Abstract
Arterial, venous, and intracardiac Doppler flow velocity waveforms were studied in 50 women with a small for gestational age (SGA) fetus according to a cross-sectional study design. No Doppler signals could be obtained in five women for technical reasons. The remaining 45 women were compared with normal control subjects matched for gestational age and maternal parity. The 45 SGA fetuses were divided into birth weight below the 5th centile for gestational age (group I, n = 35) and birth weight between the 5th and 10th centile for gestational age (group II, n = 10). A significant difference in baseline characteristics was found between both SGA subsets and normal controls. In SGA I fetuses, the pulsatility index in the umbilical artery and descending aorta was significantly higher, but lower in the middle cerebral artery when compared with normal controls. At the atrioventricular and venous level (umbilical vein, ductus venosus, and inferior vena cava) reduced time-averaged velocities were established. PIV in the ductus venosus and IVC showed a significant increase. Within the same SGA subset, no relationship could be established between arterial downstream impedance and1) atrioventricular flow velocities and 2) pulsatility index in the ductus venosus and inferior vena cava. Also, no relationship existed between flow velocity waveforms and pregnancy-induced hypertension and admission to the neonatal intensive care unit. Umbilical venous pulsations and absent/reverse flow in the umbilical artery were associated with a high intrauterine mortality rate and low birth weights. In SGA II fetuses, the pulsatility index in the umbilical artery and decending aorta was significantly higher than in normal controls. It can be concluded that fetuses with a birth weight below the 5th centile demonstrate marked changes in arterial, atrioventricular, and venous flow velocity waveforms. Atrioventricular and venous flow velocity waveforms change independently from arterial downstream impedance, suggesting that other factors, such as reduced volume flow and myocardial contraction force, may play a role in the observed changes.
Similar content being viewed by others
Main
Doppler ultrasonography has shown increased downstream impedance at the placental and fetal trunk level(1, 2) in the SGA fetus, whereas a brain-sparing effect has been demonstrated at the level of the internal carotid and middle cerebral artery(3, 4). Also, a fall in cardiac output and alterations in left ventricular function have been described(5, 6). Recently, fetal coronary blood flow has been suggested to be a possible indicator of severe compromise of the SGA fetus(7). Changes have also been described for venous flow velocity waveforms. Increased reverse flow in the IVC during atrial contraction has been reported(8), suggesting changes in cardiac function. Normal ductus venosus peak systolic velocities have been found in association with increased pulsatility index values in the umbilical artery(9), suggesting maintenance of preferential blood streaming through the ductus venosus during placental hemodynamic compromise. It can be concluded that there is a large body of information on the separate components of the abnormal circulation in the SGA fetus. However, only a few studies are available, which combine flow velocity waveforms recordings at the arterial, cardiac, and venous level(10). Insight into the intricate relationship between flow velocity waveform changes at different locations of the circulation in the SGA fetus may aid in the understanding of underlying mechanisms responsible for these changes.
We, therefore, set out in a cross-sectional study design, to establish the relationship between arterial, cardiac, and venous flow velocity waveforms in the SGA fetus and normal controls, to compare these waveforms between both subsets, and to relate flow velocity waveforms to pregnancy-induced hypertension and pregnancy outcome.
METHODS
Subjects. This cross-sectional study was performed over a period of 18 mo in the Department of Obstetrics and Gynaecology of the University Hospital Rotterdam-Dijkzigt, which serves as a tertiary referral center for cases of fetal growth retardation. It consisted of 50 women with a singleton pregnancy. SGA was defined as a sonographic fetal upper abdominal circumference below the 5th centile for gestational age(11). A detailed anomaly scan revealed no structural abnormalities. Of the 50 women participating in the study, no technically acceptable Doppler signals could be obtained in five women due to maternal obesity, fetal position, or fetal body movements. This left flow velocity waveform recordings of 45 women for further analysis. In 35 cases SGA was confirmed by the delivery of an infant below the 5th centile for gestational age (group I), whereas in the remaining 10 cases a birth weight was found between the 5th and 10th centile for gestational age (group II) according to Kloosterman's(12) tables corrected for parity and fetal sex. All infants were structurally normal. Gestational age at entering into the study ranged between 21 and 35 wk (mean: SGA I, 29 wk; SGA II, 30 wk), and maternal age varied between 17 and 34 y (mean: SGA I, 26 y; SGA II, 28 y). Thirty-six women were nulliparous.
