Abstract
Disturbances of the intestinal integrity, reflected by an increased intestinal permeability, are reported in cystic fibrosis (CF). Controversy exists whether the increased intestinal permeability is due to CF itself or a consequence of the concomitant exocrine pancreatic insufficiency (PI). We measured intestinal permeability by the sugar absorption test in 32 PI patients: 20 CF-PI, 12 nonCF-PI with chronic pancreatitis, and 50 controls. In the sugar absorption test, the lactulose/mannitol ratio is measured in 5-h urine samples after oral ingestion of a solution of lactulose and mannitol, hypersmolar by the addition of sucrose. The lactulose/mannitol ratio was increased in both CF-PI and nonCF-PI versus controls (p< 0.0001). In CF, the L/M ratio and permeability for lactulose and mannitol did not change by increasing pancreatic enzyme supplementation by 30-50% for 2 wk (p = 0.74, p = 0.97, p = 0.74, respectively) nor by decreasing the osmolarity of the test solution by 75% (p = 0.24, p = 0.10, p = 0.39, respectively). We conclude that an increased intestinal permeability in CF is probably a consequence of PI and is not related to the dose of pancreatic enzyme supplementation nor the osmolarity of the test solution. The increase is due to an increased permeability for lactulose which might point toward a defect in the tight junctions of the villi and/or crypts. The cause of the increased intestinal permeability in the presence of PI is still unclear. An increased intestinal permeability points toward an impaired functional integrity of the small bowel, which may contribute to gastrointestinal dysfunction in CF.
Similar content being viewed by others
Main
An increased intestinal permeability for medium-sized molecules, such as mannitol, and large molecules, such as lactulose, has been shown in various gastrointestinal diseases, including celiac disease and Crohn's disease(1–3). An increased intestinal permeability is thought to reflect an impaired functional integrity of the small bowel. Measurement of intestinal permeability for a combination of two probe molecules and expressing their urinary excretion as a ratio reduces the influence of several variables, such as gastric emptying, intestinal transit, and renal excretion, on the test results(3–5). On the other hand, measurement of their selective urinary excretion indicates which of the probe molecules is involved in the increase in intestinal permeability. A hyperosmolar test solution is found to discriminate better between normal and abnormal conditions of the small bowel(5, 6).
Abnormal conditions of the small bowel are also found in CF(7). Exocrine PI is the main gastrointestinal abnormality in CF. Besides PI, a number of other gastrointestinal abnormalities have been recognized, including abnormalities in motility, intestinal mucus, and bile acid metabolism. However, their importance for the pathophysiology of gastrointestinal disease in CF is not fully understood. Also an increased intestinal permeability is described in CF-PI(8–13), and could add to gastrointestinal dysfunction in CF.
Controversy exists whether an increased intestinal permeability in CF is an effect of CF itself, a consequence of the concomitant PI, or its treatment with pancreatic enzyme supplementation(10–12). To elucidate this controversy, we studied intestinal permeability by the SAT, using lactulose and mannitol, in CF patients with PI (CF-PI), and patients with PI due to chronic pancreatitis(nonCF-PI) versus controls. To study the influence of treatment of PI with pancreatic enzyme supplementation and the influence of the hyperosmolarity of the test solution, intestinal permeability was also measured in CF-PI with different doses of pancreatic enzyme supplementation and using a less hyperosmolar test solution.
METHODS
Patients. We studied 32 patients with PI, 20 CF-PI and 12 nonCF-PI, with PI secondary to chronic pancreatitis (n = 10) or subtotal pancreatectomy (n = 2). CF was confirmed by at least two abnormal sweat chloride determinations with chloride concentration >60 mmol/L(14). Chronic pancreatitis in nonCF-PI was established by clinical history, recurrent episodes of acute pancreatitis with increased serum amylase, and/or calcifications of the pancreas on x-ray. PI had been established by the occurrence of steatorrhea, in 19/20 CF patients by fat absorption <93%, and in chronic pancreatitis patients by total fecal fat excretion >5 g/24 h(12, 15). In the two patients with subtotal pancreatectomy, PI was based on clinical steatorrhea. Steatorrhea improved in all patients after the start of pancreatic enzyme supplementation. The Quetelet index was <20 in 6/12 nonCF-PI patients. Characteristics of the CF-PI patients are given in Table 1.
