Abstract
The nutritional requirements of preterm infants for the long chain polyunsaturated essential fatty acids, arachidonic acid (AA) and docosahexaenoic acid (DHA), have not been clearly defined. The present study evaluated preterm infants of less than 2.3 kg birth weight fed a commercial formula (Preemie SMA®) devoid of AA and DHA and compared this control group with similar infant groups fed one of three formulas containing a range of 0.32 to 1.1% AA and 0.24 to 0.76% DHA. An analogous group of infants fed their mothers' breast milk and a breast milk fortifier (when indicated) was also studied. Erythrocyte membrane phospholipids were isolated from blood samples collected at 12 d of age and after a further 4 wk of feeding. Infants fed the formula without AA and DHA showed a reduction in AA level in erythrocyte phosphatidylcholine, and a reduced level of DHA in phosphatidylethanolamine in comparison with infants fed breast milk or infant formula containing AA and DHA. Supplementing infant formula with increasing levels of AA and DHA produced a clear dose response in the levels of AA and DHA found in erythrocyte membrane phospholipids. From comparison of membrane phospholipid fatty acid composition it appears that a formula level of 0.32-1.1% AA and 0.24-0.76% DHA provides sufficient levels of these fatty acids to achieve a similar fatty acid composition to that of infants fed human milk for most of the lipid fractions examined.
Similar content being viewed by others
Main
The fetal brain accrues long chain (C20 and C22) fatty acids of both then-6 and n-3 families during the last trimester of gestation(1). These fatty acids may be derived from the placenta in utero with formation of major neural tissues requiring approximately 43 mg of n-6 and 22 mg of n-3 fatty acids per week(1–3). The n-6 accretion is predominately AA (C20:4n-6), whereas DHA (C22:6n-3) is the predominate n-3 fatty acid to accrue. Estimates of the labile hepatic fatty acid stores(4) indicate that, if intrauterine development is interrupted by premature delivery, these requirements for neural tissue synthesis can be supplied from liver lipids for only a limited period of time, 9 and 2.3 d for n-6 and n-3 fatty acids, respectively. The essential fatty acid reserve develops in adipose tissue only during the last trimester of fetal growth(5). Thus, the hepatic and adipose reserves cannot meet whole body needs for essential fatty acids and total fat if fetal development is interrupted by premature birth early in the third trimester.
Quantitative analysis of the composition of human milk from mothers giving birth to preterm infants(5,6) indicates that mothers' milk provides levels of 20:4n-6 and 22:6n-3 essential fatty acids approximating the predicted requirements at d 16 of life at oral intake levels of approximately 120 kcal/kg of body weight(5). Long chain essential fatty acids are synthesized from 18:2n-6 or 18:3n-3; however, the amounts producedin vivo may be inadequate to support the accretion rate attained in breast-fed infants(6,7). Thus, it seems prudent to feed the preterm infant human milk or formulas with a fatty acid balance similar to human milk containing long chain polyenoic homologs of 18:2n-6 and 18:3n-3(6). As the infant's body weight and milk intake increase, net intake of 20:4n-6 and 22:6n-3 will rapidly exceed predicted requirements. Levels of longer chain polyenoic homologs of 18:2n-6 and 18:3n-3 suggest that an adequate intake of mothers' milk provides quantities of these cell membrane structural precursors in excess of reported intrauterine rates of fatty acid accretion in neural and liver tissues(5).
To fully evaluate the appropriate preterm formula supplementation levels of C20 and C22:n-6 and n-3 fatty acids, the efficacious dietary intake needs to be established within levels that are practical. The objective of this study was to define the dietary level of AA and DHA in preterm formula that is necessary to achieve a composition of erythrocyte membrane phospholipid constituents similar to that observed for matched infants fed human milk.