Forty-five singleton pregnancies studied within the same time frame, displaying a fetal abdominal circumference between the 10th and 90th centiles for gestational age and a birth weight between 10th and 90th centile for gestational age according to Kloosterman's(12) tables served as matched controls. These women were selected from outpatients of the Department of Obstetrics and Gynaecology of the University Hospital Rotterdam-Dijkzigt. Matching took place with respect to gestational age and maternal parity. All women consented to participate in the study. The study protocol was approved by the Hospital Ethics Committee.
Pregnancy duration was determined from the last reliable menstrual period and confirmed by ultrasonic measurement of the fetal crown-rump length (8-12 wk) or fetal biparietal diameter (12-20 wk). Pregnancy-induced hypertension was defined as a diastolic blood pressure of 90 mm Hg or more during the second half of pregnancy in a previously normotensive woman. An abnormal fetal heart rate tracing was defined as the presence of late decelerations and a heart rate band width of less than 10 beats/min. Each woman was included in the study only once. Baseline characteristics of all pregnancies are provided in Table 1.
SGA I fetuses (<5th centile; n = 35). Eight of the 35 cases(23%) of SGA fetuses ended in intrauterine death between 21 and 31 wk of gestation. Of the remaining 27 live fetuses, 23 were delivered by cesarean section because of an abnormal fetal heart rate tracing. In the normal control subjects an abnormal fetal heart rate tracing at delivery was established in 4 out of 35 fetuses, and delivery by cesarean section took place for 5 fetuses because of an abnormal fetal heart rate tracing (n = 4) or previous fibroid resection (n = 1). A statistically significant difference(p < 0.001) was established for the incidence of abnormal fetal heart rates at delivery and the cesarean section rate between SGA fetuses and normal controls. Pregnancy-induced hypertension was present at the time of the Doppler study in 19 (54%) SGA I fetuses, whereas 3 (8%) developed hypertension at a later stage (p < 0.001). Twenty (57%) out of 35 SGA I fetuses were admitted to a neonatal intensive care unit versus none in the normal control group (p < 0.001). Twenty-four (69%) SGA I fetuses had a birth weight <2.3 centile corrected for parity and fetal sex. The pH and base excess data from the SGA I and control fetuses were not statistically compared because of the different modes of delivery:i.e. a cesarean section in 23 out of 27 live SGA I fetuses as opposed to a vaginal delivery in 30 out of 35 normal controls.
SGA II fetuses (5th-10th centile; n = 10). All 10 fetuses were born alive. of which 7 were delivered by cesarean section because of an abnormal fetal heart rate tracing (n = 5), fetal growth arrest(n = 1), or previous fibroid resection (n = 1) against none in the normal control group. The fetal heart rate tracing at delivery was normal in all 10 normal controls. Pregnancy-induced hypertension was present at the time of the Doppler study in two SGA II fetuses. Five fetuses were admitted to a neonatal intensive care unit versus none in the normal control group. Similar to the subset of SGA I fetuses, the pH and base excess were not statistically compared because of a cesarean section in 7 SGA II fetuses against a vaginal delivery in all normal controls.
Doppler recordings. Ultrasound Doppler studies were performed using a Hitachi EUB 450 combined transabdominal real-time and pulsed Doppler system with a carrier frequency of 3.5 MHz (real-time) and 3.0 MHz (Doppler)(Hitachi Medical Corporation, Tokyo, Japan). The system operates at power outputs of less than 100 mW/cm2 spatial peak-temporal average in both imaging and Doppler modes by manufacturer's specifications. Doppler recordings were performed by one examiner (P.v.S.). To avoid bias, clinicians were not informed about the Doppler findings.
At arterial level flow velocity waveforms were obtained from the descending aorta, middle cerebral artery, and umbilical artery. Flow velocity waveforms from the thoracic part of the descending aorta were recorded from a sagittal crosssection through the fetal trunk, displaying a major section of the fetal spine(13). Middle cerebral artery flow velocity waveforms were obtained from a transverse section through the lower part of the fetal cerebrum. The middle cerebral artery can be required as a major branch of the circle of Willis running anterolaterally toward the edge of the orbit(14). Umbilical artery flow velocity waveforms were obtained from a straight section of the free-floating loop of the umbilical cord.
Flow velocity waveforms at atrioventricular level were obtained from the cardiac “four chamber” view. Cardiac anomalies were ruled out. The Doppler sample volume was placed immediately distal to the mitral and tricuspid valve. Blood flow velocity recordings through the foramen ovale were made either from a four-chamber view or a modified short-axis view(15). The sample volume was placed across the septal opening.
