Abstract
In utero hypoxia may affect the development of the brain and result in altered respiratory responses postnatally. Using a barometric plethysmograph, we examined the effects of exposing pregnant guinea pigs to 200 ppm carbon monoxide (CO) for 10 h/d from d 23-25 of gestation until term(≈68 d) on the ventilatory responses of their 4-5-d-old neonates at rest, and during progressive asphyxia and steady state hypercapnia. Exposure to this concentration of CO produced significantly higher levels of carboxyhemoglobin(COHb) in maternal (8.53 ± 0.6% versus 0.25 ± 0.1%) and fetal blood (13.0 ± 0.4% versus 1.6 ± 0.1%) from CO-treated animals when compared with controls. Hematocrit was significantly higher in the CO-treated neonates (46.3 ± 1.0% versus 41.3± 0.9%) at 5-6 d of age, although no difference existed between the groups for COHb at this time. There was no difference between the groups for length of gestation, litter size, or birth weight, but CO-treated neonates were significantly smaller at 4 d of age (102.4 ± 3.7 g) compared with controls (132.0 ± 5.0 g). At 4-5 d of age there was no difference between the groups for either tidal volume (VT), respiratory frequency (f), or minute ventilation (VE) at rest, but during steady state hypercapnia (4 and 6% CO2) the CO-treated neonates had a significantly greater VT and VE (but not f) than did controls. During progressive asphyxia, CO-treated animals had a significantly greater VT than did controls from 1-8% CO2. There was a significant fall in f at 1 and 3% CO2 in CO-treated animals; however, this effect did not persist, resulting in a significantly increased VE from 3 to 8% CO2. The inspiratory flow rate(VT/expiratory time) was significantly increased in the CO-treated neonates during progressive asphyxia; this occurred in the absence of a difference in inspiratory time between the groups. These results indicate that prenatal exposure to CO increases CO2 sensitivity in 4-5-d-old guinea pigs. This may be due to developmental alterations in the areas of the brainstem responsible for respiratory control.
Similar content being viewed by others
Main
Smoking by pregnant women is associated with a significantly increased risk of sudden infant death syndrome(1). Furthermore, cigarette smoking by pregnant women has been characterized as a highly significant preventable cause of pregnancy loss and perinatal mortality and morbidity(2), and is now the single most preventable risk factor for sudden infant death syndrome today(1).
Of the several thousand chemicals contained in cigarette smoke, it is generally accepted that nicotine, carbon monoxide (CO), and hydrogen cyanide are the agents primarily responsible for the adverse effects of smoking during pregnancy(3). CO readily crosses the placenta and binds to fetal Hb, thus causing fetal hypoxia. In the fetus, where blood and tissue O2 partial pressures are low and probably close to the critical levels for anoxic damage, any interference with the blood O2 tension or O2 carrying capacity, such as that caused by increasing COHb formation, may result in profound tissue hypoxia(4). Furthermore, under steady state conditions, fetal COHb concentrations exceed that of the mother, and therefore the oxygenation of fetal tissues is more severely effected than maternal tissues by the inhalation of CO(5). Some fetal responses may serve to ameliorate the effects of CO-induced hypoxia. Hypoxia-induced redistribution of blood flow from “nonessential” tissues such as skeletal muscle and the gut, in favor of the brain, may help protect the brain(6).
Several studies have demonstrated neurologic and behavioral deficits after prenatal exposure to CO. Exposing pregnant rats to 100 ppm CO resulted in significant increases in the concentration of 5-hydroxytryptamine and noradrenaline in the brainstem and cortex of the newborn(7). Rats exposed prenatally to high levels of CO (1200 ppm) for short periods showed delayed development in several standard neurologic tests(8). Thus, if chronic exposure to CO causes alterations in the development of brainstem pathways controlling breathing, CO exposure may result in persisting changes in the level of responsiveness when the infant is faced with a cardiorespiratory challenge, such as asphyxia. Progressive asphyxia is a physiologically common stimulus that involves stimulation of both CO2 and O2 receptors, and nonsteady state concentrations of CO2 between blood, extracellular fluid, and cerebrospinal fluid(9). It occurs commonly in infants where ventilation may be compromised by airway obstruction or hypoventilation of central origin. Steady state hypercapnia, although an unnatural stimulus, is regarded as a good indicator of the sensitivity of the central chemoreceptors(10), and is thus a useful indicator of modification to cardiorespiratory centers in the brainstem.
