Abstract
Aldosterone, the most important mineralocorticoid, regulates electrolyte excretion and intravascular volume mainly through its effects on renal distal tubules and cortical collecting ducts, where it acts to increase sodium resorption from and potassium excretion into the urine. Excess secretion of aldosterone or other mineralocorticoids, or abnormal sensitivity to mineralocorticoids, may result in hypokalemia, suppressed plasma renin activity, and hypertension. The syndrome of apparent mineralocorticoid excess(AME) is an inherited form of hypertension in which 11β-hydroxysteroid dehydrogenase (11β-HSD) is defective. This enzyme converts cortisol to its inactive metabolite, cortisone. Because mineralocorticoid receptors themselves have similar affinities for cortisol and aldosterone, it is hypothesized that the deficiency allows these receptors to be occupied by cortisol, which normally circulates at levels far higher than those of aldosterone. We cloned cDNA and genes encoding two isozymes of 11β-HSD. The liver (L) or type 1 isozyme has relatively low affinity for steroids, is expressed at high levels in the liver but poorly in the kidney, and is not defective in AME. The kidney (K) or type 2 isozyme has high steroid affinity and is expressed at high levels in the kidney and placenta. Mutations in the gene for the latter isozyme have been detected in all kindreds with AME. Moreover, the in vitro enzymatic activity conferred by each mutation is strongly correlated with the ratio of cortisol to cortisone metabolites in the urine [tetrahydrocortisone (THF) + allo-THF]/THE. This suggests that the biochemical phenotype of AME is largely determined by genotype.
Similar content being viewed by others
Main
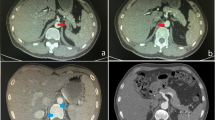
Aldosterone, the most important mineralocorticoid, regulates electrolyte excretion and intravascular volume mainly through its effects on renal distal tubules and cortical collecting ducts, where it acts to increase sodium resorption from and potassium excretion into the urine (Fig. 1) (reviewed inRef. 1). Excess secretion of aldosterone or other mineralocorticoids, or abnormal sensitivity to mineralocorticoids, may result in hypokalemia, suppressed plasma renin activity, and hypertension. Such conditions often have a genetic basis. Glucocorticoid-suppressible hyperaldosteronism and congenital adrenal hyperplasia due to 11β-hydroxylase deficiency are examples of autosomal dominant and recessive forms of mineralocorticoid excess, respectively(2). This article reviews studies of another such syndrome, AME, that provide valuable insights into normal and abnormal physiology of mineralocorticoid action.
Schematic of mineralocorticoid action. Top, a normal mineralocorticoid target cell in a renal cortical collecting duct. Aldosterone occupies nuclear receptors (MR) that bind to hormone response elements, increasing transcription of genes and directly or indirectly increasing activities of apical sodium (Na) channels and the basolateral sodium-potassium (Na/K) ATPase. This increases resorption of sodium from and excretion of potassium into the tubular lumen. Cortisol, which circulates at higher levels than aldosterone, cannot occupy the receptor because it is oxidized to cortisone by 11β-HSD.Bottom, a cell from a patient with the syndrome of apparent mineralocorticoid excess. Because 11β-HSD is absent, cortisol inappropriately occupies mineralocorticoid receptors, leading to increased gene transcription, increased activity of sodium channels and the Na/K ATPase, increased resorption of sodium and excretion of potassium, and hypertension.
Clinical features of the syndrome of apparent mineralocorticoid excess. AME is an inherited syndrome in which children present with hypertension, hypokalemia, and low plasma renin activity. Other clinical features include moderate intrauterine growth retardation and postnatal failure to thrive. Consequences of the often severe hypokalemia include nephrocalcinosis, nephrogenic diabetes insipidus, and rhabdomyolysis. Complications of hypertension have included cerebrovascular accidents, and several patients have died during infancy or adolescence. Several affected sibling pairs have been reported, but parents have usually been asymptomatic, suggesting that AME is a genetic disorder with an autosomal recessive mode of inheritance.
