Abstract
The effect of hypoxia-ischemia (HI) on IL-1, and IL-6 bioactivity in relation to expression of IL-1α, IL-1β, and IL-6 mRNA was studied, and the neuroprotective efficacy of IL-1 receptor antagonist (IL-1ra) was evaluated in neonatal rats. HI was induced in 7-d-old rats by unilateral carotid artery ligation and hypoxia for 70-100 min. Animals were killed at different time points up to 14 d after HI, and brains were analyzed for IL-1 and IL-6 bioactivity using bioassays and for mRNA for IL-1α, IL-1β, and IL-6 with reverse transcription followed by a polymerase chain reaction. In separate animals, IL-1ra was administered intracerebrally before or after HI, and the extent of brain injury was assessed 14 d after HI. A transient increase of IL-1 bioactivity occurred after HI, reaching a peak at 6 h of recovery. IL-1β mRNA followed a similar time course but attained maximum expression at 3 h. IL-6 bioactivity and mRNA were also stimulated by HI and followed a similar time course as IL-1. Pretreatment with IL-1ra reduced HI brain damage from 54.5 ± 9.3 to 41.4 ± 10.0% (p ≤ 0.01), and IL-1ra posttreatment increased the proportion of animals devoid of brain injury (40%) compared with vehicle-treated controls (13%) (p≤ 0.05). In conclusion, a transient activation of IL-1 and IL-6 occurred after HI, and IL-1ra reduced HI brain injury to a moderate degree.
Similar content being viewed by others
Main
Recent studies indicate that immunoinflammatory mechanisms are important in the biochemcal cascade leading to brain injury after hypoxic episodes(1–3). Cytokines, regulatory peptides of the immune system, have been implicated as participating in the inflammatory response to HI(4). In the adult brain, mRNA for the proinflammatory cytokine IL-1β is expressed after ischemia in animals(5–7), and IL-1β immunoreactivity is increased in the cerebrospinal fluid of patients suffering from ischemic insults(c8, c9). IL-1β is neurotoxic if applied to the brain, the IL-1ra reduces excitotoxic and ischemic brain injuries(10), and overexpression of IL-1ra induced by an adenoviral vector attenuates ischemic injuries(11), suggesting that IL-1 is involved in the processes leading to brain injury.
The properties of the immune system changes during maturation(12, 13), which makes it important to specifically evaluate the role of cytokines for development of perinatal brain injuries in the newborn(14). It was recently found that IL-1β mRNA(15) is expressed in CNS after HI in 7-d-old rats, and high doses of systemic IL-1ra reduced injury formation in the same model(16). It is well recognized that IL-1 production is regulated both at the transcriptional and translational level(17) meaning that mRNA expression is not necessarily accompanied by production of IL-1 bioactive protein, especially not after HI when protein synthesis is known to be severely depressed(18, 19). It is therefore important to study the IL-1 bioactivity in relation to IL-1α and β mRNA expression after HI. Systemically administered IL-1ra could have effects on carbohydrate metabolism, temperature control, and the immune system outside the CNS which in turn may affect the extent of brain injuries(17). It is therefore warranted to complement these studies with evaluation of the neuroprotective effect of IL-1ra administered intracerebrally.
IL-6 is a cytokine that has never been studied before in relation to HI in newborns. It is generally considered that IL-6 is a proinflammatory cytokine as the levels often correlate to the severity of the infectious disease(17) and to the extent of brain lesion after ischemia in patients(8, 9). The production of IL-6 is often triggered by IL-1 and these two cytokines often respond to the same pathologic insults, but the IL-6 increase is often more protracted, and significant concentrations appear in the blood stream(20). In contrast to IL-1β, IL-6 lacks direct toxicity(17), activates anti-proteases(17), inhibits lipopolysaccharide-induced TNF-α(21), and stimulates circulating IL-1ra and soluble TNF receptor(22), suggesting that IL-6 may also have anti-inflammatory properties. Recently, IL-6 was found to suppress demyelination(23) and to reduceN- methyl-D-aspartate-receptor toxicity and ischemic damage in vivo in adult animals(24). It may therefore be of interest to study changes in IL-6 bioactivity and IL-6 mRNA in relation to IL-1 after neonatal HI.
