Abstract
Suitability of a recently proposed noninvasive L-[13C]leucine breath test for assessment of whole body leucine oxidation in maple syrup urine disease (MSUD) was examined. Oral L-[1-13C]leucine loads (38 μmol/kg body weight) were performed in overnight fasted MSUD patients (n = 6, classical form), obligate heterozygote parents (n = 6), and control subjects (n = 10). Three-hour 13CO2 exhalation kinetics were evaluated using curve fitting procedures. Venous blood was obtained in most cases and analyzed for 13C-labeled plasma metabolites. In control subjects, maximal 13CO2 exhalation was reached at tmax = 55 ± 18 min. Cumulative 13CO2 output at 3 h amounted to 4.7 ± 0.7 μmol × (kg body weight)-1. Estimated total 13CO2 exhalation was 7.2± 1.4 μmol × (kg body weight)-1 (19.0 ± 3.6% of the dose). Half of this amount was expired at t1/2 = 130± 18 min. The data show a considerable degree of intersubject variability. Intraindividual variability was comparable, however, when checked in two volunteers. In obligate heterozygotes, 13CO2 kinetics were similar to controls (tmax = 35 ± 8 min,t1/2 = 95 ± 16 min). Total 13CO2 output[5.7 ± 1.4 μmol × (kg body weight)-1] tended to be in the lower control range. None of the MSUD patients under study exhibited a significant increase in 13CO2 output after load. Maximal increase of label in plasma 4-methyl-2-oxopentanoate, the physiologic precursor of 13CO2, was 16.1 ± 3.5 MPE in control subjects. In MSUD, label dilution was increased and correlated with the patients' leucine/4-methyl-2-oxopentanoate plasma levels. Considering the generally high variability of 13CO2 output and the unstable substrate pools in MSUD, we discuss the limitations of whole body leucine oxidation measurements by noninvasive approaches.
Similar content being viewed by others
Main
In MSUDs (McKusik 248600), activity of the mitochondrial BCOA-DH (EC 1.2.4.4) is impaired. BCAA and BCOA accumulate in blood and other body fluids and can exert neurotoxic effects by yet unclarified mechanisms. The severity of the disease, ranging from severe classical to mild variant types, is commonly classified by more indirect parameters. These are, for example, onset of symptoms, L-leucine tolerance, and residual BCOA-DH activity as measured in vitro in skin fibroblasts or white blood cells of the patients[for a comprehensive review, see Chuang and Shih(1)].
The correlation of the clinical severity of MSUD and the residual BCOA-DH activity as determined in the patients' cells in vitro is not always satisfying(1). Thus, for accurate classification of MSUD patients and for validation of specific therapeutic interventions, for example thiamine treatment(2), a direct assessment of the severity in an affected patient, that is determination of whole body BCOA-DH flux, is desired(1, 3).
Whereas numerous reports are available on BCAA catabolism in healthy subjects, only a few in vivo studies have been performed in MSUD patients. In general, the (primed) continuous infusion approach and isotopically labeled L-leucine as a substrate have been used. In MSUD patients with stated classical form of the disease, about 50% exhibited measurable WBLO, ranging from 8% up to 43% of control values(4–7). These findings appear to be somewhat contradictory to the generally very low or virtually absent leucine oxidation that is usually found in the patients' cells in vitro(1).
To overcome the problems inherent in invasive experimental approaches, a noninvasive breath test has recently been proposed(8). L-[1-13C]Leucine was administered orally and WBLO then deduced from the recovery of 13CO2 in exhaled air. Again, the rates of WBLO in MSUD patients were rather variable and only partially compatible with the residual BCOA-DH activity in the patients' cells.
This led us to reexamine the significance of this approach. Loading tests with L-[1-13C]leucine were performed in patients with the classical form of MSUD, obligate heterozygote parents, and healthy volunteers. The kinetics of 13CO2 exhalation were thoroughly studied and, when available, compared with the kinetics of leucine metabolites in plasma. The main questions to be answered by the present study were: 1) can residual WBLO be detected in classical MSUD by this approach? 2) can heterozygotes be differentiated from controls by 13CO2 exhalation measurements? and 3) can quantitative data on WBLO be derived by the proposed noninvasive procedure?
METHODS
Subjects. The clinical characteristics of the MSUD patients, heterozygote parents, and healthy subjects (controls) under study are compiled in Table 1. The control subjects had a normal physical examination. None of them received medication, had an acute or chronic illness, or a family history thereof. The two subjects undergoing multiple loading tests consumed their normal diet during the course of the study. No significant changes in body weight were noted. Written informed consent was obtained from all subjects before they entered the study. The experimental protocol had been approved by the Ethikkommission of the Heinrich-Heine-Universität Düsseldorf.
