Abstract
Coagulase-negative staphylococcal septicemia is the most prominent nosocomial infection in neonatal intensive care units. Immaturity of host defenses in premature neonates is assumed to constitute an important risk factor. Opsonophagocytosis is considered to be the key host defense system against staphylococci with IgG antibodies as a major opsonin. For this reason we have studied serum IgG antibody titers and opsonic activity to coagulase-negative staphylococci in 20 infants with septicemia and 40 matched control subjects. In addition, we assessed the effect of administration of fresh frozen plasma (FFP) on IgG antibody titer and serum opsonic activity in 12 patients with septicemia. IgG antibodies, quantified by ELISA and opsonic activity, determined by flow cytometry, were expressed as a percentage of the value of pooled normal human reference serum. Both patients and control subjects showed low IgG titers (median, 21%; range, 1-192%) and a low opsonic activity (median, 33%; range, 8-484%) at birth. During the first 2 postnatal wk IgG titers decreased significantly in septicemia patients (from a median of 30 to 17%, p = 0.025), but not in control subjects, whereas opsonic activity remained unchanged. The titer of IgG antibodies increased significantly in septicemia patients after FFP administration (from a median of 17 to 41%, p = 0.002), whereas the effect on opsonic activity was unpredictable, showing a moderate increase in 10 out of 12 infants, and in 2 patients even a substantial decrease (>50%), despite adequate opsonic activity in the corresponding FFP batches. Immunoblotting of sepsis isolates with the corresponding patient sera demonstrated that septicemic infants may generate IgG antibodies against their blood isolate. Neonates who acquire coagulase-negative staphylococcal septicemia cannot be distinguished from control subjects on the basis of IgG antibodies and opsonic activity to staphylococci either at birth or during the first 2 postnatal wk. The administration of FFP to septicemia neonates has an unpredictable effect on opsonic activity and therefore does not seem to be a useful addition to antibiotic therapy.
Similar content being viewed by others
Main
Nosocomial septicemia due to coagulase-negative staphylococci remains the most prominent type of hospital-acquired infection in neonatal intensive care units. It is reported to account for 31-55% of all nosocomial infections in these units(1–3). Several risk factors have been identified, such as central intravascular lines, total parenteral nutrition, prematurity(1–4), and endotracheal intubation(5). In addition, in previous studies we found suggestive evidence for a relation between the immaturity of host defenses in premature infants and the risk of developing coagulase-negative staphylococcal septicemia(4). It has been established that opsonophagocytosis is an essential host defense mechanism against staphylococci with IgG antibodies and complement component C3 as major opsonins(6, 7). Opsonic activity to coagulase-negative staphylococci was diminished in serum from premature infants as compared with adult serum and was related to the degree of prematurity. Opsonic activity in premature serum proved to be exclusively dependent on complement activation(8). It was concluded from these data that transplacental IgG antibodies to coagulase-negative staphylococci present in newborn serum were opsonically deficient. Subsequent studies by others have confirmed the opsonic defect in neonatal IgG against staphylococci(9). In addition to a qualitative deficiency in transplacental IgG, Lassiter et al.(10) found an IgG concentration in serum from neonates of <350 mg/dL to be a predisposing factor for the acquisition of septicemia.
Intravenous administration of IgG was shown to reduce the incidence of septicemia when the IgG concentration was maintained at a minimum level of 700 mg/dL(11). However, studies concerning the prophylactic use of IVIG yielded controversial results. Fanaroff et al.(12) studied prophylactic use of IVIG in a large, prospective, double-blind, placebo-controlled, multicenter trial among 2416 infants. IVIG failed to reduce the incidence of hospital-acquired infections in very low birth weight infants(12). Baker et al.(13), however, showed a significant reduction in late onset, nosocomial infection after administration of IVIG (500 mg/kg). Furthermore, the time to infection was increased in the IVIG-treated patients, whereas the duration of hospital stay was decreased, although the latter was probably more related to a therapeutic effect of IVIG, rather than to a prophylactic effect(13). The results obtained with the majority of recent IVIG neonatal prophylaxis studies in neonatal intensive care units did not warrant the use of IVIG to prevent nosocomial infections, as suggested by Hill(14) in a recent review. Therefore, it is still controversial whether IVIG administration is of value in protecting premature neonates against nosocomial coagulase-negative staphylococcal septicemia. In addition, it has never been formally addressed whether low IgG antibody titers or poor opsonic activity to coagulase-negative staphylococci in serum of premature neonates are predictive for the development of coagulase-negative staphylococcal septicemia.