The effects of chronic prenatal exposure to CO on the ventilatory control of the newborn has not been studied in detail. As sudden infant death syndrome has been widely attributed as a derangement of cardiorespiratory control(11), we though it pertinent to investigate the effect of exposing pregnant guinea pigs to 200 ppm CO from d 23-25 of gestation until term (≈68 d) on the response of the newborn to a progressive asphyxic and steady state hypercapnic challenge.
METHODS
Animals. Twenty-one pregnant guinea pigs were used in this study. At d 23-25 of gestation they were assigned to either the control(n = 9) or CO-treatment (n = 12) group. Eleven animals(five control, six CO-treated) were allowed to give birth. All of the mothers and offspring were then removed from the control and CO chambers and placed in normal cages where they breathed room air. The ventilatory responses of the neonates were then studied at 4-5 d of age. The remaining 10 animals (four control, six CO-treated) were used to determine COHb levels in maternal, fetal, and neonatal blood at 5-6 d of age.
CO treatment. CO exposure occurred in a chamber consisting of a large plastic box (100 cm × 50 cm × 50 cm) sealed with a Perspex lid. Built into the Perspex lid were two hand ports which could be opened for feeding and animal retrieval. Within the chamber food and water were provided ad libitum. The flow of 100% CO (BOC, Australia) was controlled via a two-stage gas regulator (CIG, Australia) and a fine needle valve (Nupro, Australia), and was mixed with air (10 L/min) in a manifold before entering the chamber. The level of CO within the chamber was continuously monitored using a CO monitor (Air Met-Monotox, Australia) and recorded on a dot recorder(Sekonic, Australia). All gas exited the chamber via an externally vented passive extraction system. The timing of CO exposure (1000-2000 h) was automated by inserted a two-way normally closed solenoid valve (Asco, model SOD2020, Australia) between the two-stage regulator and fine needle valve, which was then controlled by a 24-h timer (Kambrook, Australia). As the safety of the animals was dependent on the supply of air, the solenoid valve was also controlled by a relay connected to a pressure comparator, which in turn received an input from a liquid-filled pressure transducer connected to the air line. This ensured that, if there was a fall in pressure in the air line, the solenoid valve would be closed, thus preventing the entry of undiluted CO into the chamber.
All control animals were placed in a separate chamber with the same dimensions as the CO chamber, but were exposed to air only. All pregnant guinea pigs remained in these chambers until the litters were born, at which time they were removed to normal metabolic cages where they breathed air.
Measurement of COHb. To determine the level of COHb in the fetuses, mothers, and neonates in the CO and control chambers, 10 pregnant guinea pigs were assigned to either the control (n = 4) or CO(n = 6) chambers at 23-25 d of gestation. At 64 d gestation (term = 68 d), two animals from each group were removed and anesthetized with an intramuscular injection of 0.4 mL of a 3:2 mixture of ketamine (100 mg/mL):xylazine (20 mg/mL), and a 1-mL intramuscular injection of pentobarbitone sodium (60 mg/mL). Once anesthetized, the abdominal wall of the mother was opened, and the fetuses were removed one at a time. Each fetus was given a 1-mL intraperitoneal injection of pentobarbitone sodium (60 mg/mL), and blood (1-2 mL) was collected by cardiac puncture. The animals from the CO-treated group were placed in a small container flushed with 200 ppm CO for the time between the removal of each fetus. When all the fetuses had been removed, maternal blood was collected by cardiac puncture, and she was then killed by a 2-mL intracardiac injection of pentobarbitone sodium (300 mg/mL).