METHODS
Model of HI
Ipsilateral HI was induced in 7-d-old rats (Wistar strain, both sexes) as follows(25, 26). The pups were anesthetized with halothane [3% for induction and 1-1.5% for maintenance in a mixture of nitrous oxide and oxygen (1:1)]. The left common carotid artery was dissected and cut between double ligatures of prolene sutures (6-0). The duration of anesthesia was less than 10 min. The pups were left to recover for at least 1 h and then placed in a chamber perfused with a humidified gas mixture (7.70 ± 0.01% oxygen in nitrogen) for 70 min (posttreatment with IL-1ra) or 100 min(measurement of cytokines and pretreatment with IL-1ra). The temperature in the gas chamber was 36 °C. After hypoxic exposure the pups were returned to their biologic dams until they were killed. All animal experiments were approved by the ethical Committee of Göteborg (no. 34-94).
Evaluation of the Effect of IL-1ra on HI Brain Injury, Blood Glucose, and Core Temperature
Human recombinant IL-1ra was kindly supplied by Amgen Inc., Boulder, CO. A dose of IL-1ra (3.3 μg/rat pup for pretreatment and 5 μg for posttreatment) was dissolved in 1 μL of vehicle (10 mM Na-citrate, 140 mM NaC1, EDTA, pH 6.5) and administered to the left hemisphere (1.5 mm lateral to Bregma and 4 mm below the cortical surface) using a 0.4-mm diameter sterile cannula before or immediately after HI. Control pups within each litter received vehicle without IL-1ra. Brain injury was evaluated after 14 d by brain weight and was expressed as the unilateral hemisphere weight deficit as the percentage of the contralateral noninjured hemisphere(26). To determine the degree of physiologic asymmetry between hemispheres, 20 rat pups not subjected to HI were killed at postnatal d 21, the hemispheric were weighed, and the 95% confidence interval of the left hemispheric weight deficit as the percentage of the right hemispheric weight was estimated to be -4.5 to +2.5%.
The core temperature was measured 0, 1, and 2 h after HI in a separate series of IL-1ra-pretreated (3.3 μg/rat pup) and control (vehicle) animals(n = 5/time point and group) using a thermocouple (Physitemp, BAT-12, cupper/constantan). The temperature (mean ± SD) in the IL-1ra group (0 h, 34.7 ± 0.2; 1 h, 31.7 ± 1.3; 2 h, 34.4 ± 1.1) was not different from control (0 h, 34.3 ± 0.3; 1 h, 31.5 ± 1.2; 2 h, 33.3 ± 2.6 °C). Blood glucose 2 h after HI was 4.3± 0.7 (n = 5) in the IL-1ra-treated and 4.2 ± 1.0(n = 5) in the vehicle control group (not significant).
Cytokine Analysis in Tissue Specimens
Animals were killed at 1, 3, 6, 10, 20, and 48 h, and at 14 d after HI. Animals from each litter were killed at different time intervals to reduce the confounding effect of inter-litter variability. Control animals were killed at postnatal d 7. The brains were dissected out, and the hemispheres were separated, weighed, frozen in liquid nitrogen, and stored at -70 °C until analyzed.
Tissue extraction. Brain tissue was weighed and pulverized, and proteins were extracted in saline (1:10, w/v) as described for other rat tissues(27), and mRNA was extracted as described below.
IL-1 bioactivity. IL-1 bioactivity was measured with a lymphocyte-activating factor assay using thymocytes from NMRI/KI mice(27). The mouse thymus was removed aseptically after sacrificing the animal, and thymocytes were prepared according to Granholmet al.(27). The cell concentration was adjusted to 4 × 106 cells/mL, and the cell suspension was distributed in 100-μL volumes to 96-well microtiter plates. A standard preparation of rat IL-1 (see below) or sample was added in 10-μL volumes. Dose response curves were established on the basis of six different concentrations of a IL-1 standard prepared as described from rat testes and titrated against human recombinant IL-1α(27, 28). The cells were incubated for 48 h at 37 °C, and tritiated thymidine (0.5 μCi/well, Amersham, Sweden) was added for the last 2 h of incubation. Thymocyte proliferation (lymphocyte-activating factor activity) was assessed as incorporation of [3H]thymidine, and bioactivity was expressed in arbitrary units. This bioassay responds to IL-1α and IL-1β, but not to IL-6 and several other cytokines(27).