As pointed out above, complement may be essential for adequate elimination of staphylococcal infection in the premature infant. For this reason it seemed justified to administer FFP to premature infants with clinical signs of late onset sepsis. FFP is supposed to supply both complement components and specific IgG antibodies against coagulase-negative staphylococci, because most adult sera contain IgG antibodies to coagulase-negative staphylococci(15). The aims of the present study were to determine IgG antibody titers and opsonic activity in preterm infants with coagulase-negative staphylococcal septicemia and matched controls to examine whether these values are predictive for the risk of acquiring septicemia. In addition, the response in antibody titers and opsonic activity in septicemic infants and the effect of FFP administration on these parameters were studied.
METHODS
Subjects. During a period of 16 mo, all neonates admitted to the neonatal intensive care unit within 24 h after birth were included in the study. Informed parental consent was obtained for all infants. From each infant serum was collected within 24 h and subsequently after 1, 2, 4, 6, and 8 wk after birth and immediately stored at -70°C.
When clinical signs of septicemia occurred, serum was collected before therapy initiation and 7 d after the onset of septicemia. In the case of FFP administration 1-mL samples of each batch were stored at -70°C.
The decision for administering FFP was based on clinical grounds by the attending neonatologist, depending on the degree of clinical deterioration, usually when diminished peripheral circulation and hypotension occurred. When septicemia due to coagulase-negative staphylococci was proven, the patient was enrolled in the study, and two control patients were selected, matched by gestational age, birth weight, and diagnosis.
Pooled normal human serum. Serum from 30 healthy adults was collected and pooled. Sera were stored in 1-mL aliquots at -70°C until use. These sera served as reference sera.
Buffers. GHBSS (GIBCO, Paisley, UK), pH 7.2, containing 0.1% gelatin, was used for the dilution of serum, bacteria, and PMN in the phagocytosis assay. RPMI-0.1% wt/vol gelatin, pH 7.4 (GIBCO), and PBS (20 mM), pH 7.4, served as washing buffers during the preparation of PMN and in the phagocytosis assay, respectively. PBS containing 0.1% Tween 20 was used as washing buffer in the ELISA.
Bacteria . Staphylococcus epidermidis isolates, obtained from neonatal blood during infection, were maintained on blood agar plates. S. epidermidis strain 867, a blood isolate from a case of neonatal septicemia, was included in all opsonic and ELISA studies as a reference strain. The bacteria were grown overnight at 37°C in nutrient broth (containing 5 mg/mL NaCl and 20 mg/mL nutrient broth; Difco, Detriot, MI; in distilled water). The bacteria were killed by heat treatment (56°C; 1 h). Subsequently, the bacterial cells were washed three times with GHBSS and adjusted to a concentration of 5 × 108 cfu/mL using a photospectrometer (Dr. Lange, Berlin, Germany).
Polymorphonuclear leukocytes. PMNs were isolated from a fresh buffy coat. Blood from the buffy coat was diluted 1:2 in PBS. This mixture was loaded onto a layer consisting of a mixture of 12 mL of Histopaque (Pharmacia, Uppsala, Sweden) and 10 mL of Ficoll (Pharmacia). After centrifugation (400× g, 20 min), the monocytes and lymphocytes were removed. The remaining erythrocytes were lysed, using a 0.2% wt/vol NaCl solution for 90 s, and subsequently the pellet was washed with 3% wt/vol NaCl solution and centrifuged (250 × g, 10 min), which procedure was repeated twice. The cell pellet containing PMN was washed once with ice-cold (0°C) RPMI-0.1% wt/vol gelatin, pH 7.4, and adjusted to a concentration of 1 × 107 PMN/mL in GHBSS.