METHODS
Subject inclusion and exclusion criteria. Medically stable preterm infants were recruited from the Neonatal Intensive Care Unit at the Children's Health Centre, Edmonton, Alberta, Canada. Informed written parental consent was obtained for all infants. Infants were appropriate weight for gestational age (Table 1). Further inclusion criteria stipulated that infants receive 100% of their daily fluid and energy requirements enterally by d 14 of life. Infants fed a mixed feeding regime(parenteral plus enteral nutrition) beyond d 14 of life or infants who received corticosteroids or red cell/plasma transfusions or i.v. lipid emulsions beyond d 8 of life were excluded from the study group. Infants with a major congenital malformation, documented systemic or congenital infection, significant morbidity, or acute illness were excluded from the study. The study was approved by the Research Ethics Committee of the Faculty of Medicine, University of Alberta and the Special Services and Research Committee, University of Alberta Hospitals.
Study population and feeding design. Infants were divided, based on maternal preference, into human milk or formula groups. Preterm mother's milk was expressed in the hospital, or at home, frozen, and delivered to the neonatal unit within 24 h. The formulas were prepared to contain a similar overall nutrient composition but contained increasing levels of AA (0.0-1.1%) and DHA (0.0-0.76%) in the fat component of the formula(Table 2). The ratio of AA to DHA was based on levels found in human milk(5) and remained constant among the experimental formulations (Table 2). The control formula(zero level of supplementation of AA and DHA) was the commercially available Preemie SMA® (Wyeth Nutritionals International, Radnor, PA). The AA and DHA triglycerides used were obtained from single cell oils (Martek Biosciences Corporation, Columbia, MD).
Infants were studied for the first 6 wk of life (Table 3). Venous blood samples and urine samples were obtained during the 2nd wk of life (wk 2, approximately 14 d of life) and the 6th wk of life (wk 6, approximately 42 d of life). Blood samples were analyzed for the fatty acid composition of erythrocyte membrane phospholipids, lymphocyte membrane phospholipids (to be reported separately), and plasma lipoprotein phospholipid(to be reported separately).
Clinical measures and analyses. As part of the clinical care of the infants studied, the following blood values were routinely monitored: red blood cell, white blood cell and platelet counts, hemoglobin, hematocrit, mean corpuscle volume, mean corpuscular hemoglobin concentration, white blood cell differential count, serum creatinine, and urinalysis. Crown-heel length and occipitofrontal head circumference was measured weekly. Body weight was measured daily during hospitalization.
Separation of blood cells. Blood samples, drawn into EDTA vacutainers, were centrifuged at room temperature (23°C) at 400× g for 10 min. The buffy coat and red blood cells were recovered and diluted to 6 mL with 20 g/L BSA (BSA fraction V; Sigma Chemical Co., St. Louis, MO) in PBS (pH 7.4). Cell types were separated on a two-layer ficoll gradient of Histopaque 1077 and Histopaque 1119 (Sigma Chemical Co.)(8). After centrifugation at 700 × g at 23°C for 30 min, lymphocyte and erythrocyte bands were recovered. Each of the cell fractions was washed twice with 10 mL of 20 g/L BSA in PBS and centrifuged at 200 × g at 4°C for 10 min.
Erythrocyte membranes were prepared by the method of Hanahan and Ekholm(9). Briefly, erythrocytes were lysed with 30 mL of 20 mosmol Tris buffer, pH 7.6, at 4°C. Samples were centrifuged at 20 000× g for 40 min at 4°C. The supernatant was decanted, and the pellet was resuspended in 30 mL of 20 mosmol Tris buffer and recentrifuged at 20 000 × g for 40 min. The erythrocyte membranes were washed once more.
