Abstract
We determined whether antithrombin (AT III) or hirudin (a specific thrombin inhibitor) reduce both the accumulation of fibrinogen in lung parenchyma and the procoagulant activity of bronchoalveolar lavage (BAL) fluid during acute lung injury induced by pulmonary overdistention. Newborn piglets were randomized to six-hourly infusions of AT III concentrate, a continuous infusion of recombinant hirudin, or no anticoagulant therapy. All animals were subjected to 24 h of identical mechanical ventilation at high peak pressures(3.9 kPa or 40 cm H2O). Tidal volumes were raised to a mean of 69 mL/kg in all three groups. Mean AT III levels in supplemented piglets (n = 22) were increased to 1.46 (SD 0.24) U/mL at 24 h, compared with 0.67 (SD 0.16) U/mL in controls (n = 23). The median activated partial thromboplastin time in animals receiving hirudin (n = 18) was prolonged to 53 s versus 34 s in untreated animals. The intrapulmonary accumulation of i.v. administered 125I-fibrinogen was reduced by AT III concentrate or hirudin, compared with untreated littermates(p = 0.003). The procoagulant activity of BAL fluid was also decreased by both thrombin inhibitors (p = 0.001). Intrapulmonary accumulation of fibrinogen and the procoagulant activity of BAL fluid were reduced by AT III or hirudin during lung injury caused by pulmonary overdistention. Future investigations should determine whether tangible clinical benefits result from this reduced potential for fibrin deposition in the injured lung.
Similar content being viewed by others
Main
Interstitial and alveolar fibrin deposition is a pathognomonic feature of acute lung injury(1). The presence of fibrin implies that clotting occurs in the extravascular compartment of the injured lung. There is also evidence that acute lung injury is associated with intravascular activation of the coagulation system. Postmortem studies in patients with neonatal or adult respiratory distress syndrome frequently show microvascular thrombosis in the lung as well as in other organs(2–4). In addition, Schmidt et al.(5) have recently demonstrated a significant correlation between the plasma concentration of thrombin/antithrombin complexes, a biochemical marker of thrombin formation, and the severity of neonatal respiratory distress syndrome.
These observations support, but do not prove, the hypothesis that thrombin formation and fibrin deposition exacerbate acute lung injury. It is conceivable that thrombin may simply be a coincidental marker of the disease process, rather than a cause of lung injury. To exclude this possibility, intervention trials with suitable thrombin inhibitors are necessary in experimental animals and, ultimately, in humans(6). So far, such studies have been scarce; moreover, more recent observations have largely been confined to animal models of endotoxemia(7, 8).
The objective of the present experiments in newborn piglets was therefore to determine whether two different thrombin inhibitors, AT III and hirudin, would reduce the intrapulmonary accumulation of circulating125 I-fibrinogen as well as the procoagulant activity of BAL fluid during acute lung injury induced by pulmonary overdistention through mechanical ventilation at high airway pressures.
METHODS
Animals
One- to two-day-old Yorkshire piglets of either sex were obtained from a closed herd with excellent health status (Arkell Swine Research Centre, University of Guelph, Ontario, Canada). For the main series of experiments, 69 piglets were studied in groups of three littermates from 23 litters. In addition, four healthy unintubated and unventilated piglets from four different litters were used in initial pilot experiments to establish the specificity of two outcome measures, i.e. lung uptake of circulating125 I-fibrinogen and lung histology. All animal procedures were carried out in accordance with the guidelines of the Canadian Council on Animal Care, and the regulations under the Province of Ontario “Animals for Research Act.” The experimental protocol was approved by the local Animal Research Ethics Board.