Fluorometric opsonophagocytosis assay. For opsonization, 20μL of 5 × 108 FITC-labeled staphylococci were mixed with 80μL of serum dilution in GHBSS and incubated at 37°C for 30 min in a gently shaking waterbath. The reaction was stopped by adding 2.5 mL of ice-cold PBS. Subsequently, the bacteria were spun down at 1500 ×g at 4°C for 15 min to concentrate the opsonized bacteria. Next, 50-μL samples of PMN suspension (1 × 107 PMN/mL) were added, whereafter the mixtures were incubated at 37°C in a shaking waterbath for 12 min. The reaction was stopped by adding 2.5 mL of ice-cold PBS. PMN and PMN-associated staphylococci were separated from free bacteria by differential centrifugation at 160 × g and 4°C for 7 min, washed twice with PBS, and suspended in 100 μL of GHBSS and 100 μL of 2% wt/vol paraformaldehyde. The cells were then examined by flow cytometry using a FACScan (Becton Dickinson, Mountain View, CA). FITC emission was measured using a 530/30 nm filter. The opsonic activity of all sera was expressed as the inverse of the percentage of serum corresponding to 50% positive(fluorescent) PMN. The opsonic activity of patient sera and FFP were related to the opsonic activity of pooled normal human serum, which was set at 100%. As an internal control, opsonization of S. epidermidis strain 867 in pooled normal human serum was included in all opsonization studies. The percentage of pooled normal human serum needed to induce 50% positive PMN was remarkably stable and was in all experiments 0.6%. The amount of pooled normal human serum needed to induce 50% positive PMN with the septicemia strains was also remarkably similar and ranged from 0.34 to 1.03%, with one extreme value of 1.79% for one of the patient strains. All experiments were performed in duplicate.
ELISA for S. epidermidis IgG antibodies. The ELISA was performed in polyvinyl chloride microtiter plates (Flow Laboratories, McLean, VA). The plates were coated by adding 100 μL of bacterial suspension (1 × 107 cfu/mL in PBS), incubation at 37°C for 1 h, and subsequent incubation at 4°C overnight. PBS containing 0.1% Tween 20 was used as the washing buffer after each coating or incubation step. Sera (50 μL) were serially 2-fold diluted in PBS containing 0.05% Tween 20 and 1% BSA, and the dilutions were incubated in the microtiter plates at 37°C for 1 h. Next, a goat anti-human IgG-H/L-peroxidase (Nordic, Tilburg, The Netherlands) (50 μL, 1:1000 in PBS/0.05% Tween 20/1% BSA) was added and incubated at 37°C. After extensive washing, 50 μL of a substrate mixture consisting of tetramethylbenzidine (Sigma Chemical Co., St. Louis, MO) (6.0 mg of DMSO/mL) and urea peroxide (144 mg/7.5 mL H2O) in 0.1 M sodium acetate/citrate buffer (pH 5.5) were added to each well, and the plates were incubated at 37°C for 10 min. Substrate conversion was stopped by the addition of 50μL of 1 M sulfuric acid. Absorbance values at 450 nm were determined using a multivalent ELISA reader.
The ELISA values of individual sera were expressed as percentage of the pooled normal human serum value, which was arbitrarily set at 100%. All ELISAs were performed in duplicate.
Immunoblotting of staphylococcal lysates. Staphylococcal cell wall proteins were isolated and analyzed essentially as described previously(16). Briefly, staphylococcal cell wall proteins were isolated by treating bacterial suspensions of 1010 cfu/mL with lysostaphin. After centrifugation (14 000 × g, 15 min) the supernatants containing cell wall proteins were subjected to SDS-PAGE. After electrophoresis, the gel was incubated in blot-buffer to remove remaining SDS. Subsequently, the staphylococcal cell wall proteins were blotted from the gel onto a nitrocellulose membrane. Free protein sites on the membrane were blocked by blocking buffer (containing gelatin and Tween 20). After washing, the membrane was cut into strips which were incubated with pooled normal human serum or polyclonal rabbit hyperimmune serum raised against a mixture of coagulase-negative staphylococcal blood isolates. After washing three times, the strips were subsequently incubated with either a goat anti-human IgG-H/L- or a goat anti-rabbit IgG-H/L-peroxidase-labeled conjugate. The membrane strips were washed once more and stained by tetramethylbenzidine (Sigma Chemical Co.) 0.2% wt/vol and dioctyl sulfosuccinate (Serva, Heidelberg, Germany) 0.8% wt/vol dissolved in 10 mL of a buffer mixture consisting of ethanol 96%, citric acid, and Na2HPO4. The reaction was started by adding H2O2 and stopped by rinsing with tap water.
C3 deposition on S. epidermidis. All procedures except the incubations were executed on ice. The sera were diluted in GHBSS. To 80-μl samples of the serum dilutions, 50 μL of bacteria (5 × 108 cfu/mL) were added, whereafter the mixtures were incubated at 37°C for 30 min. After incubation, the bacteria were washed twice with ice-cold PBS. Deposited C3 was determined by adding 50 μL of FITC-conjugated F(ab′)2 fragments of goat anti-human C3(Cappel-Organon Teknika, Turnhout, Belgium; diluted 1:200) to the bacterial suspension and incubating the mixture at 4°C for 30 min. Subsequently, the bacteria were washed twice with ice-cold PBS. Next, the pellet was suspended into 200 μL of GHBSS. Mean fluorescence was determined by FACScan (Becton Dickinson), and the values obtained for the individual sera were expressed as a percentage of the value of pooled normal human serum, which was arbitrarily set at 100%.
