Abstract
We have previously observed a developmental difference in mucosal permeability (i.e. the younger the animal, the greater the increase in permeability) after exposure to luminal nutrients derived from cow's milk-based infant formulas. There has been tremendous speculation and some clinical evidence that mother's milk may be protective against mucosal injury in developing intestine. In this study, we hypothesized that instillation of sow's milk into the intestinal lumen of developing piglets would causeno differences in either intestinal metabolic demand (oxygen uptake) or mucosal permeability among age groups. Intestinal blood flow (total and fractionated), arteriovenous oxygen content difference, venous pressure, and capillary pressure were measured, and vascular resistance and oxygen uptake were calculated, after 30 min of intraluminal instillation of predigested and solubilized sow's milk in 1-d-old, 3-d-old, 2-wk-old, and 1-mo-old piglet jejunoileum. In a separate group of animals, plasma-to-lumen clearance of chromium-51 EDTA was evaluated during luminal perfusion with digested and solubilized sow's milk in 1-d-old, 3-d-old, and 1-mo-old piglet jejunoileum. Intestinal oxygen uptake was similar among age groups of developing piglets, but EDTA clearance was significantly higher for intestinal segments perfused with sow's milk in 1-d-old, compared with older, animals. Thus, luminal perfusion with predigested and bile acid-solubilized sow's milk in 1-d-old piglet jejunoileum, compared with perfusion in older piglets, causes increased mucosal permeability in 1-d-old intestine, but this increased permeability is not due to increased intestinal oxygen uptake (i.e. increased metabolic demand).
Similar content being viewed by others
Main
It was initially believed that infants fed breast milk never developed necrotizing enterocolitis, but cases have been reported in infants fed only breast milk(1–11) as well as those who have never been fed(9, 13–17). The incidence, however, of necrotizing enterocolitis in breast-fed babies does appear to be less overall than that for formula-fed infants(4, 9, 15–20). Many possible reasons for this differential effect have been postulated, but the protective factor(s) in mother's milk against mucosal injury in developing intestine has yet to be identified.
Based on previous work in our laboratory investigating changes in postprandial hemodynamics, oxygenation, and mucosal permeability in developing intestine(21–24), we questioned whether mother's milk may be protective against mucosal injury due to a smaller increase in postprandial metabolic demand compared with that elicited by infant formulas. Therefore, the objectives of this study were 1) to evaluate the hemodynamic and oxygenation responses to intraluminal mother's milk in developing piglet intestine, and 2) to determine the effect on mucosal permeability of digested and solubilized sow's milk, hopefully providing insight into whether developmental differences in intestinal oxygenation may explain the protective effect of mother's milk against mucosal injury in developing intestine.
METHODS
Preparation of sow's milk. Sow's milk was expressed from the sow during labor and delivery and was predigested for 3 h at 37°C with pancreatic enzymes (Pancrease MT 16; McNeil Pharmaceutical, Spring House, PA, containing lipase, 16,000 U; amylase, 48,000 U; and protease, 48,000 U/capsule, with one capsule used to digest 120 mL of milk). The lipid components were solubilized with 10 mmol/L taurocholic acid (sodium salt, 98%; Sigma Chemical Co., St. Louis, MO). For the 1-mo-old animals, sow's milk that had been collected and frozen was thawed and prepared as above because it was not possible to obtain fresh milk from the sow at the time that the piglets were 1-mo-old. Frozen sow's milk was also used in one-half of the intestinal segments from 1-d-old animals for the mucosal permeability studies. Four (of five total) 1-d-old animals (eight intestinal segments perfused with frozen milk; 12 segments perfused with fresh milk) were studied to assure that there were no differences in mucosal permeability for fresh versus frozen sow's milk.
