Abstract
Cerebrovascular reactivity is preserved after acute severe asphyxia/reventilation in piglets. We hypothesize that prolonged, partial asphyxia with hypotension causes loss of cerebrovascular reactivity and altered cerebral hemodynamics during recovery. We investigated the changes in cerebrospinal fluid cAMP and cGMP, pial arteriolar diameters and flow, and cerebral blood flow during 1 h of asphyxia and 1 h of recovery. During asphyxia, blood pressure decreased from 10 ± 0.7 to 4.7 ± 0.3 kPa and increased during recovery to 6 ± 0.7 kPa. cAMP increased 3-fold by 20 min of asphyxia, returning to baseline at 40 min of asphyxia. During recovery, cAMP increased 2-fold initially, followed by a decrease to 50% below baseline. cGMP increased after 20 min of asphyxia, with maximum levels observed at 40 min; reventilation resulted in a transient increase in cGMP. Pial arteriolar diameters increased at the onset of asphyxia, then decreased toward baseline; during recovery, a similar pattern occurred. Blood flow to the cerebrum (microspheres) decreased during asphyxia and remained very low during recovery. Pial arteriolar flow but not pial arteriolar diameters followed the changes in cortical cerebral blood flow (i.e. virtually no flow during recovery). During recovery, pial arteriolar reactivity to isoproterenol and histamine decreased significantly. We conclude that 60 min of asphyxic-hypotensive insult results in alterations of cerebral cAMP metabolism which may compromise cellular communications during recovery. Prolonged asphyxia induces “no-reflow” during recovery, even when partial pressures of arterial CO2 and O2 have returned to baseline values, and blood pressure is within the autoregulatory range.
Similar content being viewed by others
Main
Hypoxic-ischemic encephalopathy, a common neurologic sequela of perinatal asphyxia, is a significant cause of neonatal mortality and morbidity. In human neonates, perinatal asphyxic/ischemic or hypoxic injury may result from different conditions with varying degrees of insults and therefore with variable outcomes. Similarly, in experimental asphyxia, cerebral hemodynamic alterations and manifestations appear dependent upon the species, the model of asphyxia, and the kind of interventions that were made during insult or recovery(1–5). Thus, reports differ as to changes in postasphyxic CBF. Increases in CBF up to 150% and“luxury perfusion” have been described(6, 7). Others have reported on decreases in CBF and the “no-reflow phenomenon” after asphyxia(8–11). Experiments in primates have suggested that, to cause disability, asphyxia may need to be prolonged and nearly fatal(12). The most severe outcome is observed with prolonged partial asphyxia(12), especially with concomitant hypotension(13–16). We have found that in total asphyxia, i.e. respiratory arrest of short duration(1) or with partial asphyxia of 30-min duration(17), piglets recovered from asphyxic insult without systemic hypotension. In addition, during recovery, cerebrovascular reactivity was preserved in total asphyxia but attenuated in partial asphyxia(1, 5, 17).
Postasphyxic hypotension is a frequent finding in babies with severe asphyxic insult. The purpose of this study was to develop a model of“partial” asphyxia in newborn pigs, severe enough to produce systemic hypotension. We hypothesized that prolonged, partial asphyxia with hypotension causes loss of cerebrovascular reactivity and altered cerebral hemodynamics during recovery. In an effort to better understand the effects of prolonged partial asphyxia on the cerebral circulation, we monitored the changes in periarachnoid CSF, cAMP and cGMP concentrations, pial arteriolar BF(qualitatively) and diameters, regional and hemispheric CBF, and cerebrovascular reactivity.
METHODS
The surgical and experimental procedures were reviewed and approved by the Animal Care and Use Committee of The University of Tennessee, Memphis.
