Abstract
The involvement of protein kinase C (PKC) and protein tyrosine kinase (PTK) in hypercapnia-induced cerebral vasodilation in newborn pigs was investigated with closed cranial windows using the PKC stimulator phorbol 12-myristate 13-acetate (PMA), and the PTK inhibitors, genistein and herbimycin A. The influence of prostaglandin I2 was eliminated using the prostaglandin cyclooxygenase inhibitor, indomethacin. Changes in pial arteriolar diameters in response to hypercapnia [partial pressure of arterial CO2 ≃ 9.3 kPa (70 torr)] were analyzed. Genistein (40 μg/mL), herbimycin A (10μM), or PMA (1 μM) did not affect cerebral vasodilation to hypercapnia when applied topically. Indomethacin (5 mg/kg i.v.) treatment blocked the dilation to hypercapnia and attenuated hypercapnia-induced increase in cortical cAMP. Genistein and herbimycin A restored the response to hypercapnia to indomethacin-treated piglets. PMA also restored the pial arteriolar dilation and the cAMP response to hypercapnia to indomethacin-treated piglets. One-hour exposure to 10 μM PMA, to down-regulate PKC, blocked vasodilation to hypercapnia but did not inhibit vasodilation to sodium nitroprusside. After prolonged (2 h) topical exposure of indomethacin-treated piglets to 10 μM PMA, neither genistein nor iloprost could restore dilation to hypercapnia. These results indicate that PKC stimulation and/or PTK inhibition may permit hypercapnia-induced vasodilation. These data further suggest that PKC is downstream from PTK in the regulatory pathway. Because previous data showed prostaglandin I2 at subdilator concentrations can also return dilation to hypercapnia to piglets treated with indomethacin, prostaglandin I2 could provide its permissive input by activating PKC and/or inhibiting PTK.
Similar content being viewed by others
Main
Current evidence, largely from newborn pigs, suggests that cerebral prostanoids play a role in the regulation of neonatal cerebral hemodynamics(1). In newborn pigs, hypercapnia elicits vasodilation that is accompanied by increased prostanoid synthesis and is inhibited by the prostaglandin cyclooxygenase inhibitor indomethacin(2–5). Prostacyclin (prostaglandin I2) has been shown to have a permissive role in hypercapnic vasodilation(6). By permissive it is meant that prostacyclin does not act directly, but permits or initiates a series of events resulting in vasodilation. Thus, the prostacyclin receptor agonist, iloprost, at a constant, subdilator concentration restores the cerebral vasodilation that has been blocked by indomethacin(6). Also, in newborn pigs, cyclic nucleotides are involved in cerebral vasodilation in response to hypercapnia via a prostanoid-dependent mechanism(7). Prostacyclin can cause an increase in cAMP through receptor-mediated activation of adenylyl cyclase(13). However, the mechanism of the permissive action of prostaglandin I2 is not known, because the prostacyclin concentration necessary to return the dilation to hypercapnia after indomethacin treatment is insufficient to increase cAMP. Indomethacin not only inhibits the vasodilation to hypercapnia, but also inhibits the increase in cAMP produced by hypercapnia in the cerebral microvasculature and surrounding cells(7, 13), suggesting that the effect of indomethacin is, at least in part, to inhibit the elevation in vascular smooth muscle cAMP produced by hypercapnia. Therefore, it is likely that the mechanism by which prostacyclin plays its permissive role in hypercapnic cerebral vasodilation in the piglet is functionally at or upstream from the vascular smooth muscle adenylyl cyclase.
Phosphorylation is used by prokaryotic and eukaryotic cells to control the properties of a wide variety of proteins, including enzymes, receptors, ion channels, and regulatory and structural proteins. Due to its reversibility, protein phosphorylation can act as a regulatory mechanism. The steady-state level of phosphorylation of a protein reflects the ratios of its rates of phosphorylation and dephosphorylation; these rates depend on the intrinsic activity of the kinase(s) and phosphatase(s) for which the protein is a substrate. The protein kinases most commonly studied in eukaryotic cells phosphorylate the hydroxyamino acids serine, threonine, and tyrosine(8–10). The relative level of tyrosine phosphorylation is balanced by the antagonistic actions of the protein-tyrosine kinases and the protein-tyrosine phosphatases(11).