IL-6 bioactivity. Bioactivity of IL-6 was assayed using a 7TDI hybridoma cell line(29). Cells (2 × 104 cells/mL) were suspended in culture medium without IL-6, and 100-μL aliquots of cell suspension were added to a 96-well plate with serial dilutions of samples in the same volume. Mouse IL-6 (Genzyme; Novakemi AB, Stockholm, Sweden) was used as a standard, beginning with 1 μg/well and then diluted 10-fold in eight steps. After 3 d at 37 °C in 6% CO2, the cultures were pulsed with 1 μCi of [3H]thymidine in 10 μL of PBS and further incubated for 6 h. The cultures were harvested onto glass fiber strips with an automated cell harvester. Filter strips were dried, individual filter disks were transferred to vials, and scintillation liquid was added. The radioactivity was determined with a scintillation counter, and bioactivity was expressed in arbitrary units.
Neutralization of IL-1 bioactivity from rat brain. Extracted protein from rat brain (subjected to HI) producing 80% of maximal IL-1 bioactivity was used to stimulate murine thymocytes in IL-1 bioassay as described above. In one set of experiments, different concentrations of a rabbit hyperimmune antiserum against murine IL-1α (Genzyme) which cross-reacts with rat IL-1α according to the supplier's data and our own experience. A 1:50 dilution of this antiserum has been reported to neutralize 10 units of mouse IL-1α. The antiserum was preincubated with the rat brain protein extract for 1.5 h at room temperature and then added to the IL-1 bioassay. Normal rabbit serum was used as control and was found not to inhibit rat brain IL-1 bioactivity. In another set of experiments, a human recombinant IL-1ra in different doses (Bachem Feinchemikalien AG, Bubendorf, Switzerland) was coincubated with the rat brain protein extract. This preparation of IL-1ra has previously been found to neutralize IL-1α from rat testis. It does not affect thymocyte proliferation in the absence of IL-1 (O. Söder, unpublished observations). The thymocytes were cultured and harvested as described above. Positive controls received no IL-1α antiserum or IL-1ra.
RNA extraction and reverse transcription and PCR. Poly(A) RNA was isolated from the tissues using the Micro-Fast Track kit (Invitrogen, San Diego, CA) as suggested by the manufacturer. The isolated poly(A) RNA was precipitated with ethanol and stored at -20 °C. For synthesis of cDNA, the superscript cDNA kit (Life Technologies, Inc., Gaithersburg, MD) was used. Typically, 1 μg of poly(A) RNA was subjected to cDNA synthesis according to the manufacturer's instructions.
For each cytokine, specific primers were synthesized (Innovagen, Lund, Sweden) (Table 1). The primers were deliberately chosen so that they would encompass several exons to avoid confusion with any amplified genomic DNA. PCR was performed on a Perkin-Elmer DNA thermal cycler 480 in a reaction volume of 50 μL in the presence of 1.5-2 mM MgCl2 and 1.5 U of Ampli-Taq DNA polymerase (Perkin-Elmer, Norwalk, CT). Typically, the steps in the PCR cycle were 96 °C for 1 min; 53 °C for 30 s, and 72 °C for 3 min, for a total of 35 cycles. Aliqouts were separated on 2% agarose gels containing ethidium bromide and photographed under UV light. The semiquantitative reverse transcription-PCR data are given in arbitrary units: 0, (+), +, and ++ based on densitometric data in relation to an internal RNA standrard. The number of animals used was 4-16/group for IL-1α, IL-1β, and IL-6.
Statistics
Cytokine bioactivity and brain injury are expressed as mean ± SD. Zero or negative values in the bioassay were set to 0 ± the respective SD. Differences of cytokine bioactivity between control and different time periods of HI were statistically evaluated using analysis of variance with Fisher's correction. The difference between the hypoxic and HI hemisphere was evaluated with the Mann-Whitney U test. The effect of IL-1ra on brain injury was evaluated using Mann-Whitney U test orχ2 analysis with Fisher's correction. The levels of significance are as given in the figure legends.