Statistics. IgG titers and opsonic activity of patient sera were presented as median and range. Differences between patients and controls were assessed by Mann-Whitney U test; differences between paired data within either septicemia patients or control patient groups were assessed by the Wilcoxon matched pairs signed rank test. Correlations were calculated by Spearman's rank correlation method and expressed as rank correlation coefficient ρ. All calculations were performed by the use of SPSS 7.5 for Windows (SPSS Inc., Chicago, IL).
RESULTS
Demographic characteristics of patients with coagulase-negative staphylococcal septicemia. During the study period 497 patients were admitted to our neonatal intensive care unit. Coagulase-negative staphylococcal septicemia occurred in 22 patients (incidence, 4.5%). Complete documentation was available for 20 septicemia patients. Therefore, 60 patients entered the study (20 with septicemia and 40 control patients). Both the median and mean gestational ages of the patients with septicemia were 30 wk(range, 26-32.5 wk) and of the control infants 29 wk (range, 27-32 wk). The mean birth weight of the septicemia infants was 1285 g, median birth weight 1230 g (range, 750-2200 g); for the control infants these values were mean 1140 g, median 1130 g (range, 650-1610 g), respectively. The male to female ratio was 9:11. The mean age at onset of coagulase-negative staphylococcal septicemia was 14 d, median 13 d (range, 6-26 d).
Antibody and opsonic responses of patients with coagulase-negative staphylococcal septicemia. The titer of IgG antibodies and opsonic activity to coagulase-negative staphylococci in premature serum were expressed as percentage of the values in pooled normal human serum. The data, presented as median and range, are summarized in Table 1. The values for both the IgG titers and opsonic activity at birth were in the low range; the cumulative 75% values for IgG titers and opsonic activity were 61 and 51%, respectively. The median IgG titer was 21% of pooled normal human serum(range, 1-192%), the median serum opsonic activity 33% (range, 8-484%). However, the IgG titers at birth of the septicemia patients were higher than of the control patients; median 30% (range 1-192%) in the septicemia patients and 10% (range 1-126%) in the control patients, although this difference was just not statistically significant at the 5% level (p = 0.06). As expected, a decrease in IgG titer was noticed from the day of birth to either the age of 14 d (in the control patients), or the day of onset of septicemia. In the septicemia and control patients together, the IgG titer decreased from a median of 21% at birth to 9.5% (range, 1-187%) (p = 0.17). When considering the IgG titers in septicemia and control patients separately, it was found that the IgG titer in the septicemia patients showed a significant decrease, from a median of 30 to 17% (range, 1-79%) (p = 0.025), whereas the decrease in IgG titer in the control patients, from a median of 10 to 5% (range, 1-187%) was not significant (p = 0.344). The IgG levels at either d 14 in controls or at the day of septicemia in septicemia patients were not significantly different (p = 0.322).
Unlike the pattern found in IgG titers, serum opsonic activity changed little in the first 2 postnatal wk in the two patient groups, from a median of 33% at the day of birth, to a median of 28% (range, 3-112%) either at the age of 14 d in control subjects or at the day of onset of septicemia. When the opsonic activity in septicemia and control patients was considered separately, again only very small differences were found within both groups. In the septicemia patients the opsonic activity decreased from a median of 28%(range, 8-484%) at birth to 25% (range, 3-112%) at onset of septicemia. In the control patients the opsonic activity increased slightly from a median of 38%(range, 14-90%) at birth to 41% (range, 5-104%) at the age of 14 d. None of these small differences was statistically significant. In contrast to the higher IgG titer found at birth in the septicemia patients compared with the control patients, the serum opsonic activity was higher in the control patients than in the septicemia patients, both at birth and at 14 d or at onset of septicemia, respectively. However, these differences were not statistically significant (p = 0.152 and p = 0.114, respectively).
In 12 of the septicemia patients FFP was administered during the first 3 d after onset of septicemia. The effect of FFP administration on antistaphylococcal IgG titers is presented in Figure 1. Compared with the titer at the moment of onset of septicemia, an increase in IgG titers was observed in all patients. The median IgG titer increased from 17% (range, 1-79% of pooled normal human serum) to a median of 41% (range, 4-212%) (p = 0.002). The increase in IgG titer after FFP administration did not correlate with the highly varying titers, from 10 to 170% of pooled normal human serum, of the FFP batches used (Spearman ρ =-0.091, p = 0.803).