Lipid analysis. Lipids from plasma, erythrocyte, and lymphocyte membranes were extracted by a modified Folch method(10) using chloroform:methanol (2:1 vol/vol) solution containing 0.05% (vol/vol) ethoxyquin as an antioxidant. Phospholipid classes were separated on silica H plates (Analtech, Newark, DE) using a solvent system of chloroform/methanol/2-propanol/0.25% wt/vol KCl/triethylamine(30:9:25:6:18, by volume)(11). Thin layer chromatography plates were visualized under UV light with 0.01% wt/vol anilino naphthalene sulfonic acid in water and phospholipid classes were compared against appropriate standards. Fatty acid methyl esters were prepared with 14% wt/wt boron trifluoride in methanol following the method of Morrison and Smith(12). Heptadecanoic acid was added before methylation for quantification of the fatty acid content of the plasma phospholipid fraction.
Fatty acid analysis. Fatty acid methyl esters were separated by automated gas-liquid chromatography, a Varian model 6000 equipped with a Vista 654 data system, and a Vista 8000 autosampler (Varian Instruments, Georgetown, ON) using a bonded fused silica BP20 capillary column(25 m × 0.25 mm inside diameter) and quantitated using a flame ionization detector(13). These conditions are capable of separating methyl esters of saturated, cis-monounsaturated and cis-polyunsaturated fatty acids from 14 to 24 carbons in chain length. Fatty acid content was calculated on a percent wt/wt basis and also where appropriate on a μg/mL basis from the known amount of standard added and determination of appropriate response factors. Quantitation and identification of peaks was based on relative retention times compared with known standards(pufa 1 and 2, bacterial methylester mix CP, gas-liquid chromatography mixes 10-100, and methylester mix-14; Supelco Canada, Mississauga, ON, Canada).
Statistical analysis. Statistical analyses included repeated measures ANOVA followed by Duncan's multiple range comparison or Bonferroni's pairwise comparison to assess the effect of feeding and postnatal age, respectively(14). Values are expressed as mean± SE. Statistical significance was accepted for p values<0.05.
RESULTS
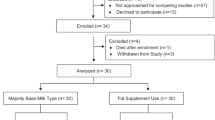
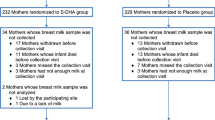
A total of 117 infants were enrolled in the study, and 91 infants successfully completed the study protocol. Eight infants in the human milk-fed group were disqualified from the study; six infants for protocol violations including receiving formula feeds, i.v. lipids or blood transfusions, and two infants failed to return for the second blood sampling period. Twenty-five infants receiving their own mother's milk (180-200 mL/kg/d) completed the protocol. A total of 18 infants from the formula groups did not complete the study protocol (six infants in the highest supplementation group and four infants in each of the remaining three formula groups). Eleven of these infants were disqualified due to protocol violations, five infants failed to return for the second sampling period, and two infants were excluded as per their physicians' request.
Demographic characteristics of infants are described inTable 1. Birth weight and head circumference were similar for all groups. However, gestational age and birth weight was significantly greater in the formula group with the high AA and DHA levels.
At wk 2 of life, body weight, length, and head circumference were similar among infants of all five diet groups (Table 3). By the 6th wk of life, formula-fed infants exhibited greater rates of growth in body weight and length compared with breast-fed infants. No differences in infant growth rates were observed among infants in the four formula groups regardless of AA + DHA supplementation.
Clinical values observed were within the normal range for all study groups; therefore, only the mean values for all groups at wk 2 and 6 are listed as follows: hemoglobin (g/L), 133 ± 2.2 and 96.7 ± 1.5; hematocrit(L/L), 0.39 ± 0.01 and 0.28 ± 0.0; white blood cell count(×109 cells/L), 11.5 ± 0.40 and 8.88 ± 0.27; mean corpuscle volume (g/L), 103 ± 0.49 and 94.0 ± 0.44; mean corpuscular Hb concentration (g/L), 342 ± 0.77 and 343 ± 0.71; red blood cell count (×1012 cells/L), 3.77 ± 0.06 and 3.00± 0.04; platelets (×109 cells/L), 427.9 ± 15.6 and 427.3 ± 15.1; lymphocytes (%), 56.2 ± 1.26 and 70.1 ± 1.01; neutrophils (%), 28.5 ± 1.12 and 17.5 ± 0.80; eosinophils(%), 3.42 ± 0.33 and 3.13 ± 0.26; basophils (%), 0.41 ± 0.08 and 0.29 ± 0.05.
