Abstract
The nitrogen washout technique usually involves exposure of the patient to 100% oxygen for several minutes. This may be dangerous in preterm infants who are at risk of retinopathy of prematurity (ROP). We wanted to know whether heliox (79% He, 21% O2) can be used instead of oxygen when determining functional residual capacity (FRC). FRC measurements were made in 14 preterm infants [median (range) gestational age at birth 34 wk (27-37 wk), and at time of study 36 wk (33-40 wk)] who were breathing room air. FRC was measured using a computerized infant pulmonary function system, beginning in random order with either 100% O2 followed by heliox or vice versa. There was no systematic difference between the two methods with regard to lung volume measurements: mean (SD) FRC values, corrected for body weight, were 22.9 (7.1) mL/kg for O2 and 23.4 (7.0) mL/kg for heliox. We did not observe a systematic influence of the type of washing gas used (heliox or oxygen) on FRC in these infants. Our results suggest that the use of heliox instead of pure oxygen may be a suitable and safer alternative for FRC measurements with the nitrogen washout technique in preterm infants who are breathing low concentrations of inspired oxygen and are still at risk of ROP.
Similar content being viewed by others
Main
Gas dilution techniques are increasingly used to assess FRC in infants. The nitrogen washout technique, however, which is one of the methods available for this purpose, requires exposure of the patient to 100% oxygen for several minutes to empty the lung completely of any residual nitrogen. This raises concern with regard to the application of this technique to preterm neonates because of the possible relationship between high blood oxygen levels and ROP(1). In this respect, it is particularly worrying that retinal vasoconstriction, which results from hyperoxemia and may be one of the pathomechanisms involved in ROP, can persist for more than 1 wk after exposure to hyperoxemia(2). It would therefore be desirable to develop a method that permits performance of the nitrogen washout procedure without exposing the patient to high oxygen levels.
The aim of this study was to assess the feasibility of using heliox to measure lung volume with the nitrogen washout technique. We wanted to know whether lung volume measurements obtained with this gas mixture would be comparable, both in vitro and in vivo, to those obtained with the “gold standard,” i.e. 100% oxygen.
METHODS
Subjects. We studied 14 preterm infants (10 boys; median gestational age at birth 34 wk, range 27-37 wk; median birth weight 1680 g, range 720-2530 g) who were clinically considered well, i.e. had no congenital malformations and no chronic lung disease. Their median postconceptional age at the time of study was 36 wk (33-40 wk), with a median weight of 1940 g (1520-2310 g). Two infants had been ventilated after birth(for 1 and 7 d, respectively), and five had required additional inspired oxygen; but all were breathing spontaneously, and none was receiving additional inspired oxygen at the time of study. All infants were studied in the supine position during spontaneous unsedated sleep, at least 30 min after their last feed.
It was estimated that paired measurements in 14 subjects would give a power of >90% to detect a difference between the two washing gases equivalent to 1 SD (i.e. 7 mL/kg) at the 5% significance level.
Written informed consent was obtained from parents of all infants and ethical approval to this study given by the institutional Ethics Committee.
Nitrogen washout (Fig. 1). Measurements were made using an open circuit nitrogen washout method based on the technique described by Gerhardt et al.(3). A computerized data acquisition system (Sensormedics 2600 Pediatric Pulmonary System, Anaheim, CA) was used. It continuously measures the volume of nitrogen expired after switching the inspired gas from room air to a nitrogen-free washout gas (100% oxygen or heliox in this study) at end-expiration. Assuming a constant bias flow, which has to exceed the patient's inspiratory peak flow during tidal breathing, the integrated expired N2 concentration is multiplied by the constant flow of the washout gas to obtain the volume of expired nitrogen. For each washout gas, a calibration factor was obtained before each measurement session from a two-point calibration with known volumes of N2(4). The test was complete when the nitrogen concentration in the mixing chamber reached 0%, which took approximately 1-2 min. The nitrogen concentration was measured photospectrometrically and the amount of washed-out nitrogen calculated by the computer from the area under the nitrogen concentration curve displayed on the screen. The computer calculation took the dead space of the face mask (10 mL) into account and corrected FRC values for body temperature and 100% water vapor saturation.
For the in vitro measurements, calibrated syringes were used as a model lung with known volumes (20, 40, 60, or 80 mL) and manually ventilated at a rate of 30-40/min with a stroke volume of 20 mL. The measurements were repeated 10 times for each volume and washing gas.
For the in vivo measurements, a face mask of appropriate size was used, and an airtight seal was achieved by placing a rim of therapeutic silicone putty between the infant's face and the mask. A constant bypass flow of room air (2 L/min) was used between FRC measurements to prevent an increase in minute ventilation due to the increased dead space otherwise created by the face mask. This bypass flow was stopped approximately 10 s before each FRC measurement. A pneumotachograph (Fleisch size 0) was introduced into the circuit to identify potential leaks at the face mask during test occlusions and to check whether the slide valve had truly been switched at end-expiration(4). Only measurements where this had been achieved and which also had a good washout curve were accepted. A period of at least twice the washout time was allowed between measurements. Measurements were repeated at least three times with each washout gas, and the mean of three technically acceptable measurements was taken for analysis(4). Infants were randomly allocated to start their measurement session with either oxygen first followed by heliox or vice versa.