Piglets 2-5 d of age (1-2 kg) of either sex were anesthetized and instrumented before the experiments. Piglets were initially anesthetized with intramuscular ketamine hydrochloride (33 mg/kg) and acepromazine (3.3 mg/kg) and maintained on i.v. α-chloralose (50 mg/kg initially plus 3 mg/kg/2 h). The animals were ventilated with room air through a tracheostomy tube using a Bournes BP200 infant ventilator. Catheters were inserted into the femoral vein for maintenance of anesthesia and fluid administration (100 mL/kg/d of 5% dextrose in water), into the femoral arteries to record BP and heart rate, for blood gas sampling, and also for reference withdrawal in microspheres studies. A fourth catheter was inserted into the ventricle through the right carotid artery to inject the microspheres. In piglets, ligation of one carotid artery has no detectable effect on hemispheric CBF(4, 18). A closed cranial window was inserted over the parietal cortex for measurements of pial arteriolar diameters, qualitative assessments of pial arteriolar flow, and collection of cortical periarachnoid CSF for measurement of cAMP and cGMP. Body temperature was maintained between 37 and 38 °C.
Protocol. Two groups of piglets were studied, a time-control group and an asphyxia group. In the time-control group (n = 8), pial arteriolar diameters, periarachnoid CSF cyclic nucleotides, and CBF were measured at intervals under normoxic and normotensive conditions maintained for 2 h. In the asphyxia group (n = 11), 30 min after stabilization from surgery, asphyxia was produced for 60-min duration by ventilating the piglets with a gas mixture of 10% CO2, 10% O2, and 80% N2 and by decreasing the minute volume. Respiratory support and the gas mixture were manipulated to maintain the systemic BP around 4 kPa and the heart rate between 50 and 80 beats/min. At the end of 60 min of asphyxia, the minute volume was increased, and the piglets were ventilated with room air. Piglets were evaluated during 60-90 min of recovery. Arterial blood was collected every 10 min for blood gases and pH measurement using an Instrumentation Blood Gas Analyzer (Instrumentation Laboratory, Lexington, MA). BP and heart rate were monitored continuously during the experiments. Cortical periarachnoid CSF was collected every 10 min for later measurements of cAMP and cGMP. Diameters of two to four pial arterioles were recorded every 2 min during the experiments. Vascular reactivity to topically applied isoproterenol(10-4 M) and histamine (10-4 M) was evaluated before asphyxic insult and repeated during 60-90 min of recovery. Measurements of pial arterioles after application of each compound were taken every minute for 10 min. At the end of 10 min, the space under the cranial window was flushed with artifical CSF for 15-30 min before application of the second compound. CBF and cardiac output determinations were made at baseline, at 10, 30, and 60 min of asphyxia, and at 10 and 60 min of recovery.
Radioactive microsphere determinations Of CBF distribution. A known amount of radioactivity in 15-μm microspheres (≥1 000 000 microspheres) was injected into the left ventricle, and the injection line was flushed with 1 mL of saline. Withdrawal of reference blood samples (1.03 mL/min from the descending aorta) was begun 15 s before microsphere injections and continued for 2 min. Withdrawn blood was replaced with donor piglet blood. At the end of the experiments, the piglets were killed by injecting KCI into the left ventricle, and the brain was removed. The brain was subdivided into right and left hemispheres and major regions (cerebrum, white matter, gray matter, caudate nucleus, pons, medulla, diencephalon/mesencephalon, cerebellum, and choroid plexus). Samples were counted in a gamma-counter. The energy from each nuclide was separated by differential spectroscopy. Aliquots of the actual microsphere solutions injected were used for overlap calculations. The nuclides and energy windows used were (in keV) 46Sc 840-1240, 95Nb 710-810, 103Ru 480-510, 113Sn 370-440,57 Co 100-150, and 125I 36-70. The lungs were counted to detect extensive arteriovenous shunting of microspheres. “Lung blood flow” (comprised of bronchial flow and whole body arteriovenous shunt flow) averaged 2% of cardiac output, indicating that no extraordinary shunting of microspheres occurred. Cardiac output was calculated as (reference withdrawal rate) × (counts injected) × (counts in reference withdrawal)-1. BF to each brain region at the time the microspheres were injected was calculated by using the formula: Q = C× R × CR-1, where Q = organ blood flow in mL/min × 100 g, C = counts/100 g of tissue,R = rate of withdrawal of reference blood sample in mL/min, and CR = total counts in reference arterial blood sample.