Loading tests. After an overnight fast, subjects and patients underwent oral loading tests with L-[1-13C]leucine [99% 1-13C, 38 μmol × (kg body weight)-1]. Three of the MSUD patients (see Fig. 8) and all of the healthy subjects gave consent to the invasive type of study, which was then performed in the pediatric department. The study protocol was exactly as detailed previously(9). That is, control samples of blood and breath were collected before the administration of tracer. After ingestion of tracer, samples were collected at 15-min intervals during a 3-h experimental period. Additionally, spontaneous urine was collected before and at the end of the experiment.
Some MSUD patients and the obligate heterozygotes were not available for examination in the hospital and required noninvasive investigation in their habitual environment. At home, subjects were studied in sitting position. Breath samples were collected as above. Total CO2 production was estimated assuming an endogenous production of 5 mmol × [min × m2 (body surface)]-1(10). Body surface was estimated using the weight-height formula given by Haycock et al.(11).
Analytical procedures. The sources for chemicals, reagents, and13 C-labeled L-leucine were as in Bodner et al.(9). Established procedures were used for measurement of BCAA and BCOA, and CO2 exhalation as well as for mass spectrometric estimation of 13C enrichment in breath CO2, plasma leucine, and KIC as previously described(9).
Calculations. MPE in metabolites was calculated as in Bodner et al.(9). The increase APE in expired CO2 was calculated as the difference of 13CO2 in breath samples withdrawn before (control value) and after the oral loads. Rates of extra 13CO2 exhalation per min were calculated from the APE on the basis of the CO2 exhalation rate. When available, the latter was calculated from the mean CO2 output measured within a 10-min period preceding the withdrawal of air samples for isotope ratio-mass spectrometry analysis. Otherwise, the CO2 exhalation rate was estimated from the body surface as described above. From the exhalation rates at each time point, the cumulative extra 13CO2 exhalation was calculated using trapezoidal methods.
Total 13CO2 exhalation was assessed by curve-fitting procedures. Using sets of 13CO2 exhalation rates of 6-h L-[13C]leucine loading tests as provided by Elsas et al.(8), the present approach was established, and its plausibility was checked as depicted in Figure 1. First, data from the initial 180 min of the loading tests were fitted to nonlinear functions using the Marquardt-Levenberg algorithm for nonlinear regression analysis (as provided by the curve fit procedure of Sigma Plot 2.0 from Jandel Scientific). Among various models tested, the functionEquation (1) where ai and ki are constants and t is the time in minutes, allowed the most satisfying fit of the 13CO2 kinetic data[y(t), in μmol × min-1 × (kg body weight)-1] using q = 4 (Fig. 1,upper). With the data sets tested (n = 7), the coefficients of determination amounted to R2 > 0.9915(mean ± SD, 0.9921 ± 0.0055). Reliability was examined as is shown in Figure 1 (upper). When estimates for the 13CO2 exhalation rate [y(t)] for the time period 3-6 h were computed for each experiment and compared with the experimental data as provided in Elsas et al.(8), a satisfactory agreement was obtained (r> 0.9053; mean, 0.9702 ± 0.0325).
Principle of the evaluation of 13CO2 exhalation in L-[1-13C]leucine breath tests. Experimental13 CO2 exhalation rates (⊙, •) as reported in Elsas et al.(8) for a 6-h study period were used. Upper panel: 13CO2 exhalation rates from the initial 3 h were fitted to Equation 1 using nonlinear regression analysis (dotted line, fit-curve; coefficient of determination,R2 > 0.995; see “Methods”). Reliability was examined by correlation of extrapolated (solid line) and experimental 13CO2 exhalation rates during the the following 3-6 h study period (correlation coefficient r > 0.987). Lower panel: Comparison of cumulative 13CO2 exhalation values as calculated by trapezoidal methods (•) and the computed integral of the above fit-curve (solid line; see Equation 2); correlation of experimental and predicted data, r > 0.999).

The area under the curve of 13CO2 exhalation rate versus time is equivalent to the amount of exhaled13 CO2. Values for 13CO2 output[Y(t)), in μmol × (kg body weight)-1] at time t can thus be estimated using the parameter estimates ai and ki and the integratedEquation 1, that is Equation (2)

Plausibility of this calculation was checked as depicted in Figure 1 (lower). Y(t) estimates of 13CO2 output were computed for the 6-h study periods and compared with the corresponding cumulative values as obtained from the measured 13CO2 exhalation rates by trapezoidal methods. In all data sets, a strong correlation between model-predicted and experimental values was obtained (correlation coefficients of at least r > 0.9999).
Based on these results, total 13CO2 output[Y(t∞); in μmol × (kg body weight)-1] in the present experiments was then assessed by insertion of the parameter estimates ai and ki as obtained by nonlinear fitting of the individual 13CO2 exhalation kinetics into Equation 3 which was derived from formula(Equation 2) by extrapolation to infinite time.

