Abstract
Insulin sensitivity was studied before and after 3 mo of continuous cycling peritoneal dialysis (CCPD) in seven uremic patients, before and after 3 mo of hemodialysis (HD) in another seven uremic patients, and in seven healthy controls. There were no significant differences in the height, weight, anthropometric measures, or intakes of protein and total calories between the CCPD and the HD groups before and after the 3 mo of dialysis therapy. There were no differences in other biochemical parameters between patients on CCPD and patients on HD either at the initiation of dialysis or at the end of 3 mo of dialysis therapy. Residual renal function was not different between the two groups. Mean Kt/Vurea in the CCPD group was 2.10/wk and that for the HD group was 1.20/session. The CCPD group and the HD group both had higher fasting glucose concentrations (p < 0.02), but normal fasting serum immunoreactive insulin concentrations compared with controls. The hyperinsulinemic euglycemic clamp technique was used to measure insulin sensitivity. Before dialysis, insulin sensitivity was low in both patient groups (CCPD 128 ± 11 mg/m2/min; HD 130 ± 11) compared with controls (320 ± 26) (p < 0.01 in both cases) but not different between the patient groups. After 3 mo of dialysis therapy, insulin sensitivity increased by 80 ± 7% in the CCPD group and by 38± 4% in the HD group (p < 0.01 compared with predialysis values in both groups). Insulin sensitivity in both groups after 3 mo of dialysis was still lower than in the control group (p < 0.01 in both cases). However, both the percentage increase as well as the final insulin sensitivity were significantly higher in the CCPD group (230 ± 19 mg/m2/min) than the HD groups (179 ± 16) (p < 0.01 in both cases).
Similar content being viewed by others
Main
Insulin resistance, as evidenced by reduced peripheral sensitivity to insulin action, is common in patients with uremia(1, 2). The site of the insulin resistance in uremia is likely to be peripheral. Hepatic glucose production is not increased and is suppressed normally in response to insulin in patients with uremia(3). DeFronzo et al.(3) directly quantitated leg glucose exchange in uremic patients and showed that insulin-mediated glucose uptake was decreased and that this decrease in leg glucose exchange correlated well with the decrease in total body insulin-mediated glucose uptake. Because adipose tissue accounts for the disposal of less than 1-2% of the glucose load, the muscle tissue must represent the primary tissue responsible for the insulin resistance in uremic patients. The etiology of insulin resistance in uremia, however, remains unclear. Previous data on insulin resistance in uremia have been obtained in patients with preterminal chronic renal failure(3, 4) and patients on HD(5, 6). There is little data on insulin metabolism in patients with uremia on peritoneal dialysis. The aim of the present study is to compare the effect of CCPD to that of HD on insulin sensitivity in patients with uremia.
METHODS
Fourteen patients with uremia were studied. They were all initially examined just before starting dialysis therapy for management of their uremia. They were matched for age, and the study was performed over a 2-y period. There were no significant changes in dialysis procedures over this period of time. Seven patients (age 17 ± 1 y) received CCPD, from 8 to 10 cycles nightly. The underlying diagnoses in this group included focal segmental glomerulosclerosis, mesangial capillary glomerulonephritis, reflux nephropathy, prune belly syndrome, and unknown etiology. They were dialyzed on Baxter Pac-X peritoneal dialysis cyclers with a mean cycle volumes of 35± 5 mL/kg. Peritoneal dialysis adequacy was assessed by calculatingKt/Vurea from urea clearance of a 24-h peritoneal fluid collection (dialysate BUN/plasma BUN × 24-h drain, vol/vol of urea distribution). The volume of urea distribution was assumed to be equal to total body water and was estimated from nomograms(18). The other seven patients (age 17 ± 1 y) received regular HD, 3-4 h/session, three sessions a week. The underlying diagnoses in this group included focal segmental glomerulosclerosis, renal dysplasia, reflux nephropathy, obstructive uropathy, and unknown etiology. They were dialyzed with CA 90 dialyzers with mean blood flows of 180 ± 15 mL/min. Hemodialysis adequacy was assessed from Kt/Vurea calculated from urea reduction ratios [Kt/Vurea =-logn (post-dialysis BUN/predialysis BUN)](19). The patients were assigned to their respective modalities of dialysis based on individual preferences. There were no differences in socialeconomic status between the two groups. Residual renal function had been assessed in the two groups of patients by 24-h creatinine clearance and was not different (CCPD 0.9 ± 0.4 mL/min and HD 1.1± 0.5 mL/min). The patients were all then restudied 3 mo after initiation of dialysis. There were no significant changes in clinical parameters such as weight, height, and blood pressure; or