Fifty healthy controls were drawn from the children of the medical staff(n = 24) and the medical staff itself (n = 26). None of them had a family history associated with either PI or CF, no one was receiving any medication or was known to use alcohol excessively. Detailed results of the controls are reported elsewhere(16). Intestinal permeability in the children was not different from that in the medical staff itself (p = 0.52). Therefore, results from both groups were combined.
Procedures. In 26 of the 32 patients with PI, the SAT was performed after the start of pancreatic enzyme supplementation. In these patients, pancreatic enzyme supplementation was continued except for the day when the SAT was performed. In the remaining six patients, five with nonCF-PI, pancreatic enzyme supplementation was started after the SAT had been performed. In 10 CF-PI patients, the SAT was repeated after increasing the pancreatic enzyme supplementation 30-50% for 2 wk.
Sugar absorption test. After an overnight fast of 8 h in subjects older than 2 y, and of 4 h in younger subjects, the subject drank the standard hyperosmolar test solution (2 mL/kg, maximum 100 mL) containing 5 g of lactulose, 2 g of mannitol, and 40 g of sucrose made up to 100 mL with demineralized water. The osmolarity of the test solution was 1560 mosm/L. The subject continued to fast for 2 h. All urine passed in the 5 h after test fluid ingestion was collected, and 0.5 mL of chlorohexidine digluconate 20% was added as a preservative. The urine volume was measured, and samples were stored frozen at -20°C. Samples were analyzed for lactulose, mannitol, and sucrose by gas chromatography by our laboratory of clinical chemistry as previously described(16, 17). The urinary excretion of lactulose, mannitol, and sucrose was expressed as a percentage of the ingested dose. The L/M ratio was expressed as (lactulose excretion divided by mannitol excretion) × 100%.
In nine CF-PI patients, intestinal permeability was also measured with a 75% less hyperosmolar test solution (378 mosm/L) by omitting sucrose from the test solution. Besides the difference in osmolarity of the test solution, the test procedure was identical to that of the SAT with the standard hyperosmolar test solution.
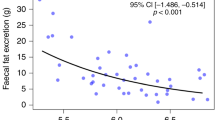
Data analysis. The normal range (χ ± 2 SD) in controls for lactulose excretion was 0-1.4%, for mannitol 4.8-28.8%, for sucrose 0-1.7%, and for the L/M ratio 0-7.2%. For variables with a skewed distribution, the Mann-Whitney U test was used. The t test for paired samples was used for the results in the CF-PI with different test solutions or different doses of pancreatic enzyme supplementation. Correlations were determined by Pearson's correlation coefficient. For all tests, a p value <0.05 was considered statistically significant.
RESULTS
Standard hyperosmolar test solution. The median L/M ratio did not differ in CF-PI and nonCF-PI (p = 0.20). The L/M ratio was higher in both CF-PI and nonCF-PI than in controls (both p < 0.0001). The L/M ratio was increased in 14/20 (70%) of CF-PI, 10/12 (83%) of nonCF-PI, and in 2/50 (4%) of the controls (Fig. 1)
The median lactulose excretion did not differ in CF-PI and nonCF-PI(p = 0.17). The lactulose excretion was higher in both CF-PI and nonCF-PI than in controls (both p < 0.0001). The lactulose excretion was increased in 12/19 (63%) CF-PI, 7/12 (58%) nonCF-PI, and 2/50(4%) of the controls (Fig. 2).
The median mannitol excretion in CF-PI was higher than in both nonCF-PI(p < 0.01), and controls (p < 0.0005). The mannitol excretion did not differ in nonCF-PI and controls (p = 0.56). The mannitol excretion was increased in 10/19 (53%) CF-PI, and 2/50 (4%) of the controls. The mannitol excretion was decreased in 2/19 (11%) CF-PI and 2/50(4%) of the controls (Fig. 3).
The median sucrose excretion did not differ in CF-PI and nonCF-PI(p = 0.06). The sucrose excretion in CF-PI (p < 0.005), but not in nonCF-PI (p = 0.71), was higher than in controls. However, the sucrose excretion was not increased in any of the CF-PI, and increased in 1/49 (2%) of the controls.
