Abstract
S Fetal alcohol syndrome is one of the leading causes of mental retardation in the United States, but the pathogenesis of the associated brain damage is unknown. We tested the hypothesis that neonatal cerebrovascular responses to CO2 and/or hypoxia may be altered by moderate chronic maternal ethanol exposure early in gestation. We studied 26 newborn lambs (1-4 d old). Their mothers had received daily i.v. infusions of either ethanol (1 g/kg; ethanol concentration = 167 ± 3 mg/dL; mean ± SEM) or a similar volume of saline for 3 wk during the first trimester. In nine lambs, we studied cerebral responses to CO2 (saline, n = 4; ethanol,n = 5) and in 17 lambs, cerebral responses to hypoxia (saline,n = 7; ethanol, n = 10). Cerebrovascular responses to CO2 were not different between the groups. However, the cerebral vasodilatory response to hypoxemia was significantly attenuated in the ethanol lambs, such that cerebral O2 delivery was not maintained. During severe hypoxia (arterial Po2 = 30 mm Hg), cerebral blood flow increased 106± 23% (mean ± SEM) above baseline in the saline-treated group, but increased only 32 ± 15% above baseline in the ethanol-treated group(p < 0.02). Similarly, cerebrovascular resistance in the saline group decreased 52 ± 6% from baseline, but decreased only 16 ± 11% in the ethanol group (p < 0.02). We conclude that moderate maternal ethanol infusion early in pregnancy attenuates neonatal hypoxic, but not CO2, cerebrovascular responsivity.
Similar content being viewed by others
Main
Fetal brain damage from maternal ethanol abuse is considered one of the leading causes of mental retardation in the United States, yet how ethanol affects brain development and function is largely unknown(1, 2). Ethanol is known to have both acute and chronic effects on cerebral blood vessels. Acute (generally high dose) ethanol exposure decreases cerebrovascular responses to hypercapnia, impairs cerebral autoregulation, depresses cerebral O2 consumption, and may cause either cerebral vasoconstriction and/or vasodilation, depending on the experimental conditions(3–7). Chronic high dose ethanol exposure alters cerebral vascular responses to vasoactive agents, such as adenosine, acetylcholine, histamine, and epinephrine(8–10).
Ethanol intoxication during pregnancy affects the fetoplacental unit as well as the mother. Acute maternal ethanol intoxication causes alterations in placental blood flow, constriction of umbilical blood vessels, fetal hypoglycemia, and decreased fetal cerebral blood flow and oxygen consumption, an effect that increases with advancing gestation(11–14). Chronic maternal ethanol exposure alters the development of both neurons and blood vessels and alters regulation of neurotransmitters and their receptors(10, 15–18).
No studies have examined cerebral vascular reactivity in vivo after chronic in utero ethanol exposure. Furthermore, most studies or models of fetal alcohol effects have used large doses of alcohol, similar to those used by alcoholics; low to moderate maternal alcohol consumption is considerably more common, and consequently, any observed fetal effects would be of great clinical interest. We hypothesized that chronic moderate maternal ethanol intoxication early in pregnancy could alter fetal cerebral vascular development so that normal neonatal cerebrovascular responses to CO2 and/or hypoxia would be impaired. Abnormal neonatal cerebral vascular reactivity could provide an important clue to the pathogenesis of brain damage after fetal alcohol exposure.
METHODS
All surgical procedures and experimental protocols were approved by our institutional Animal Care and Use Committee.
Subjects and preparation. Pregnant ewes. Twenty-one mixed-breed adult pregnant ewes were obtained from time-dated pregnancies confirmed by mating and cycling dates. At 31 ± 1 (SEM) d of gestation(range 28-35 d), the ewes were brought to the laboratory. One day before starting the i.v. infusions, the ewe was placed under general anesthesia with halothane (1-2%) and a 16-gauge Intracath (Deseret Medical Inc., Sandy, UT) was inserted into the external jugular vein and sutured into place. Benzathine and procaine penicillin (1 200 000 U) were administered intramuscularly to the ewes just before catheter insertion. On the day after surgery, and then daily for the next 3 wk, an i.v. solution of either pure ethanol (Warner Graham Co., Cockeysville, MD), 1 g/kg, diluted 1:2 in normal saline, volume 3.8 mL/kg or normal saline (3.8 mL/kg) was infused over 1 h. Ewes were given free access to water and food during the infusions. After each infusion, the catheter was flushed with 3 mL of normal saline and then filled with 2 mL of heparinized saline (10 U/mL). Benzathine and procaine penicillin (1 200 000 U) were administered intramuscularly to the ewes once per week. Blood samples (1.5 mL) were drawn twice weekly for measurements of alcohol, glucose, and lactate concentrations (pre- and immediately postinfusion) from the opposite external jugular vein. At the end of 3 wk, catheters were removed, and the ewes were observed overnight and then returned to the farm and allowed to deliver spontaneously at term. At the farm, ewes were evaluated using abdominal ultrasound at 60-80 d of gestation to confirm pregnancy and to estimate fetal size and number.
