Abstract
We studied the effect of maternal concentration and mode of administration on transfer rate of TSH-releasing hormone (TRH) in an in vitro model of dually perfused isolated lobule of human term placenta. Varying concentrations (4-40 μg dL-1) of TRH were added either to the open maternal circulation to mimic an infusion or as a single bolus dose to the closed maternal circulation. TRH was measured by RIA. Perfusion efficienty in each experiment was determined by using antipyrine and creatinine as diffusable markers. At a concentration equivalent to the usual clinical dose of 400 μg, transplacental transfer of TRH was 0.4 ± 0.1%, with an fetal/maternal ratio of 0.01 ± 0.003. Placental clearance rate(y = 0.07x; R2 = 0.97; p < 0.001; n = 28) and uptake of TRH (y = 0.40x; R2 = 0.95; p < 0.001) in the closed experiments increased exponentially with increasing maternal concentration. Placental clearance (y = 0.05x; R2 = 0.99;p < 0.001; n = 30), and uptake of TRH (y = 0.35x; R2 = 0.98; p < 0.01) under steady state also correlated with maternal TRH concentration. For a given concentration, placental clearance and uptake of TRH was comparable whether given as a bolus or an infusion. We conclude that TRH is transferred sparingly across the human term placenta and its transfer rate is a function of the maternal concentration of TRH and not its mode of administration.
Similar content being viewed by others
Main
TRH, is a tripeptide with a molecular weight of 330(1, 2). In obstetric practice, maternal administration has been shown to stimulate the release of fetal TSH and production of thyroid hormones(3–6). By virtue of this property TRH has been used with glucocorticoids to enhance the synthesis and secretion of surfactant from the fetal lung(7–10). Although initial trials showed promising beneficial effects, recent meta analysis of randomized trials of maternally administered TRH shows conflicting results in terms of efficacy against respiratory distress syndrome(7–13). Although the reason for this is not known, it is plausible that use of different dosage regimens and mode of administration may be responsible. Whereas most studies used 400 μg of TRH, the largest trial and a preliminary report using the lower 200-μg dose(12, 13) failed to show beneficial effects on fetal lung maturation. This raises the possibility that the fetal thyrotrophic response to maternal TRH is dose-dependent.
We hypothesized that dose and mode of administration of TRH might influence the extent of fetal exposure. Certainly stimulation of the adult pituitary gland by TRH is known to occur in a dose-dependent manner(14, 15). Second, as fetal endogenous levels of TRH are higher(16) than those in the mother, it seems likely that transplacental TRH passage may depend upon maternal concentration,i.e. the higher the maternal concentration, the greater the transfer. Third, the recent observation that human placenta constitutes an enzymatic barrier to free passage of TRH(17) further suggests that its placental transfer rate is likely to increase with increasing maternal concentrations. The mode of administration of a drug can influence the net placental flux by altering the effective plasma concentration. This may be especially important in relation to TRH, which has a short half-life of 5.5 min(1, 2). Although little is known about the pharmacokinetics of TRH during pregnancy, the maternal concentration when given i.v. as a bolus would be expected to decline rapidly to baseline values within 5 min of its administration. In contrast, administration at a constant rate by slow infusion should maintain the transplacental concentration gradient of TRH throughout the infusion, to allow transplacental transfer over a more prolonged period.
To test the hypothesis that the dose and the mode of administration of TRH can influence its net transfer across the placental, we undertook a series of experiments where varying concentrations of TRH were added to the open(infusion) or closed (bolus) maternal circulation of an in vitro model of perfused human term placenta.
METHODS
Analytical grade TRH, creatinine, and TC-199 perfusion media were purchased from Sigma Chemical Co. (Poole, Dorset, UK). All other reagents and chemicals were of analytical grade and obtained from BDH (Leicestershire, UK).
Placental Perfusion Technique
Placentae were obtained immediately after vaginal or cesarean deliveries between 37 and 42 wk of gestation. Perfusion of the isolated lobule was commenced within 5 min at 37 °C under optimal physiologic conditions of oxygenation, pressure, flow, osmotic pressure, and acid/base status(18). Both open and closed circuit experimental designs were used as described previously(19).