A low salt diet or blockade of mineralocorticoid receptors with spironolactone ameliorate the hypertension, whereas ACTH and hydrocortisone exacerbate it. Levels of all known mineralocorticoids are low(3, 4). These findings suggest that cortisol(i.e., hydrocortisone) acts as a stronger mineralocorticoid than is normally the case. Indeed, patients with AME have abnormal cortisol metabolism. Cortisol half-life in plasma is prolonged from approximately 80 min to 120-190 min(3). Very low levels of cortisone metabolites are excreted in the urine as compared with cortisol metabolites, indicating a marked deficiency in 11β-HSD, the enzyme catalyzing the conversion of cortisol to cortisone (Fig. 2). This is most often measured as an increase in the sum of the urinary concentrations of THF and allo-THF, divided by the concentration of THE [(THF + allo-THF)/THE]. However, 11-reduction is unimpaired; labeled cortisone administered to patients is excreted entirely as cortisol and other 11β-reduced metabolites(5). There is also an increase in the ratio of 5α- to 5β-reduced cortisol metabolites, allo-THF/THF(6), suggesting that 5β reduction is also impaired. The (THF + allo-THF)/THE is usually much higher than the allo-THF/THF ratio, and the two ratios are linearly related, implying that the primary defect in this disorder is indeed one of 11β-dehydrogenation. This has been assayed directly by administering 11α-[3H]cortisol to subjects and measuring the appearance of tritiated water.
Similar but milder abnormalities occur with licorice intoxication(7). The active component of licorice, glycyrrhetinic acid, inhibits 11β-HSD in isolated rat kidney microsomes(8). Thus, it appears that licorice intoxication is a reversible pharmacologic counterpart to the inherited syndrome of apparent mineralocorticoid excess.
WHY DOES 11β-HSD DEFICIENCY CAUSE HYPERTENSION?
Aldosterone acts through transcriptional effects mediated by a specific nuclear receptor referred to as the mineralocorticoid or “type 1 steroid” receptor. These receptors are expressed at high levels in renal distal tubules and cortical collecting ducts but also in other mineralocorticoid target tissues, including salivary glands and the colon. The mineralocorticoid receptor has a high degree of sequence identity with the glucocorticoid or “type 2” receptor(9), and it has very similar in vitro binding affinities for aldosterone and for glucocorticoids such as corticosterone and cortisol(9, 10).
It has been proposed(7, 11, 12) that oxidation by 11β-HSD of cortisol or corticosterone to cortisone or 11-dehydrocorticosterone, respectively, represents the physiologic mechanism conferring specificity for aldosterone upon the mineralocorticoid receptor (Fig. 1). Although cortisol and corticosterone bind the receptor well in vitro, cortisone and 11-dehydrocorticosterone are poor agonists for this receptor. Aldosterone is a poor substrate for 11β-HSD, because, in solution, its 11-hydroxyl group is normally in a hemiacetal conformation with the 18-aldehyde group. Thus, in AME or licorice intoxication, 11β-HSD deficiency permits cortisol to occupy the mineralocorticoid receptor. Because cortisol normally circulates at levels 100-1000 times those of aldosterone, this leads to signs of mineralocorticoid excess even when aldosterone secretion is suppressed. To confirm this hypothesis, we cloned cDNA and genes for two isozymes of 11β-HSD and tested their involvement in AME.
