Abstract
The objective of the present study was to determine the characteristics of Doppler flow velocity wave forms in branch pulmonary arteries in relation to gestational age. A total of 111 singleton normal pregnancies were studied during the second half of pregnancy using a combined color-coded Doppler and two-dimensional real-time ultrasound system. Pulsed Doppler measurements of the most proximal branch of the right or left pulmonary artery were attempted during fetal apnea from a transverse cross-section of the fetal chest at the level of the cardiac four-chamber view after visualization with color Doppler. The success rate in obtaining the pulmonary arterial wave form was 85%. The wave form displayed a rapid systolic velocity acceleration, followed by an initially rapid but then more gradual velocity deceleration which was interrupted in most cases by a short reversed flow interval at the beginning of the diastolic phase of the cardiac cycle. The diastolic phase was characterized by forward flow. Peak systolic, end-diastolic and time-averaged velocity, pulsatility index, and systolic integral remained constant during gestation. Changes in vessel diameter or compliance may play a role in this. A gestational age-dependent rise was established for peak diastolic velocity, diastolic integral, and early peak diastolic reverse flow, whereas a gestational age-determined decline was found for the peak systolic/peak diastolic ratio. Fetal heart rate demonstrated a statistically significant increase relative to gestational age. However, the observed relation between the flow velocity wave form parameters, pulsatility index calculations, and gestational age was independent of fetal heart rate. It is speculated that peak diastolic velocity, diastolic integral, and peak systolic/peak diastolic ratio rather than the pulsatility index are useful in detecting gestational age-related changes in human fetal pulmonary vascular resistance.
Similar content being viewed by others
Main
Studies on fetal lambs have demonstrated that pulmonary flow increases and pulmonary vascular resistance decreases with advancing gestational age(1). However, when corrected for wet weight of the lungs, pulmonary blood flow does not change, and total pulmonary resistance even increases with advancing gestation(2).
The use of combined two-dimensional real-time and color-coded Doppler systems has provided a host of information on the early and late human fetal systemic circulation(3, 4). It has been demonstrated that the normally developing fetus during the second half of gestation is characterized by a low fetoplacental vascular resistance with well defined and reproducible arterial, cardiac, and venous flow velocity wave forms(5).
Lately, data have become available on Doppler velocimetry in the human fetal pulmonary circulation, which is mainly due to the introduction of more sensitive color-coded Doppler systems(6–8). In the present cross-sectional study we addressed the characteristics of branch pulmonary artery flow velocity wave forms in the human fetal lung during the second half of pregnancy. This information may contribute to our understanding of the normal fetal pulmonary circulation and of hemodynamic changes underlying structural pathology such as lung hypoplasia(9).
METHODS
Study design. During a period of 24 mo, a total of 111 nonsmoking women with a normal singleton pregnancy consented to participate in a cross-sectional study design. All women were recruited from the routine antenatal clinic of the Department of Obstetrics and Gynaecology of the University Hospital Rotterdam-Dijkzigt. The study protocol was approved by the Hospital Ethics Committee. Gestational age at entering the study ranged between 20 and 40 wk (median 30 wk), and maternal age varied between 18 and 46 y (median: 28 y). Pregnancy duration was determined from the last reliable menstrual period and confirmed or adjusted by ultrasonic measurement of the fetal crown-rump length (8-12 wk) or fetal biparietal diameter (12-20 wk). None of these pregnancies was associated with congenital anomalies, including lung pathology. All pregnancies were uneventful with normal fetal biometry and normal amniotic fluid volumes. As expected, 80% of the fetal birth weights was situated between the 10th and 90th centile according to the Kloosterman tables, adjusted for maternal parity and fetal sex(10). Women were selected according to 10 gestational age subgroups (20-22,..., 38-40 wk), to guarantee a homogeneous distribution. Each woman was included in the study only once.
Recording technique. Ultrasound Doppler studies were performed using a Toshiba SSH 140 with combined transabdominal real-time and color Doppler imaging facilities (Toshiba Corp., Medical Systems Division, Tokyo, Japan). The Doppler carrier frequency was 5 MHz. The spatial peak temporal average power output was less than 100 mW/cm2 in both imaging and Doppler modes according to manufacturer's specifications.