Closed circuit experiments. In these experiments, both maternal and fetal perfusates were recirculated. Autologous maternal blood from the intervillous space and fetal blood from the cord vessels was collected(18), centrifuged and blood cells washed and resuspended in the perfusate. The maternal and fetal perfusates consisted of modified TC-199 medium(17–19) with washed autologous maternal and cord red blood cells, respectively. Bovine albumin(0.5 g L-1) was added to the perfusate to maintain colloid-osmotic pressure across the placental membrane. Closed circuit perfusion of the fetoplacental circulations was established by cannulating a chorionic artery and vein. The fetal arterial perfusion pressure was 24-30 mm Hg, and venous outflow ranged between 6 and 9 mL min-1. The fetal circulatory volume was 110-125 mL. The maternal-placental circulation was established by placing five cannulae in the intervillous space. The maternal arterial perfusion pressure was 12-16 mm Hg, and venous flow rate was set at 24 mL min-1. The maternal circulating volume was between 140 and 160 mL. Maternal and fetal perfusates had median hematocrit values of 5 (range 3-9) and 10 (range 4-22), respectively. Tissue oxygenation was maintained throughout the experiment by oxygenating the maternal circulation with 95% oxygen and 5% carbon dioxide. Perfusion efficiency and diffusional transfer rate was determined in each experiment by measuring the rate of trasplacental transfer of creatinine as a freely diffusable marker. Experiments were considered valid only when the maternal to fetal transfer of creatinine had fallen at the end of 2 h to within the predefined range of 8-16% of the initial dose(20). Experiments were discarded if fetal perfusion pressure increased by 10 mm Hg or when there was a shift in fetal circulating volume across the placental membrane in excess of 5 mL.
TRH and creatinine were added to the closed maternal circulation as a single bolus dose to attain drug concentrations of 8 μg dL-1 and 20 mg dL-1, respectively (n = 7). This dose of TRH was selected to mimic a clinically administered 400-μg dose. This was calculated based on the total blood volume in normal pregnancy after 30 wk being approximately 5 L and maternal circulating volume in our system 150 mL.
The effect of maternal concentration on transfer and uptake of TRH by the perfused placental lobule was studied over the concentration range of 4(n = 6), 16 (n = 5), 20 (n = 5), and 40 μg dL-1 (n = 5). These concentrations were chosen because 4 and 8 μg dL-1 are equivalent to clinically administered 200- and 400-μg doses, whereas 16, 20, and 40 μg dL-1 were used to study the effect of increasing concentration.
Open circuit experiments. In open circuit experiments, neither the maternal nor fetal perfusate was recirculated. The maternoplacental and fetoplacental circulations were established as for closed circuit experiments with comparable perfusion pressure and flow rate. The following modifications were made: 1) both maternal and fetal perfusates were non-blood-based, comprising tissue culture media TC-199, as in the closed circuit experiments except that 16 g L-1 instead of 4 g L-1 dextran 60 was added to maintain colloid osmotic pressure across the membrane and 2) the fetal circulation was also oxygenated. A known concentration of TRH (4-200 μg dL-1) along with 30 mg dL-1 antipyrine and creatinine were added to the maternal perfusate. This experimental design had the advantage that a known concentration of TRH can be delivered to the placenta throughout the experiment, thus mimicking administration of TRH as an i.v. infusion. The protein concentration was similar to that of the closed circuit experiments.
The effect of maternal concentration on transfer and uptake of TRH by the placenta was studied over the concentration range as for closed circuit experiments. Four experiments were undertaken for each concentration except for 4 μg where six experiments were performed.
Experiment protocol. Two milliliters of maternal and fetal samples were collected in closed circuit experiments at 15-min intervals for 2 h, whereas in open circuit experiments, both maternal and fetal venous efflux were sampled at 5-min intervals. Samples were centrifuged (3000 ×g, 15 min) and plasma stored at -20 °C for subsequent assay of TRH, antipyrine, and creatinine.
At the end of the perfusion period, both circuits were drained, and their volumes were measured. The perfused lobule was excised, pressure blotted to remove the perfusate from the intervillous space, and stored at -20 °C for subsequent analysis.