The remaining animals in the CO (n = 4) and control (n= 2) groups were allowed to deliver and were then removed from the chambers to normal cages where they breathed air. At 5-6 d postpartum, before the collection of the brains from these neonates for immunohistochemical analysis as part of a companion study(12), blood was collected from both the mothers and neonates by cardiac puncture after onset of anesthesia produced by pentobarbitone sodium injected intraperitoneally (60 mg/mL).
An aliquot (200 μL) of each blood sample was deoxygenated using a blood deoxygenation kit (D684-10-80, Radiometer, Copenhagen) within 5 min of collection. COHb and Hb were measured using an OSM2 Hemoximeter (Radiometer, Copenhagen). Before measurement of COHb, the Hemoximeter was calibrated using adult guinea pig blood. A sample of blood was also drawn into microhematocrit tubes and spun at 2500 rpm for 5 min for the determination of Hct.
Ventilatory measurements. Ventilation was measured using a barometric plethysmograph, which consisted of two cylindrical Perspex chambers; one contained the animal and the other acted as a pressure reference chamber(13). The animal chamber was constructed so that one end wall could be moved like a piston so that, during the progressive asphyxia tests, the volume of the chamber could be adjusted to the size of the animal (600 mL/100 g of body weight). This was done to standardize the length of time taken for each animal to become progressively asphyxic.
Relative humidity and chamber temperature were measured using the probe of a humidity and temperature meter (model HM34, Vaisala, Finland). The pressure change caused by the tidal movement of gas within the chamber was measured by a volumetric pressure transducer (model PT5A; Grass, Quincy, MA). This signal was amplified (model 79C; Grass), and recorded using a MacLab analog-digital converter (model 8E, AD Instruments, Australia) and Power Macintosh computer(61006). Rectal temperature was measured at the beginning and end of the experiment. The O2 and CO2 contents of the gas in the chamber were measured continuously by drawing gas (2 L/min) through polarographic(model 0A277, Taylor Servomex, England) and infra-red (Normocap CO2 Monitor, Datex, Finland) monitors, and then returning the gas to the chamber.
At 4-5 d of age, each newborn guinea pig was placed in the plethysmograph and exposed to room air for at least 20 min. The chamber was then sealed, and the basal ventilatory measurements were obtained over the next 30-60 s. Ventilatory responses to either steady state hypercapnia or progressive asphyxia were then determined; the order of the experiments was random, and separated from the other by at least 2 h, during which time the neonate was returned to its mother. Some of the neonates from the CO-treated and control groups were exposed to 12% O2 for 10 min to investigate whether these animals had a measurable ventilatory response to this level of hypoxia. This level of hypoxia did not produce a significant change of VT, f, or VE. This is consistent with previous findings that guinea pigs do not have a significant respiratory response to hypoxia(14), and this procedure was not tested further.
Steady state hypercapnia. To measure the ventilatory response to steady state hypercapnia, the volume of the measurement chamber was adjusted to a standard volume of 1500 mL in all experiments to prevent the accumulation of CO2 and reduction of O2 in the chamber during breathing measurements. The animal was placed in the chamber and allowed to sit quitely for 20 min while air was passed through at 5 L/min. The chamber was then sealed, and a measurement of basal ventilation was taken. Air was mixed with 10% CO2 to expose the animals to 2, 4, and 6% CO2. After the measurement of basal ventilation the chamber was flushed with 2% CO2 for 5 min, and a record of ventilation was again taken over at least 2 min. At this time the chamber temperature, relative humidity, O2 and CO2 concentrations, and the change in pressure caused by the injection of a known volume of air (for the purpose of calibration) were recorded. Once a record of ventilation was taken, the chamber was flushed with air for 10 min, and the animal was then exposed to 4% CO2 and, after 10 min of air breathing, to 6% CO2.
Progressive asphyxia. To measure the ventilatory response to progressive asphyxia, the animal was placed in the chamber, the volume of which was adjusted to 600 mL/100 g body weight; it was allowed to settle while breathing air for at least 20 min. The chamber was then sealed, and a record of ventilation obtained immediately. O2 and CO2 concentrations in the chamber were monitored continuously. A record of the respiratory pressure variations over at least 1 min was obtained each time the CO2 percentage increased by a whole number (e.g. 1, 2, 3%...) up to 8% CO2. The chamber temperature, relative humidity, O2 and CO2 concentrations, and the change in chamber pressure caused by the injection of a known volume of air (for the purpose of calibration) were recorded on the computer. The experiment ended when the CO2 concentration in the chamber reached 8%, and a record of ventilation had been obtained over 1 min.
