Abstract
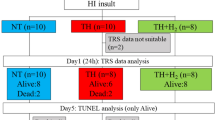
Reoxygenation and reperfusion after severe hypoxia and ischemia (HI) contribute substantially to birth asphyxia-related brain injury. Excess production of free radicals via metabolization of arachidonic acid, xanthine oxidase, and non-protein-bound iron play an important role. Cerebral reperfusion injury is characterized by a decrease in perfusion, oxygen consumption, and electrical activity of the brain. Reduction of free radical production may attenuate these features. We therefore induced severe HI in 35 newborn lambs, and upon reperfusion the lambs received a placebo [control(CONT), n = 7], the cyclooxygenase inhibitor indomethacin (INDO, 0.3 mg/kg/i.v., n = 7), the xanthine oxidase inhibitor allopurinol(ALLO, 20 mg/kg/i.v., n = 7), the iron chelator deferoxamine (DFO, 2.5 mg/kg/i.v., n = 7), or a combination of these drugs (COMB,n = 7). In each group changes (%) from pre-HI values were investigated for brain perfusion [measured by carotid artery flow(Qcar, mL/min)], (relative) cerebral O2 metabolism(CMRO2), and electrocortical brain activity (ECBA, µV) at 15, 60, 120, and 180 min post-HI. Qcar decreased significantly at 120 and 180 min post-HI in CONT (p < 0.05), but not in INDO, ALLO, DFO, and COMB groups. CMRO2 decreased significantly in CONT at 60 min post-HI (p < 0.05), remained stable in DFO and INDO, and was significantly higher in ALLO and COMB (p < 0.05) at 120 and 180 min post-HI. ECBA was significantly lower in CONT during the whole post-HI period (p < 0.05), ECBA in INDO and COMB were significantly decreased at 60 and 120 min post-HI (p < 0.05), but recovered afterward, whereas DFO and ALLO remained stable during the post-HI period. In conclusion preservation of Qcar and CMRO2, and recovery of ECBA occurred after treatment with INDO, ALLO, and DFO; combination of these drugs did not have an additional positive effect.
Similar content being viewed by others
Main
During severe birth asphyxia, HI results in inadequate mitochondrial oxidative phosphorylation leading to energy failure and brain cell damage. Although reperfusion is necessary to prevent further damage to neuronal tissue, the renewed availability of oxygen to previously ischemic brain tissue has been increasingly recognized as an important mechanism for additional brain injury. This reperfusion injury is for a substantial part mediated by the formation of free radicals(1–3). Generation of free radicals occurs through the conversion of superoxide and hydrogen peroxide from metabolization of arachidonic acid via cyclooxygenase(4), from the production of superoxide via metabolization of hypoxanthine by xanthine oxidase(1), and by transition metals such as iron to the highly toxic hydroxyl radical(5).
Administration of the cyclooxygenase inhibitor INDO, the xanthine oxidase inhibitor ALLO, or the iron chelator DFO immediately after the HI insult may reduce post-HI-reperfusion injury of the newborn brain. Moreover, the combination of these drugs may have an additional positive effect.
Because reperfusion injury after severe birth asphyxia has been characterized by cerebral hypoperfusion, and a reduced cerebral oxygen consumption and electrical activity of the brain(6–11), we investigated the patterns of brain perfusion, cerebral oxygen metabolism, and electrical brain activity during the first 3 h after severe HI in five groups of newborn lambs which received either a placebo, INDO, ALLO, DFO, or a combination of these three drugs upon reperfusion and reoxygenation. Changes in brain perfusion were assessed by measuring Qcar artery flow. Electrocorticol brain activity was monitored using a cerebral function monitor.
METHODS
Animal preparation. Surgical and experimental procedures used were reviewed and approved by the Animal Research Committee of the Leiden University Hospital and the Scientific Board of the Department of Pediatrics.