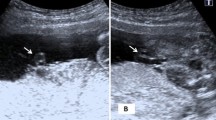
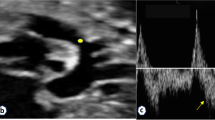
At the venous level, flow velocity waveform recordings were obtained from the extraabdominal umbilical vein, ductus venosus, and IVC. Flow velocity waveforms from the umbilical vein were collected from a free-floating loop of the umbilical cord. The sample volume was placed over a straight section of the cord. The fetal ductus venosus is localized in the liver, approximately between the right and left liver lobe. Its course is from caudal to cranial, from ventral to dorsal, and slightly oblique to the left. It originates from the posterior side of the umbilical sinus and joins the IVC close to the right atrium. The sample volume was placed immediately above the umbilical sinus, visualized in a transverse cross-sectional view(16). IVC flow velocity waveforms were recorded in a sagittal view, which included the fetal right atrium, right ventricle, and ascending aorta(17).
The angle of insonation for the descending aorta was less than 45°; for the middle cerebral artery, atrioventricular valves, and venous vessels less than 30°; and for the foramen ovale less than 20°. Sample volume length for all flow velocity waveform recordings ranged between 0.2 and 0.4 cm; the high pass filter was set at 100 Hz.
All Doppler studies were performed with the women in the semirecumbent position and during fetal apnea, because the latter may modulate flow velocity waveforms(18). The total examination time for the Doppler recordings was limited to 20 min in each instance. All flow velocity waveforms were recorded on hard copies. Waveform analysis was performed by one examiner (P.v.S.) using a microcomputer (Olivetti M24; Olivetti B.V., Leiden, The Netherlands) linked to a graphics tablet. For all waveforms the envelope of the waveform was measured.
The degree of pulsatility in the descending aorta, umbilical artery, and middle cerebral artery was expressed by the PI as calculated according to Gosling and King(19). Peak systolic (cm/s), end-diastolic (cm/s), and TAV (cm/s) were determined in the descending aorta and middle cerebral artery.
Analysis of the atrioventricular waveforms consisted of calculation of1) TAV (cm/s), 2) peak velocity (cm/s) of E wave (passive atrial filling) and A wave (atrial contraction), and 3) E/A ratio. The foramen ovale waveform consists of two components: 1) peak systolic velocity and 2) peak diastolic velocity coinciding with passive atrial filling(15). Flow velocity decreases to zero during atrial contraction. Extraabdominal umbilical venous pulsations were defined as at least three consecutive negative deflections of the venous waveform, each comprising at least 10% of the TAV and synchronous to fetal heart rate. In all recordings displaying umbilical venous pulsations, maximal velocity (cm/s), minimal or late diastolic velocity coinciding with atrial contraction (a; cm/s), and TAV (cm/s) were determined for three consecutive cardiac cycles from the maximum frequency envelop. In case of umbilical venous waveforms without pulsations, the TAV was analyzed at three different measuring points on the maximum frequency envelop in the continuous flow velocity waveform. Waveform analysis in the ductus venosus and the IVC consisted of calculation of 1) peak velocity (cm/s) during both systole and diastole and 2) TAV (cm/s). Moreover, the late diastolic flow velocity component coinciding with atrial contraction, was determined in the ductus venosus as minimal forward velocity (a; cm/s) and in the IVC as peak reverse velocity (a; cm/s). In the IVC time-velocity integral as expressed by the percentage of total forward flow was calculated. The degree of pulsatility in all three venous vessels, reflecting preload at venous level, was determined according to the following equation(10): PIV = (S - a)/TAV, in whichS = peak systolic velocity. Three consecutive flow velocity waveforms with the highest velocity and similar appearance were used to calculate the different parameters in each vessel.
Data analysis. Partial correlation coefficients were calculated to assess in both subsets for the gestational age-adjusted relationship between the pulsatility index in the umbilical artery and descending aorta and1) atrioventricular flow velocity waveform parameters and2) flow velocity waveform recordings in the umbilical vein, ductus venosus, and IVC. Partial correlation coefficients(20) were calculated to determine the interrelationship between the PIV in1) the umbilical vein and ductus venosus and 2) in the ductus venosus and IVC. For comparison between SGA fetuses and normal controls, the paired t test and McNemar's test were used for continuous and dichotomous variables, respectively. The t test and the Fisher exact test were used to compare independent groups for continuous and dichotomous variables, respectively. Logistic regression was used to estimate within the SGA fetus the association between flow velocity waveform parameters and the dependent variables: pregnancy-induced hypertension, intrauterine death, cesarean section rate, and admission to the neonatal intensive care unit. Taking a cut-off level of 14 d for relating velocity Doppler data to fetal heart rate tracings from SGA fetuses, the number of abnormal tracings in SGA I fetuses was too small (n = 5) for statistical analysis, whereas no abnormal tracings were established in SGA II fetuses at the time of Doppler examination. Relating flow velocity data to the mode of delivery was also not possible due to the small number of vaginal deliveries (SGA I, n = 4; SGA II, n = 3).