RESULTS
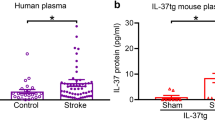
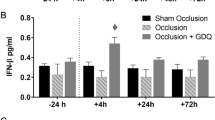
IL-1. The IL-1 bioactivity in extracts from the HI brain was inhibited in vitro almost completely (82%) by IL-1ra and to a lesser degree (66%) by IL-1 antibodies with some specificity for IL-1α(Fig. 1). There was a slight expression of IL-1α mRNA but no detectable IL-1β mRNA or IL-1 bioactivity in control brains(Figs. 2 and3 andTable 2). IL-1 bioactivity remained undetectable 1 h after the insult but was increased at 3 h, peaking at 6 h, and the levels were still significantly higher than control up to 48 h in the HI hemisphere (Fig. 2). The changes of IL-1 bioactivity were less pronounced in the hypoxic hemisphere, being significantly higher than control 3, 10, 20, and 48 h after the insult. The changes in IL-1 bioactivity were accompanied by expression of IL-1β mRNA detectable in the HI hemisphere 1 h after the insult, reaching a maximum at 3 h, and were nondetectable at later time points (Table 2 and Fig. 3). IL-1β mRNA was expressed in the contralateral hypoxic hemisphere only at 3 h (Table 2). The time course of IL-1α mRNA expression was different from IL-1 bioactivity and IL-1β mRNA: a gradual rise was observed up to 3 h, and values were still higher than control 14 d after the insult with the same magnitude of expression in both hemispheres.
Inhibition of IL-1 bioactivity (expressed in arbitrary units as mean ± SD) in HI brain extracts in vitro by IL-1 antiserum (positive control; 2 μL/mL, 1:500; or 8 μL/mL, 1:125) and IL-1ra (positive control; 0.66 ng/mL or 5.3 ng/mL). Statistical comparisonvs IL-1 control bioactivity: *p ≤ 0.05;**p ≤ 0.01; ***p ≤ 0.001.
IL-1 bioactivity (expressed in arbitrary units as mean± SD) in control (C) animals (n = 6) and 1 h(n = 4), 3 h (n = 6), 10 h (n = 6), 20 h(n = 6), 48 h (n = 6), and 14 d (n = 6) after the insult in the hemisphere subjected to HI and hypoxia. Statistical comparisons between control and HI hemisphere: *p ≤ 0.05,**p ≤ 0.01, ***p ≤ 0.001; between control and the hypoxic hemisphere: ¶¶p ≤ 0.01,¶¶¶p ≤ 0.001; and between the hemispheres:§p ≤ 0.05 and §§p ≤ 0.01.
Expression of IL-1β mRNA at 1 h (A), 3 h(B), 20 h (C), and 14 d (D) after the insult in the HI (left, L) and hypoxic (right, R) hemisphere.M, molecular size standard, Life Technologies, Inc. 123-bp ladder, fragments 123 bp, 246 bp, 369 bp, and so forth. C, positive control, RNA isolated from stimulated rat macrophages. 1-4, brain extracts from individual animals. N, control rats not subjected to HI. The visible fragment in C and in positive samples corresponds to the expected size, 524 bp. Gels containing ethidium bromide were photographed under UV light.
IL-6. A slight expression of IL-6 mRNA and IL-6 bioactivity was detectable in control brains (Fig. 4 andTable 2). In response to HI, IL-6 mRNA had already reached maximum expression at 1 h and subsided thereafter toward control values. The expression of IL-6 mRNA in the hypoxic hemisphere after the insult was not significantly affected(Table 2). The IL-6 bioactivity in the HI hemisphere followed a similar time course as IL-6 mRNA with a high bioactivity reached 6 h after the end of hypoxic exposure (Fig. 4).
IL-6 bioactivity (expressed in arbitrary units as mean± SD) in control (C) animals and 6, 10, 20, and 48 h(n = 6 in each group) after the insult in hemisphere subjected to HI and hypoxia. Statistical comparisons between control and HI hemisphere:**p ≤ 0.01 and between the HI and hypoxic hemispheres:§p ≤ 0.05.