The present study was designed to address the hypothesis that the permissive role of prostacyclin in hypercapnia-induced cerebral vasodilation involves intermediate kinase phosphorylation of key proteins in the vascular smooth muscle. Therefore, in newborn pigs, the roles of tyrosine kinases and PKCs in signal transduction associated with hypercapnic cerebral vasodilation were investigated in vivo using the PKC stimulator PMA, and the PTK inhibitors genistein and herbimycin A.
METHODS
All protocols involving animals were approved by the Animal Care and Use Committee of the University of Tennessee, Memphis.
Newborn pigs (1-3 d old) were anesthetized with ketamine hydrochloride (33 mg/kg, intramuscularly) and acepromazine (3.3 mg/kg, intramuscularly) and maintained on α-chloralose (50 mg/kg, i.v., initially plus 5 mg/kg each hour). The animals were intubated via tracheotomy and ventilated with air. Catheters were inserted in a femoral artery for monitoring the blood pressure and drawing samples for blood gases and pH analysis and in a femoral vein for administering drugs and fluids. Rectal temperature was maintained between 37 and 38°C using a heating pad. pH and blood gases were maintained within the normal limits except during hypercapnia. The head was immobilized, the scalp was incised and retracted, and a hole 2 cm in diameter was made in the skull over the parietal cortex. The dura was cut without touching the brain, and all cut edges were retracted over the bone so that the periarachnoid space was not exposed to bone or damaged membranes. A stainless steel and glass cranial window with inlet and outlet ports was placed in the hole and cemented into place with dental acrylic. The space under the window was filled with aCSF. The aCSF composition was (in mM): 132.0 NaCl, 3.0 KCl, 1.5 MgCl2, 2.5 CaCl2, 6.6 urea, 3.7 dextrose, and 24.6 NaHCO3. The aCSF was warmed to 37°C and bubbled with a gas mixture of 6% CO2 and 6% O2 in N2 and typically had a pH range of 7.33-7.44 and a Pco2 and Po2 in the ranges of 5.5-6.1 kPa (41-46 mm Hg) and 5.7-6.7 kPa (43-50 mm Hg), respectively. The volume of the fluid directly under the window was 500 μL and was contiguous with the periarachnoid space. After implantation of the window, at least 30 min were allowed for exchange and equilibrium of fluid under the window with interstitial and subarachnoid fluids before experimentation was begun. Pial arteriolar diameter was measured with a video micrometer coupled to a television camera mounted on the microscope and a video monitor. Several pial arterioles (n = 2-4), 40-140 μm in diameter, in each animal were selected for observation. The mean of the vessel diameters was considered one observation so that n = number of piglets.
Materials. Indomethacin trihydrate (gift from Merck Sharp & Dohme Research Laboratories, Rahway, NJ) was dissolved in normal saline. PMA(Sigma Chemical Co.) was dissolved in DMSO to give a stock solution of 1 mM, and final dilution was made with aCSF. Genistein (Sigma Chemical Co. and Calbiochem) dissolved in DMSO (25 μL for 1 mg) was diluted with aCSF to give 40 μg/mL; herbimycin A (Sigma Chemical Co.) dissolved in DMSO (100μM stock) was diluted with aCSF. HMG (Sigma Chemical Co.) and phenylarsine oxide (Sigma Chemical Co.) were initially dissolved in DMSO, and final working dilutions (100-300 mM and 5-15 mM, respectively) were made in aCSF. Iloprost(3 × 10-4 M; gift from Schering Pharmaceutical Research) was initially diluted with sterile water and finally with aCSF to a working dilution of 10-12 M.
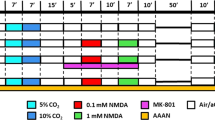
Experimental design. The experimental design, shown graphically in Figure 1, consisted of initial measurements and hypercapnia, administration of indomethacin, repeated measurements and hypercapnia, and topical administration of drug followed by repeated measurements and hypercapnia. The topical drug was either genistein (40μg/mL), herbimycin A (10 μM), or the phorbol ester PMA (1 μM). Other animals were treated with genistein or herbimycin A before administering indomethacin. PMA directly stimulates PKC, whereas herbimycin A and genistein are inhibitors of PTK. Another group of animals was treated with HMG (100-300 mM) or phenylarsine oxide (5-15 mM) after initial hypercapnia.