Data are presented as mean ± 1 SD. Statistical significance was tested at the level of 0.05.
RESULTS
Data will be presented separately for SGA I and SGA II fetuses.
SGA I Fetuses (<5th Centile; n = 35)
Baseline characteristics (Table 1). Statistically significant differences were found between SGA I fetuses and normal control subjects for the incidence of pregnancy-induced hypertension, abnormal fetal heart rate tracing at Doppler survey and delivery, cesarean section rate, gestational age at delivery, birth weight, Apgar score at 1 min, placental weight, and admission to the neonatal intensive care unit. In five normal control subjects, umbilical artery pH at delivery was below 7.18, and the base excess was below - 10 mEq/L. This was most likely the result of a prolonged labor, because there were no previous signs of placental insufficiency. These infants recovered completely after delivery with Apgar scores ≥7 and ≥8 at 5 and 10 min, respectively.
Relationship between arterial, venous, and atrioventricular flow velocity waveforms in the SGA I fetuses and normal controls(Tables 2–4). Both in SGA I fetuses and normal controls, no significant correlation could be established between the umbilical artery and descending aorta pulsatility index and atrioventricular and foramen ovale flow velocities, when adjusted for gestational age. In normal controls, transtricuspid flow velocities were significantly higher than transmitral flow velocities for E wave (mean difference -4.70, SD 5.53, p < 0.001) and TAV (mean difference-2.31, SD 5.52, p = 0.03). No such relationship could be established for A wave velocity and E/A ratio. In the SGA I fetuses, transtricuspid flow velocities were significantly higher than transmitral flow velocities for A wave velocity (mean difference -3.26, SD 7.33, p = 0.02) and TAV(mean difference -1.06, SD 2.83, p < 0.05). No relationship existed for E wave velocity and E/A ratio.
There was no significant correlation between arterial flow velocity waveforms and venous inflow parameters as expressed by umbilical venous, ductus venosus, and IVC PIV in both SGA I fetuses and normal controls. Umbilical venous pulsations were present in 17 (45%) out of 35 SGA I fetuses. After adjustment for gestational age, a statistically significant positive correlation was established between the PIV in the ductus venosus and IVC in SGA I fetuses (r = 0.74; p < 0.001) and in normal controls (r = 0.43; p < 0.05). In the SGA I fetus also, a statistically significant correlation was found between the PIV in the ductus venosus and umbilical vein (r = 0.72; p = 0.006).
When dividing umbilical artery end-diastolic velocities into present and absent (including 11 cases of reverse flow), a statistically significant difference was established for flow velocity parameters from the descending aorta, IVC, and umbilical vein (Table 5). Similarly, when dividing umbilical venous pulsations into present and absent, a statistically significant difference was observed for umbilical artery PI and IVC velocity parameters (Table 6).
Comparison of flow velocity waveforms between SGA I fetuses and normal controls (Tables 2–4). A statistically significant difference was established for all flow velocity waveform parameters, except for 1) peak systolic velocity in the middle cerebral artery, 2) all foramen ovale parameters,3) transmitral and transtricuspid E/A ratio, 4) mean difference in TAV between transmitral and transtricuspid flow velocity waveforms, and 5) peak systolic and peak diastolic velocity in the IVC. Statistical analysis of the PIV from the extraabdominal umbilical vein was not possible due to the small number (n = 1) of normal controls with umbilical venous pulsations. Reverse flow in the ductus venosus was demonstrated in two SGA fetuses. Comparison of flow velocity waveforms between SGA I fetuses and normal controls was not essentially different when taking into account the pregnancy period before and after 32 wk of gestation.