Anesthesia and Surgical Procedures
Piglets were weighed and sedated with an intraperitoneal injection (30 mg/kg) of sodium pentobarbital (Somnotol, MTC Pharmaceuticals, Cambridge, Ontario). Endotracheal 3.5 Fr tubes (Concord/Portex, Keene, NH) were placed via tracheostomies and connected to Healthdyne ventilators (model 102, Healthdyne Inc., Marietta, GA). Initial ventilator settings were chosen to ensure physiologic gas exchange: peak inspiratory pressure 1.5 kPa (15 cm H2O), positive end-expiratory pressure 0.3 kPa (3 cm H2O), inspiratory time 0.5 s, respiratory rate 30 breaths/min. A humidified gas mixture (warmed to 38°C) of 40% oxygen in nitrogen was delivered at 8 L/min. A 3.5 Fr Argyle umbilical vessel catheter (Sherwood Medical, St. Louis, MO) was inserted into the umbilical vein and advanced 5 cm for the administration of maintenance fluids (5% dextrose at 80 mL/kg/d), prophylactic ampicillin (100 mg·kg-1·d-1; Novopharm Ltd., Toronto, Ontario), and amikacin (15 mg·kg-1d-1; Bristol-Myers, Toronto, Ontario), as well as further doses of pentobarbital. The left carotid artery was cannulated with a second 3.5 Fr Argyle umbilical vessel catheter, which was secured at 5 cm, perfused with normal saline (1.5 mL/h), and used for blood sampling and continuous monitoring of blood pressure. To prevent tension pneumothorax, bilateral 10 Fr trocar catheters(Sherwood Medical, St. Louis, MO) were inserted into the chest, advanced 2 cm, and connected to Heimlich chest drain valves (Becton Dickinson Co, Lincoln Park, NJ). After these procedures, piglets were allowed to recover in prewarmed isolettes for 2 h.
Throughout the entire study period, piglets were regularly monitored for maintenance of adequate sedation, core temperature, heart rate, blood pressure, oxygen saturation, serum glucose, and urine output. If needed, sodium bicarbonate (4.2%) was given to correct metabolic acidosis. Suprapubic bladder punctures were performed every 6 h.
Experimental Protocol
To create lung injury, methods described by Tsuno et al.(9) were modified as follows. Peak inspiratory ventilator pressures were increased to 3.9 kPa (40 cm H2O), and delivered at a flow rate of 15 L/min. Positive end-expiratory pressure was reduced to 0.2 kPa(2 cm H2O), respiratory rate 20 breaths/min, whereas the inspiratory time was prolonged to 1.2 s. These maneuvers raised tidal volumes 4-5-fold. To maintain Paco2 values between 3.3 and 4.0 kPa (low enough to suppress spontaneous breathing), the dead space volume of the ventilator circuit was increased. The fraction of inspired oxygen was increased as necessary to maintain Hb oxygen saturations above 90%. During the 24-h period of mechanical ventilation at high peak pressures, the animals were nursed on either side, alternating every 6 h.
At the beginning of each experiment, three littermates were randomized(using a random number table) to receive human AT III concentrate (Kybernin, Behringwerke AG, Marburg, Germany), recombinant hirudin (Behringwerke AG, Marburg, Germany), or no anticoagulant therapy. An initial i.v. AT III loading dose of 100 U/kg was followed by six-hourly injections of 50 U/kg. On four occasions, the initial AT III dose was increased to 250 U/kg, and followed by six-hourly maintenance doses of 100 U/kg. Hirudin was administered as a continuous i.v. infusion at a rate of 3μg·kg-1·min-1, after an initial bolus injection of 180 μg/kg. Substantially higher infusion rates were found to cause serious bleeding in the first three animals.
Measurements
Pulmonary overdistention. Expiratory tidal volumes were determined throughout all experiments using the Neonatal Volume Monitor (Bear Medical Systems, Riverside CA).
Hematologic studies. Coagulation tests were performed in platelet-poor citrated plasma samples which had been stored at -70°C for batch assaying. A previously described microtechnique was used to measure the PTT(10). AT III activity was measured chromogenically(S-2238; Kabi Vitrum, Stockholm, Sweden). All standard curves were prepared using pooled plasma from 10 adult pigs. Platelet counts were determined in EDTA-anticoagulated blood samples using a Coulter counter (Coulter Electronics, Miami, FL).
Procoagulant activity of BAL fluid. BAL was performed in 13 litters immediately after each animal had been killed by an i.v. injection of sodium pentobarbital. The entire lung was lavaged in situ with 5 mL/kg of sterile 0.9% saline, while the piglet was held in an upright position. With the animal in the supine position, a suction catheter was then advanced to the tip of the endotracheal tube. Approximately 80% of the instilled fluid volume was recovered through careful aspiration. BAL samples were centrifuged at 3000 rpm for 10 min, and the supernatant was stored at-70°C until assayed. The procoagulant activity of the BAL sample (BAL plasma recalcification time) was quantitated as described by O'Brodovichet al.(11) using normal adult plasma.