Analysis. The amplitude of the pressure variation due to the tidal movement of gas, together with the pressure deflection caused by the injection of the calibration volume, were then analyzed by computer (Igor, WaveMetrics, Lake Oswego, OR). VT and VE were calculated using the equation given by Drorbaugh and Fenn(13). For the progressive asphyxia and steady-state hypercapnia experiments, VT, f, and VE were plotted against the FICO2. TI, TE, TTOTAL, and the inspiratory duty cycle(TI/TTOTAL), and a mechanical transform of the rate of rise of centrally generated inspiratory activity, the VT/TI, were also calculated(15).
Statistics. The effect of the CO exposure was evaluated by multiple analysis of variance using SPSSX Software on a VAX computer with animal, treatment, and litter size as the factors. Homogeneity of variance was tested using the Cochrane and Bartlett test, and the data were transformed before analysis where necessary. t tests were applied post hoc when multiple analysis of variance indicated a significant effect of treatment. Statistical significance was tested to the 5% level (p< 0.05). Results are expressed as the mean ± SEM.
RESULTS
COHb. The effect of exposure of pregnant guinea pigs to 200 ppm CO on fetal and maternal COHb and Hct are shown in Table 1. Maternal and fetal COHb and fetal Hct, but not maternal Hct, were increased significantly in the CO-treated animals. At 5-6 d of postnatal age, there was no difference in the concentration of COHb between the groups; however, Hct was significantly higher in the neonates from the CO-exposed group.
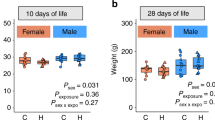
Outcome of pregnancy. The five pregnant animals exposed to air yielded 12 live newborn, whereas the six pregnant animals exposed to CO yielded 19 live pups. There was no significant difference between the groups for either length of gestation, litter size, or average birth weight(Table 2). At 4 d of age, the neonates from the CO-exposed mothers weighted significantly less than those in the control group.
Ventilatory measurements. Because of the variation in litter size between the animals, the neonates used for the ventilatory studies were drawn mainly from those litters consisting of two to four offspring, the most common litter size in our strain of guinea pigs. The few litters of five or more usually contained one or two growth-retarded neonates, which were specifically excluded from this study. Ten neonates each were selected from the five control and six CO-treated litters for the ventilatory studies.
Resting ventilation. Before the commencement of the hypercapnic tests, when the animals were at rest, a measurement of resting ventilation was taken. There was no difference between control and CO-treated groups for VT, f, VE, TI,TE, TTOTAL, or VT/TI at rest (Table 3). There was a significant difference between the groups for the inspiratory duty cycle (TI/TTOTAL), with the neonates from the CO group spending a significantly shorter period (45.6± 1.0%) inspiring per breath cycle than did the control animals (49.2± 1.0%; p < 0.05).
Steady state hypercapnia. Figure 1 shows the changes in the amplitude of the pressure variation due to the tidal movement of gas during steady state hypercapnia. Figure 2 shows the average VE, VT, f, and VT/TI during rest and during exposure to 2, 4, and 6% CO2 in the control and CO-treated groups. VT and VE were significantly increased in the CO-exposed animals at 4 and 6% CO2, this difference being due to the increase of VT, and not f. TI and TE were not different between the groups at either 2, 4, or 6% CO2. The inspiratory rate was slightly, but not significantly, greater in the CO-exposed animals, compared with controls.
Progressive asphyxia. Figure 3 shows the average VE, VT, f, and VT/TI during progressive asphyxia at 4-5 d of age. There was a significant difference between the control and CO-treated groups, evident from the time the CO2 in the chamber had reached 3%.VT was significantly larger in the CO-treated animals compared with the controls. There was a reduction in f during the progressive asphyxia, with a significant difference between the groups at 1 and 3% CO2. There was no significant difference between the groups for either TI, TE, TTOTAL, or TI/TTOTAL.VT/TI was significantly higher in the CO-treated group during progressive asphyxia compared with the control group (Fig. 3).