Pancreatic enzyme supplementation. In all patients with PI, the L/M ratio was not different in patients with (n = 26) or without(n = 6) pancreatic enzyme supplementation before the SAT(p = 0.16).
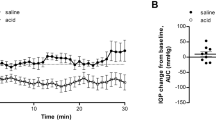
In 10 CF-PI, the L/M ratio, and intestinal permeability for lactulose and mannitol did not change by increasing the pancreatic enzyme supplementation with 30-50% for 2 wk (p = 0.74, p = 0.97, p = 0.74, respectively) (Fig. 4A). In the 17 CF-PI using the same preparation of pancreatic enzyme supplementation, the L/M ratio was not related to the amount of supplementation (r = -0.017, p = 0.95).
The L/M ratio and permeability for lactulose(L) and mannitol (M) in CF patients with PI with different doses of pancreatic enzyme supplementation: (A) normal, with normal pancreatic enzyme supplementation: extra, after 30-50% increased supplementation for 2 wk; and different osmolarities of the test solution: (B) hyper, standard hyperosmolar test solution;75% less hyper, 75% less hyperosmolar test solution. - = median value, ····· = mean value. For convenience, permeability for mannitol is expressed as percentage of ingested dose × 10-1 in both figures.
Osmolarity of the test solution. In 9 CF-PI, the L/M ratio, and intestinal permeability for lactulose and mannitol were not different when determined with the standard hyperosmolar or 75% less hyperosmolar test solution (p = 0.24, p = 0.10, p = 0.39, respectively) (Fig. 4B).
Nutritional status. In all patients with PI, the L/M ratio was not different in patients with (n = 13) or without (n = 19) malnutrition (p = 0.31), defined as weight for height ≤ P10 in CF patients and Quetelet index ≤ 20 in nonCF patients. In CF patients with PI, the L/M ratio was not different in patients with (n = 7) or without (n = 13) malnutrition (p = 0.36).
DISCUSSION
In this study, we showed that a three to four times increased intestinal permeability, as measured by the SAT, occurs not only in CF-PI but also in nonCF-PI. The increased L/M ratio in CF-PI and nonCF-PI is mainly caused by an increased permeability for lactulose. Furthermore, in CF-PI, the increased L/M ratio and permeability for mannitol and lactulose were not related to the dose of pancreatic enzyme suplementation or the osmolarity of the test solution.
Our observations extend the results of two articles in which CF-PI and nonCF-PI were studied(11, 12). In the first article(11), only six nonCF-PI (three with chronic pancreatitis, three of Schwachman's syndrome) patients were studied. All six patients had an increased L/M ratio due to increased lactulose and decreased mannitol excretion(11). In the second article(12), lactulose excretion was increased both in the 14 CF-PI patients and six patients with PI due to Schwachman's syndrome. The theoretical drawback of the second study is that, as only one probe molecule was used, the results cannot account for several variables such as gastric emptying, intestinal transit, and renal excretion(4, 5). Interestingly in the second article, lactulose excretion was not increased in 21 patients without PI, defined as fat absorption ≥93% (17 CF cases; four Schwachman's syndrome cases). Together with these findings, our results suggest that PI, unrelated to its cause, is associated with an increased intestinal permeability. An increased intestinal permeability in PI may be induced by iatrogenic factors including treatment with pancreatic enzyme supplementation and the hyperosmolarity of the test solution.
Treatment of PI with pancreatic enzyme supplementation may damage the small bowel resulting in an increased intestinal permeability. However, in our study, intestinal permeability was not different in patients with or without pancreatic enzyme supplementation, nor related to the dose of pancreatic enzyme supplementation in 17 cases of CF-PI using the same preparation of pancreatic enzyme supplementation. Furthermore, increasing the amount of pancreatic enzyme supplementation by 30-50% for 2 wk did not change intestinal permeability. Intestinal permeability was increased both in studies with discontinuation(12) and without discontinuation of pancreatic enzyme supplementation(11) (results of our study). These findings suggest that pancreatic enzyme supplementation has no major effect on intestinal permeability.
The hyperosmolarity of the test solution may increase intestinal permeability(1). To eliminate the effect of hyperosmolarity, we measured intestinal permeability also with a 75% less hyperosmolar test solution by omitting sucrose. We found that intestinal permeability (L/M ratio, lactulose and mannitol) in CF-PI was not different using either test solution.