Lung uptake of circulating 125I-fibrinogen. Human fibrinogen was labeled in the regional radiopharmacy with 125I using a previously published modification of McFarlane's method(12). On average, 97% of the labeled protein was clottable. 125I-Fibrinogen (185 kBq) was injected i.v. at time 0. At autopsy, the right lung was selectively perfused with 60 mL of normal saline through its pulmonary artery to clear 125I-fibrinogen from the intravascular space(13). The lung was then isolated and counted for 5 min in a standardized manner using a large diameter, thallium-activated sodium iodide crystal (Harshaw Chemical Co, Solon, OH). The sample-to-detector distance was large (40 cm) to minimize any sample size effects. A low background environment was created by the shadow shield of a whole body counter. The multichannel analyzer was set to detect the 28 keV photons emitted by 125I. Pulmonary uptake of 125I-fibrinogen was expressed as counts per 5 min in 1 g of wet lung tissue/counts per minute in 1 mL of whole blood at the end of each experiment.
Histologic examinations. The piglet left lung was immersed in 10% buffered formalin. After fixation for 24 h, the lung was sliced and samples from all lobes were embedded in paraffin. The samples were selected to provide a view of the lung from the hilum to the pleura. Sections cut at 5μm were stained with hematoxylin/eosin or phosphotungstic acid/hematoxylin. Slides were scored as follows:
-
Grade 0. No or focal and slight pathologic changes, involving less than 50% of the lung section.
-
Grade 1. Mild lung injury: interstitial edema, infiltration of alveolar walls with inflammatory cells, and atelectasis leading to thickening of alveolar walls. Changes involve more than 50% of the lung section.
-
Grade 2. Moderate lung injury: alveolar edema, hyaline membrane formation, alveolar wall necrosis, epithelial necrosis of terminal bronchioles. Changes involve less than 50% of the lung section.
-
Grade 3. Severe lung injury: same pathology as in grade 2, but changes involve more than 50% of the lung section.
Representative samples of these four histologic grades are shown in Fig. 1. All assessments were performed by one observer(D.d.S.), who was unaware of the treatment allocation or any other details of the experimental conditions.
Statistical Analysis
Measurements of lung function and hematologic parameters were summarized for all animals in each of the three treatment groups, using means or medians as appropriate. Unbalanced randomized block analysis(14) was used to test whether BAL plasma recalcification times and lung uptake of circulating 125I-fibrinogen differed between the treatment groups. Histologic scores were compared using Friedman's test(15). The association between histologic scores and125 I-fibrinogen uptake was examined by one-way analysis of variance. Finally, because of our empirical impression that different litters of piglets responded quite differently to the identical lung injury protocol, a two-way analysis of variance of treatments × litters was performed to estimate the contributions of both factors to the total variance in the lung uptake of125 I-fibrinogen.
RESULTS
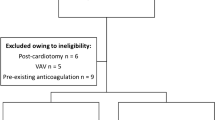
Experimental animals. A total of 69 piglets from 23 litters were studied. However, due to three deaths during the initial surgery and inappropriately high hirudin doses during the first three experiments, 23 piglets made up the untreated control group, but only 22 piglets were available for analysis in the AT III group, and 18 in the hirudin group.
Mean birth weights (SD) were comparable between the control, AT III, and hirudin groups: 1329 g (200), 1297 g (274), and 1297 g (196). Excluding the three animals that died before commencement of the treatment protocol, 4 of 23(17.4%) piglets died before completion of the 24-h study protocol in the control group, 1 of 22 (4.5%) in the AT III group, and 4 of 18 (22.2%) in the hirudin group.
Pulmonary overdistention. Thirty minutes after initiation of the lung injury protocol, mean expiratory tidal volumes were 69 mL/kg in all three treatment groups. After 24 h of continuous ventilation at the same peak airway pressure, mean expiratory tidal volumes were (±SD): control, 63 mL/kg (±12.3); AT III, 67 mL/k (±11.7); and hirudin, 68 mL/kg(±9.9).
Hematologic studies. Hematologic parameters are summarized in Table 1. The median PTT in animals receiving hirudin was prolonged approximately 1.4-fold; however, individual responses to the standardized hirudin dose were quite variable, and several animals in this treatment group bled profusely from the endotracheal tube, thoracotomy sites, and after suprapubic bladder aspirations. No such bleeding was observed in either control piglets or piglets receiving AT III concentrate.