CLONING OF cDNA-ENCODING ISOZYMES OF 11B-HSD
There are two distinct isozymes of 11β-HSD (Table 1). The first, termed the liver (L) or type 1 isozyme, was originally isolated from rat liver microsomes(13). It is a glycoprotein with a molecular mass of 34 kD that requires NADP+ as a cofactor. A cDNA clone encoding this enzyme was isolated using an antiserum to the purified rat protein(14). The fulllength cDNA is 1.4 kb long including an open reading frame of 876 bp, predicting a protein of 292 amino acids. Although the enzyme purified from rat liver functions only as a dehydrogenase, the recombinant enzyme expressed from cloned cDNA exhibits both 11β-dehydrogenase and the reverse oxoreductase activity (conversion of 11-dehydrocorticosterone to corticosterone) when expressed in mammalian cells(14). At physiologic pH in cell lysates, the kinetic constants for dehydrogenation and reduction (Km of 1.1 and 1.4 μM, respectively) are almost identical(15). These findings imply that this isozyme actually catalyzes a fully reversible reaction and that reductase activity is destroyed during purification from the liver. The corresponding human gene for this isozyme, HSD11L(HSD11B1) is located on chromosome 1, and contains 6 exons with a total length of over 9 kb(16) (Fig. 3). No mutations were identified in this gene in patients with AME(17).
Other lines of evidence also suggest that this isozyme does not play a significant role in conferring ligand specificity on the mineralocorticoid receptor. This isozyme is expressed at highest levels in the liver, which does not respond to mineralocorticoids, and although it is expressed at high levels in the rat kidney(14), it is expressed at much lower levels in human(16) and sheep(18) kidneys. Even in rat kidney, immunoreactivity to the protein is observed primarily in proximal tubules and not in distal tubules and collecting ducts, the sites of mineralocorticoid action(19).
Accordingly, a second isozyme was sought in mineralocorticoid target tissues. Evidence for such an isozyme was obtained from biochemical studies of isolated rabbit kidney cortical collecting duct cells(20). Activity of 11β-HSD in the microsomal fraction was almost exclusively NAD+ dependent and had a Km for corticosterone of 26 nM. There was almost no reduction of 11-dehydrocorticosterone to corticosterone, suggesting that, unlike the liver(L) isozyme, the kidney (K) or type 2 isozyme catalyzed only dehydrogenation. The enzyme in the human placenta had similar characteristics(21); it was NAD+-dependent and had Km values for corticosterone and cortisol of 14 and 55 nM. Partial purification using AMP affinity chromatography suggested that this isozyme had a molecular weight of 40,000. Thus far, the K isozyme has not been purified to homogeneity in active form from any source. However, a homogenous preparation was recently obtained by a combination of affinity chromatography, affinity labeling, and preparative two-dimensional electrophoresis(22).
Cloning of cDNA encoding the K isozyme of 11β-HSD was rendered more difficult by the unavailability of purified enzyme that could be used to produce an antiserum or to obtain amino acid sequence data. However, because sheep and human kidneys predominantly expressed this type of enzyme, it was feasible to clone the corresponding cDNA by expression screening strategies in which pools of clones were assayed for their ability to confer NAD+-dependent 11β-HSD activity on Xenopus oocytes or cultured mammalian cells. Positive pools were divided into smaller pools and rescreened until a single positive clone was identified. Both sheep(23) and human(24) cDNA encoding this isoform were isolated in this manner. The recombinant K isozyme has properties that are virtually identical to the activity found in mineralocorticoid target tissues. The recombinant enzyme functions exclusively as a dehydrogenase; no reductase activity is detectable with either NADH or NADPH as a cofactor(23, 24). It has an almost exclusive preference for NAD+ as a cofactor and a very high affinity for glucocorticoids. Corticosterone is the preferred substrate, with first order rate constants 10 times higher than those for cortisol, even in mammalian species in which cortisol is the predominant glucocorticoid. Reported Km values for corticosterone are 0.7-10.1 nM and for cortisol, 14-47 nM.
The protein is predicted to contain 404 (sheep) or 405 (human) amino acid residues with a total Mr of 41,000 [the published sheep sequence(23) contains a frameshift error near the 3′ end of the coding sequence]. The human and sheep predicted peptide sequences are 83% identical. A search of sequence databases reveals sequence similarity to members of the short chain alcohol dehydrogenase superfamily. The 11β-HSD K isozyme is most similar (37% sequence identity) to the type 2 (placental, NAD+-dependent, microsomal) isozyme of 17β-HSD(25). It is only 21% identical to the L isozyme of 11β-HSD. The relatively high degree of similarity between the 11β-HSD K isozyme and placental 17β-HSD (comparable to the similarity between cytochrome P450 gene family members) suggests that these two enzymes may be in the same gene family within the short chain dehydrogenase superfamily.