Newborn lambs. We studied 26 newborn lambs delivered from the 21 ewes who underwent infusions. Nine lambs (saline, n = 4 and ethanol,n = 5) underwent studies of CO2 responsivity, and 17 lambs(saline, n = 7 and ethanol, n = 10) underwent studies of hypoxic responses. Newborn lambs (1-4 d old) were brought to the animal care facility on the day of study. Standard physical examinations, including behavioral evaluations and measurement of weight and head circumference, were performed. The lambs were anesthetized with pentobarbital (15-20 mg/kg i.v.) via a small catheter placed percutaneously in the external jugular vein. Additional i.v. doses of pentobarbital (1-2 mg/kg) were administered as needed throughout the experiment. The trachea was intubated, and mechanical ventilation was begun with a respirator pump (Harvard Apparatus Inc., Natick, MA). Polyvinyl chloride catheters (Martech Medical Products, Harleysville, PA) were placed into the left ventricle and brachiocephalic artery (via axillary arteries) and into the descending aorta and inferior vena cava (via femoral artery and vein).
To gain access to the sagittal sinus, a burr hole was drilled in the midline of the skull, approximately 1 cm anterior to the lambdoid sutures. The sagittal sinus was identified, and the overlying dura was punctured with a 19-gauge needle. A polyvinyl chloride catheter was then introduced into the sagittal sinus, and its tip was positioned anterior to the confluence of the sinuses to minimize contamination from extracerebral venous blood. The skin incisions were sutured closed, and all catheters were sutured into place. The lambs were then paralyzed with pancuronium bromide, 0.1 mg/kg, i.v. Studies were performed under pentobarbital anesthesia and began after a 90-min period for postsurgery equilibration.
Physiologic measurements. Organ blood flows were measured by the radiolabeled microsphere technique, and the least squares method of differential spectroscopy(19). Approximately 1 000 000 microspheres (0.4 mL) labeled with 153Gd, 114In, 103Ru,95 Nb, 13Sn, or 46Sc (DuPont NEN, Boston, MA) were injected over 0.5 min into the left ventricle, followed by 5 mL of normal saline. Reference blood samples were withdrawn from the brachiocephalic artery at a rate of 2.55 mL/min, beginning 30 s before the microsphere injection and continuing for 1.0 min after the injection was completed. The microsphere injections were not associated with changes in heart rate, blood pressure, or pulse pressure. After completion of the study, the lamb was killed with an overdose of pentobarbital sodium followed by saturated KCl solution. Catheter placements were checked, and the brain removed at the base and divided at the cephalic border of the pons. All supratentorial tissue was pooled and counted to determine CBF. The cerebellum was removed at the peduncles and counted separately, as was the brainstem (pons and medulla). The radioactivity in all samples was determined using a multichannel gamma counter (Packard Instrument Co., Inc. Powers Grove, IL). All reference blood and tissue samples contained>400 microspheres.
Blood samples for pH, respiratory blood gases, Hb concentration, oxygen saturation, and lactate and glucose concentrations were withdrawn anaerobically into heparinized syringes. Respiratory blood gases and pH were measured at 39.5 °C using the Radiometer ABL 30 (Radiometer, Copenhagen, Denmark). Oxygen saturation and Hb concentration were measured using an OSM-3 Hemoximeter (Radiometer). Whole blood lactate and glucose concentrations were measured using the YSI model 2300 glucose-lactate analyzer (Yellow-Springs Instrument Co., Inc., Yellow Springs, OH). Maternal blood alcohol concentration was measured enzymatically via alcohol dehydrogenase oxidation(Sigma Chemical Co. Diagnostics, St. Louis, MO). Arterial blood pressure(referenced to the level of the right atrium) and heart rate were continuously monitored (Gould Instruments, Oxnard, CA).