Several hypotheses exist for the possible role of PI in increased intestinal permeability of the small bowel. PI may cause histologic damage to the small bowel by a decreased intraluminal pH due to an increased gastric acid and decreased pancreatic bicarbonate secretion(18). The histologic damage would result in an impaired functional integrity reflected by an increased intestinal permeability. In nonCF-PI, histologic abnormalities have been found(19). In CF-PI, histologic abnormalities as a result of gastric and small bowel damage are thought to be uncommon(20). However, we found histologic abnormalities, swollen mucous secreting cells between the epithelial cells of the crypts and the villous epithelium with accumulation of mucous at the surface in both stomach and small bowel, at autopsy in three CF-PI patients after lung transplantation. This is in accordance with the study of Oppenheimer and Esterly(21) and fetal abnormalities found by Gosden and Gosden(22). As no intestinal biopsies were performed in our patients, the existence of these histologic abnormalities and their possible role in increased intestinal permeability in CF cannot completely be excluded.
A second hypothesis concerns severe malnutrition, which is often found in PI, and which may impair functional integrity of the small bowel(23, 24). However, although 7 of 20 CF-PI patients had severe malnutrition (weight for height ≤10th percentile), the L/M ratio was not different in CF-PI with or without malnutrition.
Although in our study the L/M ratio was increased in both CF-PI and nonCF-PI, differences existed between the two groups in the excretion of lactulose, mannitol, and sucrose. The excretion of all three probe molecules tended to be higher in CF-PI than in nonCF-PI, although reaching significance only for mannitol. Several factors may account for the differences. First, the unstirred layer on the villi is significantly decreased as a consequence of CF(25), which may cause an increase in uptake of the probes in CF-PI. Second, intestinal transit is probably shortened in nonCF-PI(26), but prolonged in CF-PI(10, 11, 27, 28), which may lead to increased uptake of the three probes(29). Third, theVmax of Na+-linked glucose entry, produced by sucrose hydrolysis, is two to three times increased in CF, apparently due to the increased membrane potential of the luminal membrane due to the Cl- impermeability(30). The enhanced glucose uptake may provide a driving force for the paracellular fluid movement (solvent drag) and may also increase the junctional permeability, especially for mannitol(31, 32). However, as we found no differences in permeability for lactulose and mannitol using a solution with sucrose or without sucrose, our findings do not support the latter hypothesis. The fact that no differences were found could partly be explained by a decreased hydrolysis of sucrose in CF, reflected by sucrosuria in CF(33) (results of our study), and/or point toward other pathways for permeability of these probes.
The pathways for permeability of lactulose and mannitol are yet unknown. Hollander proposed that water-soluble molecules most likely pass through the tight junctions of the intestinal epithelium(34). The tight junctions in the villi are “tighter” than those in the crypts. Therefore, absorption of lactulose would predominantly take place in the crypts, whereas absorption of mannitol, would take place both in the crypts and the villi(34). We hypothesize that the increased intestinal permeability in CF-PI may result from functional changes of the tight junctions in the villi or the crypts. In rabbits, these functional changes, leading to increased intestinal permeability for lactulose, can be induced by bile acids(35). This increase was thought to result from loosening of the tight junctions in the villi. Whether these changes play a role in CF, in which alteration of the metabolism of bile acids have been described(36), remains a matter of debate.
In summary, an increase in intestinal permeability, as measured by the SAT, occurs in PI unrelated to its cause and independent of pancreatic enzyme supplementation, or the osmolarity of the test solution. However, differences in the urinary excretion of lactulose, mannitol, and sucrose exist between CF-PI and nonCF-PI, which may be due to a specific defect in CF. An increased intestinal permeability by enhancing fluid absorption, dehydration of the luminal contents, and distal ileal obstruction may contribute to gastrointestinal dysfunction in CF.
Abbreviations
- CF:
-
cystic fibrosis
- PI:
-
pancreatic insufficiency
- L/M ratio:
-
lactulose/mannitol ratio
- SAT:
-
sugar absorption test
References
Travis S, Menzies IS 1992 Intestinal permeability: functional assessment and signficance. Clin Sci 82: 471–488.