Three additional breath test parameters were defined, the time point of maximal 13CO2 exhalation rate (tmax), and the time points where 5% (t5%) and 50% (t1/2; half-time) of total extra 13CO2 exhalation were reached, respectively. The parameter values (in minutes) were computed by standard numerical methods as provided by the SOLVER procedure of the EXCEL 5.0 program using the parameter estimates, Y(t∞), and the first derivative of the general Equation 1 set equal to zero (for tmax) or the integrated form ofEquation 1 set equal to 0.05 ×Y(t∞) (for t5%) and to Y(t∞)/2 (for t1/2), respectively.
This mathematical approach was also applied for estimation of the maximal13 C enrichment in plasma [13C]KIC on the basis of the measured MPE kinetic data.
Unless otherwise noted, results are presented as means ± SD with the number of determinations in parentheses. Linear regression (least square method) was used for correlation analysis. For examination of differences, the Mann-Whitney U test was used.
RESULTS
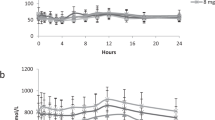
Kinetics of 13CO2 exhalation. For establishment of control values, 10 healthy volunteers were studied. After ingestion of L-[1-13C]leucine (38 μmol/kg of body weight), the rate of extra13 CO2 exhalation increased rapidly (Fig. 2). Peak exhalation rates of 40.9 ± 9.8 nmol × min-1 ×(kg body weight)-1 were reached at tmax = 55 ± 18 min (Fig. 2). Thereafter, 13CO2 release gradually decreased.
Kinetics of 13CO2 exhalation(upper) and cumulative 13CO2 output (lower) after oral loading of healthy subjects with L-[1-13C]leucine. The dose applied was 38 μmol × (kg body weight)-1. Results are means± SD (n = 10). The cumulative 95.5% prediction interval(equivalent to ± 2 SD) is indicated by the dotted lines.
When total 13CO2 output was assessed from the13 CO2 kinetics using curve fitting procedures, satisfying fits were obtained (coefficients of determination: R2 = 0.986± 0.016). Furthermore, a good correlation was found between experimental results obtained during the 3-h study period and the cumulative13 CO2 exhalation as estimated from the fit data (all data:y = 1.004 (±0.004)x + 0.065 (±0.011),sy,x = 0.07, n = 120, r > 0.9991; each individual experiment: r > 0.9998, n = 12). A compilation of cumulatives is presented in Table 2. Estimates of total 13CO2 expiration amounted to 7.2 ± 1.4μmol × (kg body weight)-1, equivalent to about 20% of the administered L-[1-13C]leucine dose. Of this amount, 5 and 50% were recovered in exhaled air within t5% = 33 ± 6 min and t1/2 = 130 ± 18 min after load, respectively.
There was a considerable interindividual variability of 13CO2 exhalation. To examine the significance of intraindividual variability, two volunteers underwent multiple loading tests. The data on cumulative13 CO2 exhalation shown in Figure 3 indicate that, somewhat unexpectedly, the intraindividual variability was similar to or even greater than the interindividual variation.
Intraindividual reproducibility of extra13 CO2 exhalation in healthy subjects after oral loading with L-[1-13C]leucine. Two volunteers underwent multiple loading tests(upper: P.S., n = 5; lower: M.H., n = 4) with 38 μmol of labeled L-leucine per kg of body weight. Results are presented as means ± 2 SD of the cumulative 13CO2 excretions. For comparison, the control range (mean ± 2 SD limits) has been indicated by dotted lines.
In subjects P.S. (n = 5) and M.H. (n = 4), peak13 CO2 exhalation rates were reached at tmax = 45 ± 15 min and 93 ± 26 min and amounted to 38.3 ± 16.0 and 32.1 ± 7.0 nmol × min-1 × (kg body weight)-1, respectively. Cumulative 13CO2 release within 3 h was 4.4 ± 1.0 and 3.8 ± 0.7 μmol × (kg body weight)-1, respectively. Estimates of total 13CO2 output amounted to 6.4 ± 0.9 and to 5.9 ± 1.0 μmol × (kg body weight)-1, respectively, equivalent to 16.8 ± 2.5 and to 15.4± 2.7 percent of the L-[1-13C]leucine dose applied, respectively. Of these amounts, 5% was recovered within t5% = 27 ± 6 min and 48 ± 10 min and 50% within t1/2= 122 ± 14 min and 140 ± 10 min, respectively.