Regions of sequence similarity between the two isozymes (Fig. 3) include part of the putative binding site for the nucleotide cofactor (residues 85-95 in the 11β-HSD K isozyme) and absolutely conserved tyrosine and lysine residues (Tyr-232 and Lys-236 in this enzyme) that function in catalysis(26, 27). The region immediately to the N-terminal side of the catalytic residues forms part of a putative steroid binding pocket in the short chain dehydrogenase that has been analyzed by x-ray crystallography, 3α,20β-HSD(28). This region is notably well conserved (10/18 identical residues) between the two isozymes of 11β-HSD, consistent with a role in binding the substrate.
The corresponding gene, termed HSD11K or HSD11B2, contains five exons spaced over approximately 6.2 kb(29)(Fig. 3). The putative binding site for the NAD+ cofactor (including the core sequence, G XXXG XG) is split between exons 1 and 2, whereas the putative catalytic residues, Tyr-232 and Lys-236, are encoded by exon 4. This structure is different from that of the HSD11L gene encoding the liver (type 1) isozyme of 11β-HSD(16), indicating that the two isozymes belong to different gene families.
HSD11K is expressed in placenta and mineralocorticoid target tissues, particularly the kidney, whereas it is not detected in the liver. Whereas human fetal and adult tissues contain transcripts of 1.9-2.0 kb(24, 29), fetal tissues also express transcripts of 5 and 7 kb(29). These may represent utilization of alternative polyadenylation sites or partially processed transcripts.
DETECTION OF MUTATIONS IN HSD11K IN PATIENTS WITH AME
We identified seven different mutations the HSD11K gene in eight kindreds with AME (Fig. 4). These mutations all affect enzymatic activity or pre-mRNA splicing, thus confirming in its entirety the hypothesis that 11β-HSD protects the mineralocorticoid receptor from high concentrations of cortisol(30). Seven other kindreds have been studied and an additional four mutations detected by others(31–33). Only one patient has been a compound heterozygote for two different mutations, whereas all other patients have carried homozygous mutations. This suggests that the prevalence of AME mutations in the general population is low, so that the disease is found mostly in limited populations in which inbreeding is relatively high. Six kindreds are of Native American origin. Three from Minnesota or Canada carry the same mutation (L250S,L251P), consistent with a founder effect, but the others are each homozygous for a different mutation. The reason for the relatively high prevalence of this very rare disease among Native Americans is not immediately apparent.
Of the mutations identified thus far, two shift the reading frame of translation, a third deletes three amino acids including a crucial catalytic residue (Tyr-232), and one is a nonsense mutation. These mutations are all presumed to completely destroy enzymatic activity. One mutation in the third intron leads to skipping of the fourth exon during processing of pre-mRNA(30). As the fourth exon encodes the catalytic site, the resulting enzyme is again presumably inactive. The other six mutations have been introduced into cDNA and expressed in cultured cells to determine their effects. One (L250P,L251S) is completely inactive and one (R337Δ3nt) has only a trace of activity. The others are all partially active in cultured cells with one, R337C, having greater than 50% of normal activity(34). Only R337C is partially active in lysed cells[although one group reported this mutation to be inactive in cell lysates(35), they did not use appropriate conditions to maximize enzyme stability(36)]. We believe that comparisons of activity are best made using the apparent first order rate constant,Vmax/Km, which predicts reaction velocity at low substrate concentrations. Valid comparisons in whole cells require controls (Western blots or determinations of mRNA levels) for transfection efficiency. However, determinations of apparent Km in whole cells need to be interpreted cautiously, particularly when high concentrations of substrate are used, because many substrates including steroids are subject to active transport into or out of cells(37). Such mechanisms, which have their own kinetics, can confound kinetic measurements of enzymes.