Experimental protocol. After stabilization of blood pressure, heart rate, and arterial blood gas values, the studies began. During each study, four to five measurements were made. For each measurement, blood samples were slowly withdrawn from the brachiocephalic artery and superior sagittal sinus (0.5 mL of each vessel) and analyzed for pH, Hb concentration, oxygen saturation, blood gases, and lactate and glucose concentration. After blood sampling, radiolabeled microspheres (0.4 mL) were injected into the left ventricle, whereas reference samples were withdrawn from the brachiocephalic artery.
CO2 responses. After two baseline measurements were made during normocapnia, defined as Paco2 = 32-38 mm Hg, the ventilator rate was adjusted to achieve a desired Paco2. The Paco2 levels chosen for hypocapnia were 18-22 mm Hg and for hypercapnia, 50-58 mm Hg. Animals returned to normocapnia after hypocapnia, and measurements were made. Then, animals were made hypercapnic. After reaching a desired Paco2, the lambs were stabilized for 15 min at each level of Paco2 (end tidal CO2 monitor; Nellcor, Hayward, CA), before measurements were made. Arterial Po2 was maintained by altering the fractional concentration of inspired O2 in the gas mixture to keep arterial oxygen saturation >92%.
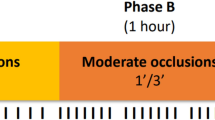
Hypoxic responses. Two baseline measurements were made during normoxia, defined as Pao2 >85 mm Hg; moderate hypoxemia was then induced by lowering the inspired O2 concentration to achieve Pao2 = 40-50 mm Hg. This level of hypoxemia was maintained for 15 min before making measurements. Severe hypoxemia was induced by further decreasing inspired O2 concentration to achieve Pao2 = 25-30 mm Hg. Animals did not return to normoxia between moderate and severe hypoxemia measurements. After this level of hypoxemia was maintained for 15 min, measurements were repeated. During the study, the ventilator rate was adjusted to maintain a constant Paco2.
Data analysis/calculations. CBF was calculated as CBF = cpmbrain/cpmref × 2.55 mL/min, where cpmbrain and cpmref represent radioactive counts/min in brain and reference samples, respectively. Cerebral O2 consumption (CMRo2) was calculated as CMRo2 = [Cao2 - Cvo2] × CBF, where Cao2 and Cvo2 represent arterial and venous oxygen content, respectively. OD was calculated as OD = [Cao2] × CBF. Cerebral oxygen extraction (E) was calculated as E = CMRo2/OD. CVR was calculated as MAP ÷ CBF, where MAP is mean arterial blood pressure.
Differences among the different conditions within groups were tested by analysis of variance for repeated measurements. For the analysis of variance, if the F test indicated significance, differences between individual means were tested using Neuman-Keuls. An unpaired t test was used to identify differences between groups. The slopes of the cerebral blood flow responses to hypoxemia were obtained by taking the average of the slopes of each individual animal; the average slopes from each group were then compared using an unpaired t test. Differences were considered significant if p < 0.05. All results are expressed as mean ± SEM.
RESULTS
Mean maternal blood alcohol concentrations immediately after the 1 h of ethanol infusions were 167 ± 3 mg/dL; levels after the last infusion were similar to those after the first infusion. Maternal ethanol infusion caused a slight decrease in maternal glucose concentration (blood glucose 38± 1 mg/dL versus 40 ± 1 mg/dL baseline) and an increase in lactic acid (blood lactate 9 ± 1 mg/dL versus 6± 1 mg/dL baseline). Saline infusion caused a slight increase in glucose concentration (42 ± 1 mg/dL versus 38 ± 1 mg/dL baseline) with no change in lactic acid concentration.
We studied 26 full-term newborn lambs at 1-4 d of age (n = 15 ethanol; n = 11 saline). Fifteen of the lambs were one of twins(n = 7 ethanol; n = 8 saline), and four were one of triplets (n = 2 ethanol; n = 2 saline). Physical and physiologic profiles of the newborn lambs are shown in Table 1. There were no differences between ethanol and saline lambs in body weight, head circumference, gestational age at infusion, or in baseline arterial blood gases, heart rate, blood pressure, Hb, or glucose or lactate concentrations. There was a difference in the age at study; saline lambs were, on average, 1 d older than ethanol lambs.