Thirty-five newborn lambs of either sex, median age 8 d (range, 4-10 d), median weight 4.0 kg (range, 3.2-5.6 kg) were studied. General anesthesia was induced with a bolus ketamine hydrochloride (3 mg/kg i.v.) and supplemented by xylazine (1 mg/kg i.m.). Local anesthesia was achieved by s.c. injection of lidocaine 1% before each skin incision. During the study period the wounds were sprayed with 1% lidocaine at regular intervals. After intubation the lambs were paralyzed with pancuronium bromide (0.2 mg/kg i.v.) and ventilated with oxygen and air, using a continuous flow, pressure-controlled ventilator(Bourns BP 200, Bear Medical Systems Inc., Riverside, CA). Ventilation was adjusted to maintain arterial Po2 and Pco2 within the normal range throughout the study. An i.v. infusion of 5% glucose in NaCl 0.9% was continued throughout the study at about 15 mL/kg/h. NaHCO3 was supplemented if the arterial pH was lower than 7.30 and the base deficit more than 5 mmol/L. Arterial blood gases and pH were measured using a Corning 178 pH/blood gas analyzer (Corning, Halstead, UK). Rectal temperature was maintained within normal range using a controlled heating mattress.
Via surgical approaches 5 or 6 F self-sealing sheaths were placed in both right and left femoral arteries and veins. The right femoral artery was used for determining Pao and for sampling of arterial blood gases, pH. Both femoral veins were used for withdrawal of blood and infusion of drugs. In the right external jugular vein a 4 F catheter was advanced retrogradely into the internal maxillary vein, to sample blood from the cerebral sinuses to measure the cerebral venous oxygen saturation. Blood from the sinuses is drained eventually by the internal maxillary veins to form the jugular veins(12). Appropriately sized ultrasonic flow transducers(Transonic Systems Inc., Ithaca, NY) were applied to fit around the carotid artery for continuous measurement of the Qcar by the transit-time technique(13). Changes in electrocortical brain activity (ECBA) were monitored using a filtered and selectively amplified one-channel Cerebral Function Monitor (Lectromed, Oxford Instruments, Oxford, UK), described by Prior(14). The Cerebral Function Monitor has a special filter which sharply attenuates frequencies below 2 and above 15 Hz, giving an amplitude-integrated recording that contains the main EEG frequencies, but with little disturbance from artifacts. The EEG signal was obtained from a pair of silver-chloride disk electrodes, placed with electrode cream at the P3 and P4 position of the 10-20 International System, i.e. in the left and right parietal region(14,15). The ECBA was recorded on a semilogarithmic scale (0-100 µV). The paper speed was 2 mm/min. Simultaneously with the amplitude curve an impedance curve records the reliability of the signal by a reference electrode positioned anterior to the scalp and shows artifacts from movement, experimental procedures, or loose electrodes. Seizures were defined as high voltage trains of sharp waves lasting more than 20-30 s.
Physiologic measurements. Changes in brain blood flow were assessed by changes in Qcar (mL/min). A recent study in fetal lambs has shown a close linear relation and acceptable assessment of agreement between Qcar and the actual brain blood flow as determined by radioactive microspheres, also during ventilation and oxygenation of these fetal lambs(16). Earlier studies in the same laboratory had shown that the cerebral perfusion in these ventilated and oxygenated fetal lambs was similar to those of newborn lambs(17). We therefore assumed that in the present study Qcar reliably assessed changes in actual cerebral blood flow. The (relative) cerebral metabolic rate of oxygen (CMRO2) was calculated as before(18), but with Qcar as a measure of actual brain blood flow: (arterial CO2 - cerebral venous CO2) ×Qcar; the results are expressed as mL O2/min, where CO2 is the blood oxygen content. CO2 is calculated as: g Hb/dL× 1.36 mL/O2/g Hb × % saturation of Hb with O2. The mean voltage of the ECBA (µV) was determined over a period of 2 min at each time point. Pao,Qcar, and the cerebral function monitor signal were measured continuously, digitized with a sample frequency of 200 Hz, and stored on a personal computer.
