min of the 1:2.5 subgroup A was an unexpected finding as it had not been reported in the clinical studies to date. This stage of the experiment was accompanied by severe fetal hypotension, acidosis, and hypoxia. Hypoxia can impair conduction in the atrioventricular node, either directly or alternatively mediated by adenosine release, which acts to depress slow channel mediated action potentials(18,19). It is likely then that direct myocardial tissue hypoxia contributed to the PR lengthening seen in the last 30 min. This pattern of PR lengthening during decelerations in association with severe acidosis and hypotension has not been observed in clinical studies, possibly because not many severely acidotic fetuses have been studied. In the two observational studies which led to the development of the PR-RR hypothesis currently under investigation, just 6 of 274 fetuses had an arterial pH < 7.10, of which two had a pH< 7.05 (6.91 and 6.99(4,5). The mean arterial pH of fetuses studied by Mohajer et al.(5) was 7.24 (SD 0.08). Such levels correspond with just the first 30 min of occlusion in the 1:2.5 group, a time when the PR-RR correlations were still negative.
The PR-RR relationship became predominantly negative in recovery in all fetuses in the 1:2.5 group, for a number of hours after occlusions. Speculatively, this may reflect the stimulatory effect of high levels of circulating catecholamines on atrioventricular conduction time at the end of the occlusion series, unopposed by tissue hypoxia(14,20). Thus it is possible that a predominantly negative PR-RR relationship before or in early labor may be a marker for a fetus who is recovering from recent significant hypoxic episodes.
It has been suggested from a small case series that heart block may reflect profound hypoxia in labor(21). In contrast, both in the present study and other reports(4,22,23), neither P wave shape changes nor the occurrence of heart block were associated with acidosis and hypotension. Heart block was more common both at heart rates of ≤70 beats/min and in the first few occlusions, consistent with the previous clinical association with heart rates of <60 beats/min(21) and an experimental study which observed various degrees of heart block after single brief periods of umbilical cord occlusion(24). In the later study, the administration of atropine prevented the conduction defects suggesting parasympathetic stimulation was their cause. This raises an interesting question; does heart block occur simply because the heart rate is very low, or does the heart rate become so low because heart block occurs? The appearance of P wave shape changes could indicate that the location of the atrial pacemaker site had changed(12,25). This has practical consequences, because we and others(6) have found that P wave shape changes caused problems for software detection of the P wave, with erroneous P wave detection and rapid oscillations in PR interval and PR-RR correlation. These errors were manually corrected during visual analysis of the recordings in the present study, but are unlikely to be detected during automated analysis.
In conclusion, the PR shortening and negative PR-RR correlation seen with the onset of occlusions is consistent with a reflex-mediated response unrelated to fetal acidosis or hypotension. This study has shown that both the stable well compensated fetus and the severely hypoxic, hypotensive fetus may show a positive PR-RR correlation. The latter state would be erroneously identified as normal within the current model of PR-RR interpretation, in which only a persistently negative correlation is considered abnormal. Thus PR-RR correlation in isolation is unlikely to significantly contribute to conventional clinical electronic fetal monitoring.
Abbreviations
- BD :
-
base deficit
- MAP :
-
mean arterial blood pressure
- MWU :
-
Mann-Whitney U test
References
Vintzileos AM, Nochimson DJ, Guzman ER, Knuppel RA, Lake M, Schifrin BS 1995 Intrapartum electronic fetal heart rate monitoring versus intermittent auscultation: a meta-analysis. Obstet Gynecol 85: 149–155.
Thacker SB, Stroup DF, Peterson HB 1995 Efficacy and safety of intrapartum electronic fetal monitoring: an update. Obstet Gynecol 86: 613–620.
Nelson KB, Dambrosia JM, Ting TY, Grether JK 1996 Uncertain value of electronic fetal monitoring in predicting cerebral palsy. N Engl J Med 334: 613–618.
Murray HG 1986 The fetal electrocardiogram: current clinical developments in Nottingham. J Perinat Med 14: 399–404.
Mohajer MP, Sahota DS, Reed NN, Chang A, Symonds EM, James DK 1994 Cumulative changes in the fetal electrocardiogram and biochemical indices of fetal hypoxia. Eur J Obstet Gynecol Reprod Biol 55: 63–70.
Luzietti R, Erkkola R, Hasbargen U, Mattson LA, Thoulon JM, Rosen KG 1997 European Community Multicentre Trial "Fetal ECG Analysis during Labour": the P-R interval. J Perinat Med 25: 27–34.