CO2 responses. Physiologic variables at baseline and during hypocapnia and hypercapnia in ethanol and saline lambs are shown in Tables 2 and 3. Baseline values are consistent with previous physiologic studies in newborn lambs. Comparison between baseline values and posthypocapnic normocapnic values showed no differences, indicating that the animals had returned to baseline before the hypercapnia measurement. Therefore, comparisons of hypercapnic and normocapnic values were done using the baseline data. Pao2 and pH increased during hypocapnia in ethanol lambs but was unchanged in saline lambs. Regional brain blood flow and percent change from baseline at different levels of Paco2 are shown in Table 3. CBF at baseline was not significantly different for saline and ethanol lambs(p = 0.45). There were no differences in blood flow responses to alterations in Paco2 between saline and ethanol lambs. During hypocapnia, CBF decreased by 34 ± 8% (saline) and 27 ± 6%(ethanol) from baseline (p = 0.15), whereas during hypercapnia, CBF increased by 121 ± 22% (saline) and 113 ± 22% (ethanol) from normocapnic values (p > 0.5). CVR measured at different levels of Pco2 is also shown in Table 3. There were no differences in CVR responses to CO2 between saline and ethanol lambs. The decreases in blood flow during hypocapnia and increases in blood flow during hypercapnia are consistent with data from previous studies of CO2 responsivity in lambs(20).
Cerebral O2 metabolism results are shown in Table 4. Similar to previous studies, fractional O2 extraction tended to increase during hypocapnia and decrease during hypercapnia and cerebral O2 delivery tended to decrease during hypocapnia and increase during hypercapnia. There were no differences between groups.
Hypoxic responses. Cardiovascular variables during nor-moxemia, moderate hypoxemia, and severe hypoxemia are shown in Table 5. Baseline values are consistent with previous physiologic studies in newborn lambs. Paco2 decreased slightly during moderate and severe hypoxemia in the ethanol group, but this decrease is physiologically insignificant with regards to CBF responses to hypoxia(21). There was a significant increase in heart rate during hypoxemia in the saline lambs, but not in the ethanol lambs. Regional brain blood flow and CVR, and percent change from baseline in response to reductions in Cao2 for both groups are shown in Table 6. Ethanol lambs showed blunted cerebral vasodilatory responses compared with saline lambs (p < 0.02, both moderate and severe hypoxia). Attenuation of blood flow in ethanol lambs was similar in cerebral cortex, brainstem, and cerebellum. Cerebral vasodilation was also blunted when results are compared with previous studies in newborn lambs(22, 23). Furthermore, a leastsquares fit of the CBF responses against the reciprocal of Cao2 was performed to achieve a linear transformation in each lamb. We previously found that use of the reciprocal of Cao2 provides a good linear fit in newborns lambs(23). The mean slope of the regression lines for the 10 ethanol lambs (258 ± 227) was considerably less than the mean slope for the saline lambs (877 ± 106).
Cerebral O2 metabolism results are shown in Table 7. Reductions in Cao2 during moderate and severe hypoxemia were similar in both groups. CMRo2 was unchanged in both groups. Cerebral oxygen delivery was maintained during hypoxia in saline lambs but decreased during severe hypoxia in ethanol lambs. Oxygen extraction increased during moderate and severe hypoxemia in both groups.
DISCUSSION
The major finding of this study is that neonatal cerebrovascular responses to CO2 after chronic alcohol exposure early in pregnancy are well maintained, but cerebrovascular responses to moderate and severe hypoxic hypoxia are attenuated, such that cerebral oxygen delivery is not maintained.
We chose our moderate maternal ethanol dosing protocol for two major reasons. First, a similar 1 g/kg i.v. dose had been used in several previous acute intoxication studies in pregnant sheep, and maternal tolerance of the dose has been well described(13, 14, 24). As expected, the blood alcohol concentration in our ewes (167 ± 3 mg/dL) was similar to that achieved in these previous studies and is equivalent to drinking ≈7.5 oz of alcohol as a 40% solution (80 proof). For reference, legal intoxication while driving (DWI) in the United States is charged at a blood alcohol level of 100 mg/dL; significant narcosis occurs at 200 mg/dL; stupor and coma occur at 300 mg/dL(25). During the 1 st wk of ethanol infusions, the ewes became drowsy and unbalanced; they often sat down. They appeared fully recovered within a few hours. The ewes developed tolerance over the 3-wk period, so that by the last week, they showed no signs of alcohol intoxication. A second reason for selecting our maternal ethanol dosing protocol is that low to moderate maternal alcohol consumption during the first trimester is more common than severe alcoholism during the entire pregnancy. Although most investigators and clinicians believe that fetal alcohol syndrome is caused only by heavy maternal alcohol abuse, there is still controversy regarding whether moderate or low maternal alcohol exposure has any adverse effects on the developing fetal brain(26). Moderate maternal alcohol consumption (especially before a woman knows she is pregnant) is thus of significant clinical and social concern.