Van Elburg RM, Uil JJ, Mulder CJJ, Heymans HSA 1993 Intestinal permeability in patients with coeliac disease and relatives of patients with coeliac disease. Gut 34: 354–357.
Van Elburg RM, Uil JJ, De Monchy JGR, Heymans HSA 1992 Intestinal permeability in pediatric gastroenterology. Scand J Gastroenterol 27( suppl): 19–24.
Menzies IS 1974 Absorption of intact oligosaccharides in health and disease. Biochem Soc Trans 2: 1042–1047.
Menzies IS 1983 Transmucosal passage of inert molecules in health and disease. In: Skadhauge E, Heintze K (eds) Intestinal Absorption and Secretion. Falk Symposium 36. MTP Press, Lancaster, pp 527–543.
Wheeler PG, Menzies IS, Creamer B 1978 Effect of hyperosmolar stimuli and coeliac disease on the permeability of the human gastrointestinal tract. Clin Sci Mol Med 54: 495–501.
Heymans HSA 1989 Gastrointestinal dysfunction and its effect on nutrition in CF. Acta Paediatr Scand Suppl 363: 74–79.
Leclercq-Foucart J, Forget PP, Sodeyez-Goffaux F, Zappitelli A 1986 Intestinal permeability to [51Cr]EDTA in children with cystic fibrosis. J Pediatr Gastroenterol Nutr 5: 384–387.
Leclercq-Foucart J, Forget PP, Van Cutsem JL 1987 Lactulose-rhamnose intestinal permeability in children with cystic fibrosis. J Pediatr Gastroenterol Nutr 6: 66–70.
Dalzell AM, Freestone NS, Billington D, Heaf DP 1990 Small intestinal permeability and orocaecal transit time in cystic fibrosis. Arch Dis Child 65: 585–588.
Murphy MS, Sheldon W, Brunetto A, Pearson ADJ, Laker MF, Eastham EJ, Nelson R 1989 Active and passive sugar absorption in pancreatic insufficiency. J Pediatr Gastroenterol Nutr 8: 189–194.
Mack DR, Flick JA, Durie PR, Rosenstein BJ, Ellis LE, Perman JA 1992 Correlation of intestinal lactulose permeability with exocrine pancreatic dysfunction. J Pediatr 120: 696–701.
Schaad U, Kraemer R, Gaze G, Hadorn B 1978 One-hour blood xylose in cystic fibrosis. Arch Dis Child 53: 756–757.
di Sant'Agnese PA, di Sant'Agnese PA, Darling RC, Perera GA 1953 Sweat electrolyte disturbances associated with childhood pancreatic disease. Am J Med 15: 777–784.
Schmerling DH, Forrer JCW, Prader A 1970 Fecal fat and nitrogen in healthy children and in children with malabsorption or maldigestion. Pediatrics 46: 690–695.
Van Elburg RM, Uil JJ, Kokke FTM, Mulder AM, van de Broek WGM, Mulder CJJ, Heymans HSA 1995 Repeatability of the sugar absorption test, using lactulose and mannitol, for measuring intestinal permeability for sugars. J Pediatr Gastroenterol Nutr 20: 184–188.
Jansen G, Muskiet FAJ, Schierbeek H, Berger R, Van der Slik W 1986 Capilary gas chromatographic profiling of urinary, plasma derivates, preceded by a simple and rapid prepurification method. Clin Chim Acta 157: 277–294.
Cox KL, Isenberg JN, Ament ME 1982 Gastric acid hypersecretion in cystic fibrosis. J Pediatr Gastroenterol Nutr 1: 559–565.
Senelas-Balas F, Bastie MJ, Balas D, Escourrou J, Bommelaer G, Bertrand C, Arany Y, Ribet A 1982 Histological variations of the duodenal mucosa in chronic human pancreatitis. Dig Dis Sci 27: 917–922.
Eggermont E, De Boeck K 1991 Small intestinal abnormalities in cystic fibrosis patients. Eur J Pediatr 150: 824–828.
Oppenheimer EH, Esterly JR 1975 Pathology of cystic fibrosis. Review of the literature and comparison with 146 autopsies cases. Perspect Pediatr Pathol 2: 241–278.