Closed cranial window placements for measurements of pial arteriolar diameters and collection of periarachnoid CSF. To implant the cranial window the scalp was cut and reflected from the skull. A hole approximately 2 cm in diameter was made in the skull. Incision was made through the dura and arachnoid membranes, and these membranes then were reflected over the edge of the bone. A stainless steel ring with a premounted glass coverslip was inserted in the hole. The window was cemented in place with dental acrylic. Three needles pierced the ring and allowed injection of artificial CSF under the window and sampling of CSF from under the window. The space under the window was filled with artificial CSF (Na+ 150 mEq/L, K+ 3 mEq/L, Ca2+ 2.5 mEq/L, Mg2+ 1.2 mEq/L, Cl- 13 mEq/L, glucose 3.7 mM, urea 6 mM, HCO3- 25 mEq/L, pH = 7.33, Pco2 = 6.1 kPa, Po2 = 5.7 kPa). The volume directly below the window was approximately 500 μL. After implantation of the window, 30 min were allowed for equilibration of CSF under the window. Pial arterioles were observed with a Wild dissecting microscope. Pial arteriolar diameters were measured with a television camera mounted on the microscope, a video monitor, and a video microscaler. Briefly, the images of the arterioles were displayed on the television monitor, and the sides of the vessels were bracketed by parallel lines projected by the microscaler. As the arteriolar diameter changed, the lines were moved manually to correspond with the vessel walls. Precalibration of the distance between the lines allowed determination of arteriolar diameter. BF changes through the pial arterioles were also qualitatively monitored during the experiments.
Cyclic nucleotide assays. Cortical periarachnoid CSF (0.4 mL) collected from under the window was mixed with EDTA (5 mM) and stored at -60°C until assayed. cAMP and cGMP were measured in CSF samples using RIA procedures and commercial 125I-cAMP or 125I-cGMP scintillation proximity assay systems (Amersham International plc, Amersham, UK). Acetylation of CSF samples with a 2:1 mixture of triethanolamine and acetic anhydride was performed immediately before assay to increase the sensitivity of the method (the analysis range is 2-128 fmol of cAMP and 4-512 fmol of cGMP/sample). These RIAs used the simultaneous addition of sample,125 I-cAMP or 125I-cGMP, rabbit cAMP or cGMP antibody, and an anti-rabbit second antibody bound to scintillant-incorporated microspheres. Samples were mixed overnight on an orbital shaker (200 rpm) at room temperature. To determine the amount of 125I-cAMP or 125I-cGMP bound to the light-producing microspheres, the vials were counted using aβ-scintillation counter. All unknowns were assayed at two dilutions. The cyclic nucleotide concentration in the CSF sample was calculated from the standard curve.
Statistical analysis. Values are reported as means ± SEM. Comparisons among different time periods were made using analysis of variance with repeated measures and followed by Fisher's protected least significant difference test. Comparisons between the two groups were made using a t test for planned comparisons (paired or unpaired, as appropriate). A p value <0.05 was considered significant. First-level Winsorization(19) was used for statistical analysis when a single value was extreme in comparison with the remainder of the sample.
RESULTS
Physiologic measurements in the time-control piglets are shown in Table 1. Arterial BP, blood gases, and pH were maintained at baseline levels over time. We observed a trend toward an increase, rather than a decrease, in pial arteriolar diameter, CBF, and cyclic nucleotides in 2 h.
Four piglets did not tolerate the asphyxic insult and expired at 30-50 min of asphyxia in spite of aggressive resuscitation. The CBF measurements were not performed in one piglet because of technical difficulty; complete CBF data were obtained from six piglets. The cranial window data were available from seven piglets. In each piglet, two to four pial arterioles of different diameters (85-220 μm) were monitored every 2 min.
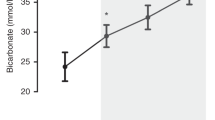
All piglets started with normal BP, pH, and blood gas values (Fig. 1). With the onset of asphyxia, BP decreased from 10± 0.7 to 4.7 ± 0.3 kPa and was maintained at that level by manipulating the degree of asphyxia (changes in inspired gas mixture). During recovery, BP increased only to 6 ± 0.7 kPa and remained at that level. With asphyxia, arterial pH decreased from 7.40 ± 0.06 to 6.90 ± 0.02, followed by a gradual increase to 7.30 ± 0.01 during recovery. During asphyxia, Paco2 increased from 4.5 ± 2 to 12.5 ± 0.5 kPa and Pao2 decreased from 11.7 ± 0.8 to 4.7 ± 0.3 kPa, respectively, both measurements quickly returning to baseline upon reventilation. During recovery, piglets were ventilated with room air, and no attempt was made to correct the metabolic acidosis or the systemic hypotension.