In unsupplemented piglets, plasma AT III activities were initially low and increased slightly over the 24-h study period. AT III levels were raised well above adult porcine reference values in animals given AT III supplements(Table 1). In those four animals that received the high dose regime of AT III concentrate, mean AT III levels at 12 and 24 h were 2.51 and 2.92 U/mL, respectively, without any evidence of clinical bleeding or prolongation of the PTT.
Procoagulant activity of bronchoalveolar lavage fluid. Group means (SD) for BAL plasma recalcification times were 40.8 (7.4) s, 47.7 (7.8) s, and 53.0 (10.0) s, respectively, for untreated (n = 13), AT III-supplemented (n = 13), and hirudin-treated (n = 9) animals. Unbalanced randomized block analysis confirmed that, compared with untreated animals, BAL plasma recalcification times were significantly longer in AT III-supplemented and hirudin-treated litter mates, suggesting that both thrombin inhibitors reduced procoagulant activity in the extravascular lung compartment (p = 0.001; Table 2).
Lung uptake of 125I-fibrinogen. The uptake of i.v. administered 125I-fibrinogen into the right lung tissues was significantly greater in control animals than in littermates who received either AT III concentrate or hirudin (p = 0.003; Table 2). Data in individual pairs of littermates (AT III-control and hirudin-control) are shown in Fig. 2. No uptake of 125I-fibrinogen was detectable in four unventilated healthy newborn piglets 24 h after an i.v. injection of 185 kBq of125 I-fibrinogen.
Lung uptake of 125I-fibrinogen, expressed as counts per 5 min in 1 g of wet lung tissue of right lung/counts per min in 1 mL of whole blood at the end of each experiment. Observations for pairs of individual littermates are shown for the AT III-control contrast in theleft panel, and for the hirudin-control contrast in the right panel. Within each panel, pairs favoring the experimental treatment are shown on the left, whereas pairs favoring the control group are shown on the right.
Lung histology. Table 3 summarizes the distribution of histologic grades by treatment group. Although histologic grades correlated with the lung uptake of 125I-fibrinogen (r= 0.39; p = 0.0018), histologic grades of lung injury did not differ significantly between littermates in the three treatment groups.
Treatment versus litter effects. The variability in the severity of lung injury in control animals suggested that inherent biologic factors strongly influenced the susceptibility to lung injury. We therefore quantitated the relative contributions of treatment code and litter effects(i.e. whether piglets were born to the same mother) to the severity of lung injury. Using lung uptake of 125I-fibrinogen as the study end point, we found that the treatment code explained 16% of the total variance, whereas “litter” explained 22%.
DISCUSSION
Intrapulmonary accumulation of fibrinogen and increased procoagulant activity of BAL fluid are two pathognomonic features of acute lung injury(13, 16). In the present studies we have shown that both events can be ameliorated by i.v. administered thrombin inhibitors. Although the clinical consequences of thrombin generation and fibrin deposition in the lung remain to be elucidated(17), increasing experimental evidence suggests that unopposed thrombin activity and the resulting fibrin formation in the intra- and extravascular lung compartments may exacerbate pulmonary hypertension(18), increase endothelial permeability(19), inactivate surfactant(20), and amplify lung inflammation and fibrosis(21–23). Reducing thrombin and fibrin in the lung may therefore be a desirable therapeutic goal.
So far, however, the available literature on the efficacy of thrombin inhibitors in acute lung injury is contradictory and largely limited to heparin. Malik and Van der Zee(24) showed that heparin reduces lung water and prevents progressive respiratory insufficiency during experimental glass bead embolism in dogs. Other investigators could not demonstrate this beneficial effect of heparin in sheep(25). Heparin pretreatment even had an adverse effect during bone marrow embolism, where the drug was thought to increase lung vascular permeability by increasing lipoprotein lipase activity and generation of FFA(26). On the other hand, low dose heparin abolished the intrapulmonary 125I-fibrinogen deposition associated with experimental pancreatitis in rats(27).