Flow velocity waveform parameters·in SGA I fetuses relative to pregnancy-induced hypertension and fetal outcome. Within the subset of 35 SGA I fetuses, there was no relationship between fetal velocity waveforms and pregnancy-induced hypertension (n = 19) or admission to the neonatal intensive care unit (n = 20). The eight cases of intrauterine death were delivered at a significantly earlier gestational age(mean 27 wk, range 21-31 wk, p<0.001) and had a significantly lower birth weight (mean 370 g; range 140-550 g, p < 0.001) than the remaining 27 fetuses that did not die in utero (mean 33 wk, range 27-39 wk; 1090 g, range 535-2420 g). Of the 11 cases of umbilical artery reverse flow, 5 were diagnosed as intrauterine death (45%) within 2 to 35 d after Doppler measurement (median 10 d). A statistically significant difference between umbilical artery end-diastolic flow velocities present and absent (including reverse flow), was established for 1) gestational age at delivery (34 ± 2.8 wk versus 29 ± 2.9 wk;p < 0.001), 2) birth weight (1279 ± 485 gversus 661 ± 292 g; p < 0.001), and 3) Apgar score at 1 min (6 ± 2.2 versus 4 ± 2.5versus; p = 0.02). A statistically significant difference between umbilical venous pulsations present and absent was observed for:1) gestational age at delivery (29 ± 3.6 wk versus 33 ± 3.2 wk; p = 0.002) and 2) birth weight (698± 366 g versus 1212 ± 517 g; p = 0.003). Of all 17 fetuses with umbilical venous pulsations, 41% died in utero within 2-35 d after Doppler measurement (median 13 d), whereas there was 100% fetal survival without umbilical venous pulsations.
There were two cases of reverse flow in the ductus venosus, both resulting in intrauterine death. The percentage reverse flow in the IVC was significantly higher (p = 0.03) in fetuses associated with intrauterine death (mean 23.34 ± 12.87%), when compared with fetal survival (mean 12.37 ± 4.33%).
SGA II Fetuses (5th-10th Centile; n = 10)
Baseline characteristics (Table 1) and flow velocity waveform data (Tables 2–4). Statistically significant differences were found between SGA II fetuses and normal controls for gestational age at delivery, birth weight, and placental weight. A statistically significant difference between SGA II fetuses and normal controls existed for the umbilical artery pulsatility index (p < 0.05), peak systolic (p < 0.05), TAV (p < 0.01) and end-diastolic velocity (p< 0.001) in the descending aorta, the ratio between descending aorta/umbilical artery pulsatility index (p < 0.05) and reverse flow in the IVC (p < 0.01). Umbilical venous pulsations were observed in three cases as opposed to none in the normal controls.
DISCUSSION
Second and early third trimester data are presented from a cross-sectional study of flow velocity waveforms at arterial, intracardiac, and venous level in normally developing and SGA fetuses. Characterization of functional aspects of the fetal cardiovascular system is of importance in the eventual understanding of normal and abnormal fetal hemodynamics. However, the contribution of Doppler flow velocity waveforms to our knowledge of fetal hemodynamics has its limitations, because no information is available on pressure or volume flow. Moreover, measuring cross-sectional vessel areas, particular in pulsating arteries, puts a restriction on the implication of Doppler ultrasound. Nevertheless, both angle-independent and angle-dependent Doppler assessment of flow velocity waveforms provide useful information on circulatory changes in the developing fetus.
Normal fetal development is characterized by a low fetoplacental vascular resistance with the objective to maintain optimal supply of oxygen and nutrients to the fetus. At cardiac level, flow velocities across the atrioventricular valves are higher during atrial contraction (A wave) than during early diastolic filling (E wave). Also, TAV at tricuspid valve level are significantly higher than at mitral valve level. Because volume flow is equal to TAV times cross-sectional vessel area, these data suggest right ventricular predominance during normal pregnancy. Right to left flow is present at the foramen ovale throughout the cardiac cycle with TAV slightly higher than at atrioventricular level.
Preferential streaming of highly oxygenated blood takes place from the placenta through the umbilical vein, ductus venosus, and foramen ovale into the left heart ensuring optimal oxygen supply to the brain and myocardium, whereas blood from the IVC is directed mainly to the right heart. In the fetal lamb, the ductus venosus acts as an important regulator of the venous circulation(21). In the present study of normal controls, mean TAV in the ductus venosus (52.1 cm/s) is more than 2-fold of that in the IVC (22.0 cm/s) and 4-fold of that in the extraabdominal umbilical vein (12.7 cm/s). The relatively high velocities in the ductus venosus are determined by the narrow vessel size which will never exceed 2 mm.
In the SGA fetus with a birth weight between the 5th-10th centile for gestational age (SGA II fetuses) significant changes occurred in umbilical artery, descending aorta and inferior vena cava flow velocity waveforms. These changes reflect some degree of raised fetal umbilical arterial downstream impedance, which would be coincident with the reduced placental weight suggesting impaired placental perfusion. The notion that the PI mainly represents downstream impedance was demonstrated in Texel ewes, in which Doppler flow velocity waveforms from the fetal descending aorta were related to peripheral vascular resistance. Vascular resistance was increased by stepwise embolization of the peripheral circulation. A rise in peripheral vascular resistance was associated with a reduction in peak and end-diastolic velocity and an increase in pulsatility index(22). However, in an other study, it was demonstrated that preservation of umbilical flow exists despite an increase in downstream impedance as expressed by systolic/diastolic ratio(23). The isolated presence of IVC reverse flow is more difficult to explain, although some reduction in atrial contraction cannot be ruled out in these mildly growth retarded fetuses.