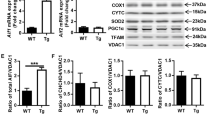
Effect of IL-1ra on HI brain injury. To control for antitrophic influences of IL-1ra, the wet and dry weights of the contralateral noninjured hemispheres were analyzed 14 d after HI. The wet weight in the IL-1ra-treated group amounted to 520 ± 29 mg (n = 23) compared with 516± 33 mg (n = 24) in the vehicle-treated control group (NS) and the dry weights were 90 ± 5 mg (n = 23) and 89 ± 6 mg (n = 24) (NS), respectively, in the IL-1ra and control groups. Intracerebral administration of IL-1ra before the insult reduced brain injury from 54.4 ± 9.3 to 41.4 ± 10.0% (p < 0.01;Fig. 5). Three pups died in the control group and none in the IL-1ra group. Treatment after HI was tested after slight modification of the model with reduction of the duration of HI from 100 to 70 min. Administration of IL-1ra immediately after the insult did not affect the mean brain injury (IL-1ra: 15.1 ± 21.5%; n = 23 compared with controls: 18.0 ± 16.0; n = 24). However, there was a slightly(p ≤ 0.05) higher number of animals (40%) devoid of injury(defined as <+3% weight deficit as a percentage of the contralateral hemisphere) compared with vehicle-treated controls (13%). Two animals died in the control group after the insult whereas four deaths occurred in the posttreatment IL-1ra group (NS).
Effect of pretreatment with IL-1ra (intracerebral administration, 3.3 μg/rat) on HI brain injury (expressed as weight deficit as a percentage of contralateral hemisphere). Diamonds indicate brain injury in each animal in the control group (C; n = 8) and the group treated with IL-1ra (IL-1ra; n = 12). Horizontal bars give the means of each group. Statistical comparison IL-1ra vs control:**p ≤ 0.01.
DISCUSSION
The principal finding in this study was that IL-1 bioactivity is markedly increased in the CNS after HI in neonatal rats. The IL-1 bioactivity in brain extracts from rats subjected to HI was blocked by IL-1ra and IL-1 antibodies supporting the fact that the bioactivity really was exerted by IL-1 and does not represent activity of cross-reacting cytokines. The murine anti-IL-1α antibody in these concentrations cannot be used to distinguish between IL-1α and β as it cross-reacts, but the close correspondence in response to HI between IL-1 bioactivity and IL-1β mRNA(cf. Fig. 2 andTable 2) supports the assumption that the distinct rise of IL-1 bioactivity is at least partly the result of expression of IL-1β mRNA. However, a contribution of IL-1α cannot be excluded even though the IL-1α mRNA expression was less distinct and its time course more protracted (Table 2). IL-1 bioactivity or immunoreactivity has not been detected before in adult or perinatal models of cerebral HI, and these results support the fact that the expression of IL-1β mRNA found after ischemia in different models(6, 7, 15, 30, 31) really is accompanied by an increase in biologic activity of this proinflammatory cytokine. This is an important finding considering that IL-1 regulation is complex(17) and mRNA expression does not always result in release of biologically active molecules, especially not after HI(19). The semiquantitatively assessed changes in IL-1β mRNA found presently with the highest expression at 3 h after HI agree with the quantitative PCR data recently published(15) in the same model with a maximum expression at 4 h.
The pathophysiologic significance of IL-1 (probably IL-1β) is supported by the neuroprotection offered by IL-1ra in vivo(Fig. 5) and by previous studies where IL-1ra was administered in adult(4, 10, 32) and neonatal models(16) of HI or the attenuation of infarction size by adenoviral induction of IL-1ra overexpression(11). However, the degree of neuroprotection found presently with prior treatment with IL-1ra is much less than the reduction by 75% previously reported with repeated s.c. injections of IL-1ra (100 mg/kg) starting even 1 h after HI. Route of administration, dosage, extent of brain injury in control animals, and method of evaluation of brain damage differed between the studies which partly may explain the discrepant findings. The present and previous studies agree that hypothermia is not responsible for the neuroprotection offered by IL-1ra(10, 16). IL-1ra could be anticipated to affect blood glucose(17) which could be an important confounding factor(33), but blood glucose was not affected by IL-1ra. Considering the trophic influences of IL-1, the effect of IL-1ra on the dry weight and wet weight of the contralateral (noninjured) hemisphere was evaluated 14 d after the insult, but was found not to differ from vehicle-treated controls. It is likely that IL-1ra exerts its salutary action by antagonizing the effects of IL-1β. Speculatively, IL-1β is produced by microglia/macrophages and activates other proinflammatory cytokines (IL-8, TNF-α), up-regulates adhesion molecules(34), and recruits neutrophils, lymphocytes, and monocytes(1–3, 17, 35–37) from the blood stream, which in turn may release neurotoxic compounds, e.g. excitatory amino acids, nitric oxide, oxygen free radicals, and neurotoxic cytokines(38–42) which may cause secondary brain injury.