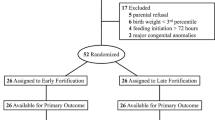
Animals. This study was approved by the Louisiana State University Medical Center Animal Resources Committee. All animals were handled in accordance with the guidelines set forth by the American Physiologic Society. Thirty-nine mixed breed piglets of either sex were divided among groups of 1-d-old, never nursed (n = 14), and 3-d-old (n = 11), 2-wk-old (n = 5), and 1-mo-old (n = 9) animals, each fasted for at least 18 h. After intramuscular injection of ketamine HCl (20 mg/kg) and xylazine (2 mg/kg), the piglets were anesthetized with i.v. sodium pentobarbital (20 mg/kg). Maintenance doses of sodium pentobarbital (5 mg/kg) were given as needed during the experiment.
Surgical procedure. Immediately after anesthetic induction, a tracheostomy was performed to artificially ventilate the animals at a respiratory rate and tidal volume to maintain normal arterial blood gases and pH. Polyethylene cannulas were inserted into the right jugular vein for administration of fluids for hydration and pentobarbital, and into the left carotid artery for monitoring of systemic blood pressure and withdrawal of blood samples. Body temperature was maintained at approximately 37°C during the experiment with a heating pad and an infrared heating lamp. The intestine was covered with plastic wrap to prevent evaporative losses.
For the intestinal blood flow experiments, the left carotid artery cannula was advanced into the left ventricle for injection of radioactive microspheres. Additional polyethylene cannulas were inserted into the left femoral artery for withdrawal of microsphere reference blood samples/monitoring of systemic blood pressure, and into the right femoral artery to provide blood for continuous perfusion of the arterial cuvette of an(a-v)o2 content difference analyzer (AVOX Systems, San Antonio, TX). After a midline laparotomy and removal of the spiral colon and cecum, the superior mesenteric artery was isolated. After exteriorizing a segment of jejunoileum, the most distal portion of the mesenteric vein was isolated. The section of intestine drained by the vein was then isolated and cannulated at both ends for luminal instillation of sow's milk. An i.v. injection of heparin sodium (5,000-10,000 U) was given immediately before temporary occlusion of the superior mesenteric artery and cannulation of the distal segment of the mesenteric vein. The venous outflow drained into a reservoir before being returned to the piglet through the right external jugular vein. Interposed in the venous circuit was a Y-connector to enable measurement of intestinal venous pressure and capillary pressure via the brief-occlusion technique(25). Also in this venous outflow circuit was a calibrated flow probe to monitor intestinal blood flow continuously. The signal from the flow probe was transmitted to a square-wave electromagnetic flowmeter (Carolina Medical Electronics, King, NC). A portion of the venous outflow was also used to provide intestinal venous blood for the(a-v)o2 content difference analyzer. Heparin-treated blood (35 mL) from a donor piglet (2-3 mo old) was used to prime all extracorporeal circuits.
For the mucosal permeability experiments, the abdomen was entered through the midline and both renal arteries were ligated to prevent urinary excretion of 51Cr-EDTA. Segments of jejunoileum, approximately 15 cm in length, were isolated and cannulated at either end for luminal perfusion (4 segments/animal).
Measurement of fractionated blood flow. Fractionated blood flow to the small intestine and total flow to each kidney were determined using two different radiolabeled microsphere suspensions (46Sc and 85Sr). The microspheres (15 ± 3-μm diameter; 3M, St. Paul, MN) were suspended in 10% dextran containing 0.05% Tween 80 to prevent aggregation. Before injection, each microsphere suspension was thoroughly mixed with a sonicator and a vortex shaker. The stock solution of microspheres contained≈2.5 × 109 microspheres/L. A volume of 0.5 mL for 1- and 3-d-olds and 1 mL for 2-wk- and 1-mo-olds was injected into the left ventricle within 15 s. Ten seconds before injection, reference sample withdrawal from the left femoral artery was begun at a rate of 0.045 mL/s and continued to a total of 110 s. A volume of donor piglet blood equal to the reference sample was simultaneously infused through the carotid cannula during the withdrawal period. At the completion of the experiment, the kidneys and intestinal segment were removed for determination of organ blood flow. The intestine was opened, rinsed with isotonic saline, blotted dry, weighed, and divided into 20-cm lengths. The middle 8 cm of each segment were left intact to measure total wall flow, and the remaining 12 cm were divided into mucosa-submucosa and muscularis-serosa fractions via blunt dissection. The kidneys were divided into smaller pieces for uniformity in the counting tubes. Organ and reference blood sample activities of 46Sc and 85Sr were measured in an LKB CompuGamma spectrometer (model 1282, LKB Instruments, Gaithersburg, MD). The error in measurement of the radioactivity induced by spillover of the isotopes was corrected using 46Sc and 85Sr microsphere standards.