In the SGA fetus with a birth weight below the 5th centile for gestational age (SGA I fetuses) significant changes were observed for nearly all cardiac and extracardiac arterial and venous flow velocity waveforms. Comparing the latter subset and normal controls, a difference was established in incidence of abnormal maternal conditions such as preeclamptic toxemia, mode of delivery and fetal outcome as expressed by fetal heart rate tracings at delivery, Apgar score at 1 min and admission to the neonatal intensive care unit. In the SGA I fetus, increased resistance to flow is demonstrated in the umbilical arteries and descending aorta, but a reduced resistance to flow is found in the middle cerebral artery, suggesting brain-sparing. Also, time-averaged and end-diastolic velocities were raised in the latter vessel as opposed to reduced velocities in the descending aorta, reflecting centralization of the fetal circulation, which is supposed to be mediated by arterial chemoreceptors(24).
Reduced transmitral and transtricuspid flow velocities were observed in the SGA I fetus, which is consistent with other studies(25, 26) and with own data on flow velocities from the ascending aorta, pulmonary artery, and ductus arteriosus(2). Velocity waveforms from atrioventricular valves reflect cardiac diastolic function. Major determinants of diastolic function such as ventricular relaxation rate and compliance were not investigated in the present study. An increase in ventricular relaxation rate associated with raised arterial downstream impedance has been established in the SGA fetus(27). As stated earlier, volume flow is equal to TAV times cross-sectional vessel area. The observed decrease in atrioventricular TAV may, therefore, be determined by a reduction in volume flow. A reduced preload suggested by a reduction in central venous return may play a role in this. Increased afterload is less likely to be the underlying mechanism for reduced atrioventricular TAV, because no relationship existed between atrioventricular flow velocities and downstream impedance as expressed by descending aorta and umbilical artery PI.
Our data suggest that right heart predominance is also present in fetal growth retardation. This is based on the TAV relationship between mitral and tricuspid valves, which is not different from normal controls. This is further supported by the presence of normal flow velocities across the foramen ovale. This observation of right ventricular predominance is at variance with other authors(6) who reported a shift of cardiac output in favor of the left heart in the SGA fetus. In our study, both absent or reverse end-diastolic flow velocities in the umbilical artery and pulsatile umbilical venous velocities, reflecting advanced fetal hypoxemia(28), are not associated with a shift to left heart predominance. Whereas our cross-sectional study design does not allow information on serial flow velocity waveform changes, the present study demonstrates that centralization of the circulation may occur before changes in cardiac right/left relationship become evident. No difference could be found in E/A ratios between SGA I and normally developing fetuses, indicating that E and A wave velocities are subject to a similar reduction in the presence of fetal growth retardation.
Reduced TAV are shown in all three venous vessels in the SGA I fetus. Studies in normal late first and early second trimester pregnancies suggest that gestational age-related changes in flow velocities are mainly determined by volume changes associated with fetal growth(29). It is speculated, therefore, that the observed reduction in TAV at the venous, arterial, and atrioventricular level in fetal growth retardation indirectly reflects a growth-related reduction in volume flow. This is further supported by the virtually unaltered TAV relationship between the three venous vessels, when compared with normal control subjects. From the pulsatility index for veins an estimate of cardiac preload can be obtained, reflecting ventricular end-diastolic pressure(10). The positive correlation between the PIV in the ductus venosus and IVC both in normal controls and SGA I fetuses is explained by the equal effect of right ventricular end-diastolic pressure changes on flow in these two vessels in the presence of a closed foramen ovale(15). In the SGA I fetus, the increase in PIV in the ductus venosus and IVC may be attributed to the marked reduction in flow velocity during atrial contraction in the presence of relatively high peak systolic and peak diastolic flow velocities, suggesting increased end-diastolic right ventricular pressure(10). In fetal hypoxemia increased downstream impedance would result in increased ventricular afterload and therefore raised ventricular systolic pressure. However, in the present study, the pulsatility index for veins in all three venous vessels appears to be independent of arterial downstream impedance as expressed by descending aorta and umbilical artery PI, suggesting other factors to play a role in the observed changes in cardiac preload, such as the time delay between reduced placental flow and rise in umbilical artery PI as mentioned earlier.