There are several possible explanations for the attenuation of newborn hypoxic vasodilation after chronic maternal alcohol exposure. First, prolonged alcohol exposure early in pregnancy could retard growth and development of cerebral blood vessels so that mature newborn blood vessels would behave like immature fetal blood vessels. We and others have shown that, in sheep, cerebrovascular CO2 response curves are virtually superimposable in immature fetuses, mature fetuses, newborns, and adults(20, 27, 28), whereas in contrast, the cerebral vasodilatory response to hypoxia is attenuated in immature fetuses, and because of this, cerebral O2 delivery is impaired(29). The mechanism for this effect is unknown except for work done by Kurth et al.(30), in which they demonstrated normal cerebral vasodilation in response to adenosine in immature fetal sheep. Thus, cerebrovascular responses of ethanol-exposed newborn lambs are similar to immature fetal sheep in that cerebrovascular responses to hypoxia are attenuated, whereas CO2 responses are not. Perhaps ethanol exposure in vivo affects hypoxic cerebral vasodilation by a similar mechanism to that which causes attenuated vasodilatory responses in immature fetal sheep. In support of this theory, several rat studies have shown decreased generation and impaired migration of cortical neurons as well as“simple” dendritic arborization caused by gestational alcohol exposure, and alcohol may affect growth of developing cerebral blood vessels similarly(15, 16, 18). Second, prenatal alcohol exposure could alter vasomotor tone in developing cerebral blood vessels by altering sensitivity to sympathetic stimulation or by creating abnormalities in neurotransmitter levels or receptor function. Sympathetic nerve stimulation reduces CBF during hypoxia in rabbits and immature cerebral blood vessels reportedly have greater sensitivity to adrenergic and cholinergic stimulation than mature vessels(31, 32). Chronic alcohol intoxication potentiates the vasoconstrictor response to epinephrine in rats and one mechanism for this could be an alteration in sympathetic vascular tone(8). If a similar mechanism occurred in developing sheep, increased reflex stimulation of the sympathetic nervous system during hypoxia might therefore oppose hypoxic vasodilation. Third, alcohol could impair dilation of cerebral blood vessels locally by affecting neuronal or endothelial synthesis or release of vasodilatory substances, such as adenosine or acetylcholine. In support of this hypothesis, ethanol-fed rats have impaired endothelium-dependent vasodilation of cerebral arterioles, believed to be due to impaired synthesis and/or release of nitric oxide, and in cats, ethanol potentiates norepinephrine-induced contraction and selectively inhibits endothelium-dependent relaxation in isolated middle cerebral arteries(4, 5). Mayhan et al.(10) reported that the vasodilatory response of cerebral arterioles to histamine was markedly attenuated, and vessels constricted in response to acetylcholine in rats chronically exposed to alcohol. Fourth, alcohol exposure could produce hypersensitivity of vascular smooth muscle to vasoconstrictor stimuli. Cerebral vasoconstriction has been described in rat vessels exposed to alcohol; calcium antagonists prevent or reverse this effect(8). Others have shown a similar effect in cat blood vessels, noting that vasoconstriction was endothelium-independent and that alcohol facilitated the vascular smooth muscle response to nor-adrenaline(4).