Erythrocyte phospholipid fatty acid composition.Phosphatidylcholine. The fatty acid profile of erythrocyte phosphatidylcholine indicated that 16:0 is the major fatty acid(Table 4). Infants showed an age-related decline in 16:0 levels and an increase in 18:0 levels with age. Breast-fed infants had a significantly higher 16:0 level compared with infants fed the low or high AA + DHA formulas. Infants fed the highest level of AA + DHA supplementation showed a higher level of 18:0 compared with other diet groups. Oleic acid showed an age-related increase in level for infants fed the control formula and the two lower levels of AA + DHA supplementation. Infants fed human milk exhibited lower 18:1n-9 at both 2 and 6 wk of age compared with all formula-fed groups.
At 2 wk of age, human milk-fed infants showed significantly higher levels of DHA in red cell phosphatidylcholine compared with all infant groups fed formula. However, by 6 wk of age, infants in formula groups supplemented at the medium or high AA + DHA levels had similar concentrations of DHA in red cell phosphatidylcholine compared with human milk-fed infants. At 6 wk of age, infants fed the control formula had significantly lower DHA levels compared with human milk-fed infants and all infant groups fed AA + DHA-supplemented formulas. Levels of 18:3n-3 and 20:5n-3 were low throughout the study period, and infants showed a significant decline in 20:5n-3 levels with age.
With age, both control formula- and breast-fed infants showed an increase in 18:2n-6 and a decline in AA content. However, at 6 wk of age, infants fed the control formula had a significantly higher 18:2n-6 level and lower AA level compared with breast-fed infants or all those with AA+ DHA-supplemented formulas. Feeding infants formula supplemented at the low or medium AA + DHA levels resulted in similar concentrations of AA compared with human milk-fed infants. The highest level of AA and DHA supplementation resulted in AA levels that were significantly higher than those observed for human milk-fed infants (Table 4).
Phosphatidylethanolamine. As in phosphatidylcholine, 16:0 levels showed a small decline with age that reached statistical significance for infants fed the control formula and formulas containing medium or high AA + DHA levels (Table 5). Oleic acid exhibited a modest increase in concentration in infants fed the control formula or the low or medium level of AA + DHA-supplemented formula.
Levels of 18:3n-3 and 20:5n-3 were low (<0.2% and<0.7%, respectively) (Table 5). Infants supplemented at the highest AA + DHA level showed significantly lower 20:5n-3 levels compared with infants from all other diet groups. Infants fed the medium AA + DHA-supplemented formula exhibited a lower 20:5n-3 level compared with human milk-fed infants. DHA levels in infants fed the control formula declined significantly from wk 2 to wk 6. At 6 wk of age, infants fed the control formula exhibited significantly lower DHA levels compared with human milk-fed and all AA + DHA-supplemented formula-fed infants. Infants supplemented at the highest AA + DHA level showed significantly higher DHA levels compared with human milk-fed infants.
Levels of 18:2n-6 increased with age in all dietary groups; however, this change reached significance only for control formula and human milk-fed infants. Levels of AA were not influenced by age or dietary treatment in erythrocyte phosphatidylethanolamine.
Phosphatidylserine. The fatty acid profile indicated that 18:0 is the major fatty acid (Table 6). Diet treatment and age had little influence on saturated and monounsaturated fatty acid composition in phosphatidylserine. As in phosphatidylcholine and phosphatidylethanolamine fractions, levels of 18:3n-3 and 20:5n-3 remained low throughout the study period at <0.2% and <0.4%, respectively.