Figure 2 shows the cyclic nucleotides concentrations from the periarachnoid CSF collected every 10 min during asphyxia and recovery. The CSF cAMP increased 3-fold by 20 min of asphyxia; at 40 min, values gradually decreased to baseline level. During early recovery, the cAMP increased 2-fold, but, as recovery continued, the CSF cAMP decreased and stabilized at 50% below baseline values. The CSF cGMP increased over 3-fold by 40 min of asphyxia. With continuation of asphyxia, cGMP decreased toward baseline. A 2-fold increase in CSF cGMP was observed in early recovery, returning toward baseline as recovery continued.
Pial arteriolar diameters increased significantly with the onset of asphyxia (Fig. 3) and then decreased during the last 30 min of asphyxia, but measurements remained above baseline. These findings persisted throughout the recovery period. At the onset of asphyxia, red cell movement within the pial arterioles appeared to increase (qualitative assessment), and the vessels were engorged. As asphyxia continued, red blood cell movement decreased, and cells became clumped together inside the vessels. During recovery, initially forward flow was noted, but soon red blood cell movement decreased and, utimately, sludging resulted. Thus there was a lack of correlation between the pial arteriolar diameter and CBF.
Regional CBF and cardiac output measurements at baseline and at 10, 30, and 60 min of asphyxia and again at 10 and 60 min of recovery are shown in Table 2. Although right and left hemispheric BF were measured, no differences were observed between hemispheres. Fluctuations of CBF during asphyxia and recovery had different patterns in different regions (Fig. 4). BF to the cerebrum, white matter, gray matter, and caudate nucleus progressively decreased during asphyxia, with“no-reflow” for the duration of reventilation. BF to the brainstem region (pons and medulla) had biphasic patterns during asphyxia and recovery; BF to these regions returned toward baseline by 60 min of recovery. During asphyxia, BF to the cerebellum and choroid plexus decreased significantly. However, during recovery, BF to these regions returned to about one-third of baseline. Cardiac output decreased during asphyxia. After a transient increase during early recovery, cardiac output decreased significantly below baseline level.
As to pial arteriolar reactivity to topical vasodilators, the percent increase in pial arteriolar diameter with isoproterenol administration decreased from 45 ± 7% to 8 ± 3% (p < 0.05). Similarly, percent increase in pial arteriolar diameter with histamine decreased from 53 ± 5% to 5 ± 3% (p < 0.05).
DISCUSSION
Our findings in newborn pigs with prolonged partial asphyxia/hypotension include: 1) a significant decrease in CSF cAMP but not cGMP during recovery, 2) a no-reflow phenomenon that was observed in higher brain regions, and 3) the loss of cerebrovascular reactivity to vasodilator stimuli.
Partial asphyxia is a common cause of perinatal brain damage in human infants(7). In this experiment, we were able to develop a model of partial asphyxia/incomplete ischemia severe enough to produce systemic hypotension during asphyxia and recovery. This model differs from total asphyxia(20) wherein there is complete cessation of gas exchange and from complete ischemia when blood is almost entirely stripped away from the cerebral circulation. During partial asphyxia/incomplete ischemia the presence of intraluminal blood may cause a greater generation of lactic acid and oxygen free radicals(10, 21–25). In our model, the persistent hypotension may be more detrimental, because systemic arterial BP is a critical factor in maintaining CBF(13, 16, 26).
Cerebral cyclic nucleotides. The effects of asphyxia/ischemia on cerebral cyclic nucleotides have not been studied extensively. The limited studies show that the brain's response to acute ischemia and hypoxia is increased brain tissue and CSF cAMP(23, 27). Our study is unique because we made longitudinal measurements of CSF cAMP and cGMP every 10 min during asphyxia and recovery. In our piglets, during prolonged partial asphyxia, CSF cAMP increased significantly and returned to baseline with continuing asphyxia. After a transient rise in CSF cAMP during early recovery, the CSF cAMP levels fell and stabilized at 45-50% below baseline, as recovery continued. Our time-control piglets did not show decrease in CSF cAMP over time.