Experimental procedure. After completion of the surgical preparation, the lambs were allowed to achieve hemodynamic stability and to wash out their ketamine, to minimize a possible effect of ketamine on the brain(19). The period between ketamine medication and the start of the experiment was always at least 3 h. After this stabilization period, blood samples were taken, and heart rate, Pao,Qcar, and ECBA registered and used as pre-HI values. Severe HI was then induced by ventilating the lamb with 6-8% O2 supplemented with a mixture of 10% CO2 in N2 for 30 min, followed by a 5 min period of hypotension (mean Pao < 35 mm Hg), achieved by careful withdrawal of blood (50-150 mL). Upon resuscitation after completion of the HI period, six lambs received an i.v. infusion of 30 mL of 0.9% NaCl, CONT group; seven lambs received 0.3 mg/kg INDO (Indocid PDA, MSD) i.v. in 30 mL of 0.9% NaCl; seven lambs received 20 mg/kg ALLO(Apurin, Multipharma) i.v. in 30 mL of water for infusion; seven lambs received 2.5 mg/kg DFO (deferoxamine mesilaat, Ciba-Geigy) i.v. in 30 mL of 0.9% NaCl; and seven lambs received a combination of 0.3 mg/kg INDO, 20 mg/kg ALLO, 2.5 mg/kg DFO i.v. in a total volume of 30 mL. In all groups the total volume of 30 mL was infused in 30 min. Similar to the routine protocol in our neonatal unit, resuscitation was performed with extra oxygen, which was progressively lowered depending on color of the tongue and arterial blood and on the arterial blood gasses determined at regular intervals starting at 2 min after the start of resuscitation. Cardiac arrest and hypotension were treated with adrenaline (1:10.000) when appropriate. The blood withdrawn to achieve hypotension was reinfused immediately after the completion of the HI period. NaHCO3 was supplemented to correct metabolic acidosis.
At 15, 60, 120, and 180 min after completion of the HI, mean Pao was registered, blood samples were taken and percent changes relative to pre-HI values were measured for Qcar, CMR02, and mean voltage of the ECBA.
Statistical analysis. Groups of data are summarized as mean± 1 SD or SEM. Analysis of variance for repeated measurements was used to assess if there were significant changes for the various parameters within groups during the respective time periods. Differences between treatment groups at each time point were assessed by one factor analysis of variance or Kruskal-Wallis one-way ANOVA of variance depending of the distribution of the variables. If significant differences were found these procedures were followed by the Student-Newman-Keuls test or by a Mann Whitney rank test. Comparisons for mean Pao and Qcar between start and finish (during hypotension) of the HI insult were done using paired t test. A p value < 0.05 was considered statistically significant.
RESULTS
Physiologic data. Animal weight, sex, and postnatal age did not differ between groups. One CONT lamb did not survive the HI period and was excluded from the study. Rectal temperature remained always stable and within the normal range in all groups. In the CONT group four animals had two or more seizures during the post-HI period, and one lamb showed a distinct pattern of burst suppression. All treatment groups had one or two animals with two to three seizures in the post-HI period.
Table 1 summarizes the mean values (± 1 SD) of arterial pH, Po2, Pco2, and mean Pao at the various time points during the study period of the five groups of lambs. We also included the data at 2 min post-HI to illustrate the severity of the HI insult, in particular indicated by the arterial pH values. All animals developed a severe metabolic acidosis with increased lactate levels (not shown). At 2 and 15 min post-HI arterial pH and base excess values (not shown) were significantly lower compared with pre-HI values. The animals were supplemented with NaHCO3 in the early post-HI period to regain normal base excess. Total amounts of NaHCO3 administered did not differ between groups. At 2 min post-HI Pco2 values were significantly higher in all groups compared with pre-HI values, but normalized at 15 min post-HI. Mean Pao recovered in the early resuscitation phase in all groups and was significantly higher in the INDO-group at 15 and 60 min post-HI compared with pre-HI. Mean Pao, however, did not differ between groups during the post-HI period.
Pao, Qcar, and ECBA during the actual HI period. Table 2 shows the mean Pao and Qcar values (± 1 SD) of the various groups, at the start and again at the end of the HI insult during deep hypotension. During the period of hypoxia all the animals showed an initial increase in Pao, with a spontaneous sustained decrease during ongoing hypoxia. During the additional hypotensive period, a further drop of mean Pao below 35 mm Hg was achieved by careful withdrawal of blood. Qcar showed an initial 2-3-fold increase after the start of hypoxia in all lambs, but subsequently dropped during ongoing hypoxia. During the additional hypotensive period Qcar decreased to values significantly lower compared with pre-HI values in all groups. No differences in mean Pao or Qcar between groups were detected. ECBA remained stable during the hypoxia; however, during the additional hypotensive period ECBA dropped to virtually zero in all lambs.
Qcar, CMRo2, and ECBA during the post-HI period. Figure 1 shows the changes of Qcar, CMRO2, and ECBA, during post-HI compared with pre-HI values.
Qcar. There was a persistent decrease of Qcar in CONT compared with pre-HI values, which was significant at 120 and 180 min post-HI (p < 0.05). Contrary to CONT, Qcar in DFO, ALLO, and INDO groups remained stable or increased during the post-HI period. DFO and COMB showed a significant increase at 180 min post-HI compared with pre-HI values (p < 0.05). Qcar values at 120 and 180 min post-HI in the treatment groups were significantly higher compared with CONT.