Placental uptake of TRH was measured by homogenizing the perfused placental tissue in an Ultraturrax high speed homogenizer in 300-400 mL of PBS buffer. Ten-milliliter aliquots of the homogenized tissue were centrifuged (3000× g, 15 min), and the concentration of TRH in the supernatant was measured.
In closed circuit experiments, the maternal and fetal concentrations of TRH were expressed as percentages of the initial dose added after correction for background activity, circuit volume, and the amount removed from previous sampling. In open circuit experiments all values are expressed as concentration of TRH in nanograms mL-1. In both experimental designs, the concentration in the perfused placental tissue was expressed as the percentage of the initial drug added to the maternal circulation.
Analytical Methods
RIA of TRH. The concentration of TRH in maternal, fetal, and placental tissue was quantified by using an antisera raised in male New Zealand White rabbits against synthetic TRH conjugate prepared by the bisdiazotized benzidine method(21) and was obtained as a gift from the MRC Unit for Reproductive Medicine, Edinburgh, UK. Briefly, the assay buffer was 0.04 mol/L disodium phosphate/monosodium phosphate, pH 7.4, containing 1% (wt/vol) human serum albumin. A 100-μL aliquot of the sample was incubated with 100 μL of antisera and 100 μL of radiolabeled TRH (12 000 cpm 0.1 mL-1) overnight at 4 °C. The final dilution of the antisera used in RIA was 1:5000. Radiolabeled ligand was obtained from DuPont (Stevenage, Hertfordshire, UK) with a specific activity of 4395μCi·μg-1 and >99% pure on reverse phase HPLC. The bound from free fraction was separated by adding 5 volumes of ice-cold ethanol followed by immediate mixing and centrifugation at 1500 rpm, 15 min. Under these RIA conditions, the lower limit of detection was 10 pg in a 300 μL of ethanol extract. Cross-reaction of the TRH analogue, His-Pro-NH2, p-Glu-Pro, p-Glu-His, p-Glu-His-Pro with anti-TRH antibody was consistently<0.0001%. The mean recovery of nonradioactive TRH from serum and tissue extract over the concentration range 10 to 5000 pg was >95%. The mean coefficients of variation for different TRH concentrations in sera and tissue extract were 2.5-12.7%. The mean interassay coefficient of variation of TRH was 10%.
Creatinine assay. Creatinine concentration was determined by colorimetric assay(22), with a coefficient of variation of 7-12%.
Antipyrine assay. The concentration of antipyrine was measured spectrophotometrically(23) with a coefficient of variation of 10-14%.
Data Analysis
All values were expressed as mean ± SEM unless otherwise indicated. A t test was used to compare data between groups. p values<0.05 were considered significant. Equilibrium between maternal and fetal circuits was determined when fetal/maternal ratios of the drug levels were close to unity. Integrated values of maternal (MAUC) and fetal (FAUC) concentration of drug were calculated by the trapezoidal rule(18). The placental permeability coefficient of TRH was calculated as: PS = n/(wt of the placenta) ×[Cm-Cf]dt mL min-1 g-1, where n = fetal concentration at 120 min, [Cm-Cf]dt is integrated concentration difference across the placenta. The clearance of TRH in closed circuit experiments was determined from the slope of a weighted line for the standard deviations of means of the fetal concentration of TRH between 15 and 120 min(17). The clearance rate of TRH under steady state was calculated as (FV - FA) × fetal flow rate/maternal arterial concentration; where FV = fetal venous concentration; FA = fetal arterial concentration.
RESULTS
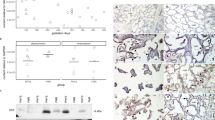
When 4 μg dL-1 TRH was added to the closed maternal circulation, maternal levels decreased rapidly from 100% at 0 min to 20.5 ± 1.4% at 120 min, as shown in Figure 1A. Fetal concentration increased linearly from undetectable levels at 0 min, to 0.2 ± 0.04% at 120 min (r = 0.91; slope of 0.001). The transfer rate of TRH was 0.01 ± 0.002 ng·mL min-1 with a permeability coefficient of 1.06 + 0.25 × 10-5 mL min-1 g-1. The MAUC and FAUC values of TRH were 3994 ± 174% dose min mL-1 and 9.6± 1.2% dose mL min-1, respectively. The fetomaternal ratio and FAUC to MAUC ratio of TRH at 2 h was 0.01 ± 0.002 and 0.002 ± 0.0003, respectively. The placental uptake of TRH was 1.8 ± 0.4% of the maternal dose. The total recovery of TRH was 22.7 ± 1.6% dose, indicating that 77 ± 1.6% of TRH was metabolized by the placenta as not detectable by RIA.