In obligate heterozygous parents (n = 6) of patients with classical MSUD, the kinetics of 13CO2 exhalation were similar to controls (Fig. 4). Maximal 13CO2 release was 42 ± 12 nmol × min-1 × (kg body weight)-1 at tmax = 35 ± 8 min. The data presented in Table 2 indicate that cumulative 13CO2 exhalation tended to be in the lower normal range. However, no statistically significant differences between controls and heterozygotes were noted. Of the estimated total 13CO2 release, 5 and 50% [5.7 ± 1.4μmol × (kg body weight)-1] was recovered within t5% = 19 ± 3 min and t1/2 = 95± 16 min, respectively.
Kinetics of 13CO2 exhalation(upper) and cumulative 13CO2 output (lower) in patients with MSUD (classical form, n = 6) and obligate heterozygous parents (n = 6) after oral loading with L-[1-13C]leucine. The dose applied was 38 μmol × (kg body weight)-1. In the patients, no significant increase of13 CO2 exhalation was found. Results for the heterozygotes are means ± SD. For comparison, the range for cumulative13 CO2 release in controls (mean ± 2 SD limits;dotted lines) has been included.
In the six patients under study, all of which had the classical form of MSUD, we were unable to observe any significant increase of13 CO2 exhalation after oral loading with L-[1-13C]leucine (Fig. 4). Noteworthy, in the loading test of patient L.U. presenting with normal plasma leucine concentrations, a low and delayed increase in 13CO2 release amounting to 0.04 μmol × (kg body weight)-1 within 3 h, equivalent to about 1% of the control values, was observed. However, when the test was repeated a few days later using sham loading conditions (citric acid solution only), we similarly found a cumulative 13CO2 output of 0.08 μmol × (kg body weight)-1, equivalent to about 2% of the control values. Thus, the increase in 13CO2 exhalation in patient L.U. was presumably not due to the administration of L-[1-13C]leucine but rather referable to the increased oxidation of naturally enriched endogenous substrate under fasting conditions.
Kinetics of plasma metabolites. The time course of the plasma concentrations of leucine and the corresponding 2-oxo acid in control subjects(n = 10) is shown in Figure 5. Before load, plasma concentrations of leucine and KIC were 129 ± 23 and 44 ± 8 μmol × L-1. Within about 45 min after load, plasma levels maximally increased by 42 ± 13% (+51 ± 10 μmol × L-1) and 25 ± 12% (+10 ± 3 μmol × L-1), respectively, and were still slightly elevated at the end of the 3-h study period.
13C-Label enrichment was examined in KIC, the metabolic precursor of the label in expired 13CO2. As depicted in Figure 6, the time course of label enrichment (MPE) largely paralleled the plasma concentration curve. Mean peak values of 16.1± 3.5 MPE were reached at tmax = 36 ± 12 min after load, 19 ± 11 min (range 8-43 min) before the appearance of the respective 13CO2 peaks in exhaled air (p < 0.001).
As with the 13CO2 exhalation, the intraindividual variability of label enrichment in plasma KIC as measured in subjects P.S. and M.H.(Fig. 7) was similar to or even greater than the interindividual variability. In M.H., the increase of plasma [13C]KIC was somewhat delayed and attenuated, compatible with the delayed time course of 13CO2 expiration observed in this subject (Fig. 3).
Intraindividual variability of the time course of13 C-label enrichment (MPE) in plasma KIC after oral L-[1-13C]leucine loads. Means ± 2 SD of two healthy volunteers(M.H., n = 4; P.S., n = 5) undergoing multiple loading tests with 38 μmol of leucine per kg of body weight are shown. For comparison, the control range (mean ± 2 SD limits) has been indicated by dotted lines.
Interestingly, in control subjects, no statistically significant correlation was found between the plasma leucine concentration or the peak label enrichment in the 2-oxo acid precursor and the inter- or intraindividual data on or peak or total 13CO2 output.
In Figure 8, the leucine plasma concentrations together with the 13C-label enrichment in KIC as obtained after L-[1-13C]leucine loading in three MSUD patients is shown. The L-leucine load induced peak increases in plasma leucine and KIC were similar to controls and amounted to +54 ± 19 and +26 ± 12 μmol × L-1, respectively.
The subsequent decrease of plasma leucine, however, appeared to be influenced by the initial plasma concentrations. In patient L.U., presenting with normal concentrations and without any measurable extra13 CO2 output after load, plasma leucine levels decreased to nearly initial values within 3 h. In the two other patients with the classical form of MSUD, plasma leucine was clearly elevated before load, and the plasma concentration remained constant (patient D.G.) or tended to increase further(patient J.F.) during the study period.
It should be noted in this context that renal clearance of leucine carbon skeletons was very low in controls as well as in MSUD patients and could, therefore, not contribute to the observed changes in leucine plasma levels(data not shown).
As evidenced by data on the 13C-isotope enrichment in KIC (MPE),in vivo dilution of the administered 13C-label appeared to be positively correlated with the leucine plasma levels. In patients L.U., J.F., and D.G., peak MPE amounted to 16.4, 6.9, and 6.1, respectively, at initial leucine plasma concentrations of 136, 430, and 450 μmol × L-1, respectively.