Statistics. The means and coefficients of variation of the three measurements were calculated for each technique in each patient. Paired measurements were compared using the Wilcoxon matched pairs test. The limits of agreement were assessed using the method described by Bland and Altman(5) where the mean of the two techniques for each subject is plotted against the difference.
RESULTS
In vitro measurements. The results of the in vitro measurements are shown in Table 1. The mean difference between the known volumes and the measured volumes never exceeded 0.5 mL, independent of the volume or method (heliox or oxygen) chosen. There was no statistically significant difference between the volumes measured with the two methods or between the known and the measured volumes.
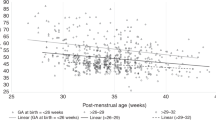
In vivo measurements. The individual results for all 14 infants are listed in Table 2 and shown in Figure 2. The mean (SD) of the FRC values, corrected for body weight, was 22.9 (7.1) mL/kg for oxygen and 23.4 (7.0) mL/kg for heliox(NS), giving a mean difference between the two measurements of 0.5 mL. The mean of the individual coefficients of variation was 10.1% for oxygen and 8.5% for heliox (NS). Hence, there was no systematic difference between the two methods with regard to either the lung volumes measured or the reproducibility of these measurements.
DISCUSSION
This study has shown that heliox as washing gas for the nitrogen washout technique yields results, both in vitro and in vivo, that are not systematically different from those obtained with the washing gas currently used most commonly with this method, i.e. 100% oxygen. Our data thus suggest that heliox, which appears to be safer than oxygen in preterm neonates because it is not associated with an increased risk of ROP, can be equally well used as oxygen for lung volume measurements in these patients.
That, theoretically, any oxygen/helium mixture can be used as the washing gas for the nitrogen washout technique was already suggested by Gerhardtet al.(3) in their original description of the open circuit nitrogen washout method. However, these authors did not provide any comparative measurements to validate this assumption. This is unfortunate because there are some concerns that breathing heliox may affect FRC. Heliox is significantly less dense than air and will therefore result in a considerable reduction in airway resistance during tidal breathing(6). Changes in airway resistance may in turn affect FRC(7). Whether this effect of heliox is also relevant to its use as a washout gas during FRC measurements, where exposure is limited to a few minutes and does also not occur immediately before the actual measurement, has not been studied previously. Our results suggest that it does not have a significant effect on FRC measurements, at least not in preterm infants without obstructive lung disease.
There are a number of technical limitations of the nitrogen washout gas technique which are independent of the type of washing gas used but should be considered in this context. First, measurement precision may be limited by the occurrence of leakage at the interface between face and mask and/or by the performance of measurements at stages in the respiratory cycle other than end-expiration. We controlled for these factors by using a pneumotachograph, which enabled us not only to exclude all measurements that were not performed at end-expiration, but also to detect potential leaks occurring between face and mask(4). Second, FRC measurements may be influenced by an increased dead space ventilation caused by the use of a face mask. This potential bias was avoided by providing a bypass flow of air between measurements. Third, FRC may vary with sleep state and/or breathing pattern(8). It has therefore been suggested that FRC measurements should ideally be confined to quiet sleep(9). However, there are several reports which failed to show a significant influence of sleep state on FRC(10–13). Moreover, episodes of quiet sleep are relatively infrequent and short in neonates(14), and our study design required performance of at least six consecutive FRC measurements during one period of spontaneous unsedated sleep. It was therefore considered impractical to confine measurements to episodes of quiet sleep only. This may explain why we observed a relatively high coefficient of variation in some infants during repeated measurements with the same washing gas, but is unlikely to have affected our data on the comparison between the two washing gases, because the sequence in which these gases were applied was varied randomly between patients.
It has been postulated that FRC may be lowered by breathing high concentrations of oxygen(15). This phenomenon, however, could not be verified by Boon et al.(16) when comparing lung volumes measured in room air and after breathing 100% oxygen for 3 min. Also, if oxygen rebreathing influences FRC, a progressive fall in FRC should occur during repeated measurements. This was not the case in either this or a previous study(4).
One reviewer pointed out that photospectrometers as used in the Sensormedics 2600 may lose their accuracy in the presence of helium. If this had been of relevance to this study, it should have caused a systematic difference in the values measured with the two washout gases and/or a higher coefficient of variation for heliox compared with oxygen. This was not the case in either the in vitro or the in vivo experiments(Tables 1 and 2). It should be stressed, however, that separate 2-point calibrations were performed for each washout gas,i.e. our measurements were corrected for any systematic influence heliox may have on the photospectrometric N2 analyzer.