Effect of FFP on IgG titer. Box plot of IgG titer to coagulase-negative staphylococci in septicemia patients at onset of septicemia(pre-FFP) and after administration of FFP (post-FFP). The box represents the median value and the cumulative 25 and 75% levels. The vertical lines represent the range. The IgG titer is expressed as percentage of IgG of pooled normal human reference serum.
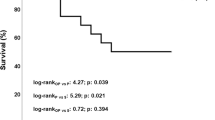
The effect of administration of FFP on opsonic activity is presented in Figure 2. The serum opsonic activity after administration of FFP moderately increased from a median of 25% (range, 3-112%) to a median of 36% (range, 1-82%) in 10 septicemia patients, which increase was not statistically significant (p = 0.099). In two patients the opsonic activity showed a substantial decrease, from 87 to 27% in one patient and from 17 to 1% in the other. Similar to the variation in IgG titers of the FFP batches, a considerable variation was noticed in the opsonic activity of the batches used (range, 6-318% of pooled normal human serum). In the two patients who showed a decrease in opsonic activity after FFP administration, the opsonic activity toward coagulase-negative staphylococci of their FFP batches used was about equal to pooled normal human serum (85 and 100%, respectively). The increased opsonic activity of patient sera after FFP administration did not correlate with the opsonic activity of FFP batches used (Spearman ρ =-0.419, p = 0.228).
Effect of FFP on opsonic activity. Box plot of opsonic activity to coagulase-negative staphylococci in septicemia patients at onset of septicemia (pre-FFP) and after administration of FFP(post-FFP). The box represents the median value and the cumulative 25 and 75% levels. The vertical lines represent the range. The opsonic activity is expressed as percentage of the value in pooled normal human reference serum.
In addition, no correlation could be established between the increase in IgG titers and the increase in opsonic activity after FFP administration(Spearman ρ = 0.067, p = 0.855).
This absence of correlation suggests a role for heat-labile opsonins(complement) in the post-FFP increased opsonic activity. For this reason C3 deposition on coagulase-negative staphylococcal isolates was estimated in four patients after FFP administration. These four patients were selected, because in three a moderate to strong increase in opsonic activity was observed, which was not accompanied by an increase in antistaphylococcal IgG titer, whereas in one other patient a strong increase in opsonic activity was associated with only a moderate increase in IgG titer. All showed an increase in C3 deposition on their blood isolate after FFP administration, and in three of the four cases there was a strong increase (7.5-54-fold). In two of these three patients, a strong increase in opsonic activity was also found (6- and 10.5-fold, respectively). However, in the third patient the increase in opsonic activity was only moderate (1.5-fold). Thus, for the amount of C3 deposited there did not seem to be also a clear correlation with an increase in opsonic activity after FFP administration.
In three patients with coagulase-negative staphylococcal septicemia who did not receive FFP, the serum opsonic activity did not change, whereas the IgG titer showed a significant increase in one of them (19-fold). Apparently, in this patient the IgG titer increased as a result of production of antistaphylococcal IgG antibody by the patient. This finding suggests that, at least in some cases, IgG antibodies to coagulase-negative staphylococci were generated by the patients themselves, without a significant contribution of FFP administration. This suggestion was confirmed by immunoblot banding patterns of surface proteins of the coagulase-negative staphylococcal blood isolates of three patients, incubated with patient sera after the sepsis episode: two of these three patients received FFP. Figure 3 shows the banding pattern of serum of patient 6, in whom septicemia was caused by two different coagulase-negative staphylococcal strains. Three days after FFP administration, this patient showed a densely stained band on immunoblotting, corresponding to a molecular mass of 34 kD in both sepsis-causing strains; this band was not found in the immunoblot of the corresponding FFP batches. In patient 7, who also received FFP, reactivity to two bands appeared (proteins of 11 and 20 kD), which bands were also not found in the immunoblot of the FFP batches. In patient 8, who did not receive FFP, reactivity to bands 20, 95, and 111 kD appeared (immunoblots of these latter two patients are not shown).