Maternofetal transfer of TRH when added as a single bolus dose of (A) 4 μg dL-1 (n = 6);(B) 8 μg dL-1 (n = 7); (C) 16 μg dL-1 (n = 5); (D) 20 μg dL-1 (n= 5); (E) 40 μg dL-1 (n = 5) to the maternal circulation at the commencement of the experiments. Maternal (•―•) and fetal(○―○) concentrations are expressed as percent initial dose added. In these experiments both maternal and fetal perfusates were recirculated.
Effect of varying maternal concentration of TRH. The effect of varying maternal concentration of TRH on placental transfer is shown in Table 1 and Figure 1. When maternal concentration of TRH was increased step wise by factors of 2 from 8 μg dL-1 to 40 μg dL-1, there was a significant increase in the maternal levels and MAUC values increased as expected. The percent dose transfer of TRH at 2 h (y = 0.12x; R2 = 0.97; p < 0.001; n = 28) and clearance rate increased in a dose-dependent manner (y = 0.07; R2 = 0.97;p < 0.001; n = 28) (Fig. 2,A and B). The placenta uptake (y = 0.40x; R2= 0.95; p < 0.001; n = 28) (Fig. 2C) and percent dose TRH metabolized (y = 81.1 - 1.4x, R2 = 0.96; p < 0.001; n = 28)(Fig. 2D) increased with higher maternal levels. For a given maternal concentration of TRH, the fetal concentration was significantly less than the placental uptake (y = 3.4x; R2 = 0.75; p < 0.001; n = 28)(Fig. 2E).
Relationship between the maternal concentration of TRH when administered as a single bolus dose and (A) fetal transfer at 120 min (y = 0.11; R2 = 0.973; p < 0.001; n = 28); (B) clearance rate (y = 0.07;R2 = 0.97; p < 0.001; n = 28);(C) placental uptake (y = 0.40x; R2 = 0.95; p < 0.001; n = 28);(D) metabolism by the placenta (y = 81.1 - 1.4x; R2 = 0.96; p < 0.001; n = 28);(E) correlation between fetal concentration and placental uptake of TRH (y = 3.4x; R2 = 0.75; p< 0.001; n = 28). In these experiments both maternal and fetal perfusates were recirculated.
Open circuit. For a given concentration of TRH, steady state was achieved within 25 min of commencement of perfusion experiments, and the resultant fetal levels are shown in Figure 3. The clearance rate of TRH at a clinical equivalent dose of 400 μg was 0.08± 0.02 with placental uptake of 3.6 ± 0.7% of dose. The clearance rate (y = 0.05x; R2 = 0.99;p < 0.001; n = 22) (Fig. 4A) and placental uptake of TRH (y = 0.35x; R2 = 0.98; p < 0.001; n = 22) (Fig. 4B) increased with maternal concentration. The maternal steady state concentration of TRH was directly proportional to dose (y = 7.2x; R2 = 0.97; p < 0.001) (Fig. 4C). The clearance rate of antipyrine and creatinine was comparable between groups of experiments with mean concentrations of 2.60 ± 0.08 mL min1 and 0.75 ± 0.04 mL min-1, respectively.
Placental transfer of TRH under steady state as a function of constant maternal arterial concentration of (A) 4 μg dL-1 (n = 6); (B) 8 μg dL-1 (n= 4); (C) 16 μg dL-1 (n = 4); (D) 20μg dL-1 (n = 4); (E) 40 μg dL-1(n = 4). The fetal (•―•) values are shown as ng mL-1 The maternal steady state levels are shown in F. Note that y axes in A to C are of different scale than those of D and E. In these experiments both maternal and fetal circuits were open.