DISCUSSION
The duration of the present experiments was 3 h compared with the 6-h period used by Elsas et al.(8). When planning the study, we experienced a poor compliance of the subjects with considerably prolonged experimental periods. Furthermore, it would have been difficult, if not impossible, to actually maintain constant experimental conditions for 6 h, especially in children and subjects undergoing invasive measurements. In addition, in the moderate catabolic state after an overnight fast, a shorter experimental period reduced the risk of an additional accumulation of BCAA and BCOA in the MSUD patients.
In fact, a distinct time course of the parameters under investigation was observed, indicating that a 3-h study period was adequate for characterization of the kinetics of 13C incorporation into plasma metabolites and breath CO2. For evaluation of 13CO2 expiration, a mathematical analysis was established using curve-fitting procedures. According to our estimates, the cumulative 13CO2 release in controls within 6 h after load amounted to about 17% of the loading dose equivalent to >90% of total extra 13CO2 exhalation. These data are comparable to the values obtained in the 6-h study(8). Furthermore, our estimates suggest that a total of about 20% of the administered L-[1-13C]leucine load was diverted into catabolic pathways. This is compatible with results from primed continuous infusion studies, where it was consistently found that about 20% of total whole body leucine flux in the postabsorptive state is due to oxidative leucine disposal(12–22).
Patients with clinically well defined classical MSUD were examined to clarify, whether specific, L-[1-13C]leucine loading-dependent increase in 13CO2 release could be detected in these severely affected subjects. So far, the findings on in vivo leucine oxidation (WBLO) in MSUD patients with the stated classical form of the disease are at some variance. Using the (primed) continuous infusion approach, Collins et al.(4) found appreciable WBLO (22-43% of control values) in all of the three patients studied. Thompson et al. reported on measurable oxidation rates in one (16% of control) out of four(5), in three (8-24% of control) out of seven(6), and in one (5% of control) of two patients(7). Elsas et al.(8) reported on variable WBLO in classical MSUD as assessed by the noninvasive L-[1-13C]leucine breath test. As discussed in Bodner et al.(9), no reliable explanation can be offered with respect to the causes for these divergent findings. In any case, however, we were unable to detect a significant increase in 13CO2 output in any of the six patients studied.
Thus, the question arises on the sensitivity of the experimental approaches. The rationale for our sensitivity estimates is as follows. The main factor limiting the detection of residual leucine oxidation in MSUD is determination of extra 13CO2 exhalation. Reportedly, the natural intraindividual variability of basal breath 13CO2 is about±0.7δ value(23). Thus, the lower limit for reliable measurement of extra 13CO2 output is an increase of at least 1δ value over baseline in expired air. Assuming a CO2 production at rest of about 120 μmol × min-1 × (kg body weight)-1 in adults, the required endogenous extra 13CO2 production is about 1.5 nmol × min-1 × (kg body weight)-1(23, 24). WBLO can be estimated from the extra 13CO2 release and 13C-label enrichment in plasma KIC as WBLO = 13CO2 release/[13C]KIC(25). Compiled data from the literature suggest that the mean WBLO in overnight fasted healthy subjects (WBLOcontrol) amounts to 340 ± 93 nmol × min-1 × (kg body weight)-1(n = 55)(12–22)[references cited in Bodner et al.(9)]. Using these data, the sensitivity (S, in percent of WBLOcontrol) can be calculated approximately as Equation

This analytical sensitivity can be achieved when the label enrichment in CO2 and KIC is fairly stable for a period of time long enough to allow multiple samples to be withdrawn for analysis, that is essentially under steady state conditions. Therefore, the sensitivity may be lower in bolus tests where the 13C-label enrichment in metabolites changes more or less rapidly. In infants and children, sensitivity of the test is further decreased because the CO2 output per unit body weight may be considerably higher than in adults(26).
In the MSUD patients L.U., J.F., and D.G., the (maximal) label enrichment in plasma KIC was 16.1, 6.9, and 6.1 MPE, respectively. Therefore, the utmost lower analytical limit of detection of residual WBLO was about 5, 10, and 10% of control values, respectively.
Interestingly, the labeling pattern in our MSUD patients suggests that dilution of the applied L-[1-13C]leucine tracer is rather closely correlated to the leucine plasma levels. The plasma concentrations of KIC appeared to have minor influence. This would be consistent with the fact that extracellular (plasma) leucine levels are only moderately lower than the intracellular levels(27). The concentration of the derived 2-oxo acid is likely to be considerably higher in plasma, however, than in the cytosol(28). Therefore, plasma leucine possibly far better reflects the total body pool than does plasma KIC or the sum of both metabolites.