Calculation of fractionated blood flow. Organ blood flow(mL/min) was calculated using the following equation Flow was normalized to milliliters·min-1·100 g-1 organ weight. The reliability of microsphere mixing during injection was assured by agreement within 10% of the total flow for right and left kidneys.
Calculation of 51Cr EDTA clearance. Equation where the perfusion rate was 1 mL·min-1 and the weight of the intestinal segment was measured in grams.
Experimental protocol. For the intestinal blood flow experiments, the preparation was allowed to stabilize until the flow and(a-v)o2 content difference were constant. To control for mechanical changes, which occur in blood flow and oxygen extraction after placement of any solution into the lumen, saline was placed into the lumen of the isolated intestinal segment, and all parameters were monitored for 30 min. The volume of saline used was that which resulted in the intestinal segment becoming full, but not distended, with fluid. Fifteen minutes after placement of saline into the lumen, blood samples were drawn for analysis of pH and blood gases. Thirty minutes after saline instillation, microspheres labeled with46 Sc were injected. Upon completion of the microsphere injection, capillary pressure was measured. After measurement of capillary pressure, the preparation was again allowed to stabilize until blood flow and (a-v)o2 content difference measurements were constant. The predigested and bile acid-solubilized sow's milk was then placed into the intestinal lumen of the isolated segment. Blood samples for pH and blood gases were again drawn at 15 min after instillation of sow's milk into the lumen, and at 30 min the microsphere procedure was repeated using 85Sr. Capillary pressure was measured a second time. The accuracy of the electromagnetic flowmeter measurements of blood flow was verified using a graduated cylinder after the animal was killed with an overdose of pentobarbital.
For the mucosal permeability experiments, each intestinal segment was perfused initially with saline for 20 min to assure that EDTA clearance was not elevated due to surgical trauma. Thereafter, the intestinal segments were perfused with predigested and solubilized sow's milk. 51Cr-EDTA(in a quantity sufficient to yield at least 2.5 × 107 cpm/L of plasma) was injected i.v. and allowed to equilibrate for 15 min. Aliquots of luminal perfusate and plasma samples (1 mL whole blood/sample = 3 mL total) for measurement of γ irradiation were then taken every 10 and 20 min, respectively, for 1 h. At the completion of the experiment, the intestinal segments were rinsed, blotted dry, and weighed.
Data analysis. All values are expressed as mean ± SEM. Oxygen uptake was calculated as the product of (a-v)o2 content difference and intestinal blood flow and was expressed as milliliters·min-1·100 g-1. Total vascular resistance, precapillary resistance, postcapillary resistance were calculated by dividing the appropriate pressure gradient by the normalized intestinal blood flow.
A two-factor repeated measures ANOVA, followed by Duncan multiple-rangepost hoc testing if the ANOVA showed differences among groups (SAS Institute, Inc., Cary, NC), was used to evaluate differences among age groups over time. Differences were considered significant at p < 0.05.