Both the wild type enzyme and most mutants are concentrated in the nucleus as determined by Western blots of cell fractions. All six mutants that we examined are expressed in decreased amounts suggesting that most of the mutations adversely affect protein stability once cells are lysed(34).
Although the number of patients with AME is small, sufficient data now exist to demonstrate a statistically significant correlation between degree of enzymatic impairment and biochemical severity as measured by the precursor:product ratio (THF + allo-THF)/THE(34). This correlation is most obvious for the partially active mutants. We assume that R337C is the only significant mutation in the patients who carry it, even though only one exon of the gene was sequenced(31). If so, a 50% impairment of enzymatic activity is apparently sufficient to compromise metabolism of cortisol in the kidney, suggesting that there is very little excess capacity to metabolize cortisol in this organ. This seems to raise a paradox, because AME is a recessive disorder and heterozygous carriers, who would be expected to have 50% of normal activity, are asymptomatic. Altered stability or kinetic properties of the R337C mutant may be important, including alterations in enzyme inhibition by end product(i.e., cortisone or corticosterone) or by other circulating steroids.
Because of the small numbers of patients, and the possible confounding effects of prior antihypertensive therapy, it is difficult to correlate biochemical severity with measures of clinical severity, although anecdotal reports suggest that mutations that do not destroy activity may be associated with milder disease(30, 31). With the elucidation of the molecular genetic basis of this disorder, ascertainment of additional cases may permit these questions to be answered.
Abbreviations
- AME:
-
apparent mineralocorticoid excess
- HSD:
-
hydroxysteroid dehydrogenase
- THF:
-
tetrahydrocortisol
- THE:
-
tetrahydrocortisone
References
White PC 1994 Disorders of aldosterone biosynthesis and action. N Engl J Med 331: 250–258.
White PC, Curnow KM, Pascoe L 1994 Disorders of steroid 11β- hydroxylase isozymes. Endocr Rev 15: 421–438.
Ulick S, Levine LS, Gunczler P, Zanconato G, Ramirez LC, Rauh W, Rosler A, Bradlow HL, New MI 1979 A syndrome of apparent mineralocorticoid excess associated with defects in the peripheral metabolism of cortisol. J Clin Endocrinol Metab 49: 757–764.
Oberfield SE, Levine LS, Carey RM, Greig F, Ulick S, New MI 1983 Metabolic and blood pressure responses to hydrocortisone in the syndrome of apparent mineralocorticoid excess. J Clin Endocrinol Metab 56: 332–339.
Shackleton CH, Rodriguez J, Arteaga E, Lopez JM, Winter JS 1985 Congenital 11β-hydroxysteroid dehydrogenase deficiency associated with juvenile hypertension: corticosteroid metabolite profiles of four patients and their families. Clin Endocrinol 22: 701–712.
Monder C, Shackleton CH, Bradlow HL, New MI, Stoner E, Iohan F, Lakshmi V 1986 The syndrome of apparent mineralocorticoid excess: its association with 11β-dehydrogenase and 5β-reductase deficiency and some consequences for corticosteroid metabolism. J Clin Endocrinol Metab 63: 550–557.
Stewart PM, Wallace AM, Valentino R, Burt D, Shackleton CH, Edwards CR 1987 Mineralocorticoid activity of liquorice: 11β-hydroxysteroid dehydrogenase deficiency comes of age. Lancet 2: 821–824.
Monder C, Stewart PM, Lakshmi V, Valentino R, Burt D, Edwards CR 1989 Licorice inhibits corticosteroid 11β-dehydrogenase of rat kidney and liver: in vivo and in vitro studies. Endocrinology 125: 1046–1053.
Arriza JL, Weinberger C, Cerelli G, Glaser TM, Handelin BL, Housman DE, Evans RM 1987 Cloning of human mineralocorticoid receptor complementary DNA: structural and functional kinship with the glucocorticoid receptor. Science 237: 268–275.