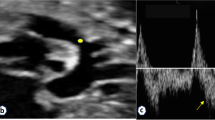
After obtaining a clear sonographic transverse cross-section of the fetal chest at the level of the cardiac four-chamber view, color Doppler was switched on to visualize the pulmonary circulation. Depending on fetal position, the pulsed Doppler sample volume (0.1-0.3 cm) was placed over the most proximal branch of the right or left pulmonary artery. The angle between the Doppler cursor and the assumed blood flow direction was always kept below 20 °. The high pass filter was set at 70 Hz. Recordings were performed with the subject in the semirecumbent position and during fetal apnea, because the latter may modulate the flow velocity wave form(11).
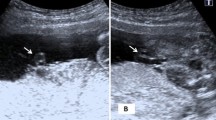
All flow velocity wave forms were recorded on hard copies. Wave form analysis was performed by one examiner (J.A.M.L.) using a microcomputer(Olivetti M24; Olivetti BV, Leiden, The Netherlands) linked to a graphics tablet. Branch pulmonary artery flow velocity wave forms (Fig. 1) are characterized by a rapid systolic velocity acceleration, followed by an initially rapid but later more gradual velocity deceleration, which in most instances is interrupted by a short reverse flow component at the beginning of the diastolic phase of the cardiac cycle(6, 9). Although slight variations in the wave form morphology were observed, these were not essentially different from the wave form demonstrated in Figure 1. In all women forward flow could be observed during the remainder of the diastolic phase of the branch pulmonary artery velocity wave form(9).
Three consecutive flow velocity wave forms with the highest velocity and of similar appearance were used to calculate the different parameters in each vessel. For each woman the mean value of the following wave form parameters was determined (Fig. 1): 1) PSV (cm/s), PDV(cm/s), EDV (cm/s), and TAV (cm/s); 2) S/D ratio; 3) RV(cm/s); 4) PI = (PSV - EDV)/TAV), according to Gosling and King(12); and 5) systolic and diastolic velocity integral (cm).
Statistical analysis. For the construction of reference centiles (P5, P50, and P95), the method described by Royston(13) was used and, if necessary, the SD was modeled as a function of gestational age as described by Altman(14). We tested for significant regression. If it was significant, the 50th centile(P50) was established by modeling the outcome variable, y, by a straight line regression model with gestational age as predictor. Further, it was tested whether adding the quadratic term was significant or whether the distribution of y depending on gestational age was skewed. If the regression was not significant, the 50th centile was established by using the mean of the outcome variable y. Next, it was checked if the residuals depended on gestational age. If so, straight line regression was used to model the absolute value of the residuals, and from this model a regression equation for the SD, depending on gestational age, was derived. Using this SD, the 5th (P5) and 95th (P95) centile were constructed. Also tested was whether the relation between the outcome variable y and gestational age was influenced by FHR by adding FHR in the regression model.
Left and right branch pulmonary artery flow velocity wave forms were compared using the t test. The level of statistical significance was set at p < 0.05.
RESULTS
Technically acceptable flow velocity wave forms were collected in 94 out of 111 women, resulting in a success rate of 85%. Recording failures were determined by fetal breathing movements, unfavorable fetal position, or maternal obesity. There was no relationship between the recording failures and the left or right lung or gestational age, although recording failures seem to occur slightly more often after 35 wk of gestation due to fetal breathing movements. The median gestational age at delivery was 40 wk (36-42 wk), and the median birth weight was 3190 g (1930-4760 g).
Regression slopes defining the relation between branch pulmonary artery velocity parameters and gestational age (5th, 50th, and 95th centiles) are presented in Table 1. A statistically significant increase with advancing gestational age was found for PDV (p < 0.0001; Fig. 2) and diastolic integral (p < 0.05; Fig. 3), whereas a statistically significant gestational age-related decrease was demonstrated for the S/D ratio(p < 0.0001; Fig. 4). RV was noted in 91(97%) out of 94 women. Maximum RV revealed a statistically significant increase with advancing gestational age (p < 0.0001;Fig. 5). Pregnancy duration in the three women with absent RV ranged between 20 and 23 wk. No statistically significant gestational age-related change existed for the TAV, PSV, and EDV velocity, PI (Fig. 6), and systolic integral.