Ischemia and recirculation appear to be situations where the fluctuating levels of the brain's ATP contribute to the regulation of cAMP(27). When the brain's O2 supply is abolished even briefly, there is a precipitous fall in ATP and a sharp rise in concentration of cAMP(28). cAMP is synthesized from ATP by the plasma-membrane-bound enzyme, adenylyl cyclase, and it is rapidly and continuously destroyed by one or more cAMP phosphodiesterases, hydrolyzing cAMP to 5′-AMP(29).
Possible causes for low CSF or brain cAMP include deficiency of ATP, increased phosphodiesterase activity, low adenylyl cyclase activity, and decreased adenylyl cyclase agonists, such as adenosine and catecholamines(30). Our observation of low levels of CSF cAMP during late recovery may be explained by sluggish ATP regeneration, which is likely to occur with associated mitochondrial damage after hypoxia/ischemia(15, 31) and hypotension(14). Irreversible alterations in mitochondrial function(3, 32) also could be induced by very low pH, leading to a permanent suppression of ATP production even when oxygen is present(3, 32). During late reperfusion, the period of“secondary ischemia,” generation of oxygen free radicals may further impair mitochondrial ATP production, leading to low levels of cAMP and neuronal death(23, 24, 33, 34).
cGMP, like cAMP, participates in intracellular signaling. However, catabolism and resynthesis of guanine nucleotides differs from the adenylate system(35). Guanylyl cyclase catalyzes the production of cGMP from GTP. Low concentrations of cGMP have been measured in the cerebral cortex of gerbils after ischemic insult(27, 30). In our piglets, at no time during asphyxia or recovery did the cGMP level decrease below baseline values.
Cerebral blood flow and pial arteriolar diameters. Cortical BF measurements by microspheres correlated well with qualitative changes in pial arteriolar BF; both showed severe decrease in flow, especially during late recovery. Term infants with evidence of hypoxic-ischemic encephalopathy have been reported to have lowered estimated CBF in the first few days of life(36, 37). Although in the lower normal range of cerebrovascular autoregulation for newborn pigs(26), BP in our piglets was not adequate to maintain cerebral perfusion pressure. Lou et al.(38) reported that in fetal lambs restoration of systemic BP by infusion of whole blood after severe hypotensive-asphyxia did not raise the CBF. Hypotension in our piglets may be explained by decreased cardiac output, probably secondary to myocardial ischemia. This postichemic hypotension was severe enough to have caused the no-reflow phenomenon. The no-reflow phenomenon, first described in adult rabbits by Ames et al.(10) and subsequently observed in several other species(11, 39), was thought to be due to cerebral vasospasm. However, we did not see any pial arteriolar vasoconstriction. Instead, we observed pial arteriolar dilation, whereas cortical CBF was minimal or absent. Thus, changes in pial arteriolar diameter were not correlated with cortical BF.
Cerebral microvascular obstruction secondary to increased blood viscosity, endothelial cell injury, polymorphonuclear leukocyte-endothelial adhesion, and/or platelet and erythrocyte aggregation could also contribute to no-reflow(10, 40). We did observe intravascular clumping of blood cells during the recovery period.
Other proposed mechanisms for the no-reflow phenomenon include microvascular compression due to perivascular edema(40), generation of oxygen free radicals(25, 34), and influx of Ca2+ ions(41). Krause et al.(41) showed that calcium antagonists inhibited postischemic brain hypoperfusion. Rosenberg et al.(34) treated newborn lambs with oxygen free radical-scavenging enzymes and observed an improvement in postasphyxial CBF.
Variations in regional CBF responses were observed in our piglets. Brainstem structures showed a biphasic BF pattern during asphyxia and recovery. Preservation of brainstem BF has also been observed with short periods of asphyxia(1, 42). We found no difference between hemispheric BF during asphyxia or recovery. A similar observation was made by Laptook et al.(4). Piglets, like human newborns, have functional collateral brain circulation.