nutritional parameters such as caloric and protein intakes, triceps skinfold thickness(TSF) or mid-arm muscular area (AMA) (Table 1). Medications included calcium carbonate, oral 1,25-vitamin D3[(OH)2D3], sodium bicarbonate, antihypertensives in the form of long acting infedipine and water-soluble vitamins (Nephrovite; R & D Laboratories, Marina Del Rey, CA). The mean dosages of vitamin D and nifedipine in the two different groups of patients were not different. There were no significant medication changes during the 3 mo of therapy. None of the patients was on corticosteroids at the time or had been on corticosteroids for 6 mo before the study. The patients did not take any of their medications on the morning of the studies. Their daily intake of carbohydrate was more than 200 g, and their body weights were stable for at least 2 mo before the studies. Their dietary intakes of sodium (2 g/d), potassium (2 g/d), and phosphorus (800 mg) were restricted, but the intake of protein was not. Dietary intakes were assessed monthly using a 3-d dietary recall and adjustments made if necessary. All patients did not have a history of or family history of diabetes mellitus. All patients had Tanner puberty scores of 5 at the beginning of the study. Controls consisted of seven healthy subjects(age 19 ± 1 y) consuming regular weight-maintaining diets and taking no medications. They did not have history of any significant illness or any family history of diabetes mellitus. All patients and controls were free from infections at the time of the studies. One control patient (age 18) was studied on five different occasions, at monthly intervals for calculations of interassay variation of insulin sensitivity.
All studies were started about 0900 h after an overnight fast of about 10-12 h. The patients on CCPD had their dialysis suspended the night before and drained their peritoneum of dialysate from the long day dwell (only 100 mL of dialysate, not a full cycle volume) the day before, so that they did not have dextrose (dialysate) in their peritoneum overnight. The patients on HD were studied just before a mid-week scheduled session. The patients or controls sat comfortably in a reclining chair and were not allowed to eat or drink apart from water during the studies. Insulin sensitivity was measured by the hyperinsulinemic euglycemic clamp technique(7). A sampling line was inserted in a vein on the dorsum of the hand. The hand was then placed in a heated box (65°C) to arterialize the blood(8). An indwelling catheter was placed in a vein in the opposite arm for infusion of glucose and insulin. After obtaining at least three fasting serum samples for glucose and insulin concentration, a prime-continuous infusion of insulin at 40 mU/m2/min was given i.v. to maintain constant hyperinsulinemia. The serum glucose concentration was measured at 5-min intervals, and a variable infusion of 20% dextrose was adjusted to maintain the glucose concentration at fasting levels. Under these steady-state conditions of euglycemia, all of the infused glucose(mg/m2/min) was taken up and yielded a measure of the body's sensitivity to the exogenously infused insulin. In patients in whom there was residual urine production, a urine sample was obtained at the end of the study to quantitate urinary losses of glucose.
Constant euglycemia and hyperinsulinemia was achieved in all euglycemic clamp studies. There was no difference in the steady state insulin concentrations during the euglycemic clamp studies in the three groups. The interassay coefficient of variation for insulin sensitivity during the euglycemic clamp studies was 8.2% from five repeated studies performed monthly in one normal subject. Serum glucose concentration was measured by the glucose oxidase method using a Yellow Springs 23 AM glucose analyzer (Yellow Springs Instruments, Yellow Springs, OH). Serum immunoreactive insulin concentration was measured by double antibody RIA (Pharmacia, Uppsala, Sweden). The intraassay and interassay coefficients of variation for serum insulin were 5.2 and 8.2%, respectively. Intact serum PTH was measured by an immunoradiometric assay (Nichols, San Juan Capistrano, CA). The intraassay and interassay coefficients of variation for serum PTH were 7.2 and 9.3%, respectively. Serum 1,25-(OH)2D3 was measured by a radioreceptor assay (Nichols). This assay is specific for both 1,25-(OH)2D3 and 1,25-(OH)2D2. It involves a preliminary extraction and purification of serum using a single column containing a C18OH-activated matrix. Once purified, the material was quantitated in a radioreceptor assay using a calf thymus receptor and tritiated 1,25-(OH)2D3. Separation of bound from free 1,25-(OH)2D3 was achieved by incubation with dextran-coated charcoal. The intraassay and interassay coefficients of variation for serum 1,25-(OH)2D3 were 8.2 and 9.9%, respectively. Serum total calcium, phosphorus, potassium, magnesium, creatinine, and blood urea nitrogen were measured by standard methods on a multichannel autoanalyzer.