Experimental design. Indomethacin was given at 5 mg/kg, i.v., and repeated at 90-min intervals. Treatments: PMA (1 μM) was placed in the aCSF under the cranial window beginning 20 min before the control period. It was removed and returned, as its effects were reversible (see“Results”). Genistein (40 μg/mL) was placed in the aCSF under the cranial window beginning 20 min before the control periods and continuing for the remainder of the experiment. Herbimycin A (10 μM) was placed in the aCSF under the cranial window, and 3 h were allowed before resuming experiments and continuing for the remainder of the experiment.Ctl., control (normocapnia); CO2, hypercapnia(Pco2 ≅ 70 mm Hg).
After 10 min (control measurements), hypercapnia was induced by ventilating the piglets with a 10% CO2-21% O2-69% N2 gas mixture for 10 min to increase arterial Pco2 to ≃ 9.3 kPa (70 mm Hg). Pial arteriolar diameter was measured every 2 min during the hypercapnia. After 10 min of hypercapnia, the ventilation gas was returned to room air and the cerebral surface was repeatedly flushed with aCSF over 30 min. Indomethacin (5 mg/kg, i.v.) was given initially after the control CO2 response, and was repeated every 90 min, because previous experiments have shown that the cerebral vascular effectiveness of indomethacin is diminished by 2 h(5). Thirty minutes after indomethacin administration, hypercapnia induction was repeated. About 20 min were allowed for the drug to equilibrate and act, and for the vessels to return to control size after topical PMA or genistein, and 3 h were allowed with herbimycin A.
In the PMA group, in addition to the experiment shown in Figure 1, the vasodilatory response to topical isoproterenol (10-7 M) was recorded before indomethacin treatment and at the end of the experiment. Maximal vasodilation, which usually occurred within 5 min of application, was recorded as the response to isoproterenol. The dose of 10-7 M was selected to produce a readily reversible and highly reproducible vasodilation similar to that produced by 10% CO2. Isoproterenol was used to detect any generalized change in vascular reactivity, because we have found responses to isoproterenol to be consistent over time and not to be affected by indomethacin treatment.
In another set of experiments, prolonged treatment with PMA (10 μM) was used to attempt to down-regulate PKC. PMA (10 μM) treatment caused massive platelet aggregation and severe vasoconstriction that began about 70-80 min after treatment. Removal of PMA at 1 h did not prevent the deterioration. Therefore, in separate animals, the response to hypercapnia or sodium nitroprusside (10-6 M) (control for vascular reactivity) was determined before and after 60 min of PMA treatment (after removal of the PMA). Pial arteriolar vasodilation to hypercapnia was also examined in the presence of 10μM PMA after 30 min of treatment. In indomethacin-treated piglets, 10 μM PMA did not cause platelet aggregation or vasoconstriction. Therefore, 10μM PMA was placed under the window for 2 h with indomethacin. Genistein or iloprost was topically applied subsequently. Pial arteriolar responses to hypercapnia were measured before and after PMA and indomethacin, and after genistein or iloprost.
Cortical periarachnoid CSF (300 μL) was sampled from under the window for examination of cerebral production of cyclic nucleotides. CSF collections were made by slowly infusing aCSF into an inlet port of the cranial window and allowing the CSF to drip freely into a collection tube from an outlet port. The collection tubes contained EDTA (final concentration 5 mM) buffered in Tris base to pH 7.4. Immediately after collection, the CSF samples were frozen and stored at -60°C before assays for cyclic nucleotides. cAMP content in aCSF was determined by RIA, using 125I-cAMP (Amersham Corp.) as a radioligand.
Statistical analysis. All values are presented as means± SEM. Comparisons among populations used analysis of variance with repeated measures. Fisher protected least significant difference was used to determine differences between groups. p < 0.05 was required for inference that the populations were different.
RESULTS
No significant changes in blood gases, pH, or mean arterial blood pressure were observed within or between groups before, during, or after topical administrations of PMA, genistein, or herbimycin A except during hypercapnia compared with normocapnia. Arterial gases, pH, and blood pressures were within normal limits for newborn pigs.