CMRo2. There was a persistent decrease of CMRo2 in CONT during the post-HI period, reaching significance at 60 min post-HI versus pre-HI values (p < 0.05). Contrary to CONT, CMRo2 in all treatment groups remained stable or increased during the post-HI period; ALLO and COMB groups showed significantly higher CMRo2 values compared with pre-HI values at 180 min post-HI (p < 0.05). CMRo2 values at 120 and 180 min post-HI were significantly higher in the treatment group than the CONT group.
ECBA. There was a persistent decrease of ECBA in CONT, which was significant during the whole post-HI period compared with pre-HI values(p < 0.05). DFO and ALLO showed no significant change in ECBA values from pre-HI values during the entire post-HI period, whereas INDO and COMB, however, showed an initial decrease of ECBA post-HI, which was significant at 60-120 min post-HI (p < 0.05) compared with pre-HI values, but both groups recovered at 180 min post-HI. At this time point all treatment groups had significant higher ECBA values compared with CONT (p < 0.05).
DISCUSSION
During HI the actual insult leads to a calcium-mediated generation of free radical substances leaking to the cytoplasm of neuronal cells and to liberation of iron from its binding proteins(20–22). The free radical species induce lipid peroxidation of the cell membrane leading to formation of arachidonic acid(20,23). Simultaneously, hypoxanthine will cumulate during the actual HI insult.
Upon reoxygenation arachidonic acid will be converted to prostaglandins, thromboxanes, and leukotrienes(4), and the cumulated hypoxanthine will be metabolized to uric acid by xanthine oxidase(1,20). Both reactions give rise to excessive formation of the free radicals superoxide and hydrogen peroxide during reperfusion, which subsequently can react to form the highly toxic hydroxyl radical(1). A third important pathway for post-asphyxial free radical formation is the hydroxyl production via the non protein bound iron catalyzed Fenton or Haber-Weiss reaction(22). In terms of perfusion disturbances of the brain in the early reperfusion phase, large amounts of superoxide are also produced in the cerebral microcirculation, giving rise to subsequent plugging of capillaries by stimulated neutrophils and migration of inflammatory cells to brain tissue(3,24).
Because of the prominent role of free radical and non-protein-bound iron formation in relation to reperfusion injury of the brain after severe birth asphyxia(25), we investigated the single and combined effect(s) of INDO, ALLO, and DFO with respect to reduction of reperfusion injury of the brain. INDO prevents production of prostaglandins via cyclooxygenase inhibition leading to less production of superoxide(26). ALLO and its active metabolite oxypurinol inhibit the formation of xanthine oxidase and hence the metabolization of hypoxanthine, and at high plasma concentrations it can also act as a free radical scavenger as well as an iron chelator(27–29). DFO is an iron chelator, preventing non-protein-bound iron to react with hydrogen peroxide to form the hydroxyl radical(5,25).
The present study shows that severe hypoxic ischemia induces a decrease in Qcar and CMRO2, and an abnormally low ECBA during at least the first 3 h upon reperfusion and oxygenation. Experimental studies in neonatal and adult animals exposed to global cerebral ischemia reported a relation between early postischemic cerebral hypoperfusion and a disturbed cerebral metabolism of oxygen on the one hand and brain tissue damage and brain edema on the other hand(8,24,30,31). Treatment with free radical scavengers prevented this early decrease in cerebral perfusion and oxygen metabolism(6,10,11) and hence brain tissue damage and edema(31,32). Moreover, a recent study in severe asphyxiated newborn babies showed a relation between a decrease in cerebral blood volume during the first 12 h of age and adverse outcome(33). Although the cerebral electrical activity quickly disappears during and after severe perinatal HI, long before any brain injury has occurred(15), prolonged neurologic depression is predictive of poor outcome(9,34). We therefore suggest that the significant post-HI decrease in Qcar, CMRO2, and ECBA in the placebo-treated lambs strongly suggest reperfusion injury of the brain. We further suggest that reduction of free radical formation with the various drugs used in these study curtails or even prevents these hemodynamic, metabolic, and electrical abnormalities of the brain and hence reperfusion damage.