At 6 wk of age, infants fed the control formula exhibited significantly lower 22:6n-3 levels compared with human milk-fed infants or infants fed the medium or high AA + DHA-supplemented formulas.
Phosphatidylinositol. As in phosphatidylserine, 18:0 is the major fatty acid (Table 7) in phosphatidylinositol. Human milk-fed infants exhibited significantly lower 18:1n-9 levels compared with infants in all formula-fed groups. At 6 wk of age, 22:6n-3 level from infants fed the control formula was significantly lower than for the infants fed human milk. AA levels are high in phosphatidylinositol, but were unaffected by the diet treatment.
Total plasma phospholipid. Fatty acid content. Analysis of the quantitative fatty acid content of plasma phospholipids indicated a clear effect of diet resulting in significantly lower AA and DHA levels from infants fed the control formula compared with human milk-fed infants or infants fed formula supplemented with AA + DHA(Table 8). Feeding a formula supplemented with low or medium levels of AA + DHA produced levels of AA and DHA in the plasma phospholipid fraction similar to levels observed for infants fed human milk. However, feeding the highest level of supplementation resulted in levels of these fatty acids in plasma phospholipid that were significantly higher than levels from human milk-fed infants.
DISCUSSION
In North America, infant formulas do not contain long chain homologs of 18:2n-6 and 18:3n-3. The C20 and C22 essential fatty acids have just recently been introduced in formulas marketed in Europe. Inclusion of AA and DHA in formula fat blends has proven problematic as most sources of oil high in DHA and prepared in a manner acceptable for use in infant formulas contain little or no AA but have significant levels of 20:5n-3. Previous feeding studies have used addition of a fish oil(15–18). Our search for triglyceride source having potential to provide an optimal balance of long chain polyenoic fatty acids ruled out most marine oil sources on the basis of being too high in 20:5n-3 and relatively low in 20:4n-6(AA). Cultivation of freshwater catfish provided a source of high quality oil for purification of a triglyceride that contained a more acceptable but not ideal balance of long chain polyenoic essential fatty acids when combined with the appropriate levels of other triglyceride sources used in the normal fat components of formula(19). This modified formula contained approximately half the AA level typical of human milk, significant levels of other C20 and C22 carbon n-6 fatty acids to C20 and C22 carbon n-3 fatty acids(19). Preterm infants receiving this long chain polyenoic essential fatty acid balance exhibited plasma lipid fractions with similar fatty acid content to that observed for infants fed human milk(19). Similar findings have been reported for another modified formula(20).
Based on the plasma phospholipid content of C20 and C22 carbonn-6 and n-3 fatty acids, it is apparent that the small intestine and liver of infants fed human milk or formula containing very long chain polyenoic fatty acids produce phospholipids of different fatty acid content compared with those fed formula lacking in C20 carbon n-6 and C22 carbon n-3 fatty acids. It is apparent that feeding the balance of C20 and C22 carbon n-6 and n-3 fatty acids found in human milk results in incorporation of these fatty acids into circulating phospholipids and erythrocyte membrane phospholipids(Table 8). Whether or not tissues, such as developing brain and retina, use the essential fatty acid constituents derived from the plasma compartment for structural membrane synthesis in a manner that also reflects similar clear diet-induced differences in fatty acid composition remains to be determined. Animal studies indicate that dietary intakes that produce physiologic change in membrane structure and function in the intestinal mucosa and in liver also result in differences in membrane composition and in transitions in the function of other tissues, including specific membranes in brain(21–25) and in retina(24,26). Diet induced differences in function have recently been demonstrated for infants and may be beneficial(27).
In all lipid fractions examined, the level of 20:5n-3 was relatively unaffected by diet treatment and was not increased by supplementing with DHA. This observation suggests that there is little retroconversion of 22:6n-3 to 20:5n-3 that may result in increased incorporation of 20:5n-3 so formed into these subcellular fractions of blood cells.