The bioactivity and mRNA of IL-6 also increased in response to HI with a similar time course to IL-1 but the changes were not as pronounced. IL-1 has been shown to trigger IL-6 production in different pathologic situations(17, 43), and the parallelism between IL-1 and IL-6 bioactivity in response to HI (Fig. 2 andFig 4) support a connection. This is the first study demonstrating IL-6 bioactivity or IL-6 mRNA expression in the brain in response to HI, although IL-6 has been found to increase in the brain after closed trauma(44) and in the blood after stroke(8, 9). IL-6 is a multifunctional cytokine(45) that possesses anti-inflammatory properties. Recent data suggest that IL-6 may have a protective role in brain injury as it promotes neuronal survival(45), suppresses demyelination(23), and reduces NMDA-receptor-mediated toxicity and ischemic damage in vivo in adult animals(24). This warrants further studies on the possible role of IL-6 and other inhibitory cytokines in the pathophysiology of perinatal brain injury(14, 46).
Abbreviations
- HI:
-
hypoxia-ischemia
- IL-1ra:
-
IL-1 receptor antagonist
- TNF-α:
-
tumor necrosis factor-α
- PCR:
-
polymerase chain reaction
References
Clark WM, Madden KP, Rothlein R, Zivin JA 1991 Reduction of central nervous system ischemic injury in rabbits using leukocyte adhesion antibody treatment. Stroke 22: 877–883
Jiang N, Zhang R-L, Chen H, Chopp M 1994 Anti-CD11b monoclonal antibody reduces ischemic cell damage after transient (2 h) but not after permanent MCA occlusion in the rat brain. Neurosci Res Commun 15: 85–93
Giulian D, Robertson C 1990 Inhibition of mononuclear phagocytes reduces ischemic injury in the spinal cord. Ann Neurol 27: 33–42
Rothwell NJ, Relton JK 1993 Involvement of interleukin-1 and lipocortin-1 in ischaemic brain damage. Cerebrovasc Brain Metab Rev 5: 178–198
Yabuuchi K, Minami M, Katsumata S, Satoh M 1994 Localization of type I interleukin-1 receptor mRNA in the rat brain. Mol Brain Res 27: 27–36
Liu T, McDonnell PC, Young PR, White RF, Siren AL, Hallenback JM, Barone FC, Feuerstein GZ 1993 Interleukin-1β mRNA expression in ischemic rat cortex. Stroke 24: 1746–1750
Buttini M, Sauter A, Boddeke HWGM 1994 Induction of interleukin-1β mRNA after focal cerebral ischaemia in the rat. Mol Brain Res 23: 126–134
Tarkowski E, Rosengren L, Blomstrand C, Wikkelsö C, Jensen C, Ekholm S, Tarkowski A 1995 Early intrathecal production of interleukin-6 predicts the size of brain lesion in stroke. Stroke 26: 1393–1398
Fassbender K, Rossol S, Kammer T, Daffertshofer M, Wirth S, Dollman M, Hennerici M 1994 Proinflammatory cytokines in serum of patients with acute cerebral ischemia: kinetics of secretion and relation to the extent of brain damage and outcome of disease. J Neurol Sci 122: 135–139
Relton JK, Rothwell NJ 1992 Interleukin-1 receptor antagonist inhibits ischaemic and excitotoxic neuronal damage in the rat. Brain Res Bull 29: 243–246
Betz AL, Yang G-Y, Davidson BL 1995 Attenuation of stroke size in rats using an adenoviral vector to induce overexpression of interleukin-1 receptor antagonist in brain. J Cereb Blood Flow Metab 15: 547–551
Pillay V, Savage N, Laburn H 1993 Interleukin-1 receptor antagoinst in newborn babies and pregnant women. Pflugers Arch 424: 549–551
Pirenne-Ansart H, Paillard F, De Groote D, Elijaafari A, Le Gac S, Blot P, Franchimont P, Vaquero C, Sterkers G 1994 Defective cytokine expression but adult-type T-cell receptor, CD8, and p56lck modulation in CD3- or CD2-activated T cells from neonates. Pediatr Res 37: 64–69
Leviton A 1993 Preterm birth and cerebral palsy: is tumor necrosis factor the missing link?. Dev Med Child Neurol 35: 549–558