Although genistein (40 μg/mL) topically applied to the cerebral surface is a mild vasodilator of cerebral arterioles (pial arteriolar diameter percent change = 15-20%), it did not alter cerebral vascular dilation in response to hypercapnia (Fig. 2). It is known that in the newborn pigs indomethacin completely inhibits hypercapnia-induced vasodilation(2–5). However, this inhibition was not observed when genistein was given before indomethacin treatment. To further investigate the effect of genistein on hypercapnia-induced vasodilation, we applied genistein after indomethacin treatment (Fig. 3). As expected, cerebral vascular reactivity to hypercapnia was largely inhibited in the presence of indomethacin (5 mg/kg). However, genistein (40 μg/mL) topically applied to the cerebral surface completely restored vasodilation to hypercapnia, in spite of the continued presence of indomethacin.
Effects of topical genistein (40 μg/mL) applied after indomethacin treatment on pial arteriolar diameter responses to hypercapnia (n = 3 piglets). The basal pial arteriolar diameter(mean ± SEM in μm) during normocapnia before indomethacin, after indomethacin, and after indomethacin plus genistein were 70 ± 5, 71± 4 and 78 ± 3, respectively. *p < 0.5 compared with control response; #p < 0.05 compared with no change.
Although herbimycin A (10 μM, topical) produced immediate vasodilation of pial arterioles, which persisted for almost 2 h, by 3 h the baseline diameter was not significantly different from the first control. Further, 3-h treatment with herbimycin A did not alter the cerebral vascular dilation to hypercapnia (Fig. 4). Indomethacin treatment did not inhibit hypercapnia-induced vasodilation when herbimycin A was given before indomethacin administration. To further investigate the effect of herbimycin A on hypercapnia-induced vasodilation, we applied herbimycin A after indomethacin treatment (Fig. 5). Cerebral vascular reactivity to hypercapnia was largely inhibited in the presence of indomethacin (5 mg/kg). Herbimycin A (10 μM) topically applied to the cerebral surface completely restored vasodilation to hypercapnia in spite of the continued presence of indomethacin.
Effects of topical herbimycin A (10 μM) applied after indomethacin treatment on pial arteriolar diameter responses to hypercapnia (n = 6 piglets). The basal pial arteriolar diameter(mean ± SEM in μm) during normocapnia before indomethacin, after indomethacin, and after indomethacin plus herbimycin A were 138 ± 19, 125 ± 17, and 137 ± 25, respectively. *p < 0.05 compared with control; #p < 0.05 compared with zero (no response).
The PKC inhibitor, HMG (100-300 mM), and the tyrosine phosphatase inhibitor, phenylarsine oxide (5-15 mM), are potent vasodilators of cerebral arterioles that altered the baseline diameters to near maximal dilation. The mean ± SEM arteriolar diameters (in μm) were 111 ± 6, 142± 5, and 154 ± 6 for control, hypercapnia, and HMG control, respectively. In the phenylarsine group, these values were 74 ± 22, 100± 22, and 112 ± 27 for control, hypercapnia, and phenylarsine control, respectively. Therefore, it was impossible to evaluate their effect on hypercapnia.
The PKC activator, PMA (1 μM), did not affect either the basal pial arteriolar diameter or dilation in response to hypercapnia when applied topically (pial arteriolar diameter, 86 ± 10 μm and 125 + 9 μm during control and hypercapnia, respectively, in the absence of PMA; 91± 12 μm and 133 ± 13 μm during control and hypercapnia, respectively, in the presence PMA). However, PMA application in the presence of indomethacin completely restored the ability of the vessels to dilate to hypercapnia (Fig. 6). The action of PMA was reversible: upon removal of PMA, arterioles did not significantly dilate in response to hypercapnia in the presence of indomethacin; return of PMA restored the dilation. The vascular reactivity was unchanged by PMA, because the response to topical isoproterenol (10-7 M) remained the same before and after PMA (Fig. 6).
Effects of topical PMA (1 μM) applied after indomethacin treatment on pial arteriolar diameter responses to hypercapnia(n = 7 piglets). The basal pial arteriolar diameter (mean ± SEM in μm) during normocapnia before indomethacin, after indomethacin and after indomethacin plus PMA were 54 ± 4, 54 ± 4, and 54 ± 5, respectively. *p < 0.05 compared with zero (no response);#p < 0.05 compared with before indomethacin.
cAMP production increased with hypercapnia, and this rise was inhibited by indomethacin treatment (Fig. 7). In addition to the ability to restore cerebral vascular reactivity to hypercapnia, PMA also restored the hypercapnia-induced increase in cortical cAMP that had been inhibited by indomethacin treatment.
