Abstract
Brain bilirubin concentrations are increased by hyperosmolality and hypercarbia, but the mechanism is not known. The same applies to the mechanism for preferential localization of bilirubin to basal ganglia. Young Sprague-Dawley rats were used. Groups were: control (n = 15), hypercarbia (n = 16, pH ≅ 6.95), and hyperosmolality(n = 13, serum osmolality ≅390 mosm/L). Hyperbilirubinemia was induced by a 5-min infusion of 50 mg/kg bilirubin, containing ≅20 μCi[3H]bilirubin. Rats were killed at 15-min intervals up to 60 min, and the brains were flushed in situ, dissected into seven regions, weighed, and dissolved. Brain bilirubin was determined by scintillation counting. The half-life of bilirubin in brain was calculated by exponential fitting, which also allowed an estimation of brain bilirubin at the end of the bilirubin bolus. The kinetics of bilirubin clearance from brain were first order. The half-life of bilirubin in brain was significantly prolonged in hyperosmolality (38.2 ± 28.8 min [mean ± SD]) compared with control (16.1 ± 7.7 min) and hypercarbia (12.6 ± 8.6 min)(F = 12.6, p < 0.0001 after log transformation) results. The estimated acute entry of bilirubin into brain was significantly increased in hypercarbia (13.9 ± 7.4 nmol/g) compared with control (5.6± 2.1 nmol/g) and hyperosmolality (6.5 ± 2.1 nmol/g)(F = 19.2, p < 0.0001 after log transformation) results. There were no significant differences between brain regions in acute entry or clearance of bilirubin. The kinetics of increased brain bilirubin differ between hypercarbia (increased acute entry) and hyperosmolality(delayed clearance). Preferential localization of bilirubin to basal ganglia is not produced under, and may not be explained by, the conditions investigated.
Similar content being viewed by others
Main
Unconjugated bilirubin inhibits neuronal function and may affect viability. Scientific data point to several possible mechanisms for these effects, including inhibition of the mitochondrial respiratory chain(1–3), inhibition of enzyme activity(4–9), interference with neurotransmitter metabolism(10–13), effects on cell membrane function and integrity(14–18), and interference with cell regulatory mechanisms and neurotransmitter release through inhibition of protein phosphorylation(7, 19, 20). There is as yet no agreement on which, if any, of these mechanisms is more important in the causation of the clinical syndromes of bilirubin encephalopathy and kernicterus.
In classical kernicterus, most often associated with Rh immunization, babies either died in the acute phase or survived with severe neurologic sequelae(21–25). These included choreoathetosis, nerve deafness, gaze paresis, and occasionally developmental delay(21, 22, 26). In infants who died and were autopsied, yellow staining of the brain was noticed, and this was usually most pronounced in the basal ganglia, giving rise to the German term kernicterus(27).
Several conditions have been shown to increase the concentration of bilirubin in brain. In the presence of an intact blood-brain barrier bilirubin entry into brain probably occurs primarily as the unbound molecule, which is found only in nanomolar concentrations in the serum of jaundiced infants(28, 29). An increased concentration of bilirubin in the brain is found when the bilirubin binding capacity is reduced (neonatal albumin, hypoalbuminemia, displacing agents), when the blood-brain barrier is opened (hyperosmolality, asphyxia, radiation), and when brain blood flow is increased (seeRef. 30 for references). In respiratory acidosis (hypercarbia) bilirubin probably enters the brain mostly as the unbound molecule(29) by a process that appears related to increased brain blood flow(31, 32). In hyperosmolality opening of the blood-brain barrier appears to be associated with entry of both albumin-bound and unbound bilirubin(29). However, previous studies have not addressed the question of whether increased brain bilirubin under different conditions is due to effects on the entry into or on the clearance of bilirubin from brain. The first hypothesis of the present study was that the kinetics of increased brain bilirubin concentration would differ in respiratory acidosis(hypercarbia) and hyperosmolality.