Cerebrovascular reactivity. We observed a generalized pial arteriolar unresponsiveness to vasoactive stimuli (isoproterenol and histamine), suggesting vasomotor paralysis(9). In newborn lambs, Rosenberg(43) observed attenuation of cerebral vasodilation to hypoxia and an absent response to hypotension during recovery from partial asphyxia. Sankaran et al.(36) reported, a loss of cerebrovascular reactivity to hypercapnia in the first few days of life in term infants with hypoxic-ischemic encephalopathy. Mechanisms suggested for impaired cerebral vasoreactivity include obstruction of resistance vessels by cerebral edema, excessive production of cerebral vasoconstrictor prostanoids, or vascular endothelial injury secondary to oxygen free radicals(25, 43). However, high levels of brain oxygen free radicals have not been found to be consistently associated with loss of cerebrovascular reactivity(44). Vascular reactivity is preserved in acute asphyxia(5) but lost or reversed in total cerebral ischemia(45, 46), each condition generating similar levels of brain oxygen free radicals.
Conclusion. Prolonged partial asphyxia with hypotension in newborn pigs resulted in no-reflow during recovery. During recovery, pial arterioles were unresponsive to topical application of vasodilators, suggesting cerebral vasoparalysis. The CSF cAMP was decreased during recovery, which may indicate cerebral mitochondrial damage secondary to systemic hypotension, metabolic acidosis, or generation of oxygen free radicals.
Abbreviations
- BF:
-
blood flow
- BP:
-
blood pressure
- CBF:
-
cerebral blood flow
- CSF:
-
cerebrospinal fluid
- ANOVA:
-
analysis of variance
- Pao2:
-
partial pressure of arterial O2
- Paco2:
-
pretial pressure of arterial CO2
References
Pourcyrous M, Leffler CW, Busija DW 1990 Role of prostanoids in cerebrovascular responses to asphyxia and reventilation in newborn pigs. Am J Physiol 259:H662–H667
Rosenberg AA, Parks JK, Murdaugh E, Parker D Jr 1989 Mitochondrial function after asphyxia in newborn lambs. Stroke 20: 674–679
Hillered L, Smith M, Siesjo BK 1985 Lactic acidosis and recovery of mitochondrial function following forebrain ischemia in rat. J Cereb Blood Flow Metab 5: 259–266
Laptook A, Stonestreet BS, Oh W 1983 The effect of carotid artery ligation on brain blood flow in newborn piglets. Brain Res 276: 51–59
Pourcyrous M, Busija D, Leffler C, Bada H, Korones S 1990 Asphyxia does not alter the cerebrovascular responses to hypercapnia, isoproterenol and norepinephrine in newborn pigs. Clin Res 38: 956A
Cohn EH, Sacks EJ, Heymann MA, Rudolph AM 1974 Cardiovascular responses to hypoxemia and acidemia in fetal lambs. Am J Obstet Gynecol 120: 817–822
Lassen NA 1966 The luxury-perfusion syndrome and its possible relation to acute metabolic acidosis localized within the brain. Lancet 2: 1113–1115
Revich M, Brann Jr AW, Shapiro HM, Myers RE 1972 Regional cerebral blood flow during prolonged partial asphyxia. In: Meyer JS, Reivich M, Lechner H, Eichorn O (eds) Research on the Cerebral Circulation. Fifth International Salzburg Conference. Charles C Thomas, Springfield, IL, pp 216–227
Langfitt TW, Weinstein JD, Kassell NF 1965 Cerebral vasomotor paralysis produced by intracranial hypertension. Neurology 15: 622–641
Ames A, Wright RL, Kowada M, Thurston JM, Majno G 1968 Cerebral ischemia. II. The no reflow phenomenon. Am J Physiol 52: 437–453
Thiringer K, Hrbek A, Karlsson K, Rosen KG, Kjellmer I 1987 Postsphyxial cerebral survival in newborn sheep after treatment with oxygen free radical scavengers and a calcium antagonist. Pediatr Res 22: 62–66