Immunoblot banding pattern of antibodies in a sepsis patient. Immunoblot pattern of antibodies in serum of patient 6, to the two coagulase-negative staphylococcal blood isolates. Immunoblot of the first strain in lanes 1-5, of the second strain in lanes 6-10. Banding pattern of antibodies on the day of birth in lanes 1 and 6, on the day of sepsis in lanes 2 and 7. Banding pattern of antibodies in FFP in lanes 3 and 8, in pooled normal human serum in lanes 5 and 10. In lanes 4 and 9, the banding pattern of serum proteins, 3 d after occurrence of septicemia, shows new bands of 34 kD. The molecular mass of marker proteins is indicated on the left side of the immunoblots.
DISCUSSION
This study demonstrates that the opsonic activity and the IgG antibody titers to coagulase-negative staphylococci are considerably lower in serum from premature newborns than in serum from normal adults, as reported previously(1, 8, 9). In previous studies, a relationship was found between gestational age and the degree of deficiency in these humoral defenses(4). Due to the low number of patients included, this relation could not be assessed in the present study. There are several risk factors for neonatal nosocomial septicemia including the degree of prematurity, low birth weight, artificial ventilation, central intravascular lines, and prolonged total parenteral nutrition. However, in spite of equal risk factors, more than 10% of the patients admitted to neonatal intensive care units are reported to develop coagulase-negative staphylococcal septicemia, suggesting individual variations in host defense mechanisms. Differences in bacterial factors might play an additional role(1, 2).
In the present study, we focused on host defenses to coagulase-negative staphylococci. Opsonic activity and IgG titers to coagulase-negative staphylococci were measured in infants with septicemia and a comparable group of infants who did not develop septicemia. At birth, no difference in opsonic activity was noted between patients with septicemia and control patients. However, the IgG titers at birth were higher in the septicemia patients than in the control patients, although this difference was just not significant(p = 0.06). These findings are in contrast with data published by Lassiter et al.(10), who showed a significantly lower total IgG titer in the serum of patients in whom nosocomial septicemia occurred than in the control group. It should, however, be noted that these authors determined total IgG rather than specific IgG antibodies to coagulase-negative staphylococci. In the septicemia patients a significant decrease of about 50% was observed in IgG titers between birth and onset of septicemia. However, because no decrease in opsonic activity was observed, the meaning of this decrease in IgG titer is questionable.
To lower the risk of the development of nosocomial septicemia, in which coagulase-negative staphylococci are the most important causative agents, studies with immunoprophylactic therapy with IVIG have been conducted, yielding controversial results(11–14). Clapp et al.(11) demonstrated a significant decrease in the incidence of nosocomial septicemia when the serum IgG levels were maintained near 700 mg/dL. Baker et al.(13) found a reduction after administration of IVIG in a dose of 500 mg/kg. These findings could not be confirmed in a multicenter trial reported by Fanaroff et al.(12), who failed to show a reduction in hospital-acquired infections in very low birth weight infants, when given 700 mg/kg (1001-1500-g birth weight) or 900 mg/kg (501-1000 g) every 14 d. Fischer et al.(17) found a marked variation in IVIG preparations with regard to antibody titers against S. epidermidis(17). They also found a comparable variation in the titer of antibodies to S. epidermidis in human plasma(15). These findings were confirmed in our study. We found a marked variation in IgG titers as well as opsonic activity to coagulase-negative staphylococci in different FFP batches. The administration of FFP in our neonatal ward to all patients with septicemia and circulatory instability, to a total volume of 45 mL/kg on three consecutive days, resulted in a significant increase in IgG titers to coagulase-negative staphylococci. However, the IgG titer also increased in one out of three patients who did not receive FFP. Moreover, no relation was found between the IgG titers of serum after FFP administration and the IgG titers to coagulase-negative staphylococci of the batches FFP used. These data suggest that the increase in IgG in patients was, at least in part, the result of production of antistaphylococcal IgG by the patient. This suggestion is in line with the appearance of specific protein bands in immunoblots of S. epidermidis blood isolates developed with the corresponding neonatal sera (Fig. 3). Indeed, in some patients we observed prior colonization with a similar S. epidermidis strain as the strain causing septicemia as judged from identical random amplification of polymorphic DNA pattern (M. E. Jones, T. G. Krediet, K. Jannssen, C. M. A. Rademaker, A. Fleer, J. Verhoef, manuscript in preparation).