Prolonged (1 h) treatment with PMA (10 μM) and then removal in piglets not treated with indomethacin blocked pial arteriolar dilation to hypercapnia. Thus, before PMA treatment, pial arterioles dilated 52 ± 7% during hypercapnia but after treatment with PMA the dilation was abolished (-4± 5%) (n = 11). This effect was not due to a generalized decrease in pial arteriolar reactivity, because such PMA treatment did not inhibit dilation to sodium nitroprusside [33 ± 4% before and 34± 9% after PMA treatment, respectively (n = 14)]. Acute PMA(10 μM) treatment of 30-min duration did not alter the baseline pial arteriolar diameter or the vasodilator response to hypercapnia (93 ± 13 to 138 ± 16 μm before and 105 ± 11 to 148 ± 16 μm in the presence of PMA, respectively, n = 6). After 2-h PMA treatment in indomethacin-treated pigs, the vasodilator response to hypercapnia was absent. Further, after this prolonged PMA treatment, neither genistein nor iloprost could restore cerebral dilation to hypercapnia(Table 1).
DISCUSSION
The major new findings of this study are that PKCs and PTKs are involved in the hypercapnic cerebral vasodilation in piglets. PKC stimulation with the phorbol ester, PMA, or PTK inhibition with genistein or herbimycin A resulted in the return of the pial arteriolar dilation response to hypercapnia after blockade by indomethacin. Further, prolonged treatment with PMA to reduce PKC activity inhibits dilation to hypercapnia and prevents restoration of the hypercapnic vasodilation by iloprost or genistein in indomethacin-treated pigs.
Prostanoids appear to be prominent in the cerebral vascular physiology of the newborn pig(1). They can be important not only in the maintenance of resting cerebral blood flow but also in the control of cerebral blood flow during altered physiologic conditions such as hypercapnia and hypotension(2–4). Indomethacin, a prostaglandin cyclooxygenase inhibitor, blocks the production of the prostanoids(5) and inhibits the prostacyclin receptors as well(13).
Endothelially derived signals acting on the vascular smooth muscle are involved in the hypercapnic cerebral vasodilation in newborn pigs. Elevated prostacyclin production in response to hypercapnia occurs in cerebral microvascular endothelial cells but not in smooth muscle cells or glial cells(14). Light/dye microvascular injury eliminates hypercapnia-induced vasodilation, but not responses to isoproterenol or sodium nitroprusside(15).
Indomethacin abolishes hypercapnic cerebral vasodilation(5). In contrast, the nitric oxide synthase inhibitors NG-methyl-L-arginine,Nω-nitro-L-arginine, and L-Nω-nitro-L-arginine methyl ester do not block this vasodilatory response(7). Therefore, the endothelial signal in hypercapnic cerebral vasodilation appears to be prostacyclin(7) rather than EDRF-nitric oxide as it is in adults of some species(26–29).
The involvement of prostacyclin in specific vasodilatory responses appears to be a permissive one rather than directly causing dilation(6). By permissive it is meant that prostacyclin does not act directly, but permits or initiates a series of events resulting in vasodilation. Thus, the prostacyclin receptor agonist, iloprost, at a constant, subdilator concentration restores the cerebral vasodilation that has been blocked by indomethacin(6). Iloprost also resurrects cerebral vasodilation in response to both hypercapnia and histamine after endothelial injury(16). Other examples of similar permissive actions in the control of the cerebral circulation have also been identified(17, 18, 22). The permissive action of prostacyclin could involve one or more of the many intermediate kinases and second messengers. Prostacyclin could activate phospholipase C(19), resulting in production of DAG, an endogenous PKC activator. It is known that in some cells and tissues cAMP production can be stimulated by the activation of PKC (serine/threonine kinase)(10, 12). An increase in periarachnoid cAMP is seen with hypercapnic cerebral vasodilation; this increase is blocked by indomethacin treatment(7). Hypercapnia produces only a moderate increase in cAMP in isolated smooth muscle cell cultures by prostanoid-independent mechanisms but produces a large increase in cAMP in cocultures of endothelial and smooth muscle cells(20). PKCs have been shown to sensitize adenylyl cyclase pathways, producing augmented responses to other stimuli(30–36). PKCs might act via phosphorylation of an inhibitory G protein or phosphorylation of adenylyl cyclase or both. In our experiments, PMA treatment could be substituted for the prostacyclin analog in reversing the indomethacin-induced blockade of hypercapnic cerebral vasodilation and CO2-induced cAMP production. However, PKC blockers resulted in maximal dilatation, thus preventing experimentation using pharmacologic inhibition of PKC. These data did, however, suggest that some PKCs might be involved in the maintenance of basal tone in the cerebral vasculature.