Beller FK 1995 A guest editorial. The cerebral palsy story: a catastrophic misunderstanding in obstertrics. Obstet Gynecol 50: 83
Yutsu FM, Lee LW, Liao CL 1975 Energy metabolism during brain ischemia; stability during reversible and irreversible damage. Stroke 6: 678–683
Schutz H, Silverstein PR, Vapalahti M, Bruce DA, Mela L, Langfitt TW 1973 Brain mitochondrial function after ischemia and hypoxia. I. Ischemia induced by increased intracranial pressure. II. Normo-tensive systemic hypoxemia. Arch Neurol 29: 408–419
Tsuji M, Naruse H, Volpe J, Holtzman D 1995 Reduction of cytochrome aa3 measured by near-infrared spectroscopy predicts cerebral energy loss in hypoxic piglets. Pediatr Res 37: 253–259
Johnson GN, Palahniuk RJ, Tweed WR, Jones MV, Wade JG 1979 Regional cerebral blood flow changes during severe fetal asphyxia produced by slow partial umbilical cord compression. Am J Obstet Gynecol 135: 48–52
Pourcyrous M, Bada H, Korones S, Leffler C 1992 Altered cerebrovascular reactivity to vasodilator stimuli following prolonged asphyxia in newborn pigs. Pediatr Res 31: 217A( abstr)
Pourcyrous M, Bada HS, Korones SB, Leffler CW 1996 Comparison of left- and right-sided brain blood flow responses in asphyxiated newborn pigs when a common carotid artery is ligated. Pediatr Res 39: 239A(absr)
Dixon W J, Massey FJ 1969 Introduction to Statistical Analysis, 3rd Ed. McGraw-Hill, New York, pp 330–332
Myers RE 1972 Two patterns of perinatal brain damage and their conditions of occurrence. Am J Obstet Gynecol 112: 246–256
Rehncrona S, Mela L, Siesjo BK 1979 Recovery of brain mitochondrial function in the rat after complete and incomplete cerebral ischemia. Stroke 10: 437–446
Ljunggren B, Ratcheson RA, Siesjo B 1974 Cerebral metabolic state following complete compression ischemia. Brain Res 73: 291–307
Nemoto EM 1978 Pathogenesis of cerebral ischemia-anoxia. Crit Care Med 6: 203–214
Hillered L, Ernster L 1983 Respiratory activity of isolated rat brain mitochondria following in vitro exposure to oxygen radicals. J Cereb Blood Flow Metab 3: 207–214
Kontos HA 1985 Oxygen free radicals in cerebral vascular injury. Circ Res 57: 508–516
Laptook A, Stonestreet BS 1982 The effects of different rates of plasmanate infusions upon brain blood flow after asphyxia and hypotension in newborn piglets. J Pediatr 100: 791–796
Kobayashi M, Lust WD, Passonneau JV 1977 Concentrations of energy metabolites and cyclic nucleotides during and after bilateral ischemia in the gerbil cerebral cortex. J Neurochem 29: 53–59
Gibson GE, Shimada M, Blass JP 1978 Alterations in acetylcholine synthesis and cyclic nucleotides in mild cerebral hypoxia. J Neurochem 31: 757–760
Parfenova H, Shibata M, Zuckerman S, Mirro R, Leffler CW 1993 Cyclic nucleotides and cerebrovascular tone in newborn pigs. Am J Physiol 265:H1972–H1982
Lust WD, Mrsulja BB, Mrsulja BJ, Passonneau JV, Klatzo I 1975 Putative neurotransmitters and cyclic nucleotides in prolonged ischemia of the cerebral cortex. Brain Res 98: 394–399
Marks KA, Mallard EC, Roberts I, Williams CE, Sirimanne ES, Johnston B, Gluckman PD, Edwards AD 1996 Delayed vasodilation and altered oxygenation after cerebral ischemia in fetal sheep. Pediatr Res 39: 48–54
Hillered L, Ernster L, Siesjo BK 1984 Influence of in vitro lactic acidosis and hypercapnia on respiratory activity of isolated rat brain mitochondria. J Cereb Blood Flow Metab 4: 430–437
White BC, Grossman LI, Krause GS 1993 Brain injury by global ischemia and reperfusion: a theoretical perspective on membrane damage and repair. Neurology 43: 1656–1665