INDO showed indeed a preservation of brain perfusion and oxygen metabolism of the brain, despite earlier studies showing that INDO lowered perinatal cerebral perfusion by inhibition of vasodilating prostaglandins(35). It may be possible that mechanisms induced by HI insult did override a prostaglandin-induced decrease of brain perfusion. With respect to a systemic effect of INDO, we did not find important changes in blood pressure and/or heart rate during the post-HI period or differences with the other groups, although INDO was the only drug inducing a transient but significant increase in Pao during the post-HI period. An earlier study in newborn lambs of comparable age showed that INDO did not alter cardiac hemodynamics and myocardial performance(36).
ALLO prevented Qcar, CMRO2, and ECBA from dropping throughout the study period. This is in line with a recent study of our group with severely asphyxiated babies treated with high dose ALLO (40 mg/kg), which showed that brain perfusion and electrical brain activity were significantly less affected in ALLO-treated compared with nontreated babies. These infants had also significant lower non-protein-bound iron and malondialdehyde concentrations in their plasma(37). Experimental studies suggest also a beneficial effect of this drug on post-asphyxial reperfusion injury(23,29). More recent studies, however, suggest a dose dependency with respect to this effect; especially high dosages are necessary to use its direct free radical scavenging abilities and metal-ion chelator properties(27–29). It must, however, be stressed that ALLO reduces plasma uric acid concentrations, an important endogenous antioxidant(38).
The DFO group showed preservation of Qcar, CMRO2, and ECBA during the entire post-HI period, and Qcar was even higher at 180 min post-HI compared with pre-HI values. Moreover, the DFO-treated lambs, together with the ALLO-treated lambs, showed ECBA values that never were significantly different from pre-HI values.
DFO has proven to ameliorate hypoxic-ischemic brain damage in newborn dogs(11). A recent study by Dorrepaal et al.(25) showed a relation between adverse outcome (death or neurologic abnormalities) due to severe birth asphyxia and the concentration of non-protein-bound iron in plasma during the first 8 h of life of full-term babies. The remarkable increase of brain perfusion in the post-HI period in the DFO-treated lambs may also be explained by the vasodilating properties of this drug(39). This mechanism may also explain the toxic effects of DFO on the systemic and cardiovascular system as described by deLemos et al.(40) in premature baboons with hyaline membrane disease. However, these animals received much higher dosages of DFO. We therefore aimed at administration of an appropriate dosage of DFO in the present study. From an earlier similar experimental protocol, in which post-HI plasma concentrations of non-protein-bound iron were measured(8), we calculated the exact amount of DFO needed to bind these non-protein-bound iron. It appeared that much smaller amounts of DFO were needed compared with other studies(5,39,40). We indeed did not detect negative cardiovascular effects in the DFO-treated lambs.
Combination therapy of INDO, ALLO, and DFO showed no synergistic effect on Qcar, CMRO2, and ECBA compared with the single treatment groups. This may be partly caused by the fact that all drugs had a more or less optimal effect on these parameters. In this study of short duration we were not able to investigate more conclusive parameters like histologic data. On the other hand, looking at the electrical brain activity data, both the INDO and COMB groups, showed a significant drop in voltage down to 70% during the post-HI period compared with pre-HI values. Although the the pattern of brain perfusion (Qcar) does not support this statement, it might be explained by an INDO-induced decrease in cerebral microcirculation; Qcar probably does not always reflect changes at the level of the microcirculation. The suggested overall free radical reducing abilities of the combination of the drugs in the COMB group might therefore not outweigh a possible negative effect of INDO on the microcirculation.
In conclusion, we did not find important differences between monoregimen and combination therapy, which focused on three important free radical generating processes, with respect to the patterns of Qcar, CMRO2, and ECBA during the reperfusion phase after severe HI. A single drug approach was as effective as combination of INDO, ALLO, and DFO to preserve perfusion, O2 metabolism, and electrical activity of the brain, although DFO and ALLO showed a somewhat better result in the preservation of post-asphyxial electrical brain activity.
Abbreviations
- ALLO :
-
allopurinol
- CMR O2 :
-
(relative) cerebral metabolic rate of oxygen
- COMB :
-
combination therapy
- DFO :
-
deferoxamine
- CONT :
-
control
- ECBA :
-
electrocortical brain activity
- HI :
-
hypoxia-ischemia
- INDO :
-
indomethacin
- P ao :
-
aortic blood pressure
- Q car :
-
carotid artery flow
References
Saugstad OD, Aasen AO 1980 Plasma hypoxanthine concentrations in pigs: a prognostic aid in hypoxia. Eur Surg Res 12: 123–129.