Our observation that hypercapnic cerebral vasodilation was preserved, whereas hypoxic cerebral vasodilation was attenuated is best explained by considering possible effects of ethanol on the separate mechanisms believed to be responsible for hypercapnic and hypoxic vasodilation(33). For example, hypoxic cerebral vasodilation is believed to be related, in part, to neuronal or endothelial release of vasodilatory substances such as adenosine, acetylcholine, and nitric oxide, whereas hypercapnic cerebral vasodilation is believed to be more dependent on the local effects of pH changes on the vascular endothelium. Any effect of ethanol on the development of neuronal or endothelial synthesis or release of vasodilatory substances might therefore be expected to affect hypoxic vasodilation more than hypercapnic vasodilation. Another differential mechanism is reflex sympathetic stimulation which opposes cerebral vasodilation. If hypercapnia causes less reflex sympathetic stimulation than hypoxia and if ethanol alters sympathetic vascular tone, then chronic ethanol exposure may cause blunting of hypoxic vasodilation, whereas hypercapnic vasodilation is preserved. Finally, activation of ATP-sensitive potassium channels is recognized as an important mediator in the regulation of vascular tone. Taguchi et al.(34) used the potassium channel blocker glibenclamide to attenuate the cerebral vasodilatory response to hypoxia in rabbits. Hypercapnic cerebral vasodilation is believed not to be mediated by activation of potassium channels, and therefore, any ethanol-induced alteration in the development and/or responsivity of potassium channels could affect hypoxic but not hypercapnic cerebral vasodilation.
Maternal alcohol use may indirectly affect developing fetal cerebral blood vessels by causing intermittent fetal hypoxia and/or placental insufficiency. High concentrations of alcohol produce spasms of human umbilical blood vessels; and chronic alcohol consumption causes decreased placental blood flow in rats(11, 35). Repeated brief episodes of ischemia induce striatal damage and sensitize the fetal brain to neuronal loss in sheep(36). Although the moderate early alcohol exposure in our studies did not cause enough placental insufficiency to produce growth retardation or signs of chronic hypoxemia, the exposure may have induced acute intermittent hypoxic/ischemic events early in gestation, which could have impaired cerebral vascular growth and function. Maternal alcohol use may also have indirectly affected developing fetal vessels via the alcohol metabolites, acetaldehyde and acetate. These metabolites have opposite effects on peripheral blood vessels; acetaldehyde acts as a pressor, whereas acetate acts as a vasodilator(8). Thus these metabolites may alter the systemic hemodynamic effects of ethanol, as well as the duration of vascular responses. Furthermore, in developing brain, metabolites may cross an immature or altered blood-brain barrier and directly affect cerebral blood vessels and neurons. Finally, prenatal alcohol exposure may have altered myocardial or carotid body development so that systemic responses to hypoxia were altered. Sterni et al.(37) have shown developmental changes in the intracellular calcium response of carotid chemoreceptor cells to hypoxia, and alcohol could alter these changes. In support of this hypothesis was our observation that ethanol-exposed lambs had no significant increase in heart rate during hypoxia. Development of an abnormal oxygen sensor (carotid chemoreceptors) or abnormal sympathetic or vagal responses could account for this finding.
The lambs in this study were anesthetized with pentobarbital, which depresses baseline CMRo2 and CBF. Newborn cerebral responses to hypoxia and CO2 are not altered by pentobarbital anesthesia, but we cannot be certain whether the same is true for alcohol-exposed newborns(22). Ethanol causes decreased CBF in awake but not pentobarbital-anesthetized dogs(38). It is therefore possible that pentobarbital blunted the CBF responses to hypoxia in alcohol-exposed lambs but not in saline controls; however, this would still suggest that alcohol exposure alters blood vessel tone or reactivity. Another potential problem with our study was the preponderance of females in both study groups. Male fetuses, in general, grow faster prenatally than female fetuses, and therefore each sex may pass through “critical periods” of vulnerability to alcohol exposure at different times(39). However, given the similar percentages of females in both groups, it is unlikely that sex had any influence on differential development of vascular responsivity. Finally, the lambs in the alcohol group were 1 d younger at study than lambs in the saline group. Age could have been a factor in the cerebrovascular differences between the groups, although by an unknown mechanism. Furthermore, there was no significant difference in age when the saline and ethanol groups were compared for the hypoxia protocol.
In conclusion, moderate maternal ethanol infusion early in pregnancy alters neonatal hypoxic, but not CO2, cerebral vascular responses. We speculate that, if fetal hypoxic responses are similarly blunted, then hypoxic brain injury may be one of the mechanisms for maternal alcohol-induced fetal brain damage. It is important to point out, however, that alcohol is rarely used (or abused) alone but rather, in combination with cigarette smoking and/or illicit substance abuse. Our study addresses only the fetal cerebral effects of moderate maternal alcohol exposure alone.