In premature infants, two controlled trials of heparin therapy were published in the presurfactant era(28, 29). Both studies failed to establish a beneficial treatment effect on the primary outcome, i.e. mortality(28, 29). However, the efficacy of heparin in study infants may have been reduced by low levels of the heparin cofactor AT III. Antithrombin deficiency may render the neonate resistant to heparin(30, 31). Alternative choices of antithrombotic agents include purified and pasteurized concentrates of AT III, the most important physiologic inhibitor of thrombin, and hirudin, an AT III-independent and selective inhibitor of thrombin. Both agents have been reported to ameliorate endotoxin-induced lung injury in sheep and pigs, respectively(7, 8). Both agents were similarly effective in the present study in reducing the procoagulant activity of BAL fluid and the uptake of circulating 125I-fibrinogen into the extravascular lung compartment. However, at the dosages used, hirudin caused significant clinical bleeding, whereas AT III concentrate did not, even when it was given in high pharmacologic doses. This may be explained by the different origin and mode of action of the two agents: AT III concentrate enhances the plasma level of an important endogenous thrombin inhibitor, whereas hirudin is an exogenous inhibitor of thrombin which naturally occurs only in the saliva of the medicinal leech. Importantly, clot-bound thrombin, including thrombin trapped in a hemostatic plug, is protected from inhibition by AT III, but is susceptible to inactivation by AT III-independent inhibitors such as hirudin(32). This difference may account, at least in part, for the different safety profile of the two agents in this study.
Pulmonary overdistention was chosen to induce acute lung injury, because baro- or volutrauma with or without air leak syndromes remains a frequent complication of intensive care. Positive pressure ventilation may lead to secondary lung injury in any infant who requires support for respiratory failure, irrespective of the underlying disease process(33). The animal model used in the present study was a modification of methods previously described by Tsuno and et al.(9). These investigators clearly demonstrated that mechanical ventilation at high peak airway pressures and large tidal volumes produces acute lung injury in healthy pigs within 24 to 48 h(9). It is important to note that the excessive tidal volumes which were used throughout the present studies to induce lung injury made it impossible to determine whether the observed reduced potential for fibrin deposition in the extravascular lung compartment is associated with improvements in gas exchange. Future experiments to answer this question will require an additional period of “rescue” ventilation during which pulmonary function can be assessed without distortion from intentional hyperventilation.
After 24 h of ventilation at high peak pressures, 65% of untreated piglets developed moderate to severe lung injury, as assessed by a single pathologist who was unaware of the details of the experimental protocol. Histologic grades correlated significantly with the lung uptake of 125I-fibrinogen, however, in contrast to the intrapulmonary accumulation of fibrinogen, histologic grades did not differ significantly between treatment groups. There are two possible explanations for this observation. It is entirely conceivable that moderate reductions in the lung uptake of 125I-fibrinogen are not reflected in the fairly crude and semiquantitative scores for lung histology, particularly after a relatively short period of mechanical ventilation. Alternatively, a beneficial treatment effect on lung histology may have been missed in the present study, due to lack of statistical power.
Like Tsuno et al. we found that the susceptibility to lung injury varied greatly between animals. In fact, we have shown in this study that a substantial proportion of the variance in outcome could be explained by a“litter” effect. A similarly striking degree of variation between litters was previously reported by Phelps and Rosenbaum(34) in another multiparous species, namely the kitten model of oxygen-induced retinopathy.
In contrast to Tsuno et al. we did not observe extensive vena cava thrombosis in animals receiving no anticoagulant therapy. Consequently, we did not have to resort to Tsuno's strategy of administering heparin to prevent this complication. One possible explanation for this difference may be the age of the experimental animals. The piglets in this study were less than 48 h old, whereas Tsuno et al. used pigs aged 2-3 wk(9). Like the human neonate, newborn piglets have an“immature” coagulation system with prolonged clotting times and low levels for most coagulation factors(35), but unlike the human infant, the porcine hemostatic system matures rapidly during the 1st wk of life(35).
In summary, we have shown that thrombin inhibitors reduce the potential for fibrin deposition during acute lung injury induced by pulmonary overdistention. These encouraging results justify further investigations in chronically ventilated piglets, which are allowed to recover from the acute injury. Until such data on the clinical effects of thrombin inhibitors become available, inferences about the therapeutic potential of antithrombotic agents in acute lung injury would be premature.