The study was approved by the Panel of Human Subjects in Medical Research at Stanford University and the Committee for Clinical Investigations at Children's Hospital of Los Angeles. The purpose and potential risks of the study was carefully explained to all patients and subjects, and written informed consent was obtained before their participation. All values are expressed as mean ± SEM. The data were tested for normality using theχ2 method. The t tests for paired and unpaired observations were used for analysis of the results. Statistical significance was recognized at the 5% level.
RESULTS
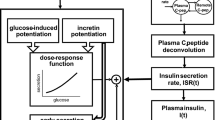
The nutritional data and serum biochemistry of the patients and controls are presented in Table 1. Both groups of patients had low serum 1,25-(OH)2D3 (p < 0.01) and high serum PTH(p < 0.01) compared with the corresponding values in controls: 35± 3 pg/mL [1,25-(OH)2D3] and 18 ± 3 pg/mL (PTH). There were significant but equal decreases in serum creatinine (p< 0.01) and BUN (p < 0.01) in both groups after dialysis, but there were no other significant differences in the biochemical parameters between patient on CCPD and patients on HD, either at the initiation of dialysis or at the end of 3 mo of dialysis therapy.Kt/Vurea for CCPD was 0.3 ± 0.03/d (or 2.10/wk), whereas Kt/Vurea for HD was 1.20 ± 0.15/session. There were no significant differences in the dietary intakes of protein, total calories, or carbohydrate between the CCPD and the HD groups during the 3 mo of dialysis therapy. The caloric intakes in the CCPD group included the contribution from the dialysate glucose absorption. The anthropometric measurements and serum albumin concentrations were also not different between the two groups, suggesting no difference in nutritional status. Fasting glucose concentrations in both CCPD and HD groups both before and after dialysis were higher than those in controls (90 ± 3 mg/dL)(p < 0.02). Fasting insulin concentrations were not different in both groups of patients (before and after dialysis) compared with controls (11± 1 μU/mL). Insulin sensitivity in both groups before and after 3 mo of dialysis therapy is presented in Figure 1. Before dialysis, insulin sensitivity was low in both patient groups (CCPD 128± 11 mg/m2/min; HD 130 ± 11) compared with controls (320± 26) (p < 0.01 in both cases), but not different between the patient groups. After 3 mo of dialysis therapy, insulin sensitivity increased by 80 ± 7% in the CCPD group and by 38 ± 4% in the HD group. Insulin sensitivity in both groups after 3 mo of dialysis was still significantly lower than that in the control group (p < 0.01 in both cases). However, both the percentage increase as well as the final insulin sensitivity were significantly higher in the CCPD group (230 ± 19 mg/m2/min) than in the HD group (179 ± 16) (p < 0.01 in both cases).
DISCUSSION
The euglycemic clamp technique is a sensitive and reproducible method of quantifying in vivo insulin sensitivity under conditions of euglycemia and hyperinsulinemia(7). During constant euglycemia, the amount of glucose infused is assumed to equal the amount being transported out of the glucose space, that is, the amount metabolized. A small correction has to be made in patients in whom there is urine output. This also carries the assumption that hepatic glucose production is suppressed by hyperinsulinemia. In normal subjects and patients with uremia, hepatic glucose production has been measured by tritiated glucose turnover technique as well as direct hepatic venous catheterization under these conditions of euglycemia and hyperinsulinemia and shown to be similarly suppressed(3). DeFronzo et al.(5) studied insulin metabolism in adult uremic patients using the euglycemic clamp technique. Before initiation of hemodialysis, insulin sensitivity was markedly reduced in uremic subjects compared with controls. After hemodialysis for 10 wk, insulin sensitivity improved significantly, although it was still lower than control values(5). This is little information on insulin sensitivity in patients on CCPD.
The present study shows that both modalities of dialysis therapy improved insulin resistance in uremic patients. Insulin sensitivity was very similar in the two groups of uremic patients before dialysis. After 3 mo of therapy, insulin sensitivity in CCPD patients was significantly higher than that in HD patients. A simple explanation would be that patients on HD were dialyzed only three times a week and were usually more uremic just before the next session, whereas patients on CCPD were dialyzed every night and therefore were less uremic in the morning. However, precautions were taken in the present study so that the patients on CCPD did not get dialysis the night before. Indeed, the serum creatinine and the BUN were not different in the patients on HD compared with those on CCPD. This precaution was also taken so that the patients on CCPD did not absorb glucose from their dialysate overnight and were therefore truly fasted. The fasting blood glucose concentrations in the patient on CCPD were the same as those in patients on HD.