In the present study it is apparent the range of supplementation for AA and DHA used does not result in any adverse effects on growth or clinical parameters normally monitored. From the fatty acid composition of erythrocyte membrane phospholipids it is clear that the medium level of AA + DHA supplementation provided for attainment of a fatty acid composition of these membranes that most closely reflected the membrane composition of a similar group of infants fed exclusively human milk. The same conclusion was also made by quantitative assessment of the available AA and DHA present in the plasma phospholipid pool. This suggests that approximately 0.6% AA and 0.4% DHA provide sufficient and perhaps optimum levels of these fatty acids in the formula fed.
Abbreviations
- AA:
-
arachidonic acid
- DHA:
-
docosahexaenoic acid
References
Clandinin MT, Chappell JE, Leong S, Heim T, m Swyer PR. Chance GW 1980; Intrauterine fatty acid accretion rates in human brain: implications for fatty acid requirements. Early Hum Dev 4: 121–129.
Clandinin MT, Chappell JE, Leong S, Heim T. Swyer PR. Chance GW 1980; Extrauterine fatty acid accretion in infant brain: implications for fatty acid requirements. Early Hum Dev 4: 131–138
Clandinin MT, Chappell JE, Leong S, Heim T. Swyer PR. Chance GW 1981; Fatty acid accretion in fetal and neonatal liver: implications for fatty acid requirements. Early Hum Dev 5: 7–14.
Clandinin MT, Chappell JE, Heim T, Swyer PR, Chance GW 1981; Fatty acid accretion in the development of the human spinal cord. Early Hum Dev 5: 1–6.
Clandinin MT, Chappell JE, Heim T, Swyer PR, Chance GW 1981; Fatty acid utilization in perinatal de novo synthesis of tissues. Early Hum Dev 5: 355–366.
Clandinin MT, Chappell Chappell JE, Heim T 1981; Do low birth weight infants require nutrition with chain elongation-desaturation products of essential fatty acids? Prog Lipid Res 20: 901–904.
Salem Jr N, Wegher B, Mena P, Uauy R 1996; Arachidonic and docosahexaenoic acids are biosynthesized from their 18-carbon precursors in human infants. Proc Natl Acad Sci USA 93: 49–54.
English D, Andersen BR 1974; Single-step separation of red blood cells. Granulocytes and mononuclear leukocytes on discontinuous density gradient of ficoll-hypaque. J Immunol Methods 5: 249–252.
Hanahan DJ, Ekholm JE 1972; Changes in erythrocyte membranes during preparation as expressed by ATPase activity. Biochim Biophys Acta 255: 413–419.
Folch J, Lees M, Sloane Stanley GH 1957; A simple method for the isolation and purification of total lipids from animal tissues. J Biol Chem 226: 497–509.
Touchstone JC, Chen JC, Beaver KM 1980; Improved separation of phospholipids in thin-layer chromatography. Lipids 15: 61–62.
Morrison WR, Smith LM 1964; Preparation of fatty acid methyl esters and dimethylacetals from lipids with boron fluoride-methanol. J Lipid Res 5: 600–608.
Hargreaves K, Clandinin MT 1987; Phosphatidylethanolamine methyltransferase: evidence for influence of diet fat on selectivity of substrate for methylation in rat brain synaptic plasma membranes. Biochim Biophys Acta 918: 97–105.
Steel RGD. Torrie JH 1960; Principles and Procedures of Statistics. McGraw-Hill, New York.
Carlson SE, Rhodes PG, Rao VS, Goldgar DE 1987; Effects of dietary long-chain polyunsaturated fatty acids on the essential fatty acid status of premature infants. Eur J Pediatr 148: 69–75.
Carlson SE, Cooke RJ, Rhodes PG, Peeples JM. Werkman SH, Tolley EA 1991; Long-term feeding of formulas high in linoleic acid and marine oil to very low birth weight infants: phospholipid fatty acids. Pediatr Res 30: 404–412.