Szaflarski J, Burtrum D, Silverstein FS 1995 Cerebral hypoxia-ischemia stimulates cytokine gene expression in the perinatal rats. Stroke 26: 1–8
Martin D, Chinookoswong N, Miller G 1994 The interleukin-1 receptor antagonist (rhIL-1ra) protects against cerebral infarction in a rat model of hypoxia-ischemia. Exp Neurol 130: 362–367
Dinarello CA 1994 Interleukin-1. In: Thomson AW (ed) The Cytokine Handbook. Academic Press, Boston, pp 31–57
Dwyer BE, Nishimura RN, Powell CL, Mailheau SL 1987 Focal protein synthesis inhibition in a model of neonatal hypoxic-ischemic brain injury. Exp Neurol 95: 277–289
Li Y, Chopp M, Zhang ZG, Zaloga C, Niewenhuis L, Gautam S 1994 p53-Immunoreactive protein and p53 mRNA expression after transient middle cerebral artery occlusion in rats. Stroke 25: 849–856
Hopkins SJ, Rothwell NJ 1995 Cytokines and the nervous system. I. Expression and recognition. Trends Neurosci 18: 83–88
Aderka DJML, Vilcek J 1989 IL-6 inhibits lipopolysaccharide-induced tumour necrosis factor production in cultured human monocytes, U937 cells, and mice. J Immunol 143: 3517–3523
Tilg H, Trehu E, Atkins MB, Dinarello CA, Mier JW 1994 Interleukin-6 (IL-6) as an anti-inflammatory cytokine: induction of circulating IL-1 receptor antagonist and soluble tumour necrosis factor receptor p55. Blood 83: 113–118
Rodriguez M, Pavelko KD, McKinney CW, Leibowitz JL 1994 Recombinant human IL-6 suppresses demyelination in a viral model of multiple sclerosis. J Immunol 153: 3811–3821
Rothwell NJ, Hopkins SJ 1995 Cytokines and the nervous system II: actions and mechanisms of action. Trends Neurosci 18: 130–136
Rice JE, Vannucci RC, Brierley JB 1981 The influence of immaturity on hypoxicischemic brain damage in the rat. Ann Neurol 9: 131–141
Andine P, Thordstein M, Kjellmer I, Nordborg C, Thiringer K, Wennberg E, Hagberg H 1990 Evaluation of brain damage in a rat model of neonatal hypoxic-ischemia. J Neurosci Methods 35: 253–260
Granholm T, Froysa B, Lundstrom C, Wahab A, Midtvedt T, Soder O 1992 Cytokine responsiveness in germfree and conventional NMRI mice. Cytokine 4: 545–550
Gustafsson K, Soder O, Pollanen P, Ritzen EM 1988 Isolation and partial characterization of interleukin-1-like factor from rat testis interstitial fluid. J Reprod Immunol 14: 139–150
VanSnick J, Cayphas S, Vink A, Uyttenhove C, Coulie PG, Rubira MR, Simpson RJ 1986 Purification and NH2-terminal amino acid sequence of a T-cell-derived lymphokine with growth factor activity for B-cell hybridomas. Proc Natl Acad Sci USA 83: 9679–9683
Minami M, Kurashi Y, Yabuuchi K, Yamazaki A, Satoh M 1992 Induction of interleukin-1β mRNA in rat brain after transient forebrain ischemia. J Neurochem 58: 390–392
Yabuuchi K, Minami M, Katsumata S, Yamazaki A, Satoh M 1994 An in situ hybridization study on interleukin-1β mRNA induced by transient forebrain ischemia in the rat. Mol Brain Res 26: 135–142
Yamasaki Y, Matsuura N, Shozuhara H, Onodera H, Itoyama Y, Kogure K 1995 Interleukin-1 as a pathogenetic mediator of ischemic brain damage in rats. Stroke 26: 676–681
Vannucci RC 1993 Experimental models of perinatal hypoxic-ischemic brain damage. APMIS Suppl 101: 89–95
Arnould T, Michiels C, Remacle J 1993 Increased PMN adherence on endothelial cells after hypoxia: involvement of PAF, CD18/CD11b, and ICAM-1. Am J Physiol 264:C1102–C1110
Kim JS, Chopp M, Chen H, Levine SR, Carey JL, Welch KMA 1995 Adhesive glycoproteins CD11a and CD 18 are upregulated in the leukocytes from patients with ischemic attacks. J Neurol Sci 128: 45–50
McRae A, Gilland E, Bona E, Hagberg H 1994 Microglia activation after neonatal hypoxic-ischemia. Dev Brain Res 84: 245–252