Thus, in the MSUD patients exhibiting leucine concentrations of about 1 mmol × L-1 (Table 1), the load induced peak increase of label in KIC can be expected to reach ≤3 MPE, and the sensitivity for detection of WBLO would thus be reduced to about 15% of control values. This is possibly far too low to allow detection of residual WBLO in classical MSUD, which is generally expected to be well below 5% of control(1).
These considerations indicate that the sensitivity of WBLO measurements, irrespective of whether steady state (primed continuous infusion) or compartmental (bolus tests) approaches are applied, is severely influenced by the amount of labeled substrate applied and the plasma metabolite concentration, and may also be dependent on the sampling protocol. Additionally, as evidenced by the findings in the sham load in patient L.U., care must be taken not to refer low increases in 13CO2 exhalation to oxidation of administered L-[1-13C]leucine unless interferences from increased release of label from naturally enriched endogenous sources are firmly excluded.
On the basis of the present results we do not imply that WBLO in all of our MSUD patients was virtually absent. We rather provide an experimental estimate of the upper limit of the individual residual WBLO. Once measurable residual WBLO in a MSUD patients have been established, it appears imperative, however, to check the repeatability of WBLO determination before applying this approach for assessment of therapeutic interventions such as thiamine treatment.
We also performed noninvasive L-[1-13C]leucine breath tests in a number of the patients' parents. The rationale was that, in parents of patients with classical MSUD, any impairment of leucine oxidation due to heterozygosity would be most easily detected. However, neither the13 CO2 kinetics nor total extra 13CO2 exhalation was found to be significantly different from healthy control subjects. In heterozygotes, the load-induced increase in 13CO2 expiration appeared to be somewhat accelerated. For reasons to be discussed below, it is unlikely, however, that minor impairments in L-[1-13C]leucine oxidation exerted significant effects on the time course of the label appearance in expired air. More probably, the slight acceleration observed in the present experiments was attributable to a somewhat enhanced gastrointestinal transit of labeled substrate and/or CO2 turnover due to the fact that the heterozygotes had to be examined noninvasively at home and in sitting position, whereas control subjects were studied invasively in the metabolic research unit and had to be kept in the supine position for indirect calorimetry measurements.
It has been stated that MSUD patients as well as heterozygous parents may be differentiated from controls by a delay in the onset of 13CO2 exhalation(8). In the present study, however, the most significant delay was observed in a healthy volunteer (subject M.H.), whereas none of the heterozygotes exhibited a suspiciously delayed 13CO2 kinetic.
To define the factors introducing delays in 13CO2 output, model calculations were performed in our laboratory using physiologically meaningful variations of parameters (P. Schadewaldt and A. Bodner, unpublished results). Our calculations showed that the main factors determining the shape of the exhalation curve are the rates of 1) total CO2 exhalation; 2) gastrointestinal transit, resorption, and transamination; 3) protein synthesis; and 4) the magnitude of the CO2 pools involved. The influence of changes in the rate of WBLO is comparatively low. Specifically, a delay in 13CO2 expiration may be caused by a decrease in CO2 exhalation, gastrointestinal transit, resorption and transamination of tracer, and, to a minor extent, a decrease in protein synthesis or increase in the CO2 pools.
In contrast, the main factors determining the amount of expired13 CO2 are the 1) rate of WBLO, 2) extension of the leucine pools, and, to a minor extent, 3) rate of protein synthesis. Thus, an attenuation of the (maximal) rate of 13CO2 output is primarily caused by a decrease in WBLO and/or an increase of leucine pools. In vivo, these effects may be at least partially counteracted by the increased availability of substrate to the BCOA-DH and/or by an enhancement of the activity state of the enzyme complex(1).
It seems reasonable to assume that, with the exception of presence of mutant gene(s) and eventually higher BCAA plasma levels (in patients), the main factors which might induce a delay in 13CO2 expiration were in the normal range in the MSUD patients as well as in their heterozygous parents. Therefore, any distinct impairment in WBLO would have been indicated by an attenuation in 13CO2 output. In heterozygotes, however, this was neither observed in our study nor by Elsas et al.(8). Thus, heterozygotes for MSUD appear to have normal WBLO, although possibly in the lower control range. Taken together, the above considerations strongly suggest that a delayed expiration of extra13 CO2 after L-[1-13C]leucine loading may not be taken as a specific indicator of MSUD or heterozygosity.