McCord JM 1985 Oxygen derived free radicals in post ischemic tissue injury. N Engl J Med 312: 159–163.
Palmer C 1995 Hypoxic-ischemic encephalopathy: therapeutic approaches against microvascular injury and role of neutrophils, PAF, and free radicals. Clin Perinatol 22: 481–517.
Wolfe L 1982 Eicosanoids: prostaglandins, thromboxanes, leukotrienes and other derivatives of carbon 20 unsaturated fatty acids. J Neurochem 38: 1–14.
Palmer C, Roberts RL, Bero C 1994 Deferoxamine posttreatment reduces ischemic brain injury in neonatal rats. Stroke 25: 1039–1045.
Thiringer K, Hrbek A, Karlsson K, Rosen KG, Kjellmer I 1987 Postasphyxial cerebral survival in newborn sheep after treatment with oxygen free radical scavengers and a calcium antagonist. Pediatr Res 22: 62–66.
Pourcyrous M, Parfenova H, Bada HS, Korones SB, Leffler CW 1997 Changes in cerebral cyclic nucleotides and cerebral blood flow during prolonged asphyxia and recovery in newborn pigs. Pediatr Res 41: 617–623.
Dorrepaal CA, Shadid M, Steendijk P, Van Der Velde ET, Van De Bor M, Baan J, Van Bel F 1997 Effect of posthypoxic-ischemic inhibition of nitric oxide synthesis on cerebral blood flow, metabolism and electrocortical brain activity in newborn lambs. Biol Neonate 72: 216–226.
Williams CE, Gunn AJ, Mallard EC, Gluckman PD 1991 Outcome after ischemia in the developing sheep brain: an electro-encephalographic and histological study. Ann Neurol 31: 14–21.
Hossmann KA 1993 Ischemia mediated neuronal injury. Resuscitation 26: 225–235.
Hurn PD, Koehler RC, Blizzard KK, Traystman J 1995 Deferoxamine reduces early metabolic failure associated with severe cerebral ischemic acidosis in dogs. Stroke 26: 688–695.
May NDS 1970 The Anatomy of Sheep: A Dissection Manual. University of Queensland press, Queensland, 133–266.
Dobsen AD, Sellers AF, McLeod FD 1986 Performance of a cuff-type blood flowmeter in vivo. J Appl Physiol 21: 1642–1648.
Prior PF 1979 Monitoring Cerebral Function: Long Term Recordings of Electrical Activity. North Holland Biomedical Press, Amsterdam, 45–301.
Hellstrom-Westas L, Rosen I, Svenningsen NW 1995 Predictive value of early continuous amplitude integrated EEG recordings on outcome after severe birth asphyxia in full term infants. Arch Dis Child 72:F34–F38.
Van Bel F, Roman C, Klautz RJM, Teitel DF, Rudolph AM 1994 Relationship between brain blood flow and carotid arterial flow in the sheep fetus. Pediatr Res 35: 329–333.
Iwamoto HS, Teitel DF, Rudolph AM 1987 Effect of birth-related events on blood flow distributions. Pediatr Res 22: 634–640.
Jones MD, Traystman RJ, Simmons MA, Molteni RA 1981 The effects of changes in arterial O2 content in cerebral blood flow in lamb. Am J Physiol 240:H209–H251.
White PF, Way WL, Trevor AJ 1982 Ketamine-its pharmacology and therapeutic uses. Anesthesiology 56: 119–136.
Morley P, Hogan MJ, Hakim AM 1994 Calcium-mediated mechanisms of ischemic injury and protection. Brain Pathol 4: 37–47.
Fellman V, Raivo KO 1997 Reperfusion injury as the mechanism of brain damage after perinatal asphyxia. Pediatr Res 41: 599–606.
Halliwell B 1992 Reactive oxygen species and the cerebral nervous system. J Neurochem 59: 1609–1623.
Vanucci RC 1990 Experimental biology of cerebral hypoxia-ischemia: relation to perinatal brain damage. Pediatr Res 27: 317–326.
Hudome S, Palmer C, Roberts RL, Mauger D, Housman C, Towfighi J 1997 The role of neutrophils in the production of hypoxic-ischemic brain injury in the neonatal rat. Pediatr Res 41: 607–616.
Dorrepaal CA, Berger HM, Benders MJNL, Van Zoeren-Grobben D, Van De Bor M, Van Bel F 1996 Nonprotein bound iron in postasphyxial reperfusion injury of the newborn. Pediatrics 98: 883–889.