Abbreviations
- CBF:
-
cerebral blood flow
- CVR:
-
cerebrovascular resistance
- Cao2:
-
arterial oxygen content
- CMRo2:
-
cerebral oxygen consumption
- OD:
-
cerebral oxygen delivery
- MAP:
-
mean arterial blood pressure
- Paco2:
-
partial pressure of arterial CO2
- Pao2:
-
partial pressure of arterial O2
References
Abel EL, Sokol RJ 1986 Fetal alcohol syndrome is now leading cause of mental retardation. Lancet 2: 1222
Committee on Substance Abuse 1993 Fetal alcohol syndrome and fetal alcohol effects. Pediatrics 91: 1004–1006.
Barry DI, Hemmingsen R 1984 Cerebral blood flow autoregulation during acute ethanol intoxication in the rat. Acta Pharmacol Toxicol 54: 227–232.
Farago M, Szabo C, Horvath I, Dora E, Kovach AGB 1991 Differential vascular actions of ethanol in feline middle cerebral and mesenteric artery. Acta Physiol Hung 78: 119–125.
Gordon EL, Nguyen T-S, Ngai AC, Winn HR 1995 Differential effects of alcohols on intracerebral arterioles. Ethanol alone causes vasoconstriction. J Cereb Blood Flow Metab 15: 532–538.
Hemmingsen R, Barry DI 1979 Adaptive changes in cerebral blood flow and oxygen consumption during ethanol intoxication in the rat. Acta Physiol Scand 106: 249–255.
Newlin DB, Golden CJ, Quaife M, Graber B 1982 Effect of alcohol ingestion on regional cerebral blood flow. Int J Neurosci 17: 145–150.
Altura BM, Altura BT 1987 Peripheral and cerebrovascular actions of ethanol, acetaldehyde and acetate: relationship to divalent cations. Alcohol Clin Exp Res 11: 99–111.
Backman C, Granholm A-C 1992 Effects of ethanol on development of dorsal rache transplants in oculo: a morphological and electrophysiological study. J Comp Neurol 320: 136–144.
Mayhan WG 1992 Responses of cerebral arterioles during chronic ethanol exposure. Am J Physiol 262:H787–H791.
Altura BM, Altura BT, Carella A, Chatterjee M, Halevy S, Tejani N 1983 Alcohol produces spasms of human umbilical blood vessels: relationship to fetal alcohol syndrome. Eur J Pharmacol 86: 311–312.
Falconer J 1990 The effect of maternal ethanol infusion on placental blood flow and fetal glucose metabolism in sheep. Alcohol Alcohol 25: 413–416.
Gleason CA, Hotchkiss KJ 1992 Cerebral responses to acute maternal alcohol intoxication in immature fetal sheep. Pediatr Res 31: 645–648.
Richardson BS, Patrick JE, Bousquet J, Homan J, Brien JF 1985 Cerebral metabolism in fetal lamb after maternal infusion of ethanol. Am J Physiol 249:R505–R509.
Detering N, Collins RM, Hawkins RL, Ozand PT, Karahasan AM 1980 The effects of ethanol on developing catecholamine neurons. Adv Exp Med Biol 132: 721–727.
Gallant DM 1987 Ethanol effects on fetal cerebral cortex. Alcohol Clin Exp Res 11: 190
Mhatre M, Ticku MK 1994 Chronic ethanol treatment up-regulates the GABA receptor β sub unit expression. Mol Brain Res 23: 246–252.
Miller MW 1986 Effects of alcohol on the generation and migration of cerebral cortical neurons. Science 233: 1308–1311.
Heymann MA, Payne BD, Hofmann JIE, Rudolph AM 1977 Blood flow measurements with radionuclide-labeled particles. Prog Cardiovasc Dis 20: 55–79.
Rosenberg AA, Jones MD Jr, Traystman RJ, Simmons MA, Molteni RA 1982 Response of cerebral blood flow to changes in PCO2 in fetal, newborn and adult sheep. Am J Physiol 242:H862–H866.
Nolan WF, Davies DG 1982 Brain extracellular fluid pH and blood flow during isocapnic and hypocapnic hypoxia. J Appl Physiol 53: 247–252.
Donegan JH, Traystman RJ, Koehler RC, Jones MD Jr, Rogers MC 1985 Cerebrovascular hypoxic and autoregulatory responses during reduced brain metabolism. Am J Physiol 249:H421–H429.