Protein kinases are involved in cellular responses to extracellular signals, and they have been implicated in the dynamic regulation of cellular metabolism. Stimulation of signaling cascades results in the activation of protein kinases, which in turn phosphorylate their respective substrates(8–10). Protein phosphatases dephosphorylate phosphoserine-, phosphothreonine-, and phosphotyrosine-containing proteins, thereby maintaining tight regulation(11). Compartmentalization of various kinases has been shown to be due to specific anchoring proteins within the cell(21).
In addition to the PKC pathway, tyrosine kinase signal transduction systems have been shown to be indispensable for different stages of cell proliferation in cell culture models(24). Lamb cerebral arteries were shown to exhibit differential sensitivity to PKC and PTK inhibition induced by staurosporine and genistein, respectively(25). Norepinephrine-induced contractions were abolished in both fetal and newborn lamb cerebral arteries by pretreatment with staurosporine; but pretreatment with genistein depressed contraction only in newborn, and not in fetal, arteries(25). In our experiments, genistein and herbimycin A, both PTK inhibitors, were able to restore hypercapnic cerebral vasodilation after indomethacin-induced blockade and hence could be substituted for the prostacyclin analog.
In the kinase cascade, the action of PTK might precede that of PKC or vice versa and there are studies to suggest both(23, 37–39). In fact, PTK and PKC may not necessarily be associated serially. A hypothetical model with the putative mechanisms involved in hypercapnic cerebral vasodilation is depicted in Figure 8. PTK might have an inhibitory effect on phospholipase C or DAG, with DAG activating PKC, thereby phosphorylating adenylyl cyclase and/or an inhibitory G protein. Prostacyclin receptor stimulation may result in stimulation of DAG via phospholipase C activation or by inhibiting the inhibitory action of PTK.
Because we could not inhibit PKC or increase the effect of PTK pharmacologically without producing dilation, we attempted to partially down-regulate PKC under the cranial window by prolonged treatment with PMA. In the absence of indomethacin, only 1 h of PMA treatment was possible before extensive platelet aggregation, initially in the veins, and complete shut down of circulation under the window. However, before platelet aggregation and vascular collapse, pial arteriolar dilation to hypercapnia was absent but dilation to sodium nitroprusside was intact. These data suggest selective inhibition of hypercapnia-induced cerebral vasodilation, possibly as a result of down-regulation of a PKC. In the presence of indomethacin more prolonged treatment with PMA did not cause platelet aggregation or vascular collapse. But the PMA treatment was not without effect. In indomethacin-treated piglets with presumably down-regulated PKC, due to continued or prolonged presence of PMA, neither iloprost nor genistein could return the dilation in response to hypercapnia. These data suggest that the mechanism by which stimulation of prostacyclin receptors and inhibition of PTK permit hypercapnic vasodilation involves PKC. These data may further suggest that PKC is downstream from PTK in the regulatory pathway.
Abbreviations
- CSF:
-
cerebrospinal fluid
- aCSF:
-
artificial cerebrospinal fluid
- EDRF:
-
endothelium-derived relaxing factor
- HMG:
-
1-O-hexadecyl-2-O-methylglycerol
- PKC:
-
protein kinase C
- PMA:
-
phorbol 12-myristate 13-acetate
- PTK:
-
protein tyrosine kinase
- Pco2:
-
partial pressure of arterial CO2
- Po2:
-
partial pressure of arterial O2
- DAG:
-
diacylglycerol
References
Leffler CW, Busija DW 1987 Arachidonic acid metabolites and perinatal cerebral hemodynamics. Semin Perinatol 11: 3142
Leffler CW, Busija DW 1985 Prostanoids in cortical subarachnoid cerebrospinal fluid and pial artery diameter in newborn pigs. Circ Res 57: 689–694.