RESULTS
For the intestinal blood flow experiments,Tables 1, 2, and 3 summarize the average values for various hemodynamic and oxygenation parameters immediately before luminal instillation of predigested and solubilized sow's milk into the jejunoileum of piglets. Table 4 provides data for the average body weight and intestinal weight, length, and volume of milk instilled into the intestinal segment for the four age groups of piglets. Arterial blood pressure was constant within age groups throughout the entire experiment during placement of both saline and sow's milk into the lumen.
Significantly different hemodynamic responses after sow's milk were seen only for changes in (a-v)o2 (Fig. 1). The younger the animal, the greater the rise in (a-v)o2 for a given time period. Although statistical significance was not achieved for differences among age groups over time in total blood flow (measured electromagnetically) and total vascular resistance, there was a trend toward higher blood flow(Fig. 2) and lower vascular resistance(Fig. 3) in the older animals. Single point in time measurements of total blood flow with radiolabeled microspheres(Fig. 4) and postcapillary resistance(Fig. 5) at 30 min did, however, reach statistical significance. Most importantly, changes in oxygen uptake(Fig. 6) were not significantly different among age groups for any time period throughout the experiment.
For the mucosal permeability experiments, definite developmental differences were apparent as demonstrated in Fig. 7. All EDTA clearance values were significantly higher (p < 0.05) in 1-d-old, as compared with 3-d-old and 1-mo-old values. In four 1-d-old animals tested, there were no differences in mucosal permeability for freshversus frozen sow's milk so that all of the data for 1-d-olds was pooled for further analysis.
DISCUSSION
It has been observed that human milk feedings appear to decrease the incidence of necrotizing enterocolitis compared with infant (cow's milk-based) formulas(4, 9, 15–20). The incidence of neonatal sepsis and infantile diarrhea among infants fed breast milk is also felt to be lower than those fed formula(26, 27). The explanation for these findings is presently unknown, but mucosal barrier protection may be related to1) substances found in milk such as IgA(28, 29), milk leukocytes(30–32), growth factors(33–35), antioxidants(36), lactoferrin(37), lysozyme(29), and platelet-activating factor acetylhydrolase(38); 2) fewer fermentation products in mother's milk versus formula due to more efficient absorption of mother's milk(39); 3) the differences in nutrient composition [in particular, protein(40) and/or lipids(24)] in mother's milk compared with cow's milk;4) less dysmotility associated with mother's milk feeding(41, 42); and/or 5) differences in intestinal metabolic demand with mother's milk compared with infant formula.
Previous studies in developing piglets have demonstrated alterations in intestinal blood flow, but no differences in intestinal oxygenation with age in the presence of artificial piglet formula(21). It was found, however, that newborn animals appeared to have maximized their capacity to increase mucosal blood flow and oxygen extraction during the physiologic stress of feeding so that they may be at higher risk of mucosal injury with a superimposed cardiovascular stress (e.g. ischemia) due to an inability to maintain tissue oxygenation. Although intestinal blood flow has been evaluated for sow's milk, compared with infant formula, in young piglets(43), no previous studies have examined the intestinal metabolic demand (oxygen uptake) of sow's milk feeding nor the intestinal hemodynamic responses to sow's milk feeding among several age groups of developing piglets.
The primary difference between the hemodynamic response to mother's milk and that to artificial pig milk in 1-d-old piglets is that total intestinal blood flow increases (and vascular resistance decreases) with luminal mother's milk, whereas vascular constriction is maintained with artificial pigs milk. Furthermore, mucosal flow increases but not at the expense of muscularis flow with mother's milk compared with artificial pigs milk, both findings suggesting that there may be greater reserve capacity in the face of a superimposed oxidative stress (and less risk of mucosal injury) for moth[horizontal bar over]er's milk compared with artificial pigs milk. Speculation regarding the nature of these differences would have to center on either nutrient compositional differences between the two milks or vasoactive components in mother's milk that are not present in artificial pigs milk.