Rosenberg AA, Murdaugh E, White CW 1989 The role of oxygen free radicals in postasphyxia cerebral hyperperfusion in newborn lambs. Pediatr Res 26: 215–219
Kleihues P, Kobayashi K, Hossmann KA 1974 Purine nucleotide metabolism in the cat brain after one hour of complete ischemia. J Neurochem 23: 417–425
Sankaran K, Peters K, Finer N 1981 Estimated cerebral blood flow in term infants with hypoxic-ischemic encephalopathy. Pediatr Res 15: 1415–1418
Van Bel F, Dorrepaal CA, Benders MJNL, Zeeuwe PEM, Van de Bor M, Berger HM 1993 Changes in cerebral hemodynamics and oxygenation in the first 24 hours after birth asphyxia. Pediatrics 92: 365–372
Lou HC, Lassen NA, Tweed WA, Johnson G, Jones M, Palahniuk RJ 1979 Pressure passive cerebral blood flow breakdown of the blood brain barrier in experimental fetal asphyxia. Acta Pediatr Scand 68: 57–62
Ginsberg MD, Myers RE 1972 The topography of impaired microvascular perfusion in the primate brain following total circulatory arrest. Neurology 22: 998–1011
del Zoppo GJ 1994 Microvascular changes during cerebral ischemia and reperfusion. Cerebrovasc Brain Metab Rev 6: 47–95
Krause GS, White BC, Aust SD, Nayini NR, Kumar K 1988 Brain cell death following ischemia and reperfusion: a proposed biochemical sequence. Crit Care Med 16: 714–726
Vannucci RC, Duffy TE 1977 Cerebral metabolism in newborn dogs during reversible asphyxia. Ann Neurol 1: 528–534
Rosenberg AA 1986 Cerebral blood flow and O2 metabolism after asphyxia in neonatal lambs. Pediatr Res 20: 778–782
Leffler CW, Thompson CC, Armstead WM, Mirro R, Shibata M, Busija DW 1993 Superoxide scavengers do not prevent ischemia induced alteration of cerebral vasodilation in piglets. Pediatr Res 33: 164–170
Pourcyrous M, Mirro R, Busija D, Leffler C 1990 Brain superoxide anion generation during asphyxia and reventilation in newborn pigs. Pediatr Res 28: 618–621
Leffler CW, Beasley DG, Busija DW 1988 Cerebral ischemia alters cerebral microcirculation in newborn pigs. Am J Physiol 257:H266–H271
Acknowledgements
The authors acknowledge the excellent technical assistance of Stanley Lopez, Alex Fedinec, and Mildred Jackson. We also thank Kristopher Arheart for performing statistical analyses and Roz Griffin for editorial assistance.
Author information
Authors and Affiliations
Additional information
Supported in part by grants-in-aid from the American Heart Association-Tennessee Affiliate, the National Institutes of Health, the Obstetrics and Gynecology Special Education Fund, the LeBonheur Children's Medical Center small grant, and a fund from UT Medical Group research grant program.
Rights and permissions
About this article
Cite this article
Pourcyrous, M., Parfenova, H., Bada, H. et al. Changes in Cerebral Cyclic Nucleotides and Cerebral Blood Flow during Prolonged Asphyxia and Recovery in Newborn Pigs. Pediatr Res 41, 617–623 (1997). https://doi.org/10.1203/00006450-199705000-00003
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199705000-00003
This article is cited by
-
The effects of sodium bicarbonate infusion on cerebrovascular function in newborn pigs
Pediatric Research (2022)
-
Does prolonged severe hypercapnia interfere with normal cerebrovascular function in piglets?
Pediatric Research (2018)
-
Milrinone, dobutamine or epinephrine use in asphyxiated newborn pigs resuscitated with 100% oxygen
Intensive Care Medicine (2010)
-
Dose-response effects of milrinone on hemodynamics of newborn pigs with hypoxia-reoxygenation
Intensive Care Medicine (2008)
-
Perinatal asphyxia: Timing and mechanisms of injury in neonatal encephalopathy
Current Neurology and Neuroscience Reports (2001)