It is possible that the patients on CCPD were overall better dialyzed than the HD group. It is difficult to compare the dose of dialysis in these two patient cohorts. The mean weekly Kt/Vurea for CCPD patients (2.10) was approximately 58% compared with that (3.60) for hemodialysis patients. These urea clearances for both dialysis modalities were within the recommended ranges for clinical well being(20). Also, their residual renal function were not different. Peritoneal dialyses yield poor small molecular clearances but better middle molecule clearances compared with HD(21). McCaleb et al.(9) partially purified and characterized a factor from uremic sera which inhibited insulin-mediated glucose disposal in normal rat adipocytes. This factor was a middle molecule(molecular weight between 1,000 and 2,000 daltons) and was specific for uremia(not present in sera from patients with other insulin-resistant states, such as obesity and diabetes mellitus). Improved clearance of uremic toxins in the form of middle molecules by peritoneal dialysis may explain the differences in insulin sensitivity between the two patient populations in the present study.
Malnutrition is common in patients with end-stage renal disease(10) and may be an important cause of insulin resistance(11). Treatment of malnutrition by i.v. nutrition has been shown to improve insulin resistance in surgical patients(12). Improved nutrition in these patients after dialysis may be an important factor in the improvement of insulin resistance. However, in the present study, dietary and anthropometric assessments did not show any significant changes in the patients after 3 mo of dialysis. There is evidence that the uremic toxins causing insulin resistance may be products of protein catabolism. Mak et al.(13) studied the effect of protein restriction on insulin sensitivity in a group of uremic adolescents. Before treatment the patients had high blood urea concentrations and were insulin-resistant as measured by the clamp technique. Six months after initiation of dietary protein restriction with amino acid and keto acid supplementation, significant reduction in blood urea concentrations were accompanied by normalization of insulin resistance. This finding was subsequently confirmed by another group of investigators in adult uremic patients(14). Although the protein catabolic rates have not been formally assessed, there is no difference in the protein intake, serum albumin, or BUN concentrations between the CCPD and HD groups. Furthermore, the heights, weights, and anthropometric measurements were not different between the two groups of patients. These data suggest that nutritional status probably does not explain the differences in insulin sensitivity.
Both groups of patients had low serum 1,25-(OH)2D3(p < 0.01) and high serum PTH compared with control values. Mak(15) showed that patients on HD with 1,25-(OH)2D3 deficiency and secondary hyperparathyroidism were glucose-intolerant, normoinsulinemic, and insulin-resistant. Intravenous 1,25-(OH)2D3 corrected glucose intolerance by increasing insulin secretion. These events occurred without any changes in serum PTH concentrations(15). Also i.v. 1,25-(OH)2D3 corrected insulin resistance in patients on HD with 1,25-(OH)2D3 deficiency and secondary hyperparathyroidism without any change in serum PTH concentrations(16). Thus, either 1,25-(OH)2D3 deficiency is an important factor in the pathogenesis of insulin abnormalities in uremia, or pharmacologic doses of the vitamin D metabolite can reverse insulin abnormalities in uremia. However, serum PTH and 1,25-(OH)2D3 concentrations were not different between the groups on HD and CCPD before or after 3 mo of dialysis. Metabolic acidosis is a frequent complication in uremia and may contribute to insulin resistance. DeFronzo and Beckles(17) studied ammonium chloride induced metabolic acidosis in humans and found impaired tissue sensitivity to both endogenous and exogenous insulin. However, metabolic acidosis cannot be a major factor in the present study, because the patients had normal serum HCO3 concentrations before and after 3 mo of dialysis. Therefore, these metabolic factors are unlikely to account for the differences in insulin sensitivity in the present study.
In summary, both CCPD and HD improved insulin sensitivity in uremic patients. However, both the percentage increase as well as the final insulin sensitivity were significantly higher in the CCPD group. Improved clearance of uremic toxins by peritoneal dialysis may explain the differences in insulin sensitivity between the two patient populations.