Pourcyrous M, Leffler CW, Bada HS 1993 Brain superoxide generation in asphyxiated piglets and the effect of indomethacin at therapeutic doses. Pediatr Res 34: 366–369.
Moorhouse PC, Grootveld M, Halliwell B, Quinlan JG, Gutteridge JMC 1987 Allopurinol and oxypurinol are hydroxyl radical scavengers. FEBS Lett 213: 23–28.
Ko KM, Godin DV 1990 Inhibition of transition metal ion-catalysed ascorbate oxidation and lipid peroxidation by allopurinol and oxypurinol. Biochem Pharmacol 40: 803–809.
Palmer C, Vannucci RC, Towfighi J 1990 Reduction of perinatal hypoxic ischemic brain damage with allopurinol. Pediatr Res 27: 332–336.
Grice SC, Chappell ET, Prough DS, Whitley JM, Su M, Watkins WD 1987 Ibuprofen improves cerebral blood flow after global cerebral ischemia in dogs. Stroke 18: 787–791.
Johshita H, Asano T, Hanamura T, Takakura K 1989 Effect of indomethacin and a free radical scavenger on cerebral blood flow and edema after cerebral artery occlusion in cats. Stroke 20: 788–794.
Tasdemiroglu E, Macfarlane E, Wei EP 1992 Pial vessel caliber and cerebral blood flow become dissociated during ischemia-reperfusion in cats. Am J Physiol 263:H533–H538.
Van Bel F, Dorrepaal C, Benders MJNL, Zeeuwe P, Van De Bor M, Berger HM 1993 Changes in cerebral hemodynamics and oxygenation in the first 24 hours after birth asphyxia. Pediatrics 92: 365–371.
Sarnat H, Sarnat M 1976 Neonatal encephalopathy following fetal distress. Arch Neurol 33: 696–705.
Van Bel F, Klautz RJM, Steendijk P, Schipper IB, Teitel DF, Baan J 1993 The influence of indomethacin on the autoregulatory ability of the cerebral vascular bed in the newborn lamb. Pediatr Res 34: 178–181.
Klautz RJM, Van Bel F, Teitel DF, Steendijk P, Baan J 1993 Myocardial perfusion and performance after indomethacin administration. Pediatr Res 33: 295–301.
Van Bel F, Shadid M, Dorrepaal CA, Fontijn J, Monteiro L, Van De Bor M, Berger HM 1998 Effect of allopurinol on postasphyxial free radical formation, cerebral hemodynamics and electrical brain activity. Pediatrics 101: 185–195.
Saugstad OD 1996 Role of xanthine oxidase and its inhibitor in hypoxia: reoxygenation injury. Pediatrics 98: 103–107.
Fordor JR, McClanahan TB, Gallagher KP, Hedlund BE, Hallaway PE, Shlafer M 1990 Hemodynamic effects of intraarterial administration of deferoxamine or deferoxamine-pentafraction conjugate to conscious dogs. J Cardiovasc Pharmacol 16: 742–749.
deLemos RA, Roberts RJ, Coalson JJ, deLemos JA, Null DM, Gerstmann DR 1990 Toxic effects associated with the administration of deferoxamine in the premature baboon with hyaline membrane disease. Am J Dis Child 144: 915–919.
Author information
Authors and Affiliations
Additional information
Supported by a grant from the Dutch Heart Association (M.S.); Sub No. 93.101.
Frank van Bel, M.D., Ph.D., Wilhelmina Children's Hospital, Department of Neonatology, PO Box 18009, 3501 CA Utrecht, The Netherlands.
Rights and permissions
About this article
Cite this article
Shadid, M., Moison, R., Steendijk, P. et al. The Effect of Antioxidative Combination Therapy on Post Hypoxic-Ischemic Perfusion, Metabolism, and Electrical Activity of the Newborn Brain. Pediatr Res 44, 119–124 (1998). https://doi.org/10.1203/00006450-199807000-00019
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199807000-00019
This article is cited by
-
Neuroprotective Effects of Indomethacin and Aminoguanidine in the Newborn Rats with Hypoxic-Ischemic Cerebral Injury
Neurochemical Research (2005)
-
Neuroprotectieve behandelingsstrategieën na perinatale hypoxie-ischemie
Tijdschrift voor kindergeneeskunde (2003)