We also know little about why bilirubin in kernicterus is more concentrated in some regions of the brain than in others. Theoretically differences in mechanisms related to uptake or entry on one side, or excretion on the other might explain this localization phenomenon. Specific transport mechanisms and differences in blood-brain barrier permeability(33) and in brain blood flow(31) might be implicated. Locally, binding to certain cellular constituents, e.g. proteins, oxidation of bilirubin(34), or redistribution might explain the localization phenomenon. We must also consider the possibility that bilirubin in kernicterus mainly serves as a marker of other events, the nature of which is still unknown.
We have previously studied rates of bilirubin clearance from brain regions in rats, and found no differences between regions under baseline conditions(35). Similarly, the acute entry of bilirubin did not differ between rat brain regions under such conditions(36). The second hypothesis in the present study was that the presence of hypercarbia or hyperosmolality would cause changes in bilirubin in-out kinetics that might explain the kernicterus localization phenomenon.
METHODS
Young adult, male Sprague-Dawley rats [n = 44, weight 179± 52 g (mean ± SD)] were purchased from Dyrlaege Møllegaards Avlslaboratorium, Ll.Skensved, Denmark. Bilirubin and BSA were from Sigma Chemical Co., St. Louis, MO, and were used without further purification. Other reagents were analytical grade. [3H]Bilirubin was purchased from Amersham Corp., Arlington Heights, IL. A gas mixture consisting of 20% CO2, 20% O2, 60% N2 was from Norgas, Oslo, Norway.
Preparation of reagents. Unlabeled bilirubin was dissolved in 0.1 N NaOH, stabilized with BSA (molar ratio bilirubin: albumin = 14), and diluted with Krebs-Ringer buffer, pH 7.4, to a concentration of 3 mg/mL. The resulting metastable bilirubin solution had a pH of ≅8. Radioactively labeled bilirubin was added in sufficient quantity to give each rat ≅740 KBq (20 μCi) in the bilirubin bolus. Carbamide was dissolved in Krebs-Ringer buffer to a concentration of 8.3 mol/L.
Preparation of the rat model. On the day of the study the rats were anesthetized with a s.c. injection of 0.15 mL of a mixture of Fentanyl(Janssen, Titusville, NJ) (0.05 mg/mL), fluanisone (2.5 mg/mL), and midazolam(1.25 mg/mL). Anesthesia was maintained throughout the study by supplementary injections as needed. A catheter (Jelco i.v. catheter placement unit 24G, Critikon) was placed in a dorsal foot vein, and another catheter was placed in the ventral tail artery by cutdown. The baseline condition was then established by i.v. injection of 75 mmol/kg carbamide (hyperosmolality,n = 13), or by placing the rats in a plexiglass box through which the CO2-containing gas was perfused throughout the duration of the experiment (hypercarbia, n = 16), or by no pretreatment (control,n = 15).
After drawing baseline blood samples, bilirubin was infused in a bolus dose of 50 mg/kg over a period of 5 min. All infusions were carried out under red light conditions, and bilirubin-containing syringes and infusion tubing were wrapped in tin foil to further reduce photo-decomposition of bilirubin. Groups of rats were killed with a bolus dose of sodium pentobarbital 15, 30, 45, and 60 min after the start of the bilirubin infusion. The chest was opened, a catheter placed in the ascending aorta, the descending aorta was clamped, the jugular veins were transected, and the brain flushed in situ with saline until the effluent was completely clear. Although this will not clear the brain vasculature completely, the remaining blood has been shown to contribute <20% to the estimated brain bilirubin values(29, 37). The study was approved through customary institutional review procedures for animal experiments.
Blood sampling and analyses. Blood was drawn from the arterial catheter at 0 and 15 min, and again immediately before sacrifice. Serum bilirubin was measured with a diazo method(38). Serum albumin was measured with the bromcresol purple method(39). Hematocrit was measured using microhematocrit tubes. Blood gases and pH were measured with a blood gas analyzer (Radiometer ABL 30, Copenhagen, Denmark). Serum osmolality was measured with a vapor pressure osmometer (Wescor model 5100C, Wescor, Logan, UT).