DISCUSSION
The COHb levels of the mothers and fetuses at 64 d of gestation were 8.5 and 13.0%, respectively, equivalent to values found in medium to heavy human smokers(16, 17). Maternal hematocrit was not increased significantly, but hematocrit was significantly higher in CO-treated fetuses and neonates at 5-6 d of age. The increase in fetal and neonatal hematocrit suggests that the animals were hypoxic as fetuses, or responded to some other effect of the COHb, sufficient to stimulate erythropoiesis. It has been found that there is only a very small reduction in maternal arterial Po2 with maternal COHb levels up to 20%(4). In the fetus, however, the arrterial Po2 was reduced by up to 50% at this level of COHb(4, 18). In organs which have a high O2 consumption, tissue hypoxia may occur when their O2 requirement exceeds the amount of O2 available in capillary blood. Hence, the effect of CO treatment on the mother and fetus is likely to be unequal because of the higher O2 consumption in the fetus and placenta(19).
The CO exposure from d 23-25 of pregnancy until parturition did not affect the length of gestation, litter size, or the average birth weight. Neonates in the CO-treated group gained significantly less weight over the first four postnatal days compared with the control neonates and were significantly smaller at 4 d of age. We cannot rule out the possibility that the CO-exposed dams produced less milk, but inspection of their mammary glands suggested that they were of normal size. The offspring of pregnant rats exposed to a high concentration (1200 ppm) of CO for 80 min/d throughout pregnancy also gained significantly less weight postnatally than did controls(8). As exposure to CO ceased at birth in both studies, it is evident that prenatal exposure to CO has significant developmental effects that persist postnatally. This may be due to either metabolic, absorptive, or neurologic changes that persist after birth. The hypoxia associated with prenatal exposure to CO may delay development of“nonessential” organ systems, including the gastrointestinal tract, and thus compromise the absorption of nutrients. The ability to feed may also be compromised, as rats with significant deficits in postnatal weight gain also showed delayed development in several standard neurologic tests(8). An increased metabolic rate, due to either changes in mitochondrial oxidative metabolism caused by the binding of CO to cytochrome P-450(4), endocrinologic changes, including increased thyroglobulin and thyroxine concentrations(20, 21), or changes in muscle metabolism due to chronic carboxymyoglobinemia(4) may also have occurred. The mechanisms involved in causing a reduction in postnatal growth thus require further investigation.
CO treatment did not alter resting ventilation of the newborn guinea pigs, except for a small but significant decrease in the ratio TI/TTOTAL. This appears to have occurred because of small changes in both TI and TE in the CO-treated neonates, although neither of these changes were significant in themselves. We are unsure of the significance of this finding. However, when ventilation was increased in response to CO2, whether given at a constant level in the inspired air or during progressive asphyxia, the VT of the CO-treated neonates was greater than in the control group. In general, there was no difference in f between the groups, except that a transient decrease in f occurred during the progressive asphyxia test and was greater in the CO-treated group during the early part of this test (i.e. when the inspired CO2 was<3%). The greater level of ventilation found in the CO-treated animals during progressive asphyxia was, therefore, primarily due to the increase in VT.
Similar effects on postnatal ventilation have been found after chronic prenatal exposure to cocaine(22). When neonatal guinea pigs exposed to cocaine throughout pregnancy were exposed to 5% CO2, they had a significantly higher VT than did controls with no difference in f between the groups. A dosedependent effect was also found, with the VT increase in response to 5% CO2 being greater at higher levels of cocaine exposure. Besides pharmacologic effects in the brain, cocaine exposure causes a significant degree of vasoconstriction in uteroplacental vascular beds, causing fetal hypoxia(23, 24). CO, through its binding to Hb, also causes tissue hypoxia. Thus, hypoxia may be the common prenatal factor that results in an increased neonatal sensitivity to CO2 after both CO and cocaine exposure.