Gehrmann J, Matsumoto Y, Kreutzberg GW 1995 Microglia: intrinsic immunoeffector cell of the brain. Brain Res Rev 20: 269–287
Gelbard HA, Dzenko KA, DiLoeto D, del Cerro C, del Cerro M, Epstein LG 1993 Neurotoxic effects of tumor necrosis factor alpha in primary human neuronal cultures are mediated by activation of the glutamate AMPA receptor subtype: implications for AIDS neuropathogenesis. Dev Neurosci 15: 417–422
Chao CC, Hu S 1994 Tumor necrosis factor-alpha potentiates glutamate neurotoxicity in human fetal brain cell cultures. Dev Neurosci 16: 172–179
Giulian D, Li J, Li X, George J, Rutecki PA 1994 The impact of microglia-derived cytokines upon gliosis in the CNS. Dev Neurosci 16: 128–136
Kuroda Y, Shimamoto Y 1991 Human tumor necrosis factor-α augments experimental allergic encephalomyelitis in rats. J Neuroimmunol 34: 159–164
Selmaj KW, Raine CS 1988 Tumor necrosis factor mediates myelin and oligodendrocyte damage in vitro. Ann Neurol 23: 339–346
Schotanus K, Tilders FJH, Berkenbosch F 1993 Human recombinant interleukin-1 receptor antagonist prevents adrenocorticotropin, but not interleukin-6 responses to bacterial endotoxin. Endocrinology 133: 2461–2468
Shohami E, Novikov M, Bass R, Yamin A, Gallily R 1994 Closed head injury triggers early production of TNFα and IL-6 by brain tissue. J Cereb Blood Flow Metab 14: 615–619
Kishimoto T, Akira A, Taga T 1992 Interleukin-6 and its receptor: a paradigm for cytokines. Science 258: 593–597
Adinolfi M 1993 Infectious diseases in pregnancy cytokines and neurological impairment: an hypotesis. Dev Med Child Neurol 35: 549–558
Nishida T, Nishono N, Takano M, Sekiguchi Y, Kawai K, Mizuno K, Nakai S, Masui Y, Harai Y 1989 Molecular cloning and expression of rat interleukin-1α cDNA. J Biochem 105: 351–357
Northermann W, Braciak TA, Hattori M, Lee F, Fey GH 1989 Structure of the rat interleukin 6 gene and its expression in macrophage-derived cells. J Biol Chem 264: 16072–16082
Acknowledgements
The authors thank Berit Fröysa and Gunnie Westerholm for expert technical assistance.
Author information
Authors and Affiliations
Additional information
Supported by Swedish Medical Research Council (09455, 8282, 11412, 10353), Swedish Society for Medical Research, The Göteborg Medical Society, the Swedish Society of Medicine, the Sven Jerring Foundation, the 1987 foundation for Stroke Research, the Åke Wiberg Foundation, the Åhlén Foundation, the Magnus Bergvall Foundation, the Frimurare Barnhus Foundation, and the medical faculty of Göteborg.
Rights and permissions
About this article
Cite this article
Hagberg, H., Gilland, E., Bona, E. et al. Enhanced Expression of Interleukin (IL)-1 and IL-6 Messenger RNA and Bioactive Protein after Hypoxia-Ischemia in Neonatal Rats. Pediatr Res 40, 603–609 (1996). https://doi.org/10.1203/00006450-199610000-00015
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199610000-00015
This article is cited by
-
Early evolution of glial morphology and inflammatory cytokines following hypoxic-ischemic injury in the newborn piglet brain
Scientific Reports (2023)
-
IL-18BP Alleviates Anxiety-Like Behavior Induced by Traumatic Stress via Inhibition of the IL-18R-NLRP3 Signaling Pathway in a Mouse Model of Hemorrhagic Shock and Resuscitation
Molecular Neurobiology (2023)
-
AD-16 Protects Against Hypoxic-Ischemic Brain Injury by Inhibiting Neuroinflammation
Neuroscience Bulletin (2022)
-
Microglia and Stem-Cell Mediated Neuroprotection after Neonatal Hypoxia-Ischemia
Stem Cell Reviews and Reports (2022)
-
Disruption to the 5-HT7 Receptor Following Hypoxia–Ischemia in the Immature Rodent Brain
Neurochemical Research (2018)