Jones MD Jr, Traystman RJ, Simmons MA, Molteni RA 1981 Effects of changes in arterial O2 content on cerebral blood flow in the lamb. Am J Physiol 240:H209–H215.
Cumming ME, Ong BY, Wade JD, Sitar DS 1984 Maternal and fetal ethanol pharmacokinetics and cardiovascular responses in near-term pregnant sheep. Can J Physiol Pharmacol 62: 1435–1439.
Pietrantoni M, Knupple RA 1991 Alcohol use in pregnancy. Clin Perinatol 18: 93–101.
Walpole I, Zubrick S, Pontre J 1990 Is there a fetal effect with low to moderate alcohol use before or during pregnancy?. J Epidemiol Commun Health 44: 297–301.
Helou SM, Hudak ML, Jones MD Jr 1991 Cerebral blood flow responses to hypercapnia in immature fetal sheep. Am J Physiol 261:H1366–H1370.
Massik J, Jones MD Jr, Miyabe M, Tang U-L, Hudak ML, Koehler RC, Traystman RJ 1989 Hypercapnia and response of cerebral blood flow to hypoxia in newborn lambs. J Appl Physiol 66: 1065–1070.
Gleason CA, Hamm C, Jones MD Jr 1990 Effect of acute hypoxemia on brain blood flow and oxygen metabolism in immature fetal sheep. Am J Physiol 258:H1064–H1069.
Kurth CD, Wagerle LC 1992 Cerebrovascular reactivity to adenosine analogues in 0.6-0.7 gestation and near-term fetal sheep. Am J Physiol 262:H1338–H1242.
Busija DW 1984 Sympathetic nerves reduce cerebral blood flow during hypoxia in awake rabbits. Am J Physiol 247:H446–H451.
Hayashi S, Park MK, Kuehl TJ 1984 Higher sensitivity of cerebral arteries isolated from premature and newborn baboons to adrenergic and cholinergic stimulation. Life Sci 35: 253–260.
Siesjo BK 1976 Brain Energy Metabolism. Wiley, New York
Taguchi H, Heistad D, Kitazano T, Faraci FM 1994 ATP-sensitive K+ channels mediate dilation of cerebral arterioles during hypoxia. Circ Res 74: 1005–1008.
Jones PJH, Leichter J, Lee M 1981 Placental blood flow in rats fed alcohol before and during gestation. Life Sci 29: 1153–1159.
Mallard EC, Williams CE, Gunn AJ, Gunning MI, Gluckman PD 1993 Frequent episodes of brief ischemia sensitize the fetal brain to neuronal loss and induce striatal injury. Pediatr Res 33: 61–65.
Sterni LM, Bamford OS, Tomares SM, Montrose MH, Carroll JL 1995 Developmental changes in intracellular Ca2+ response of carotid chemoreceptor cells to hypoxia. Am J Physiol 268:L801–L808.
Friedman HS, Lowery R, Archer M, Shaughnessy E, Scorza J 1984 The effects of ethanol on brain blood flow in awake dogs. J Cardiovasc Pharmacol 6: 344–348.
Lieberman L 1982 Normal and abnormal sexual dimorphic patterns of growth and development. In: Hall RL (ed) Sexual Dimorphism in Homo sapiens. Praeger Publishers, New York, pp 263–312.
Acknowledgements
The authors thank Debbie Flock, Ann Biser-Rohrbaugh, and George Kuck for their expert technical assistance and Karen Lingerman and Maureen Maffey for excellent secretarial support.
Author information
Authors and Affiliations
Additional information
Supported, in part, by National Institutes of Health Grant NS-20020 and by the Hospital for the Consumptives of Maryland (Eudowood).
Rights and permissions
About this article
Cite this article
Gleason, C., Iida, H., Hotchkiss, K. et al. Newborn Cerebrovascular Responses after First Trimester Moderate Maternal Ethanol Exposure in Sheep. Pediatr Res 42, 39–45 (1997). https://doi.org/10.1203/00006450-199707000-00007
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199707000-00007
This article is cited by
-
Investigation of circle of Willis variants and hemodynamic parameters in twins using transcranial color-coded Doppler sonography
The International Journal of Cardiovascular Imaging (2018)
-
Effects of l-glutamine supplementation on maternal and fetal hemodynamics in gestating ewes exposed to alcohol
Amino Acids (2014)