In the present study, a considerable interindividual variability was found in controls with all the parameters tested, except total CO2 output. Interestingly, in the primed continuous infusion studies cited above, a similar degree of interindividual variability was consistently observed. The high variability is not totally unexpected because leucine flux in vivo appears to be highly regulated and subject to numerous influences, for example diet(18, 19, 22), hormones(15, 16, 20–22), and physical activity(16, 17). Somewhat unexpected was the finding that the intraindividual variability as examined in two subjects was similar to or even greater than the interindividual variation. In subjects M.H., the delayed appearance of 13C-label in plasma and expired air was most probably referable to a considerable delay in the gastrointestinal transit time. Delay in absorption is unlikely as a cause, because the intestinal capacity for BCAA uptake is very high(29). Presumably due to the numerous factors modulating leucine metabolism, no further specific factors could be identified, however, which might be responsible for the inter- and intraindividual variability in the subjects under study.
The present finding of a relatively high intrasubject variability of leucine metabolism is probably not restricted to controls but might also occur in heterozygotes and even in MSUD patients. Therefore, it may be sometimes necessary to exclude that an effect on in vivo leucine flux, for example of thiamine treatment, once observed in a subject or patient was not actually caused by the normal intraindividual variation.
In conclusion, evidence has been presented that noninvasive oral L-[1-13C]leucine breath tests yield only limited information on WBLO, especially in MSUD patients where an expansion of the body's L-leucine pools may unpredictably dilute the 13C tracer and reduce the sensitivity of the test. Withdrawal of blood samples for determination of label enrichment in KIC appears to be inevitable. We have now started a compartmental analysis of L-[13C]leucine loading tests(30). The preliminary results indicate that, when performed invasively, the (compartmental) bolus approach may finally prove to be as useful as the steady state (primed continuous infusion) approach for classification of residual WBLO in variant and, possibly, classical forms of MSUD.
Abbreviations
- APE:
-
atom percent 13C-label enrichment
- BCAA:
-
branched chain L-amino acids
- BCOA:
-
branched chain 2-oxo acids
- BCOA-DH:
-
branched-chain 2-oxo acid dehydrogenase complex
- KIC:
-
4-methyl-2-oxopentanoate
- MPE:
-
mole percent13 C-label enrichment
- MSUD:
-
maple syrup urine disease
- WBLO:
-
whole body leucine oxidation
References
Chuang DT, Shih VE 1995 Disorders of branched chain amino acid and keto acid metabolism. In: Scriver CR, Beaudet AL, Sly WS, Valle D(eds) The Metabolic and Molecular Bases of Inherited Disease. McGraw Hill, New York, pp 1239–1277.
Elsas LJ, Danner DJ 1982 The role of thiamin in maple syrup urine disease. Ann NY Acad Sci 378: 404–421.
Schadewaldt P, Wendel U 1997 Metabolism of branched-chain amino acids in maple syrup urine disease. Eur J Pediatr 156( suppl 1): S62–S66.
Collins JE, Umpleby AM, Boroujerdi MA, Leonard JV, Sonksen PH 1987 Effect of insulin on leucine kinetics in maple syrup urine disease. Pediatr Res 21: 10–13.
Thompson GN, Bresson JL, Pacy PJ, Bonnefont JP, Walter JH, Leonard JV, Saudubray JM, Halliday D 1990 Protein and leucine metabolism in maple syrup urine disease. Am J Physiol 258:E654–E660.
Thompson GN, Francis DEM, Halliday D 1991 Acute illness in maple syrup urine disease: dynamics of protein metabolism and implications for management. J Pediatr 119: 35–41.
Thompson GN, Walter JH, Leonard JV, Halliday D 1990 In vivo enzyme activity in inborn errors of metabolism. Metabolism 39: 799–807.
Elsas LJ, Ellerine NP, Klein PD 1993 Practical methods to estimate whole body leucine oxidation in maple syrup urine disease. Pediatr Res 33: 445–451.
Bodner A, Hammen H-W, Renn W, Wendel U, Schadewaldt P 1997 Whole body branched-chain L-amino acid oxidation in overnight fasted human subjects. Isotopes Environ Health Stud 33: 189–196.
Shreeve WW, Cerasi E, Luft R 1970 Metabolism of[2-14C]pyruvate in normal, acromegalic, and HGH treated human subjects. Acta Endocrinol 65: 155–169.
Haycock G, Schwartz G, Wisotsky D 1978 Geometric method for measuring body surface area: a height-weight formula validated in infants, children and adults. J Pediatr 93: 62–66.
Brillon DJ, Zheng B, Campbell RG, Matthews DE 1995 Effect of cortisol on energy expenditure and amino acid metabolism in humans. Am J Physiol 268:E501–E513.
Cayol M, Tauveron I, Frambourdin F, Prugnaud J, Gachon P, Thielbot P, Grizard J, Obled C 1995 Whole-body protein turnover and hepatic protein synthesis are increased by vaccination in man. Clin Sci 89: 389–396.
Mc Cullough AJ, Mullen KD, Tavill AS, Kalhan SC 1996 In vivo differences between the turnover rates of leucine and leucine's ketoacid in stable cirrhosis. Gastroenterology 103: 571–578.