Absent or even reverse end-diastolic flow in the umbilical artery is accompanied by a further reduction in IVC and umbilical venous flow velocities. Fetal birth weight in this subgroup of SGA I fetus is approximately half of that in the presence of end-diastolic flow velocities even though a mean gestational age difference of 5 wk may be responsible for most of this weight difference. Also, the Apgar score at 1 min was lower in cases with absent or reverse end-diastolic velocities, indicating fetal hypoxemia. One may speculate that, next to diminished fetal growth, reduced myocardial contraction force associated with fetal hypoxemia may be responsible for the further deterioration of venous flow velocities. Intrauterine death occurred in nearly half of the cases with end-diastolic reverse flow in the umbilical artery, although in one instance the time interval between the Doppler recording of reverse flow and intrauterine death was as long as 35 d. Similar findings were done in the presence of umbilical venous pulsations. The high intrauterine mortality rate (44%) confirms results from other studies on umbilical venous pulsations in SGA fetuses(10, 30, 31).
The degree of hemodynamic adaptation to chronic hypoxemia as seen in intrauterine growth retardation is related to fetal maturity, e.g. gestational age(10). However, in the present study velocity differences between SGA I fetuses and normal controls were not essentially different when comparing the pregnancy period before and after 32 wk.
It can be concluded that cardiovascular changes are most prominent in SGA fetuses with a birth weight below the 5th centile for gestational age. Whereas there is a change from a low uteroplacental vascular resistance to a high vascular resistance at placental and fetal trunk level, redistribution of blood flow takes place in favor of the fetal brain. Flow velocity waveforms at cardiac and venous level change independently from arterial downstream impedance, suggesting other factors may play a role in these changes, such as a time delay between change in umbilical flow and change in umbilical downstream impedance. Longitudinal studies will be needed to elucidate the natural history of cardiovascular changes in the SGA fetus.
Abbreviations
- a:
-
late diastolic venous velocity
- IVC:
-
inferior vena cava
- PI:
-
pulsatility index for arteries
- PIV:
-
pulsatility index for veins
- SGA:
-
small for gestational age
- TAV:
-
time-averaged velocity
References
Trudinger BJ, Giles WB, Cook CM, Bombardieri J, Collins L 1985; Fetal umbilical artery flow velocity waveforms and placental resistance: clinical significance. Br J Obstet Gynaecol 92: 23–30.
Groenenberg IAL. Wladimiroff JW, Hop WCJ 1989; Fetal cardiac and peripheral arterial flow velocity waveforms in intrauterine growth retardation. Circulation 80: 1711–1717.
Wijngaard van den JAGW, Gr Groenenberg IAL, Wladimiroff JW, Hop WCJ 1989; Cerebral Doppler ultrasound of the human fetus. Br J Obstet Gynaecol 96: 845–849.
Noordam MJ, Heydanus R, Hop WCJ, Hoekstra FME, Wladimiroff JW 1994; Doppler colour flow imaging of fetal intracerebral arteries and umbilical artery in the small-for-gestational age fetus. Br J Obstet Gynaecol 101: 504–508.
Reed KL, Anderson CF, Shenker L 1987; Changes in intracardiac Doppler blood flow velocities on fetuses with absent umbilical artery diastolic flow. Am J Obstet Gynecol 157: 774–779.
Rizzo G, Arduini D 1991; Fetal cardiac function in intrauterine growth retardation. Am J Obstet Gynecol 165: 876–882.
Gembruch U, Baschat AA 1996; Demonstration of fetal coronary blood flow by color-coded and pulsed wave Doppler sonography: a possible indicator of severe compromise and impending demise in intrauterine growth retardation. Ultrasound Obstet Gynecol 7: 10–16.
Rizzo G, Arduini D, Romanini C 1992; Inferior vena cava flow velocity waveforms in appropriate and small for gestational age fetuses. Am J Obstet Gynecol 166: 1271–1280.
Kiserud T, Eik-Nes SH, Blaas HG, Hellevik LR, Simensen B 1994; Ductus venosus blood velocity and the umbilical circulation in the seriously growth-retarded fetus. Ultrasound Obstet Gynecol 4: 109–114.
Hecher K, Campbell S, Doyle P, Harrington K, Nicolaides K 1995; Assessment of fetal compromise by Doppler ultrasound investigation of the fetal circulation. Arterial, intracardiac, and venous blood flow velocity studies. Circulation 91: 129–138.
Snijders RJM, Nicolaides KH 1994; Fetal biometry at 14-40 weeks' gestation. Ultrasound Obstet Gynecol 4: 34–38.