Abbreviations
- AT III:
-
antithrombin
- BAL:
-
bronchoalveolar lavage
- PTT:
-
activated partial thromboplastin time
References
Bachofen M, Weibel ER 1977 Alterations of the gas exchange apparatus in adult respiratory insufficiency associated with septicemia. Am Rev Respir Dis 116: 589–615.
Saldeen T 1976 Trends in microvascular research. The micro-embolism syndrome. Microvasc Res 11: 227–259.
Dairaku M, Sueishi K, Tanaka K 1982 Disseminated intra- vascular coagulation in newborn infants. Pathol Res Pract 174: 106–115.
Conover PT, Abramowsky C, Beyer-Patterson P 1990 Immunohistochemical diagnosis of disseminated intravascular coagulation in newborns. Pediatr Pathol 10: 707–716.
Schmidt B, Vegh P, Weitz J, Johnston M, Caco C, Roberts R 1992 Thrombin/Antithrombin III complex formation in the neonatal respiratory distress syndrome. Am Rev Respir Dis 145: 767–770.
Schmidt B 1994 Antithrombin III deficiency in neonatal respiratory distress syndrome. Blood Coagul Fibrinolysis 5: S13–S17.
Redens TB, Leach WJ, Bogdanoff DA, Emerson TE 1988 Synergistic protection from lung damage by combining antithrombin-III andα1-proteinase inhibitor in the E. coli endotoxemic sheep pulmonary dysfunction model. Circ Shock 26: 15–26.
Hoffmann H, Siebeck M, Spannagl M, Weis M, Geiger R, Jochum M, Fritz H 1990 Effect of recombinant hirudin, a specific inhibitor of thrombin on endotoxin-induced intravascular coagulation and acute lung injury in pigs. Am Rev Respir Dis 142: 782–788.
Tsuno K, Miura K, Takeya M, Kolobow T, Morioka T 1991 Histopathologic pulmonary changes from mechanical ventilation at high peak airway pressures. Am Rev Respir Dis 143: 1115–1120.
Johnston M, Zipursky A 1980 Microtechnology for the study of the blood coagulation system in newborn infants. Can J Med Technol 42: 159
O'Brodovich H, Berry L, D'Costa M, Burrows R, Andrew M 1991 Influence of fetal pulmonary epithelium on thrombin activity. Am J Physiol 261: L262–L270.
Ikeno LC, Bowen BM, Der M 1981 Commercial production of125 I-fibrinogen injection. J Radioanal Chem 65: 179–188.
Sitrin RG, Brubaker PG, Fantone JC 1987 Tissue fibrin deposition during acute lung injury in rabbits and its relationship to local expression of procoagulant and fibrinolytic activities. Am Rev Respir Dis 135: 930–936.
Kleinbaum DG, Kupper LL, Muller KE 1988 Applied Regression Analysis and Other Multivariable Methods. PWS-Kent, Boston MA, pp 469–472.
Conover WJ 1971 Practical Nonparametric Statistics. John Wiley & Sons, New York, pp 265–274.
Idell S, Peters J, James KK, Fair DS, Coalson J 1989 Local abnormalities of coagulation and fibrinolytic pathways that promote alveolar fibrin deposition in the lungs of baboons with diffuse alveolar damage. J Clin Invest 84: 181–193.
McDonald JA 1990 The yin and yang of fibrin in the airways. N Engl J Med 322: 929–930.
Seeger W, Neuhof H, Hall J, Roka L 1988 Pulmonary vasoconstrictor response to soluble fibrin in isolated lungs: possible role of thromboxane generation. Circ Res 62: 651–659.
Malik AB, Horgan MJ 1987 Mechanisms of thrombin-induced lung vascular injury and oedema. Am Rev Respir Dis 136: 467–470.
Seeger W, Elssner A, Gunther A, Kramer H, Kalinowski HO 1993 Lung surfactant phospholipids associate with polymerizing fibrin: loss of surface activity. Am J Respir Cell Mol Biol 9: 213–220.
Garcia JGN, Perlman MB, Ferro TJ, Johnson A, Jubiz W, Malik AB 1988 Inflammatory events after fibrin microembolization. Am Rev Respir Dis 137: 630–635.
Kuhn C, Boldt J, King TE, Crouch E, Vartio T, McDonald JA 1989 An immunohistochemical study of architectural remodelling of connective tissue synthesis in pulmonary fibrosis. Am Rev Respir Dis 140: 1693–1703.