In our study group FHR demonstrated a statistically significant increase(p < 0.04) in relation to advancing gestational age. However, the observed relation between the flow velocity wave form parameters, PI calculations, and gestational age was independent of FHR.
In nearly all cases, left and right branch pulmonary artery flow velocity wave forms were not obtained from the same patient. When separating left(n = 37) and right (n = 57) branch pulmonary flow velocity wave forms, no statistically significant mean differences were observed for any of the flow velocity parameters studied.
DISCUSSION
The present study describes characteristics of the human fetal branch pulmonary artery flow velocity wave form during the second half of normal pregnancy. The total complement of pulmonary arterial and venous branch vessels, which is formed in the pre-acinar region of the lung, is attained by 20 wk of gestation(15).
The human fetal pulmonary artery velocity wave form obtained from the most proximal branch of the left or right pulmonary artery displays a unique Doppler wave form pattern characterized by a rapid initial flow acceleration phase and an equally rapid deceleration phase, producing a needle-shaped systolic peak. This is followed by a more gradual decline in flow velocity, which in nearly every instance is interrupted by a short reverse flow pattern at the beginning of diastole(6). Forward flow was observed throughout the remainder of diastole(9). The latter is at variance with pulmonary artery flow velocity wave form recordings in the fetal lamb, which are characterized by absent end-diastolic flow(16). This may be due to the invasive recording techniques applied in fetal lamb studies or anatomical differences between lamb and human subjects. However, also in the human fetus, different descriptions of end-diastolic flow in the branch pulmonary artery have been given. Although we observed forward flow during end-diastole, absent end-diastolic flow was reported by Emerson and Cartier(6), and present or absent forward end-diastolic flow was established by Rasanen et al.(8). One explanation for these somewhat different findings could be the setting of the high pass filter, which was lower in our recording equipment (70 Hz) than in the study by Rasanen et al.(8) (100 Hz), but not reported in the study by Emerson and Cartier(6).
The physical basis for the shape of the fetal branch pulmonary artery flow velocity wave form remains speculative and is probably determined by several factors, such as vascular pressure, resistance, impedance, and ventricular contractility(6). Most of our knowledge of the fetal pulmonary circulation is derived from fetal lambs(1, 16). Blood flow through the lungs is low during fetal life, which has been explained on the basis of a high pulmonary vascular resistance. Flow velocity profiles have been recorded in pulmonary arteries of fetal lambs by chronically implanted cuff-type electromagnetic flow transducers(16). These profiles show forward flow with a sharp peak early in systole with almost no flow during mid-systole, and with reverse flow during late systole and early diastole; throughout the remainder of diastole there is no significant forward or backward flow. This velocity pattern, which partly resembles the profile found in our study, has been explained on the basis of a high (relative to systemic) pulmonary vascular resistance and the presence of a patent ductus arteriosus(16, 17). During early systole, blood is ejected at high velocity through the pulmonary arterial circulation. As velocity falls, blood passes preferentially through the ductus arteriosus into the descending aorta. Because pulmonary vascular resistance is high, reverse flow is recorded as blood flow from the branch pulmonary arteries through the ductus arteriosus in association with elastic recoil of these vessels(17, 18). A late systolic to early diastolic reversal of flow, coming from the ductus arteriosus and increasing with gestational age, has previously been demonstrated in the human fetal aortic isthmus(19). This would suggest that an open ductus arteriosus will also permit pressure and flow changes in the systemic circulation to affect the pulmonary velocity profile.
The present study revealed no significant change in TAV, PSV, and EDV with advancing gestational age. Similar findings were done by Stanley et al.(20) for PSV in the right pulmonary artery of normally developing human fetuses. Changes in vessel diameter and/or compliance may play a role in velocity parameters, such as TAV, PSV, and EDV remaining constant in the present study. The presence of elastic tissue in the proximal half of the preacinar airway may also be responsible for this observation because of the high tensile strength which counteracts the distending tendency of blood pressure and maintains the patency of the pulmonary arterial vessels(21). Because we did not measure pulmonary vessel area, no information is available on volume flow. In the fetal lamb, the absolute total rise of pulmonary blood flow(1, 22), has been attributed to the expansion of the total cross-sectional pulmonary vascular bed with advancing gestational age(23).