Krozowski ZS, Funder JW 1983 Renal mineralocorticoid receptors and hippocampal corticosterone binding species have identical intrinsic steroid specificity. Proc Natl Acad Sci USA 80: 6056–6060.
Edwards CR, Stewart PM, Burt D, Brett L, McIntyre MA, Sutanto WS, de Kloet ER, Monder C 1988 Localisation of 11β-hydroxysteroid dehydrogenase-tissue-specific protector of the mineralocorticoid receptor. Lancet 2: 986–989.
Funder JW, Pearce PT, Smith R, Smith AI 1988 Mineralocorticoid action: target tissue specificity is enzyme, not receptor, mediated. Science 242: 583–585.
Lakshmi V, Monder C 1988 Purification and characterization of the corticosteroid 11β-dehydrogenase component of the rat liver 11β-hydroxysteroid dehydrogenase complex. Endocrinology 123: 2390–2398.
Agarwal AK, Monder C, Eckstein B, White PC 1989 Cloning and expression of rat cDNA encoding corticosteroid 11β-dehydrogenase. J Biol Chem 264: 18939–18943.
Agarwal AK, Tusie-Luna MT, Monder C, White PC 1990 Expression of 11 betahydroxysteroid dehydrogenase using recombinant vaccinia virus. Mol Endocrinol 4: 1827–1832.
Tannin GM, Agarwal AK, Monder C, New MI, White PC 1991 The human gene for 11β-hydroxysteroid dehydrogenase. Structure, tissue distribution, and chromosomal localization. J Biol Chem 266: 16653–16658.
Nikkila H, Tannin GM, New MI, Taylor NF, Kalaitzoglou G, Monder C, White PC 1993 Defects in the HSD11 gene encoding 11β-hydroxysteroid dehydrogenase are not found in patients with apparent mineralocorticoid excess or 11-oxoreductase deficiency. J Clin Endocrinol Metab 77: 687–691.
Yang K, Smith CL, Dales D, Hammond GL, Challis JR 1992 Cloning of an ovine 11β-hydroxysteroid dehydrogenase complementary deoxyribonucleic acid: tissue and temporal distribution of its messenger ribonucleic acid during fetal and neonatal development. Endocrinology 131: 2120–2126.
Rundle SE, Funder JW, Lakshmi V, Monder C 1989 The intrarenal localization of mineralocorticoid receptors and 11β-dehydrogenase: immunocytochemical studies. Endocrinology 125: 1700–1704.
Rusvai E, Naray-Fejes-Toth A 1993 A new isoform of 11β-hydroxysteroid dehydrogenase in aldosterone target cells. J Biol Chem 268: 10717–10720.
Brown RW, Chapman KE, Edwards CR, Seckl JR 1993 Human placental 11 beta-hydroxysteroid dehydrogenase: evidence for and partial purification of a distinct NAD-dependent isoform. Endocrinology 132: 2614–2621.
Brown RW, Chapman KE, Murad P, Edwards CR, Seckl JR 1996 Purification of 11β-hydroxysteroid dehydrogenase type 2 from human placenta utilizing a novel affinity labelling technique. Biochem J 313: 997–1005.
Agarwal AK, Mune T, Monder C, White PC 1994 NAD+-dependent isoform of 11β-hydroxysteroid dehydrogenase: cloning and characterization of cDNA from sheep kidney. J Biol Chem 269: 25959–25962.
Albiston AL, Obeyesekere VR, Smith RE, Krozowski ZS 1994 Cloning and tissue distribution of the human 11-HSD type 2 enzyme. Mol Cell Endocrinol 105:R11–R17.
Wu L, Einstein M, Geissler WM, Chan HC, Elliston KO, Andersson S 1993 Expression cloning and characterization of human 17β-hydroxysteroid dehydrogenase type 2, a microsomal enzyme possessing 20α-hydroxysteroid dehydrogenase activity. J Biol Chem 268: 12964–12969.