Kloosterman GJ. 1970; On intrauterine growth. Int J Gynaecol Obstet 8: 895–912.
Eik-Nes SH, Brubakk AO, Ulstein MK 1980; Measurement of human fetal blood flow. BMJ 280: 283–284.
Wladimiroff JW. Tonge HM, Stewart PA 1986; Doppler ultrasound assessment of cerebral blood flow in the human fetus. Br J Obstet Gynaecol 93: 471–475.
van Eyck J, Stewart PA, Wladimiroff JW 1990; Human fetal foramen ovale flow velocity waveforms relative to behavioral states in normal term pregnancy. Am J Obstet Gynecol 163: 1239–1242.
Huisman TWA. Stewart PA, Wladimiroff JW 1992; Ductus venosus blood flow velocity waveforms in the human fetus; a Doppler study. Ultrasound Med Biol 18: 33–37.
Reed KL. Appleton CP, Anderson CF, Shenker L, Sahn DJ. 1990; Doppler studies of vena cava flows in human fetuses; insight into normal and abnormal cardiac physiology. Circulation 81: 498–505.
Maršál K. Eik-Nes SH, Lingblad A, Lingman G. 1984; Blood flow in the fetal descending aorta; intrinsic factors affecting fetal blood flow, i.e. fetal breathing movements and cardiac arrhythmia. Ultrasound Med Biol 10: 339–348.
Gosling RG, King DH. 1975; Ultrasonic angiology. In: Marcus W, Adamson L (eds) Arteries and Veins. Churchill-Livingstone, Edinburgh 61–98.
Altman DG. 1993; Relation between two continuous variables. In: Practical Statistics for Medical Research. Chapman & Hall, London, 296–298.
Edelstone DI. Rudolph AM, Heymann MA 1978; Liver and ductus venosus blood flows in fetal lambs in utero. Circ Res 42: 426–433.
Noordam MJ. Wladimiroff JW, Lotgering FK, Struyk PC. Tonge PM 1987; Fetal blood flow velocity waveforms in relation to changing peripheral vascular resistance. Early Hum Dev 15: 119–227.
Giles WB. Lingman G, Maršál K. Trudinger BJ 1986; Fetal volume blood flow and umbilical artery flow velocity waveform analysis: a comparison. Br J Obstet Gynaecol 93: 461–465.
Bartelds B, van Bel F, Teietl DF. Rudolph AM 1993; Carotid, non aortic chemoreceptors mediate the fetal cardiovascular response to acute hypoxaemia in lambs. Pediatr Res 34: 51–55.
Reed KL, Meijboom EJ, Sahn DJ, Scagnelli SA, Valdes-Cruz LM. Shenker L 1986; Cardiac Doppler flow velocities in human fetuses. Circulation 73: 41–46.
Stoddard MF, Pearson AC, Kern MJ, Ratcliff J, Mrosek DG, Labovitz AJ 1989; Influence of alteration in preload on the pattern of left ventricular diastolic filling as assessed by Doppler echocardiography in humans. Circulation 79: 1226–1236.
Tsyvian P, Malkin K, Wladimiroff JW 1995; Assessment of fetal left cardiac isovolumic relaxation time in appropriate and small-for-gestational age fetuses. Ultrasound Med Biol 21: 739–743.
Hecher K, Snijders R, Campbell S, Nicolaides K 1995; Fetal venous, intracardiac, and arterial blood flow measurements in intrauterine growth retardation: relationship with fetal blood gases. Am J Obstet Gynecol 173: 10–15.
van Splunder P, Stijnen T, Wladimiroff JW 1996; Fetal atrioventricular waveforms and their relation to arterial and venous flow velocity waveforms at 8-20 wk of gestation. Circulation 94: 1372–1378.
Indik JH, Chen V, Reed KL 1991; Association of umbilical venous with inferior vena cava blood flow velocities. Obstet Gynecol 77: 551–557.
Arduini D, Rizzo G, Romanini C 1993; The development of abnormal heart rate patterns after absent end-diastolic velocity in umbilical artery: analysis of risk factors. Am J Obstet Gynecol 168: 43–50.
Author information
Authors and Affiliations
Additional information
Supported by the Dutch Organization for Scientific Research NWO Grant 900-516-139.
Rights and permissions
About this article
Cite this article
Van Splunder, P., Stijnen, T. & Wladimiroff, J. Fetal Atrioventricular, Venous, and Arterial Flow Velocity Waveforms in the Small for Gestational Age Fetus. Pediatr Res 42, 765–775 (1997). https://doi.org/10.1203/00006450-199712000-00008
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199712000-00008