Copeland KC, Nair KS 1994 Acute growth hormone effects on amino acid and lipid metabolism. J Clin Endocrinol Metab 78: 1040–1047.
Lamont LS, McCullough AJ, Kalhan SC 1995 β-adrenergic blockade heightens the exercise-induced increase in leucine oxidation. Am J Physiol 268:E910–E916.
Welle S, Thornton C, Statt M 1995 Myofibrillar protein synthesis in young and old human subjects after three months of resistance training. Am J Physiol 268:E422–E427.
Macallan DC, McNurlan MA, Milne E, Calder AG, Garlick PJ 1995 Whole-body protein turnover from leucine kinetics and the response to nutrition in human immunodeficiency virus infection. Am J Clin Nutr 61: 818–826.
Carbonel F, Messing B, Darmaun D, Rimbert A, Rgnier M, Rigal O, Koziet J, Thuillier F, Desjeu JF 1995 Energy and protein metabolism in malnutrition due to neoplastic gastrointestinal diseases. Metabolism 44: 1110–1115.
Petrides AS, Luzi L, DeFronzo RA 1994 Time-dependent regulation by insulin of leucine metabolism in young healthy adults. Am J Physiol 267:E361–E368.
Giordano M, Castellino P, Carroll CA, DeFronzo RA 1995 Comparison of the effects of human recombinant insulin-like growth factor I and insulin on plasma amino acid concentrations and leucine kinetics in humans. Diabetologia 38: 732–738.
Welle S, Statt M, Barnard R, Amatruda J 1994 Differential effect of insulin on whole-body proteolysis and glucose metabolism of normal-weight, obese, and reduced-obese women. Metabolism 43: 441–445.
Schoeller DA, Schneider JF, Salomons NW, Watkins JB, Klein PD 1977 Clinical diagnosis with the stable isotope 13C in CO2 breath tests: methodology and fundamental considerations. J Lab Clin Med 90: 412–421.
Saccomani MP, Bonadonna RC, Caveggion E, DeFronzo RA, Cobelli C 1995 Bicarbonate kinetics in humans: identification and validation of a three-compartment model. Am J Physiol 269:E183–E192.
Schwenk W, Beaufrère B, Haymond MW 1985 Use of reciprocal pool specific activity to model leucine metabolism in humans. Am J Physiol 249:E646–E650.
Elia M 1992 Energy expenditure in the whole body. In: Kinney YM, Tucker HN (eds) Energy Metabolism: Tissue Determinants and Cellular Corollaries. Raven Press, New York, pp 19–59.
Bergstöm J, Fürst P, Norée L-O, Vinnars E 1974 Intracellular free amino acid concentration in human muscle tissue. J Appl Physiol 36: 693–697.
Matsuo Y, Yagi M, Walser M 1993 Arteriovenous differences and tissue concentrations of branched-chain ketoacids. J Lab Clin Med 121: 779–784.
Schadewaldt P, Hammen H-W, Dalle-Feste C, Wendel U 1990 On the mechanism of L-alloisoleucine formation: studies on a healthy subject and in fibroblasts from normals and patients with maple syrup urine disease. J Inher Metab Dis 13: 137–150.
Cobelli C, Saccomani MP, Tessari P, Biolo G, Luzi L, Matthews DE 1991 Compartmental model of leucine kinetics in humans. Am J Physiol 261:E539–E550.
Schadewaldt P, Beck K, Wendel U 1989 Analysis of maple syrup urine disease in cell culture: use of substrates. Clin Chim Acta 184: 47–56.
Acknowledgements
We thank all the subjects who participated in the study and Dr. U. Matthiesen (Düsseldorf) for performing GC-MS analyses. We are indebted to Dr. D. Leupold (Ulm) and to Dr. E. Mönch(Berlin) for allowing us to investigate their MSUD patients.
Author information
Authors and Affiliations
Additional information
Supported in part by Grants We 614/9-1 and 614/9-2 from the Deutsche Forschungs-gemeinschaft.
Some preliminary results have been presented at the 1994 Annual Meeting of the Arbeitsgemeinschaft Stabile Isotope, Kiel, Germany. This communication contains parts of the doctoral thesis of A.B.
Rights and permissions
About this article
Cite this article
Schadewaldt, P., Bodner, A., Brösicke, H. et al. Assessment of Whole Body L-Leucine Oxidation by Noninvasive L-[1-13C]Leucine Breath Tests: A Reappraisal in Patients with Maple Syrup Urine Disease, Obligate Heterozygotes, and Healthy Subjects. Pediatr Res 43, 592–600 (1998). https://doi.org/10.1203/00006450-199805000-00006
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199805000-00006
This article is cited by
-
Laboratory approach to mitochondrial diseases
Journal of Physiology and Biochemistry (2001)