Liu CF, Carlson SE, Rhodes PG, Rao VS, Meydrech EF 1987; Increase in plasma phospholipid docosahexaenoic and eicosapentaenoic acids as a reflection of their intake and mode of administration. Pediatr Res 22: 292–296.
Carlson SE, Rhodes PG, Ferguson MG 1986; Docosahexaenoic acid status of preterm infants at birth and following feeding with human milk or formula. Am J Clin Nutr 4: 798–804.
Clandinin MT, Parrott A, Van Aerde JE, Hervada AR, Lien E 1992; Feeding preterm infants a formula containing C20 and C22 fatty acids simulates plasma phospholipid fatty acid composition of infants fed human milk. Early Hum Dev 1: 41–51.
Koletzko B, Schmidt E, Bremer HJ, Haug M, Harzer G 1989; Effects of dietary long-chain polyunsaturated fatty acids on the essential fatty acid status of premature infants. Eur J Pediatr 148: 69–75.
Foot M, Cruz TF, Clandinin MT 1983; Effect of dietary lipid on synaptosomal acetylcholinesterase activity. Biochem J 211: 507–509.
Hargreaves K, Clandinin MT 1987; Phosphocholine transferase activity in plasma membrane: effect of diet. Biochem Biophys Res Commun 145: 309–315.
Clandinin MT, Field CJ, Hargreaves K, Morson LA, Zsigmond E 1985; Role of diet fat in subcellular structure and function. Can J Physiol Pharmacol 63: 546–556.
Connor WE, Neuringer M 1988; The effects ofn-3 fatty acid deficiency and repletion upon the fatty acid composition and function of the brain and retina. Biological membranes: aberrations in membrane. Prog Clin Biol Res 282: 275–294.
Jumpsen JA, Lien E, Goh YK, Clandinin MT 1997; Diets varying in n-3 and n-6 fatty acid content produce differences in phosphatidylethanolamine and phosphatidylcholine fatty acid composition during development of neuronal and glial cells in rats. J Nutr (in press)
Suh M, Wierzbicki AA, Clandinin MT 1994; Dietary fat alters membrane composition in rod outer segments in normal and diabetic rats: impact on content of very long chain (C ≥ 24) polyenoic fatty acids. Biochim Biophys Acta 1214: 54–62.
Carlson SE, Werkman S, Tolley EA 1996; Effect of long-chain n-3 fatty acid supplementation on visual acuity and growth of preterm infants with and without bronchopulmonary dysplasia. Am J Clin Nutr 63: 687–697.
Author information
Authors and Affiliations
Additional information
Supported by the Natural Sciences and Engineering Research Council of Canada, the Medical Research Council of Canada, and Wyeth Nutritionals International.
Rights and permissions
About this article
Cite this article
Clandinin, M., Van Aerde, J., Parrott, A. et al. Assessment of the Efficacious Dose of Arachidonic and Docosahexaenoic Acids in Preterm Infant Formulas: Fatty Acid Composition of Erythrocyte Membrane Lipids. Pediatr Res 42, 819–825 (1997). https://doi.org/10.1203/00006450-199712000-00017
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199712000-00017
This article is cited by
-
Enzymatic Modification of Anhydrous Milkfat with n‐3 and n‐6 Fatty Acids for Potential Use in Infant Formula: Comparison of Methods
Journal of the American Oil Chemists' Society (2016)
-
Aberrations in Plasma Phospholipid Fatty Acids in Lung Cancer Patients
Lipids (2012)
-
The rationale for the use of parenteral omega-3 lipids in children with short bowel syndrome and liver disease
Pediatric Surgery International (2008)
-
Soy‐Based Infant Formula Supplemented with DHA and ARA Supports Growth and Increases Circulating Levels of these Fatty Acids in Infants
Lipids (2008)
-
Controversies in neonatal nutrition: docosahexanoic acid (DHA) and nucleotides
Journal of Perinatology (2007)