The regulation of fetal pulmonary flow depends on the high resistance of the pulmonary vasculature. A low total cross-sectional pulmonary vascular area appears to be the major factor determining the high vascular resistance(6, 24). During fetal life, the wall thickness of the muscular and partially muscular pulmonary arteries is considerable, and the lumen is small(21). In the human fetus pulmonary artery, wall thickness is twice that in the adult, which results in a relatively high pulmonary vascular resistance to maintain reduced lung blood flow during fetal life(21). Fetal lamb studies revealed a decrease of pulmonary vascular resistance with advancing gestational age(17, 18, 22). Levin et al.(23) demonstrated in the fetal lamb that increased pulmonary blood flow and decreased vascular resistance with advancing gestational age are due to a rise in the total number of vessels and vasomotor activity is related to an increase in total amount of smooth muscle whereas the muscle thickness in individual vessels remains constant.
Of interest is, however, that, when corrected for wet weight of the lungs, pulmonary artery flow remains constant and total pulmonary vascular resistance rises(2). This suggests that the rising pulmonary artery flow does not keep pace with the increase in pulmonary vascularity(6).
In the present study, the PI, which at fetal trunk and placental level has been used as a measure of downstream impedance, remained constant. This is in contrast the results of Rasanen et al.(8), who attributed a drop in branch pulmonary artery PI up to 34-35 wk of gestation to a reduction in pulmonary vascular resistance. However, recently the same group(25) reported that weight-indexed pulmonary vascular resistance appears to increase after 30 wk of gestation, which is consistent with fetal lamb data. As in our study, Emerson and Cartier(6) failed to identify a fall in downstream impedance in the high resistance pulmonary circuit. They proposed that this was due to insensitivity of the PI to small changes in resistance, rather than the constancy of the resistance in the fetal pulmonary circulation. We were able to establish significant gestational age-related changes in the diastolic component of the branch pulmonary artery wave form. Both the PDV and diastolic integral displayed a significant increase with advancing gestational age, whereas S/D ratio showed a significant decrease, suggesting reduced pulmonary vascular resistance.
An approximately 2.5-fold increase was established for RV, which probably represents the preferential escape of blood from the branch pulmonary arteries through the ductus arteriosus into the descending aorta(17, 18). The increase in RV, therefore, may be the result of diminishing arterial downstream impedance at lower body and placental level, but also at the level of the upper body and brain(19). Comparison with other data(8) was possible for the PSV and PI; a similar scatter was observed.
It can be concluded that technically acceptable flow velocity wave forms can be obtained from human fetal branch pulmonary arteries during the second half of gestation applying combined color-coded and pulsed Doppler techniques. Changes in vessel diameter and/or compliance may play a role in the constancy of TAV, PSV, and EDV in branch pulmonary arteries. We speculate that the measurement of PDV, diastolic integral, and S/D ratio rather than the PI is useful in detecting gestational age-related changes in human fetal pulmonary vascular resistance. The clinical implications of these findings will be investigated in relation to pathologic conditions such as lung hypoplasia.
Abbreviations
- PSV:
-
peak systolic velocity
- PDV:
-
peak diastolic velocity
- EDV:
-
end diastolic velocity
- TAV:
-
time-averaged velocity
- S/D ratio:
-
peak systolic/peak diastolic ratio
- RV:
-
early peak diastolic reverse flow velocity
- PI:
-
pulsatility index
- FHR:
-
fetal heart rate
References
Rudolph AM, Heymann MA 1970 Circulatory changes during growth in the fetal lamb. Circulation Res 26: 289–299.
Morin FC, Egan EA 1992 Pulmonary hemodynamics in fetal lambs during development at normal and increased oxygen tension. J Appl Physiol 21: 163–184.
Van Splunder P, Huisman TWA, de Ridder MAJ, Wladimiroff JW 1996 Fetal venous and arterial flow velocity wave forms between eight and twenty weeks of gestation. Pediatr Res 40: 158–162.
Groenenberg IAL, Wladimiroff JW, Hop WCJ 1989 Fetal cardiac and peripheral arterial flow velocity wave forms in intrauterine growth retardation. Circulation 81: 1711–1717.
Hecher K, Campbell S, Doyle P, Harrington K, Nicolaides K 1995 Assessment of fetal compromise by Doppler ultrasound investigation of the fetal circulation. Circulation 91: 129–138.