Wagerle LC, Mishra OP 1988 Mechanisms of CO2 response in cerebral arteries of the newborn pig: role of phospholipase, cyclooxygenase, and lipooxygenase pathways. Circ Res 62: 1019–1026.
Leffler CW, Armstead WM, Shibata M 1993 Role of eicosanoids in cerebral hemodynamics. In: Phillis JW (ed) The Regulation of Cerebral Blood Flow, Chap. 19. CRC Press, Boca Raton, FL, pp 217–313.
Leffler CW, Mirro R, Shibata M, Parfenova H, Armstead WM, Zuckerman S 1993 Effects of indomethacin on cerebral vasodilator responses to arachidonic acid and hypercapnia in newborn pigs. Pediatr Res 33: 609–614.
Leffler CW, Mirro R, Pharris LJ, Shibata M 1994 Permissive role of prostacyclin in cerebral vasodilation to hypercapnia in newborn pigs. Am J Physiol 267:H285–H291.
Parfenova H, Shibata M, Zuckerman S, Leffler CW 1994 CO2 and cerebral circulation in newborn pigs: cyclic nucleotides and prostanoids in vascular regulation. Am J Physiol 266:H1494–H1501.
Girault J-A 1994 Protein kinases and phosphatases. Neurotransmissions 10: 1–6.
Pawson T 1994 Introduction: protein kinases. FASEB J 8: 1112–1113.
Jacobowitz O, Iyengar R 1994 Phorbol ester-induced stimulation and phosphorylation of adenyl cyclase 2. Proc Natl Acad Sci USA 91: 10630–10634.
Stone RL, Dixon JE 1994 Protein-tyrosine phosphatases. Minireview. J Biol Chem 269: 31323–31326.
Morimoto BH, Koshland DE 1994 Conditional activation of cAMP signal transduction by protein kinase C. J Biol Chem 269: 4065–4069.
Parfenova H, Hsu P, Leffler CW 1995 Dilator prostanoid-induced cyclic AMP formation and release by cerebral microvascular smooth muscle cells: inhibition by indomethacin. J Pharmacol Exp Ther 272: 44–52.
Hsu P, Shibata M, Leffler CW 1993 Prostanoid synthesis response to high CO2 in the newborn pig brain microvascular endothelial cells. Am J Physiol 264:H1485–H1492.
Leffler CW, Mirro R, Shanklin DR, Armstead WM, Shibata M 1994 Light/dye microvascular injury selectively eliminates hypercapnia-induced pial arteriolar dilation in newborn pigs. Am J Physiol 266:H623–H630.
Leffler CW, Fedinec AL, Shibata M 1995 Prostacyclin receptor activation and pial arteriolar dilation following endothelial injury in piglets. Stroke 26: 2103–2111.
Wagerle LC, Degiulio PA 1994 Indomethacin-sensitive CO2-reactivity of cerebral arterioles is restored by dilator prostaglandin. Am J Physiol 266:H1332–H1338.
Armstead WM, Mirro R, Busija DW, Leffler CW 1989 Permissive role of prostanoids in acetylcholine-induced cerebral constriction. J Pharmacol Exp Ther 251: 1012–1019.
Namba T, Oida H, Sugimoto Y, Kakizuka A, Negishi M, Ichikawa A, Narumiya S 1994 cDNA cloning of mouse prostacyclin receptor. Multiple signaling pathways and expression in thymic medulla. J Biol Chem 269: 9986–9992.
Parfenova H, Leffler CW 1995 Effects of hypercapnia on dilator prostanoid and cyclic AMP production by cerebral microvascular endothelial and smooth muscle cell cultures. Am J Physiol 270:C1503–C1510.
Mochly-Rosen D 1996 Localization of protein kinases by anchoring proteins: a theme in signal transduction. Science 268: 247–250.
Iadecola C, Zhang F, Xu X 1994 SIN-1 reverses attenuation of hypercapnic cerebro-vasodilation by nitric oxide synthase inhibitors. Am J Physiol 267:R228–R235.
Kozawa K, Suzuku A, Oiso Y 1995 Tyrosine kinase regulates phospholipase D activation at a point downstream from protein kinase C in osteoblast-like cells. J Cell Biochem 57: 251–255.