Widmark C, Lindecrantz K, Murray H, Rosen KG 1992 Changes in the PR, RR intervals and ST waveform of the fetal lamb electrocardiogram with acute hypoxemia. J Dev Physiol 18: 99–103.
van Wijngaarden WJ, de Haan HH, Sahota DS, James DK, Symonds EM, Hasaart TH 1996 Changes in the PR interval-fetal heart rate relationship of the electrocardiogram during fetal compromise in chronically instrumented sheep. Am J Obstet Gynecol 175: 548–554.
de Haan HH, Gunn AJ, Gluckman PD 1997 Fetal heart rate changes during brief repeated umbilical cord occlusion do not reflect cardiovascular deterioration in fetal lambs. Am J Obstet Gynecol 176: 8–17.
de Haan HH, Gunn AJ, Williams CE, Gluckman PD 1997 Brief repeated umbilical cord occlusions cause sustained cytotoxic cerebral edema and focal infarcts in near-term fetal lambs. Pediatr Res 41: 96–104.
Mallard EC, Gunn AJ, Williams CE, Johnston BM, Gluckman PD 1992 Transient umbilical cord occlusion causes hippocampal damage in the fetal sheep. Am J Obstet Gynecol 167: 1423–1430.
Warner MR, Loeb JM 1987 Reflex regulation of atrioventricular conduction. Am J Physiol 252:H1077–H1085.
Jensen A, Lang U 1992 Foetal circulatory responses to arrest of uterine blood flow in sheep: effects of chemical sympathectomy. J Dev Physiol 17: 75–86.
Jensen A, Kunzel W, Kastendieck E 1987 Fetal sympathetic activity, transcutaneous PO2, and skin blood flow during repeated asphyxia in sheep. J Dev Physiol 9: 337–346.
Bartelds B, Van Bel F, Teitel DF, Rudolph AM 1993 Carotid, not aortic, chemoreceptors mediate the fetal cardiovascular response to acute hypoxemia in lambs. Pediatr Res 34: 51–55.
Giussani DA, Spencer JA, Moore PJ, Bennet L, Hanson MA 1993 Afferent and efferent components of the cardiovascular reflex responses to acute hypoxia in term fetal sheep. J Physiol 461: 431–449.
Jensen A, Hanson MA 1995 Circulatory responses to acute asphyxia in intact and chemodenervated fetal sheep near term. Reprod Fertil Dev 7: 1351–1359.
Hirata A 1990 Effect of hypoxia on electrical activity of atrioventricular nodal cells and atrial cells of the rabbit's heart. J Electrocardiol 23: 69–76.
Clemo HF, Bourassa A, Linden J, Belardinelli L 1987 Antagonism of the effects of adenosine and hypoxia on atrioventricular conduction time by two novel alkylxanthines: correlation with binding to adenosine A1 receptors. J Pharmacol Exp Ther 242: 478–484.
Rosen KG, Hrbek A, Karlsson K, Kjellmer I 1986 Fetal cerebral, cardiovascular and metabolic reactions to intermittent occlusion of ovine maternal placental blood flow. Acta Physiol Scand 126: 209–216.
Mohajer MP, Sahota DS, Reed NN, James DK 1995 Atrioventricular block during fetal heart rate decelerations. Arch Dis Child Fetal Neonat Ed 72:F51–F53.
Pardi G, Tucci E, Uderzo A, Zanini D 1974 Fetal electrocardiogram changes in relation to fetal heart rate patterns during labor. Am J Obstet Gynecol 118: 243–250.
Marvell CJ, Kirk DL, Jenkins HM, Symonds EM 1980 The normal condition of the fetal electrocardiogram during labour. Br J Obstet Gynaecol 87: 786–796.
Yeh MN, Morishima HO, Niemann WH, James LS 1975 Myocardial conduction defects in association with compression of the umbilical cord. Experimental observations on fetal baboons. Am J Obstet Gynecol 121: 951–957.
Boyden PA, Dresdner KP 1990 Electrogenic Na(+)-K+ pump in Purkinje myocytes isolated from control noninfarcted and infarcted hearts. Am J Physiol 258:H766–H772.
Author information
Authors and Affiliations
Additional information
Supported by the Health Research Council of New Zealand, the Auckland Medical Research Foundation, the New Zealand Lotteries Board, and U.S. Public Health Service Grant RO1-HD-32752.
Rights and permissions
About this article
Cite this article
Westgate, J., Gunn, A., Bennet, L. et al. Do Fetal Electrocardiogram PR-RR Changes Reflect Progressive Asphyxia after Repeated Umbilical Cord Occlusion in Fetal Sheep?. Pediatr Res 44, 297–303 (1998). https://doi.org/10.1203/00006450-199809000-00006
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199809000-00006
This article is cited by
-
A systematic review of cardiac time intervals utilising non-invasive fetal electrocardiogram in normal fetuses
BMC Pregnancy and Childbirth (2018)
-
Comparison of ECG-based physiological markers for hypoxia in a preterm ovine model
Pediatric Research (2016)
-
Design and Testing of a Percutaneously Implantable Fetal Pacemaker
Annals of Biomedical Engineering (2013)
-
Foetal ECG and STAN technology—a review
European Clinics in Obstetrics and Gynaecology (2005)