Emerson DS, Cartier MS, 1995 The fetal pulmonary circulation. In: Copel JA and Reed KL (eds) Doppler Ultrasound in Obstetrics and Gynecology. Raven Press, New York, pp 307–323.
Laudy JAM, Huisman TWA, de Ridder MAJ, Wladimiroff JW 1995 Normal fetal pulmonary venous blood flow velocity. Ultrasound Obstet Gynecol 6: 277–281.
Rasanen J, Huhta JC, Weiner S, Wood DC, Ludomirski A 1996 Fetal branch pulmonary arterial vascular impedance during the second half of pregnancy. Am J Obstet Gynecol 174: 1441–1449.
Laudy JAM, Gaillard JLJ, vd Anker JN, Tibboel D, Wladimiroff JW 1996 Doppler ultrasound imaging: a new technique to detect lung hypoplasia before birth? A case report. Ultrasound Obstet Gynecol 7: 189–192.
Kloosterman G 1970 On intrauterine growth. Int Gynecol Obstet 8: 895–912.
Marsˇal K, Lindblad A, Lingman G 1984 Blood flow in the fetal descending aorta; intrinsic factors affecting fetal blood flow, i.e. fetal breathing movements and cardiac arrhythmia. Ultrasound Med Biol 10: 339–348.
Gosling RG, King DH 1975 Ultrasound angiology. In: Marcus AW, Adamson J (eds) Arteries and Veins. Churchill-Livingstone, Edinburgh, pp 61–98.
Royston P 1991 Constructing time-specific reference ranges. Stat Med 10: 675–690.
Altman D 1993 Constructing of age-related reference centiles using absolute residuals. Stat Med 12: 917–924.
Inselman LS, Mellins RB, 1981 Growth and development of the lung. J Pediatr 98: 1–15.
Lewis AB, Heymann MA, Rudolph AM 1976 Gestational changes in pulmonary vascular responses in fetal lambs in utero. Circulation Res 39: 536–541.
Rudolph AM 1979 Fetal and neonatal pulmonary circulation. Annu Rev Physiol 41: 383–395.
Rudolph AM 1977 Fetal and Neonatal pulmonary circulation. Am Rev Respir Dis 115: 11–18.
Fouron JC, Zarelli M, Drblik SP, Lessard M 1994 Flow velocity profile of the fetal aortic isthmus through normal gestation. Am J Cardiol 74: 483–486.
Stanley JR, Veille JC, Zaccaro D 1994 Description of right pulmonary artery blood flow by Doppler echocardiography in the normal human fetus from 17 to 40 wk of gestation. J Matern Fetal Invest 4:S14.
Hislop A, Reid L 1972 Intra-pulmonary arterial development during fetal life-branching pattern and structure. J Anat 113: 35–48.
Rudolph AM 1974 The pre- and postnatal pulmonary circulation. In: Congenital Diseases of the Heart. Yearbook Medical Publishers, Chicago, pp 29–48.
Levin DL, Rudolph AM, Heymann MA, Phibbs RH 1976 Morphological development of the pulmonary vascular bed in fetal lambs. Circulation 53: 144–151.
Long W 1990 Development pulmonary circulatory physiology. In: Long W (eds) Fetal and Neonatal Cardiology. WB Saunders, Philadelphia, pp 76–95.
Rasanen J, Wood DC, Weiner S, Ludomirski A, Huhta JC 1996 Role of the pulmonary circulation in the distribution of human fetal cardiac output during the second half of pregnancy. Circulation 94: 1068–1073.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Laudy, J., De Ridder, M. & Wladimiroff, J. Doppler Velocimetry in Branch Pulmonary Arteries of Normal Human Fetuses during the Second Half of Gestation. Pediatr Res 41, 897–901 (1997). https://doi.org/10.1203/00006450-199706000-00016
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199706000-00016
This article is cited by
-
Pulmonary vascular reactivity in growth restricted fetuses using computational modelling and machine learning analysis of fetal Doppler waveforms
Scientific Reports (2024)
-
Advanced dynamic Doppler flow of the pulmonary artery in a normal population: reference values from 18 to 41 weeks of gestation calculated by automatic Doppler waveform analysis
Archives of Gynecology and Obstetrics (2014)