We found a relatively large intersubject variability for FRC (Fig. 2). Our mean values, however, are similar to those reported by other investigators for the nitrogen washout technique in term and preterm infants(4, 17, 18). The high intersubject variability is thus most likely related to the heterogenicity of the population of infants studied (with birth weights ranging from 720 to 2530 g and gestational ages at birth from 27 to 37 wk) and/or to the fact that measurements were performed during both quiet and active sleep. There was also one patient in this study who showed low FRC values (<10 mL/kg) with both washout gases despite being clinically perfectly well. He was the smallest of all infants studied (1520 g, birth weight 800 g), but had never been ventilated and had not received additional inspired oxygen. This discrepancy between the FRC values measured and the clinical status of the infant is difficult to explain and may reflect the limitations of the nitrogen washout technique and/or of the Sensormedics system in very small infants.
In conclusion, we did not observe a systematic influence of the type of washing gas used (heliox or oxygen) on FRC in these preterm infants. We therefore suggest that heliox rather than pure oxygen should be used for FRC measurements with the nitrogen washout technique particularly in preterm infants who are still at risk of ROP.
Abbreviations
- FRC:
-
functional residual capacity
- ROP:
-
retinopathy of prematurity
- heliox:
-
mixture of 21% oxygen and 79% helium
References
Flynn JT, Bancalari E, Snyder ES, Goldberg RN, Feuer W, Cassady J, Schiffman J, Feldman HI, Bachynski B, Buckley E, Roberts J, Gillings D 1992 A cohort study of transcutaneous oxygen tension and the incidence and severity of retinopathy of prematurity. N Engl J Med 326: 1050–1054.
Aranda JV, Saheb N, Stern L, Avery ME 1971 Arterial oxygen tension and retinal vasoconstriction in newborn infants. Am J Dis Child 122: 189–194.
Gerhardt T, Hehre D, Bancalari E, Watson H 1992 A simple method for measuring functional residual capacity by N2 washout in small animals and newborn infants. Pediatr Res 19: 1165–1169.
Gappa M, Fletcher ME, Dezateux CA, Stocks J 1993 Comparison of nitrogen washout and plethysmographic measurements of lung volume in healthy infants. Am Rev Respir Dis 148: 1496–1501.
Bland JM, Altman DG 1986 Statistical methods for assessing agreement between two methods of clinical management. Lancet 1: 307–310.
Wolfson MR, Bhutani VK, Shaffer TH, Bowen FW 1984 Mechanics and energetics of breathing helium in infants with bronchopulmonary dysplasia. J Pediatr 104: 752–757.
Greenough A, Pool J, Price JF 1989 Changes in functional residual capacity in response to bronchodilator therapy among young asthmatic children. Pediatr Pulmonol 7: 9–11.
Henderson-Smart DJ, Read DJC 1979 Reduced lung volume during behavioral active sleep in the newborn. J Appl Physiol Respir Environ Exercise Physiol 46: 1081–1085.
American Thoracic Society/European Respiratory Society 1993 Society/European Respiratory Society 1993 Respiratory mechanics in infants: physiologic evaluation in health and disease. Am Rev Respir Dis 147: 474–496.
Moriette G, Chaussain M, Radvanyi-Bouvet M-F, Walti H, Pajot N, Relier J-P 1983 Functional residual capacity and sleep states in the premature newborn. Biol Neonate 43: 125–133.
Walti H, Moriette G, Radvanyi-Bouvet MF, Chaussain M, Morel-Kahn F, Pajot N, Relier JP 1986 Influence of breathing pattern on functional residual capacity in sleeping newborn infants. J Dev Physiol 8: 167–172.
Stokes GM, Milner AD, Newball EA, Smith NJ, Dunn C, Wilson AJ 1989 Do lung volumes change with sleep state in the neonate?. Eur J Pediatr 148: 360–364.
Beardsmore CS, MacFadyen UM, Moosavi SSH, Wimpress SP, Thompson J, Simpson H 1989 Measurement of lung volumes during active and quiet sleep in infants. Pediatr Pulmonol 7: 71–77.
Dittrichová J 1966 Development of sleep in infancy. J Appl Physiol 21: 1243–1246.
Geubelle F, Francotte M, Beyer M, Louis I, Loginoff MM 1977 Functional residual capacity and thoracic gas volume in normoxic and hyperoxic newborn infants. Acta Paediatr Belg 30: 221–225.
Boon AW, Ward-McQuaid JMC, Milner AD, Hopkin TE 1981 Thoracic gas volume, helium functional residual capacity and air-trapping in the first six hours of life: the effect of oxygen administration. Early Hum Dev 5: 157–166.
Sjöqvist BA, Sandberg K, Hjalmarson O, Olsson T 1984 Calculation of lung volume in newborn infants by means of a computer-assisted nitrogen washout method. Pediatr Res 18: 1160–1164.
Yuksel B, Greenough A, Chan V, Russell RR 1993 Comparison of helium dilution and nitrogen washout measurements of functional residual capacity in premature infants. Pediatr Pulmonol 16: 197–200.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Poets, C., Rau, G., Gappa, M. et al. Comparison of Heliox and Oxygen as Washing Gases for the Nitrogen Washout Technique in Preterm Infants. Pediatr Res 39, 1099–1102 (1996). https://doi.org/10.1203/00006450-199606000-00027
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199606000-00027