Relationship between the maternal concentration of TRH when administered as an infusion and (A) placental clearance rate[(y = 0.05x; R2 = 0.99; p < 0.001; n = 22); (B) placental uptake (y = 0.35x; R2 = 0.98; p < 0.001;n = 22); (C) maternal steady state levels (y = 7.23x; R2 = 0.99; p < 0.001). In these experiments both maternal and fetal perfusates were not recirculated.
Comparison of mode of administration of TRH. For a given concentration of TRH, the clearance rate and placental uptake of TRH over 4μg dL-1 to 40 μg dL-1 in closed and open perfusion experiments were comparable (Fig. 5).
DISCUSSION
This study shows that transplacental transfer of TRH depends upon the maternal concentration rather than its mode of administration. It also confirms our recent observation(17) that TRH does not cross the term human placenta in substantial quantities, in contravention of a widely held clinical assumption(6–10). In that study, however, we used radiolabeled TRH, and it is possible that the immunologic activity of radiolabeled TRH may not be comparable to the biologic activity of the natural molecule.
Therefore in the current study we used a commercial preparation of TRH, which has both the required bioactivity and immunogenicity to elicit a therapeutic response. We developed a highly sensitive RIA to quantitate TRH levels by using a specific antibody raised in the rabbit. We tested the specificity and cross-reactivity of this antibody and found no cross-reaction with any of its known metabolites or other peptide hormones and is highly specific for the intact TRH molecule. This allowed us to study placental metabolism of TRH indirectly from the initial concentration added and the total amount recovered at the end of experiment.
We studied transplacental transport and uptake of TRH in an in vitro model of perfused human term placenta. By altering the experimental design, it was also possible to determine the effect of mode of administration in a time- and concentration-dependent manner. Ideally, in vivo studies should be used to determine the effect of mode of administration of TRH on placental transfer rate, because apart from placental permeability and maternal integrated levels of TRH, fetal clearance could additionally influence the extent of fetal exposure to TRH, which cannot be determined in this model. The major limitation of an in vivo study, however, is that ethically it is not feasible to evaluate the dose response of TRH on placental transfer.
Accordingly, we undertook an in vitro study because this knowledge is pertinent to the formulation of dose, frequency, and mode of administration in clinical practice as well as to understanding of the mechanism by which TRH crosses the placenta. To study placental transfer kinetics independent of enzymatic degradation by serum(24), we used washed autologous blood cells suspended in tissue culture medium as the perfusate. This had the added advantage of maintaining tissue oxygenation(25). It is unlikely that use of a low protein-based perfusate influences the transplacental transfer rate of a nonprotein-bound drug such as TRH. Furthermore, our preliminary experiments using autologous blood-based perfusate suggest that absence of serum degrading enzymes in the maternal or fetal perfusate does not increase transplacental transfer of TRH; if anything it reduces its transfer probably because of decrease in maternal concentration gradient. Accordingly, we modified the composition of the perfusate to differentiate whether poor transfer of TRH was due to degradation activity of the maternal serum, placenta, or both.
In the current study, we used both open and closed perfusion preparations. In the open system, we used both creatinine and antipyrine as a marker to normalize the transfer rate of TRH for effective flow and membrane-related variables thereby reducing interexperimental variability. Use of antipyrine also allowed us to compare the diffusion of TRH with other drugs studied under similar experimental designs. In the closed system, the concentration of antipyrine equilibrates rapidly between maternal and fetal circulation(19, 20) and hence cannot be used to predict altered flow rates or back filtration from the fetal to maternal circulations. Use of creatinine in both circuit types provided an index of available exchange area and thus comparability between the two designs.