Theoretically, no differences among age groups in the increase in intestinal oxygen uptake during intraluminal mother's milk would imply no increased risk for mucosal injury in newborn, compared with older, intestine in the face of a superimposed oxidative stress. We found that there was indeed no difference in oxygen uptake among the different age groups, similar to the response to intraluminal artificial pigs milk formula(21). Although not technically feasible in our laboratory, measurement of mucosal Po2 would more specifically address the issue of cellular oxidative metabolism and may be more sensitive than are total wall oxygen uptake calculations in detecting changes at the level in which metabolic activity is greatest during nutrient absorption.
Although we observed no change in total wall oxygen uptake with mother's milk, we did observe a developmental difference in mucosal permeability during luminal perfusion with digested and solubilized sow's milk(Fig. 7), with mucosal permeability being significantly greater in 1-d-old intestine compared with that of the older age groups. Compared with artificial piglet formula(22), mucosal permeability in 1-d-old piglets was approximately 5-fold greater after perfusion with sow's milk, whereas there were no differences for 3-d- or 1-mo-old animals. Compared with preterm and term formulas(24), however, sow's milk caused a significantly smaller increase in mucosal permeability in 1-d-olds (10-fold less than preterm formula; 4-5 fold less than term formula). The increase in mucosal permeability was also 10-fold less in sow's milk-perfused, compared with preterm and term formula-perfused, intestine in 1-mo-old animals, although the overall increase in permeability was significantly lower than that for 1-d-olds.
In previous studies of mucosal permeability changes in response to luminal nutrients, no developmental differences have been demonstrated during luminal perfusion with artificial piglet formula, although imposition of ischemia and reperfusion caused injury which was greater in 1-d-old piglets compared with all older age groups(22). This increase in mucosal permeability could be abolished on removal of the lipid from the formula(23). With the higher fat content-containing human infant formulas, mucosal permeability was significantly increased in 1-d-old, compared with 1-mo-old, intestine, even in the absence of ischemia and reperfusion(24). Furthermore, in the presence of superimposed ischemia and reperfusion, necrotizing enterocolitis consistently and reproducibly occurred in newborn piglets during luminal perfusion with solubilized and digested preterm infant formula and this could be prevented by removal of the lipid from the preterm formula(24).
Interestingly, the increase in mucosal permeability for sow's milk was similar to that seen after removal of lipid from preterm formula in the absence of ischemia and reperfusion(24), despite sow's milk being of similar (or greater) fat content as preterm formula. Although it would have been of interest to determine whether sow's milk perfusion would prevent the development of necrotizing enterocolitis after ischemia and reperfusion, these studies could not be done due to difficulties with the sow's milk becoming gelatinous after 2-3 h despite being continuously stirred and warmed. One could reasonably speculate, however, that given the similar changes in mucosal permeability as with delipidated preterm infant formula, it is likely that perfusion with sow's milk would also not result in necrotizing enterocolitis after ischemia and reperfusion.
Thus, despite the high fat content in sow's milk, it may be more efficiently digested or mucosal injury may be counteracted by other“protective factors” in mother's milk. The fact that mucosal permeability was not different for fresh versus frozen milk argues against cellular elements in the milk playing a role in protection, at least in the context of our index of injury. The protection afforded by mother's milk also does not appear to be explained by changes in metabolic demand(oxygen uptake) based on the lack of age-related correlation with changes in mucosal permeability during intraluminal mother's milk, although measurement of mucosal Po2, if possible, may demonstrate changes at the mucosal level which are not evident on measurement of total wall oxygen uptake. Sow's milk does, however, appear to be less injurious to the intestinal mucosa of piglets than does either human infant preterm or term formula, although it is unknown whether this finding is generalizable to the human infant as relates to the issue of necrotizing enterocolitis.