Murate T, Sage S, Hamaguchi M, Asano H, Ito T, Watanabe T, Adachi K, Koizumi KT, Yoshida S, Saito H, Hotta T 1995 Herbimycin A inhibits phorbol ester-induced morphological changes, adhesion and megakaryocytic differentiation of the leukemia cell line, MEG-01. Proc Soc Exp Biol Med 209: 270–278.
Wagerle LC, Moliken W, Russo P 1994 Developing lamb cerebral arteries exhibit differential sensitivity to inhibitors of protein kinase C and tyrosine kinase. FASEB J 8:A558.
Hardelo JE, Kahrstrom J, Owman C, Salford LG 1987 Endothelium-dependent relaxation by uridine tri- and diphosphate in isolated human pial vessels. Blood Vessels 24: 150–155.
Katusic ZS, Shepherd JT, Vanhoutte PM 1984 Vasopressin causes endothelium-dependent relaxations of the canine artery. Circ Res 55: 575–579.
Nishimura H, Rosenblum WI, Nelson GH, Boyriton S 1991 Agents that modify EDRF formation alter antiplatelet properties of brain arteriolar endothelium in vivo. Am J Physiol 261:H15–H21.
Wei EP, Ellis EF, Kontos HA 1980 Role of prostaglandins in pial arteriolar responses to CO2 and hypoxia. Am J Physiol 238:H226–H230.
Gordeladze JO, Bjoro T, Torjesen PA, Ostberg BC, Haug E, Gautvik KM 1989 Protein kinase C stimulates adenylate cyclase activity in prolactin-secreting rat adenoma (GH4C1) pituicytes by inactivating the inhibitory GTP-binding protein Gi . Eur J Biochem 183: 397–406.
Yoshimasa T, Sibley DR, Bouvier M, Lefkowitz RJ, Caron MG 1987 Cross-talk between cellular signaling pathways suggested by phorbol-ester-induced adenylate cyclase phosphorylation. Nature 327: 67–70.
Johnson RA, Towes ML 1990 Protein kinase C activators sensitize cyclic AMP accumulation by intact 1321 N1 human astrocytoma cells. Mol Pharmacol 37: 296–303.
Johnson JA, Friedman J, Halligan RD, Birnbaumer M, Clark RB 1991 Sensitization of adenylyl cyclase by P2 purinergic and M5 muscarinic receptor agonists in L cells. Mol Pharmacol 39: 539–546.
Watson EL, Jacobson K, Meir K 1993 Phorbol ester has different effects on forskolin and beta-adrenergic stimulated cAMP accumulation in mouse parotid acini. Cell Signal 5: 583–592.
Cote S, Van Sande J, Boeynaems JM 1993 Enhancement of endothelial cAMP accumulation by adenine nucleotides: role of methylxanthine-sensitive sites. Am J Physiol 264:H1498–H1503.
Iyengar R 1993 Molecular and functional diversity of mammalian Gs-stimulated adenylyl cyclases. FASEB J 7: 768–775.
Ting CC, Hargrove ME, Wang J, Patel AD 1995 Differential requirement of protein tyrosine kinase and protein kinase C in the generation of IL-2 induced LAK cell and a CD 3-AK cell responses. Cell Immunol 160: 286–296.
Paul A, Pendreigh RH, Plevin R 1995 Protein kinase C and tyrosine pathways regulate lipopolysaccharide-induced nitric oxide synthase activity in RAW 264.7 murine macrophages. Br J Pharmacol 114: 482–488.
Khalil RA, Menice CB, Wang CLA, Morgan KG 1995 Phosphotyrosine-dependent targeting of mitogen-activated protein kinase in differentiated contractile vascular cells. Circ Res 76: 1101–1108.
Acknowledgements
The authors thank Mildred Jackson, Alex Fedinec, and Stanley Lopez for their technical assistance; Danny Morse and Laura Malinick for the illustrations; Jin Emerson-Cobb for editorial assistance, and Maria Swayze for her secretarial assistance.
Author information
Authors and Affiliations
Additional information
Supported by National Institutes of Health Grants HL42851 and HL34059.
Rights and permissions
About this article
Cite this article
Rama, G., Parfenova, H. & Leffler, C. Protein Kinase Cs and Tyrosine Kinases in Permissive Action of Prostacyclin on Cerebrovascular Regulation in Newborn Pigs. Pediatr Res 41, 83–89 (1997). https://doi.org/10.1203/00006450-199701000-00013
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199701000-00013