Persson B, Krook M, Jornvall H 1991 Characteristics of short-chain alcohol dehydrogenases and related enzymes. Eur J Biochem 200: 537–543.
Obeid J, White PC 1992 Tyr-179 and Lys-183 are essential for enzymatic activity of 11β-hydroxysteroid dehydrogenase. Biochem Biophys Res Commun 188: 222–227.
Ghosh D, Weeks CM, Grochulski P, Duax WL, Erman M, Rimsay RL, Orr JC 1991 Three-dimensional structure of holo 3α,20β-hydroxysteroid dehydrogenase: a member of a short-chain dehydrogenase family. Proc Natl Acad Sci USA 88: 10064–10068.
Agarwal AK, Rogerson FM, Mune T, White PC 1995 Gene structure and chromosomal localization of the human HSD11K gene encoding the kidney (type 2) isozyme of 11β-hydroxysteroid dehydrogenase. Genomics 29: 195–199.
Mune T, Rogerson FM, Nikkila H, Agarwal AK, White PC 1995 Human hypertension caused by mutations in the kidney isozyme of 11β-hydroxysteroid dehydrogenase. Nat Genet 10: 394–399.
Wilson RC, Krozowski ZS, Li K, Obeyesekere VR, Razzaghy-Azar M, Harbison MD, Wei JQ, Shackleton CH, Funder JW, New MI 1995 A mutation in the HSD11B2 gene in a family with apparent mineralocorticoid excess. J Clin Endocrinol Metab 80: 2263–2266.
Wilson RC, Harbison MD, Krozowski ZS, Funder JW, Shackleton CH, Hanauske-Abel HM, Wei JQ, Hertecant J, Moran A, Neiberger RE, Balfe JW, Fattah A, Daneman D, Licholai T, New MI 1995 Several homozygous mutations in the gene for 11β-hydroxysteroid dehydrogenase type 2 in patients with apparent mineralocorticoid excess. J Clin Endocrinol Metab 80: 3145–3150.
Stewart PM, Krozowski ZS, Gupta A, Milford DV, Howie AJ, Sheppard MC, Whorwood CB 1996 Hypertension in the syndrome of apparent mineralocorticoid excess due to mutation of the 11β-hydroxysteroid dehydrogenase type 2 gene. Lancet 347: 88–91.
Mune T, White PC 1996 Apparent mineralocorticoid excess: genotype is correlated with biochemical phenotype. Hypertension 27: 1193–1199.
Obeyesekere VR, Ferrari P, Andrews RK, Wilson RC, New MI, Funder JW, Krozowski ZS 1995 The R337C mutation generates a high Km 11β-hydroxysteroid dehydrogenase type II enzyme in a family with apparent mineralocorticoid excess. J Clin Endocrinol Metab 80: 3381–3383.
Tusie-Luna MT, Traktman P, White PC 1990 Determination of functional effects of mutations in the steroid 21-hydroxylase gene(CYP21) using recombinant vaccinia virus. J Biol Chem 265: 20916–20922.
Gruol DJ, Bourgeois S 1994 Expression of the mdr1 P-glycoprotein gene: a mechanism of escape from glucocorticoid-induced apoptosis. Biochem Cell Biol 72: 561–571.
Author information
Authors and Affiliations
Additional information
Supported by National Institutes of Health Grant DK42169.
Rights and permissions
About this article
Cite this article
White, P., Mune, T., Rogerson, F. et al. 11β-Hydroxysteroid Dehydrogenase and Its Role in the Syndrome of Apparent Mineralocorticoid Excess. Pediatr Res 41, 25–29 (1997). https://doi.org/10.1203/00006450-199701000-00004
Issue Date:
DOI: https://doi.org/10.1203/00006450-199701000-00004
This article is cited by
-
Colfibrate attenuates blood pressure and sodium retention in DOCA-salt hypertension
Kidney International (2008)