In addition, we observed a complete lack of correlation between increased IgG titers and opsonic activity after FFP administration. In some patients even a marked decrease in opsonic activity to coagulase-negative staphylococci occurred, despite adequate opsonic activity in the corresponding FFP batches and an increase in IgG titer. We can only speculate about the mechanisms of these phenomena. In terms of IgG production by the patient this must mean that the patient IgG lacks opsonic activity. Another explanation is that administered IgG might be subject to structural changes after infusion into the neonate resulting in partial or complete loss of opsonic function, analogous to transplacentally derived IgG, which has been shown to be less opsonically active than maternal IgG(8). For the latter phenomenon both damage of the IgG molecule during transport across the placenta and preferential transport of opsonically less active subclasses of IgG might serve as explanations, as suggested by Cates et al. and by us(8, 9). Support for this hypothesis that functional loss of IgG (partial or complete) in the neonate is based on a similar mechanism, may be derived from recent data indicating that the transplacental Fc receptor and the IgG protection receptor are similar(18, 19). An additional assumption in this case must be that these receptors in the neonate have a greater negative impact on IgG function than in the adult. Alternatively, the IgG protection receptor may be less abundant in the neonate, i.e. more quickly saturated, resulting in increased catabolism and (partial) loss of function of infused IgG molecules. Whatever the mechanism, it suggests a more important role for complement activity in FFP in the opsonization of coagulase-negative staphylococci by premature infants. In the four patients in whom C3 deposition on a coagulase-negative staphylococcal blood isolate was determined, increases after FFP administration were noted in all four. However, as with IgG deposition and opsonic activity, the effect of FFP, particularly the amount of C3 deposited, and the relation to opsonic activity were unpredictable.
In summary, low IgG titers and low opsonic activity to coagulase-negative staphylococci at birth are not predictive for late-onset septicemia due to these bacteria in premature infants. The administration of FFP resulted in a significant increase in IgG titer to coagulase-negative staphylococci in all patients, although there was marked interindividual variation. The opsonic activity to the corresponding blood isolate showed a moderate increase in the majority of patients, but an even more striking finding was that the administration of FFP could also result in a strong decrease in opsonic activity, despite good opsonic activity in the corresponding FFP batches. No correlation was found between opsonic activity and IgG titers to coagulase-negative staphylococci of FFP and patient sera. In addition, the increase in opsonic activity was not related to the increase in IgG titers to coagulase-negative staphylococci. In some cases opsonic activity appeared to be related to the degree of C3 deposition on the coagulase-negative staphylococcal blood isolate, although this association also seemed to be unpredictable.
In conclusion, the results of our study show that the level of IgG titers and opsonic activity to coagulase-negative staphylococci are not predictive for the development of late-onset septicemia due to these bacteria in premature infants. Moreover, no support is found for an important role for FFP in enhancing opsonic defense to coagulase-negative staphylococci in the premature neonate. As a result, we have abandoned the use of FFP for this indication in our unit.
Abbreviations
- FFP:
-
fresh frozen plasma
- IVIG:
-
i.v. immunoglobulin
- PMN:
-
polymorphonuclear neutrophils
- GHBSS:
-
gelatin in Hanks' balanced salt solution
- cfu:
-
colony-forming unit
References
Hall SL 1991 Coagulase-negative staphylococcal infections in neonates. Pediatr Infect Dis J 10: 57–67.
Stoll BJ, Gordon T, Korones SB, Shankaran S, Tyson JE, Bauer CR, Fanaroff AA, Lemons JA, Donovan EF, Oh W, Stevenson DK, Ehrenkranz RA, Papile LA, Verter J, Wright L 1996 Late-onset sepsis in very low birth weight neonates: a report from the national institute of child health and human development neonatal research network. J Pediatr 129: 63–71.
Gaynes RP, Edwards JR, Jarvis WR, Culver DH, Tolson JS, Marlone WJ, National Infectious Surveillance System 1996 Nosocomial infections among neonates in high risk nurseries in the United States. Pediatrics 98: 357–361.
Fleer A, Senders RC, Visser MR, Bijlmer RP, Gerards LJ, Kraaijeveld CA, Verhoef J 1983 Septicemia due to coagulase-negative staphylococci in a neonatal intensive care unit: clinical and bacteriological features and contaminated parenteral fluids as a source of sepsis. Pediatr Infect Dis J 2: 426–431.
Davies AJ, Ward-Platt M, Kirk R, Marshall R, Speidel BD, Reeves DS 1984 Is coagulase-negative staphylococcal bacteraemia in neonates a consequence of mechanical ventilation?. J Hosp Infect 5: 260–269.