The inspiratory rate (VT/TI) was significantly higher during progressive asphyxia in CO-treated neonates over the entire range of CO2 (1-8%). This occurred in the absence of a significant change in TI or TI/TTOTAL, possibly suggesting that a change in pulmonary stretch receptor afferent input into the brainstem was not responsible for this effect. Myelinated afferent vagal fibers arising from slowly adapting pulmonary stretch receptors in the lung terminate in the dorsal respiratory group neurons and in pontine structures, such as the Kolliker-Fuse and medial parabrachial nuclei(25). Stimulation of these receptors by increased lung volume act to shorten TI and thus limit the tidal volume. The increased inspiratory flow rate (VT/TI) observed in the present study occurred in the absence of a change in TI, an effect also seen in a previous study examining the effects of breathing 2% CO2 in normal human infants(15). The absence of any difference in inspiratory flow rate (VT/TI) between the groups during resting ventilation suggests that the difference observed during hypercapnia (whether steady state or progressive) arose through centrally mediated mechanisms linked to the increased CO2 sensitivity in these animals.
Much work has been done to elucidate the site and mechanisms of chemoreception in the guinea pig(26, 27). By recording from cranial hypoglossal nerve roots, it has been shown that chemoreceptive areas are found primarily on the ventral surface of the medulla(26). Immunohistochemical analysis of the brainstems of neonatal guinea pigs from the CO-exposed litters has shown that there is an increase in tyrosine hydroxylase and substance P immunoreactive staining in the nucleus tractus solitarius and lateral reticular nucleus(12) (and unpublished observations). Thus, significant changes in the neurochemistry of brainstem nuclei in areas relevant to breathing and chemoreception are present after prenatal exposure to CO. Whether these changes can account for the increase in CO2 sensitivity that has been described in this study will require further work(e.g. examination of the excitability of medullary respiratory neurones using in vitro techniques) to establish the connection, if any, between physiologic and neurochemical changes in the newborn wrought by CO exposure during pregnancy.
Abbreviations
- COHb:
-
carboxyhemoglobin
- f:
-
respiratory frequency
- Hct:
-
hematocrit
- ppm:
-
parts per million
- TE:
-
expiratory time
- TI:
-
inspiratory time
- TTOTAL:
-
total cycle time between breaths
- TI/TTOTAL:
-
inspiratory duty cycle
- VE:
-
minute ventilation
- VT:
-
tidal volume
- VT/TI:
-
inspiratory flow rate
References
Mitchell EA, Ford RP, Stewart AW, Taylor BJ, Becroft DM, Thompson JM, Scraag R, Hassal IB, Barry DM, Allen EM, Roberts AP 1993 Smoking and the sudden infant death syndrome. Pediatrics 91: 893–896
Foy A 1988 Cigarette smoking in pregnancy. Med J Aust 148: 377–378
Kelly J, Mathews KA, O'Connor M 1984 Smoking in pregnancy: effects on the mother and fetus. Br J Obstet Gynaecol 91: 111–117
Longo LD 1977 The biological effects of carbon monoxide on the pregnant woman, fetus and newborn infant. Am J Obstet Gynecol 129: 69–103
Garvey DJ, Longo LD 1978 Chronic low level maternal carbon monoxide exposure and fetal growth and development. Biol Reprod 19: 8–14
Rudolph AM, Itskovitz J, Iwamoto H, Reuss ML, Heymann MA 1981 Fetal cardiovascular responses to stress. Semin Perinatol 5: 109–121
Schellenberger MK 1982 Persisting effects on adult brain monoamines of neonatal distress and carbon monoxide exposure. Neuroscience 7: 667–671
Tachi N, Aoyama M 1990 Postnatal growth in rats prenatally exposed to cigarette smoke or carbon monoxide. Bull Environ Contam Toxicol 45: 641–648