Abbreviations
- CCPD:
-
continuous cycling peritoneal dialysis
- HD:
-
hemodialysis
- 1,25-(OH)2D3:
-
1,25-dihydroxyvitamin D3
- BUN:
-
blood urea nitrogen
- HCO3:
-
bicarbonate
- K t /V urea :
-
fractional urea clearance
References
Mak RHK, DeFronzo RA 1992 Glucose and insulin metabolism in uremia. Nephron 61: 377–382
Mak RHK 1994 Renal disease, insulin resistance and glucose tolerance. Diabetes Rev 2: 19–28
DeFronzo RA, Alvestrand A, Smith D, Hendler R, Hendler E, Wahren J 1981 Insulin resistance in uremia. J Clin Invest 67: 563–570
Mak RHK, Haycock GB, Chantler C 1983 Glucose intolerance in children with chronic renal failure. Kidney Int 24( suppl 15): S22–S26
DeFronzo RA, Tobin JD, Rowe JW, Andres R 1978 Glucose intolerance in uremia: quantification of pancreatic beta cell to glucose and tissue sensitivity to insulin. J Clin Invest 62: 425–435
Mak RHK, Bettinelli A, Turner C, Haycock GB, Chantler C 1985 The influence of hyperparathyroidism on glucose metabolism in uremia. J Clin Endocrinol Metab 60: 229–233
DeFronzo RA, Tobin J, Andres R 1979 Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol 237:E214–E223
McGuire EAH, Helderman JH, Tobin JD, Andres R, Berman M 1976 Effects of arterial versus venous sampling on analysis of glucose kinetics in man. J Appl Physiol 41: 565–573
McCaleb ML, Izzo MS, Lockwood DH 1985 Characterization and partial purification of a factor from uremic human sera that induces insulin resistance. J Clin Invest 75: 391–398
Kopple JD 1978 Abnormal amino acid and protein metabolism in uremia. Kidney Int 14: 340–348
Feldman HA, Singer I 1975 Endocrinology and metabolism in uremia and dialysis: a clinical review. Medicine 54: 345–376
Church JM, Hill GL 1988 Impaired glucose metabolism in surgical patients improved by intravenous nutrition: assessment by euglycemic-hyperinsulinemic clamp. Metabolism 37: 505–509
Mak RHK, Turner C, Thompson T, Haycock GB, Chantler C 1986 The effect of dietary protein restriction and amino acid/keto acid supplements on glucose metabolism in uremic children. J Clin Endocrinol Metab 63: 985–989
Apracio M, Gin H, Potaux L, Bouchat JL, Morel D, Aubertin J 1989 Effect of a ketoacid diet on glucose tolerance and tissue insulin sensitivity. Kidney Int 36( suppl 27): S231–S225
Mak RHK 1992 1,25 dihydroxycholecalciferol corrects glucose intolerance in hemodialysis patients. Kidney Int 41: 1049–1054
Mak RHK 1992 Amelioration of hypertension and insulin resistance by 1,25 dihydroxycholecalciferol reverses insulin resistance and hypertension in hemodialysis patients. Pediatr Nephrol 6: 377–382
DeFronzo RA, Beckles AD 1979 Glucose intolerance following chronic metabolic acidosis in man. Am J Physiol 236:E328–E334
Friis-Hansen B 1961 Body water compartments in children: changes during growth and related changes in body composition. Pediatrics 28: 169–181
Gotch FA, Sargent JA 1985 A mechanistic analysis of the National Cooperative Dialysis Study (NCDS). Kidney Int 28: 526–534
Gotch FA 1993 Adequacy of peritoneal dialysis. Am J Kid Dis 21: 96–98
Boen S, Haagsma-Schouter W, Birnie R 1978 Long-term peritoneal dialysis and a peritoneal dialysis index. Dial Transplant 7: 377–378
Acknowledgements
The author thanks Stella Chang, M.S., and Joanne Wong, M.D., for assistance in the performance of some of the studies. He also thanks the the nurses in the dialysis units for their generous support and patience during the studies.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Mak, R. Insulin Resistance in Uremia: Effect of Dialysis Modality. Pediatr Res 40, 304–308 (1996). https://doi.org/10.1203/00006450-199608000-00019
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199608000-00019
This article is cited by
-
Insulin and its role in chronic kidney disease
Pediatric Nephrology (2008)
-
The prevalence of insulin resistance in nondiabetic nonobese patients with chronic kidney disease
Advances in Therapy (2006)
-
Comparison of glucose tolerance in renal transplant recipients and hemodialysis patients
BMC Nephrology (2004)