Peterson PK, Wilkinson BJ, Kim Y, Schmeling D, Douglas SD, Quie PG, Verhoef J 1978 The key role of peptidoglycan in the opsonization of Staphylococcus aureus. J Clin Invest 61: 597–609.
Verbrugh HA, van Dijk WC, Peters R, van Erne ME, Daha MR, Peterson PK, Verhoef J 1980 Opsonic recognition of staphylococci mediated by cell wall peptidoglycan: antibody-independent activation of human complement and opsonic activity of peptidoglycan antibodies. J Immunol 124: 1167–1173.
Fleer A, Gerards LJ, Aerts P, Westerdaal NAC, Senders RC, van Dijk H, Verhoef J 1985 Opsonic defense to Staphylococcus epidermidis in the premature neonate. J Infect Dis 152: 930–937.
Cates KL, Goetz C, Rosenberg N, Pantschenko A, Rowe JC, Ballow M 1988 Longitudinal development of specific and functional antibody in very low birth weight premature infants. Pediatr Res 23: 14–22.
Lassiter HA, Tanner JE, Cost KM, Steger S, Vogel RL 1991 Diminished IgG, but not complement C3 or C4 or Factor B, precedes nosocomial bacterial sepsis in very low birth weight neonates. Pediatr Infect Dis J 10: 663–668.
Clapp DW, Kliegman RM, Baley JE, Shenker N, Kyllonen K, Fanaroff AA, Berger M 1989 Use of intravenously administered immune globulin to prevent nosocomial sepsis in low birth weight infants: report of a pilot study. J Pediatr 115: 973–978.
Fanaroff AA, Korones SB, Wright LL, Wright EC, Poland RL, Bauer CR, Tyson JE, Philips JB, Edwards W, Lucey JF, Catz CS, Shankaran S, Oh W, for the National Institute of Child Health and Human Development Neonatal Research Network, 1994 A controlled trial of intravenous immune globulin to reduce nosocomial infections in very-low-birth-weight infants. N Engl J Med 330: 1107–1113.
Baker CJ, Melish ME, Hall RT, Casto DT, Vasan U, Givner LB, and the Multicenter Group for the Study Of Immune Globulin in Neonates 1992 Intravenous immune globulin for the prevention of nosocomial infection in low-birth-weight neonates. N Engl J Med 327: 213–218.
Hill HR 1993 Intravenous immunoglobulin use in the neonate: role in prophylaxis and therapy of infection. Pediatr Infect Dis J 12: 549–559.
Cieslak TJ, Wilson SR, Fischer GW 1992 Marked variation in antibody directed against Staphylococcus epidermidis in IVIG and human plasma. Program and Abstracts of the 32nd Interscience Conference on Antimicrobial Agents and Chemotherapy, Anaheim, CA. Abstract 167
Timmerman CP, Fleer A, Besnier JM, De Graaf L, Cremers F, Verhoef J 1991 Characterization of a proteinaceous adhesin of Staphylococcus epidermidis which mediates attachment to polystyrene. Infect Immun 59: 4187–4192.
Fischer GW, Cieslak TJ, Wilson SR, Weisman LE, Hemming VG 1994 Opsonic antibodies to Staphylococcus epidermidis: in vitro and in vivo studies using human intravenous immune globulin. J Infect Dis 169: 324–329.
Simister NE, Story CM 1996 Fcγ receptors in human placenta. In: van de Winkel JGJ, Capel PJA (eds) Human IgG Fc Receptors. Springer Verlag, Heidelberg, PP 25–38.
Junghans RP, Anderson CL 1996 The protection receptor for IgG catabolism is the β2-microglobulin-containing neonatal intestinal transport receptor. Proc Natl Acad Sci USA 93: 5512–5516.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Krediet, T., Beurskens, F., Van Dijk, H. et al. Antibody Responses and Opsonic Activity in Sera of Preterm Neonates with Coagulase-Negative Staphylococcal Septicemia and the Effect of the Administration of Fresh Frozen Plasma. Pediatr Res 43, 645–651 (1998). https://doi.org/10.1203/00006450-199805000-00013
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199805000-00013
This article is cited by
-
Staphylococcus epidermidis biofilms induce lower complement activation in neonates as compared with adults
Pediatric Research (2013)
-
Does IVIg administration yield improved immune function in very premature neonates?
Journal of Perinatology (2010)
-
Prevention and Treatment of Nosocomial Sepsis in the NICU
Journal of Perinatology (2004)
-
Nosocomiale sepsis in de neonatale intensieve zorg
Tijdschrift voor kindergeneeskunde (2000)