Ting P, Wang P, Song H, Xu S 194 Neuro-pathophysio-biochemical profiles of neonatal asphyxia. Acta Neurochir Suppl 60: 203–206
Eldridge FL, Kilay JP, Millhorn DE 1984 Respiratory effects of carbon dioxide induced changes of medullary extracellular fluid pH in cats. J Physiol 355: 177–189
Hunt CE 1992 The cardiorespiratory control hypothesis for sudden infant death syndrome. Clin Perinatol 19: 757–771
Tolcos M, McGregor HP, Westcott K, Walker DW, Rees S 1996 Prenatal carbon monoxide exposure and its effects on brainstem development and respiratory regulation in the newborn guinea pig. Proc Aust Neurosci Soc 7: 121
Drorbaugh JE, Fenn WO 1955 A barometric method for measuring ventilation in newborn infants. Pediatrics 16: 81–87
Cragg PA, Menzies KJ 1992 Ventilatory responses of guinea pigs to hypercapnia and hypoxia. Proc Physiol Soc NZ 12: 17
Haddad GG, Leistner HL, Epstein RA, Epstein MA, Grodin WK, Mellins RB 1980 CO2-induced changes in ventilation and ventilatory pattern in normal sleeping infants. J Appl Physiol 48: 684–688
Heron HJ 1962 The effects of smoking during pregnancy: a review with a preview. NZ Med J 61: 545
Mactutus CF 1989 Developmental neurotoxicity of nicotine, carbon monoxide, and other tobacco smoke constituents. Ann NY Acad Sci 562: 105–122
Christensen PJ, Gronlund J, Carter AM 1986 Placental gas exchange in the guinea pig: fetal blood gas tensions following the reduction of maternal oxygen capacity with carbon monoxide. J Dev Physiol 8: 1–9
Moll W, Herberger J 1976 Oxygen uptake of the guinea pig at decreased and increased maternal placental blood flow. Adv Exp Med Biol 75: 705–712
Ericsson UB, Ivarsson SA, Persson PH 1987 Thyroglobulin in cord blood. The influence of the mode of delivery and the smoking habits of the mother. Eur J Pediatr 146: 44–47
Meberg A, Marstein S 1986 Smoking during pregnancy-effects on fetal thyroid function. Acta Paediatr Scand 75: 762–766
Olsen GD, Weil JA 1982 In utero cocaine exposure. Effect on neonatal breathing in guinea pigs. J Pharmacol Exp Ther 261: 420–428
Morgan MA, Silavin SL, Randolph M, Payne GG, Sheldon RE, Fishburne JI, Wentworth RA, Nathanielsz PW 1991 Effect of intravenous cocaine on uterine blood flow in the gravid baboon. Am J Obstet Gynecol 164: 1021–1027
Woods JR, Plessinger MA, Clark KE 1987 Effect of cocaine on uterine blood flow and fetal oxygenation. JAMA 257: 957–961
Taylor AE, Rehder K, Hyatt RE, Parker JC 1989 Clinical Respiratory Physiology. WB Saunders, Philadelphia, pp 199
Morin-Surun MP, Boudinst E, Schafer T, Denavit-Saubie M 1995 Localisation of chemosensitive structures in the isolated brainstem of the adult guinea pig. J Physiol 485: 203–212
Wennergren J, Wennergren M 1983 Neonatal breathing control mediated via the central chemoreceptors. Acta Physiol Scand 119: 139–146
Acknowledgements
The authors thank Phil Reynolds and Will Brenton for their assistance in designing and constructing the CO exposure chamber, Richard Carr for his assistance with data analysis, Dr. Sandra Rees and Mary Tolcos for providing neuroanatomical advice, and Prof. Richard Harding for reviewing this manuscript.
Author information
Authors and Affiliations
Additional information
Supported by a grant from the National Sudden Infant Death Council of Australia. H.P.M. was a Postgraduate Scholar of the Victorian Sudden Infant Death Research Foundation.
Rights and permissions
About this article
Cite this article
McGregor, H., Westcott, K. & Walker, D. The Effect of Prenatal Exposure to Carbon Monoxide on Breathing and Growth of the Newborn Guinea Pig. Pediatr Res 43, 126–131 (1998). https://doi.org/10.1203/00006450-199801000-00019
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199801000-00019