Tani K, Yasuoka S, Ogushi F, Asada K, Fujisawa K, Ozaki T, Sano N, Ogura T 1991 Thrombin enhances lung fibroblast proliferation in bleomycin-induced pulmonary fibrosis. Am J Respir Cell Mol Biol 5: 34–40.
Malik AB, Van der Zee H 1977 Time course of pulmonary vascular response to microembolization. J Appl Physiol 43: 51–58.
Binder AS, Nakahara K, Ohkuda K, Kageler W, Staub NC 1979 Effect of heparin or fibrinogen depletion on lung fluid balance in sheep after emboli. J Appl Physiol 47: 213–219.
Burhop KE, Selig WM, Beeler DA, Malik AB 1987 Effect of heparin on increased pulmonary microvascular permeability after bone marrow embolism in awake sheep. Am Rev Respir Dis 136: 134–141.
Berry AR, Davies GC, Millar AM, Taylor TV 1983 Changes in the biophysical properties and ultrastructure of lungs, and intrapulmonary fibrin deposition in experimental acute pancreatitis. Gut 24: 929–934.
Markarian M, Lubchenco LO, Rosenblut E, Fernandez F, Lang D, Jackson JJ, Bannon AE, Lindley A, Githens JH, Martorell R 1971 Hypercoagulability in premature infants with special reference to the respiratory distress syndrome and hemorrhage. II. The effect of heparin. Biol Neonat 17: 98–111.
Gobel U, von Voss H, Jurgens H, Petrich C, Pothmann Rr, Sprock I, Lemburg P 1980 Efficiency of heparin in the treatment of newborn infants with respiratory distress syndrome and disseminated intravascular coagulation. Eur J Pediatr 133: 47–49.
Schmidt B, Buchanan MR, Ofosu F, Brooker L, Hirsh J, Andrew M 1988 Antithrombotic properties of heparin in a neonatal piglet model of thrombin-induced thrombosis. Thromb Haemost 60: 289–292.
Schmidt B, Ofosu FA, Mitchell L, Brooker LA, Andrew M 1989 Anticoagulant effects of heparin in neonatal plasma. Pediatr Res 25: 405–408.
Weitz JI, Hudoba M, Massel D, Maraganore J, Hirsh J 1990 Clot-bound thrombin is protected from inhibition by heparin-antithrombin III but is susceptible to inactivation by antithrombin III independent inhibitors. J Clin Invest 86: 385–391.
O'Brodovich HM, Mellins RB 1985 Bronchopulmonary Dysplasia. Unresolved neonatal acute lung injury. Am Rev Respir Dis 132: 694–709.
Phelps DL, Rosenbaum AL 1977 The role of tocopherol in oxygen-induced retinopathy: kitten model. Pediatrics 59: 998–1005.
Massicotte P, Mitchell L, Andrew M 1986 A comparative study of coagulation systems in newborn animals. Pediatr Res 20: 961–965.
Acknowledgements
The authors gratefully acknowledge M. Andrew, M.D., C. E. Webber, Ph.D., and J. Weitz, M.D., for their valuable advice and help, P. Vegh and L. Berry for their excellent technical support, and R. Roberts, M.Sc. and G. Foster, M.Sc., for their assistance with data management and statistical analysis. We also thank Behringwerke, AG, Marburg, Germany, for a generous gift of antithrombin III concentrate and recombinant hirudin.
Author information
Authors and Affiliations
Additional information
Supported by grants-in-aid from the Heart and Stroke Foundation of Ontario, and the Medical Research Council of Canada. B.S. is a Career Investigator of the Heart and Stroke Foundation of Ontario.
Presented in part at the Annual Meeting of the Society for Pediatric Research in Washington, DC, 1993, and at the Annual Meeting of the American Thoracic Society in Boston, MA, 1994.
Rights and permissions
About this article
Cite this article
Schmidt, B., Davis, P., La Pointe, H. et al. Thrombin Inhibitors Reduce Intrapulmonary Accumulation of Fibrinogen and Procoagulant Activity of Bronchoalveolar Lavage Fluid During Acute Lung Injury Induced by Pulmonary Overdistention in Newborn Piglets. Pediatr Res 39, 798–804 (1996). https://doi.org/10.1203/00006450-199605000-00009
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199605000-00009