Using this experimental model, we first studied transfer and uptake of TRH at a concentration equivalent to the 400-μg dose commonly used in the clinical practice. Despite a rapid decline in the maternal concentration of TRH, net placental flux was less than 1%. This minimal transplacental transfer of TRH is unlikely to be due to failure to achieve juxtaposition of maternal and fetal circulations, as we included experiments only where transplacental transfer of creatinine was within a predefined range(20) with total recovery >95%. The total amount of TRH recovered in these experiments was only 20%, significantly lower than expected for drugs of similar molecular weight under similar experimental conditions(17–19). Although we made no attempt to isolate the metabolites of TRH, the low recovery of TRH found in this study is consistent with our previous finding(17), that restricted passage of TRH across the membrane is predominantly due to its enzymatic degradation by the placenta. Such a mechanism is also in keeping with the expected increase in percent dose of TRH recovered shown in this study with increasing maternal concentration. In contrast to our finding, Devaskar et al.(26) showed that125 I-TRH crosses the rabbit placenta readily. However, in their study radioactivity in the fetal circulation was measured at 90 min of maternal administration, and the integrity of TRH was determined by trichloracetic acid precipitation. Given the half-life of TRH to be 5.5 min and molecular mass of 330 D, it is highly unlikely that intact TRH molecules would be present in the fetal circulation after 90 min. Another difference between the two studies may be attributed to disimilarities in placental structure. Endogenous production of TRH by the placenta(27) seems unlikely to account for minimal transplacental transfer of TRH, because using 125I-labeled TRH, which has an added advantage of determining transplacental transfer over and above the endogenous production by the placenta, we have shown fetal levels to be comparable to the current study.
Although no direct information is available regarding the mechanism by which TRH crosses the placenta, it has been inferred that, like most drugs(18, 19), transport occurs by simple diffusion. However, there is a possibility that placental transport of TRH may take place by an energy-dependent pathway, particularly so when TRH receptors are present in the syncytiotrophoblast(27), and carrier-mediated transport has been implicated in its transfer across intestinal mucosa(28, 29). To elucidate the mechanism of transport across the placenta, we studied the transfer as a function of concentration in a time-dependent manner. There was a linear relationship between rate of transport and the concentration of TRH, consistent with transfer by passive diffusion across the placental membrane. Had it been by an energy-dependent pathway, a saturable process for the transport and uptake of TRH with increasing concentration would be expected(28, 29). Our observation of a linear relationship between placental accumulation and maternal concentration of TRH also suggests that both uptake and transport of TRH follow a first order passive diffusion process. Although we did not attempt to separate intact the TRH molecule from its active metabolite, based on our previous work(17), which shows that metabolites formed during placental transport do not permeate the basolateral membrane, we suggest that transcellular rather than paracellular passive diffusion is a major pathway for the transport of TRH across the placental membrane.
If transfer of TRH across the membrane is restricted because of degradation as we have suggested, it is difficult to explain why placental uptake and clearance seem dose-dependent. The cellular uptake versus transport of TRH indicates that the rate of transfer should be about one-third of the placental uptake. Together this suggests that TRH is metabolized during its transport by transcellular diffusion from the maternal to fetal circulation. We found a positive correlation between the rate of transport, metabolism of TRH, and its concentration. Given the evidence that TRH is rapidly degraded by placental enzymes(17), one would have expected the incremental trend to plateau at a substrate concentration that is 10-fold higher than the dose used in clinical practice. Although we made no attempt to study the kinetics of enzyme and substrate relationships, our limited experimental data suggest that placental enzyme has a high affinity for the TRH molecule, and a 20-50-fold higher dose of TRH would be necessary to saturate the enzymatic pathway. This may also be one of the reasons why the placental clearance rate of TRH was comparable when studied under steady state or after administration as a single bolus dose.
In this study we also attempted to evaluate the effect of mode of administration of TRH on placental clearance rate and hence fetal exposure. Because TRH does not bind to plasma proteins(1, 2), the only factor which can influence fetal exposure in relation to mode of administration is the integrated maternal concentration and placental permeability of TRH. Our data show that, for a given concentration of TRH, placental clearance was independent of whether given as a bolus or infusion. This observation was in keeping with clinical studies, which have not shown any difference in clinical outcome in relation to mode of administration(7, 9–13). Furthermore, placental uptake between the two groups further suggests that placental metabolism of TRH did not depend upon mode of administration.
We appreciate that, as we used an in vitro model of perfused human term placenta, it is difficult to extrapolate this findings in terms of clinical usage where TRH is given between 24 and 32 wk of gestation to enhance fetal lung maturity. It is plausible that in the preterm placenta TRH degrading enzyme(s) is either absent or its activity is suppressed by concomitant use of dexamethasone. Hence further in vivo and in vitro studies are necessary to determine the ontogeny of the TRH degrading placental enzymes and the factors influencing their activity.