Abbreviations
- (a-v)o2:
-
arteriovenous oxygen
- ANOVA:
-
analysis of variance
References
Reisner SH, Garty B 1977 Necrotizing enterocolitis despite breast feeding. Lancet 2: 507–507
Denes J, Gergely K, Wohlmuth G, Le'b J 1970 Necrotizing enterocolitis of premature infants. Surgery 68: 558–561
Stein H 1977 Necrotizing enterocolitis in black neonates. S Afr Med J 51: 199–200
Yu VYH, Tudehope DI, Gill GJ 1977 Neonatal necrotizing enterocolitis. 2. Perinatal risk factors. Med J Aust 1: 688–693
Bunton GL, Durbin GM, McIntosh N 1977 Necrotizing enterocolitis: controlled study of 3 years' experience in a neonatal intensive care unit. Arch Dis Child 52: 772–777
Guinan M, Schaberg D, Bruhn FW, Richardson CJ, Fox WW 1979 Epidemic occurrence of neonat˙al necrotizing enterocolitis. Am J Dis Child 133: 594–597
Eidelman AI, Inwood RJ 1980 Necrotizing enterocolitis and enteral feedings: is too much just too much?. Am J Dis Child 134: 545–546
Kliegman RM, Pittard WB, Fanaroff AA 1979 Necrotizing enterocolitis in neonates fed human milk. J Pediatr 95: 450–453
Wilson R, Kanto WP Jr, McCarthy BJ, Feldman RA 1982 Age of onset of necrotizing enterocolitis: risk factors in small infants. Am J Dis Child 136: 814–816
Moriartey RR, Finer NN, Cox SF 1979 Necrotizing enterocolitis and human milk. J Pediatr 94: 295–296
Eyal F, Sagi E, Arad I, Avital A 1982 Necrotizing enterocolitis in the very low birthweight infant: expressed breast feeding compared with parenteral feeding. Arch Dis Child 57: 274–276
Deleted in proof
Kosloske AM, Martin LW 1973 Surgical complications of neonatal necrotizing enterocolitis. Arch Surg 107: 223–228
Kliegman RM, Fanaroff AA 1981 Neonatal necrotizing enterocolitis: a nine-year experience. I. Epidemiology and uncommon observations. Am J Dis Child 135: 603–607
Marchildon MB, Buck BE, Abdenour G 1982 Necrotizing enterocolitis in the unfed infant. J Pediatr Surg 17: 620–624
Stoll BJ, Kanto WP Jr, Glass RI, Nahmias AJ, Brann AW Jr 1980 Epidemiology of necrotizing enterocolitis: a case control study. J Pediatr 96: 447–451
Krouskop R 1980 Influence of feeding practices in neonatal necrotizing enterocolitis. In: Brown EG, Sweet AY (eds) Neonatal Necrotizing Enterocolitis. Grune & Stratton, New York, pp 57–67
Lucas A, Cole TJ 1990 Breast milk and neonatal necrotizing enterocolitis. Lancet 336: 1519–1523
Frantz ID, L'Heureux P, Engel RR, Hunt CE 1975 Necrotizing enterocolitis. J Pediatr 86: 259–263
Brown EG, Sweet AY 1978 Preventing necrotizing enterocolitis in neonates. JAMA 240: 2452–2454
Crissinger KD, Burney DL 1991 Postprandial hemodynamics and oxygenation in developing piglet intestine. Am J Physiol 260:G951–G957
Crissinger KD, Granger DN 1989 Mucosal injury induced by ischemia and reperfusion in the piglet intestine: influences of age and feeding. Gastroenterology 97: 920–926
Crissinger KD, Tso P 1992 The role of lipids in ischemia/reperfusion-induced changes in mucosal permeability in developing piglets. Gastroenterology 102: 1693–1699
Crissinger KD, Burney DL, Velasquez OR, Gonzalez E 1994 An animal model of necrotizing enterocolitis induced by infant formula and ischemia in developing piglets. Gastroenterology 106: 1215–1222
Granger DN, Perry MA, Kvietys PR, Taylor AE 1983 A New method for estimating intestinal capillary pressure. Am J Physiol 244:G341–G344
Winberg J, Wessner G 1971 Does breast milk protect against septicaemia in the newborn?. Lancet 1: 1091–1094