Gosden CM, Gosden JR 1984 Fetal abnormalities in cystic fibrosis suggest a deficiency in proteolysis of cholecystokinin. Lancet 2: 541–546.
Lunn PG, Northrop-Clewes CA, Downes RM 1991 Intestinal permeability, mucosal injury, and growth faltering in Gambian infants. Lancet 338: 907–910.
Heyman M, Boudraa G, Sarrut S, Giraud M, Evans L, Touhami M, Desjeux JF 1984 Macromolecular transport in jejunal mucosa of children with severe malnutrition: a quantitative study. J Pediatr Gastroenterol Nutr 3: 357–363.
Sinaasappel M 1992 Relationship between intestinal function and chloride secretion in patients with cystic fibrosis. Neth J Med 41: 110–4.
Layer P, Rippel K, von der Ohe M, Groger G, Holtmann G, Goebell H 1993 Altered fed and interdigestive intestinal motility in severe pancreatic insufficiency. Gastroenterology 104:A539.
Bali A, Stableforth DE, Asquith P 1983 Prolonged small-intestinal transit time in cystic fibrosis. BMJ 287: 1011–1012.
Escobar H, Perdomo M, Vasconez F, Camarero C, del Olmo MT, Suarez L 1992 Intestinal permeability to 51Cr-EDTA and orocaecal transit time in cystic fibrosis. J Pediatr Gastroenterol Nutr 14: 204–207.
Brunetto AL, Pearson ADJ, Gibson R, Bateman DN, Rashid MU, Laker MF 1990 The effect of pharmacological modification of gastric emptying and mouth-to-caecum transit time on the absorption of sugar probe marker molecules of intestinal permeability in normal man. Eur J Clin Invest 20: 279–284.
Baxter P, Goldhill J, Hardcastle J, Hardcastle PT, Taylor CJ 1990 Enhanced intestinal glucose and alanine transport in cystic fibrosis. Gut 31: 817–820.
Pappenheimer JR, Volpp K 1992 Transmucosal impedance of small intestine: correlation with transport of sugars and amino acids. Am J Physiol 263:C480–C493.
Bijlsma PB, Peeters RA, Groot JA, Dekker PR, Taminiau JAJM, Meer R van der 1995 Differential in vivo and in vitro intestinal permeability to lactulose and mannitol in animals and man: a hypothesis. Gastroenterology 108: 687–696
Gryboski JD, Thayer WR, Gabrielson IW, Spiro HM 1963 Disacchariduria in gastrointestinal disease. Gastroenterology 45: 633–637.
Hollander D 1992 The intestinal permeability barrier. A hypothesis as to its regulation and involvement in Crohn's disease. Scand J Gastroenterol 27: 721–726.
Fasano A, Budillon G, Guandalini S, Cuomo R, Parrilli G, Cangiotti AM, Morroni M, Rubino A 1990 Bile acids reversible effects on small intestinal permeability. An in vitro study in the rabbit. Dig Dis Sci 35: 801–8.
Roy CC, Weber AM, Lepage G, Smith L, Levy E 1988 Digestive and absorptive phase anomalies associated with exocrine pancreatic insufficiency of cystic fibrosis. J Pediatr Gastroenterol Nutr 7( suppl): S1–S7.
Acknowledgements
The authors thank Prof. Dr. W. G. Zijlstra for his helpful suggestions in the preparation of the manuscript.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Van Elburg, R., Uil, J., Van Aalderen, W. et al. Intestinal Permeability in Exocrine Pancreatic Insufficiency Due to Cystic Fibrosis or Chronic Pancreatitis. Pediatr Res 39, 985–991 (1996). https://doi.org/10.1203/00006450-199606000-00010
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199606000-00010
This article is cited by
-
The Enigmatic Gut in Cystic Fibrosis: Linking Inflammation, Dysbiosis, and the Increased Risk of Malignancy
Current Gastroenterology Reports (2017)
-
Does probiotic supplementation affect pulmonary exacerbation and intestinal inflammation in cystic fibrosis: a systematic review of randomized clinical trials
World Journal of Pediatrics (2017)
-
Disrupted tight junctions in the small intestine of cystic fibrosis mice
Cell and Tissue Research (2014)