In summary our results show that TRH crosses the human term placenta sparingly, and the rate of transfer is proportional to the dose, but not mode of administration. In terms of clinical usage of maternal TRH administration to enhance fetal maturation, our data suggest that a higher dose might facilitate transplacental transfer of TRH to the fetus. However, it is possible that, unlike that of adults(30), the thyrotrophic response in the human fetus is not dose-dependent as shown by a recent in vivo study(31). One reason for this finding is that, as in neonatal rats, the human fetal pituitary may have increased affinity for TRH(32). Alternatively maternal administration of TRH may stimulate the fetal pituitary-thyroid axis indirectly via secretion of TSH-like substances by the placenta. Before any modification to therapeutic regimes can be contemplated, further data regarding maternal and fetal pharmacokinetics and pharmacodynamics of TRH in vivo in relation to dose, route of administration, frequency, and gestational age are needed.
Abbreviations
- TRH:
-
TSH-releasing hormone
- MAUC:
-
maternal area under the curve
- FAUC:
-
fetal area under the curve
References
Jackson IMD 1982 Thyrotropin releasing hormone. N Engl J Med 306: 145–155
Horita A, Carino MA, Lai H 1986 Pharmacology of thyrotropin-releasing hormone. Annu Rev Pharmacol Toxicol 26: 311–332
Roti E, Gnudi A, Braverman LE, Robuschi G, Emanuele R, Bandini P, Benassi L, Pagliani A, Emerson CH 1981 Human cord blood concentrations of thyrotropin, thyroglobulin, and iodothyronines after maternal administration of thyrotropin-releasing hormone. J Clin Endocrinol Metab 53: 813–817
Moya F, Mena P, Foradori A, Becerra M, Inzunza A, Germain A 1991 Effect of maternal administration of thyrotropin releasing hormone on the preterm fetal pituitary-thyroid axis. J Pediatr 119: 966–971
Moya F, Mena P, Heusser F, Foradori A, Paiva E, Yazigi R, Michaud P, Gross I 1986 Response of the maternal, fetal, and neonatal pituitary-thyroid axis to thyrotropin-releasing hormone. Pediatr Res 20: 982–986
Thorpe Beeston JG, Nicolaides KH, Snijders RJ, Butler J, McGregor AM 1991 Fetal thyroid-stimulating hormone response to maternal administration of thyrotropin-releasing hormone. Am J Obstet Gynecol 164: 1244–1245
Ballard PL, Ballard RA, Creasy RK, Padbury J, Polk DH, Bracken M, Moya FR, Gross I 1992 Plasma thyroid hormones and prolactin in premature infants and their mothers after prenatal treatment with thyrotropin-releasing hormone. Pediatr Res 32: 673–678
de Zegher F, Spitz B, Devlieger H 1992 Prenatal treatment with Thyrotropin releasing hormone to prevent neonatal respiratory distress. Arch Dis Child 67: 450–454
Morales WJ, O'Brien WF, Angel JL, Knuppel RA, Sawai S 1989 Fetal lung maturation: the combined use of corticosteroids and thyrotropin-releasing hormone. Obstet Gynecol 73: 111–116
Knight DB, Liggins GC, Wealthall SR 1994 A randomized, controlled trial of antepartum thyrotropin-releasing hormone and betamethasone in the prevention of respiratory disease in preterm infants. Am J Obstet Gynecol 171: 11–16
Crowther CA, Alfirevic Z 1995 Antenatal thyrotropin-releasing hormone prior to preterm delivery. In: Renfrew MJ, Crowther CA, Neilson JP (eds) Cochrane Database of Systematic reviews-Pregnancy and Childbirth Module, Version 1.2, Disk Issue 2, Record 4749
ACTOBAT Study Group: 1995 Australian Collaborative trial of antenatal TRH for prevention of neonatal respiratory disease. Lancet 345: 877–881
Ceriani J, Cernadas JM, Fiascone JM, Althabe F, Althabe O 1992 Controlled trial of prenatal betamethasone plus TRH for prevention of respiratory syndrome (RDS). Pediatr Res 32: 738( abstr 9)
Snyder PJ, Utiger RD 1972 Response to thyrotropin releasing hormone (TRH) in normal man. J Clin Endocrinol Metab 34: 380–385