Larsen SA Jr, Homer DR 1978 Relation of breastversus bottle feeding to hospitalization for gastroenteritis in a middle-class U.S. population. J Pediatr 92: 417–419
Goldman AS, Garza C, Nichols BL, Goldblum RM 1982 Immunologic factors in human milk during the first year of lactation. J Pediatr 100: 563–567
Peitersen B, Bohn L, Andersen H 1975 Quantitative determination of immunoglobulins, lysozyme, and certain electrolytes in breast milk during the entire period of lactation, during a 24-hour period, and in milk from the individual mammary gland. Acta Paediatr Scand 64: 709–717
Slade HB, Schwartz SA 1989 Antigen-driven immunoglobulin production by human colostral lymphocytes. Pediatr Res 25: 295–299
Speer CP, Gahr M, Pabst MJ 1986 Phagocytosis-associated oxidative metabolism in human milk macrophages. Acta Paediatr Scand 75: 444–451
Pitt J, Barlow B, Heird WC 1977 Protection against experimental necrotizing enterocolitis by maternal milk. I. Role of milk leukocytes. Pediatr Res 11: 906–909
Head JR 1977 Immunobiology of lactation. Semin Perinatol 1: 195–210
Petschow BW, Talbott RD 1991 Response ofBifidobacterium species to growth promoters in human and cow milk. Pediatr Res 29: 208–213
Zumkeller W 1992 Relationship between insulin-like growth factor-I and -II IGF binding proteins in milk and the gastrointestinal tract: growth and development of the gut. J Pediatr Gastrocnterol Nutr 15: 357–369
Buescher ES, McIlheran SM 1992 Colostral antioxidants: separation and characterization of two activities in human colostrum. J Pediatr Gastroenterol Nutr 14: 47–56
Kawakami H, Lonnerday B 1991 Isolation and function of a receptor for human lactoferrin in human fetal intestinal brush-border membranes. Am J Physiol 261:G841–G846
Moya FR, Eguchi H, Zhao B, Furukawa M, Sfeir J, Osorio M, Ogawa Y, Johnston JM 1994 Platelet-activating factor acetylhydrolase in term and preterm human milk: a preliminary report. J Pediatr Gastroenterol Nutr 19: 236–239
Alemi B, Hamosh M, Scanlon JW, Sal/mman-Mann C, Hamosh P 1981 Fat digestion in very low-birth-weight infants: effect of addition of human milk to low-birth-weight formula. Pediatrics 68: 484–489
Clark DA, Thompson JE, Weiner LB, McMillan JA, Schneider AJ, Rokahr JE 1985 Necrotizing enterocolitis: intraluminal biochemistry in human neonates and a rabbit model. Pediatr Res 19: 919–921
Tomomasa T, Hyman PE, Itoh K, Hsu JY, Koizumi T, Itoh Z, Kuroume T 1987 Gastroduodenal motility in neonates: response to human milk compared with cow's milk formula. Pediatrics 80: 434–438
Berseth CL 1989 Gestational evolution of small intestinal motility in preterm and term infants. J Pediatr 115: 646–651
Yao AC, Gootman PM, Frankfurt PP, DiRusso SM 1986 Effect of sow's milk versus formula on the superior mesenteric blood flow of newborn piglets. In: Tumbleson ME (ed) Swine in Biomedical Research. Plenum Press, New York, pp 1313–1318
Author information
Authors and Affiliations
Additional information
Supported by National Institutes of Health Grant DK 43785.
Rights and permissions
About this article
Cite this article
Crissinger, K., Burney, D. Intestinal Oxygenation and Mucosal Permeability with Luminal Mother's Milk in Developing Piglets. Pediatr Res 40, 269–275 (1996). https://doi.org/10.1203/00006450-199608000-00013
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199608000-00013