Snyder PJ, Utiger RD 1972 Thyrotropin response to thyrotropin releasing hormone in normal females over forty. J Clin Endocrinol Metab 34: 1096–1098
Lambardi G, Lupoli G, Scopacasa F, Panza R, Minozzi M 1972 Plasma immunoreactive thyrotropin releasing hormone (TRH) values in normal newborns. J Endocrinol Invest 1: 69–72
Bajoria R, Oteng Natim E, Fisk NM 1996 Transfer and metabolism of thyrotropin releasing hormone across the perfused human term placenta. J Clin Endocrinol Metab 81: 3476–3482
Bajoria R, Contractor SF 1992 Transfer of heparin across the human perfused placental lobule. J Pharm Pharmacol 44: 952–959
Bajoria R, Contractor SF 1993 Maternal-fetal transfer of warfarin across an in vitro model of perfused placenta; effect of albumin binding. Br J Haematol 84: 59
Eaton BM, Browne MJ, Contractor SF 1985 Maternal to fetal movement of creatinine as a measure of perfusion efficiency and diffusional transfer in the isolated human placental lobule. Placenta 6: 341–346
Bassiri RM, Utiger RD 1972 The preparation and specificity of antibody to thyrotropin releasing hormone. Endocrinology 90: 722–727
Heinegard D, Tiderstrom G 1973 Determination of serum creatinine by a direct colorimetric method. Clin Chim Acta 43: 305–310
Brodie BB, Axelrod J, Soberman R, Levy BB 1949 The estimation of antipyrine in biological materials. J Biol Chem 179: 25–31
Neary JT, Nakamura C, Davies IJ, Soodak M, Malord I 1978 Lower levels of thyrotropin-releasing hormone degrading activity in human cord and in maternal sera than in the serum of euthyroid non pregnant adults. J Clin Invest 21: 1–5
Contractor SF, Eaton BM, Firth JA, Bauman KF 1984 A comparison of the effects of different perfusion regimes on the structure of the isolated human placental lobule. Cell Tissue Res 237: 609–617
Devaskar U, Nitta K, Szewczyk K, Sadiq HF, deMello D 1987 Transplacental stimulation of functional and morphologic fetal rabbit lung maturation: effect of thyrotropin-releasing hormone. Am J Obstet Gynecol 157: 460–464
Shambaugh G 3rd, Kubek M, Wilber J 1979 Thyrotropin-releasing hormone activity in the human placenta. J Clin Endocrinol Metab 48: 483–486
Yokohama S, Yoshioka T, Yamashita K, Kitamori N 1984 Intestinal absorption mechanisms of thyrotropin-releasing hormone. J Pharmacobiodyn 7: 445–451
Yokohama S, Yoshioka T, Kitamori N, Shimamoto T, Kamada A 1985 Intestinal absorption mechanisms ofγ-butyrolactone-γ-carbonyl-L-histidyl-L-prolinamide citrate(DN-1417) and thyrotropin-releasing hormone (TRH). J Pharmacobiodyn 8: 278–285
Weeke J 1975 The response of thyrotropin and triiodothyronine to various doses of thyrotropin releasing hormone in normal man. Eur J Clin Invest 5: 447–453
Crowther C, Haslam R, Hiller J, McGee T, Ryall R, Robinson J 1995 Thyrotropin-releasing hormone: does two hundred micrograms provide effective stimulation to the preterm fetal pituitary gland compared with four hundred micrograms?. Am J Obstet Gynecol 173: 719–723
Banerji A, Prasad C 1982 The postnatal development of the pituitary thyrotropin-releasing hormone receptor in male and female rats. Endocrinology 110: 663–664
Acknowledgements
The authors thank Dr. H Fraser, MRC Unit for Reproductive Medicine, Edinburgh, for providing anti-rabbit TRH antibody.
Author information
Authors and Affiliations
Additional information
Supported by a project grant from Action Research.
Rights and permissions
About this article
Cite this article
Bajoria, R., Fisk, N. Maternofetal Transfer of Thyrotrophin-Releasing Hormone: Effect of Concentration and Mode of Administration. Pediatr Res 41, 674–681 (1997). https://doi.org/10.1203/00006450-199705000-00012
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199705000-00012