Measurement of brain bilirubin concentration. The brains were dissected into the following seven regions: cerebral cortex, hippocampus, striatum, midbrain, hypothalamus, cerebellum, and medulla oblongata, and each region was weighed(40). For the purpose of scintillation counting the cerebral cortex was subdivided into left, right, and frontal cortex. The brain regions were dissolved in 3 mL of Soluene-350(Packard Instrument Co., Meriden, CT) at room temperature for 5-6 d, after which 10 mL of Hionic-Fluor scintillation fluid (Packard Instrument Co.) were added. β-Radiation was counted in a Packard 1500 Tri-Carb scintillation analyzer. Quench correction was achieved using the automated external standard. The counting efficiency was in the range of 30-40%. The disintegrations/min values from the tissue specimens were compared with those from identically treated duplicate 10-μL samples of serum obtained immediately before sacrifice. The concentration of bilirubin in each brain region was calculated based on the specific radioactivity for bilirubin in serum at the time of sacrifice. The concentration of bilirubin in whole brain was found by adding the disintegrations/min for all the regions.
Data handling. Rates of clearance of bilirubin from brain as well as the concentration of bilirubin in brain at 5 min (C5,i.e. at the conclusion of the bilirubin infusion) were estimated for each group and brain region using the program Expofit(41). This program fits values of concentration by least-squares to values of time according to the equation C =C0 e-kT, and calculates the initial concentration, C0, the rate constant, k, and the half-life. The program is an alternative to semilogartihmic plotting and assumes first order kinetics. The data were therefore also plotted using the program SigmaPlot(42) to verify the fit of the curves. The clearance rates and C5 values from the seven brain regions as well as from whole brain in the three groups were compared with analysis of variance using the program InStat(43). Some data were reanalyzed after logarithmic transformation [log10(n + 10)] when Bartlett's test showed significant heterogeneity of variance. However, post-tests were done on the nontransformed data using Welch's t test, which does not assume homogeneity of variance.p < 0.05 was chosen as the level of statistical significance.
RESULTS
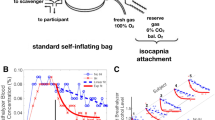
There were significant differences between the groups in the kinetics of bilirubin entry into and clearance from whole brain. Thus, acute entry of bilirubin into brain was significantly increased in hypercarbia, whereas the clearance of bilirubin from brain was significantly delayed in hyperosmolality(Table 1). Therefore, the mechanisms of increased brain bilirubin concentration are different under these conditions. However, as shown in Figure 1, the clearance of bilirubin from brain showed a good fit to first order kinetics in all groups. The goodness of fit was not significantly improved by fitting to second to fourth order kinetics in any of the groups.
Bilirubin half-life in brain. Semilogarithmic plot of bilirubin concentrations in whole brain at 15, 30, 45, and 60 min after the start of a 5-min infusion of bilirubin, 50 mg/kg. ○, Control, lower regression line, first order r2 = 0.90; □, hypercarbia, steeper regression line, first order r2 = 0.86; ▵, Hyperosmolality, upper regression line, first order r2 = 0.66.
There were no differences between rates of clearance from brain regions in any of the groups studied. The half-lives of bilirubin in brain regions are listed in Table 2. The data from the hypercarbia and hyperosmolality groups were logarithmically transformed[log10(n + 10)] before ANOVA to ensure homogeneity of variance. There were also no differences between brain regions in the acute entry of bilirubin in any of the groups. These data are listed inTable 3.
The data from the blood and serum analyses are summarized inTable 4. Some results require additional comments. The barely significant difference in serum bilirubin values at 15 min would appear to be due to higher levels in the hyperosmolar group. The difference could not be verified on posttests, and is unlikely to have influenced the main results. The half-life of bilirubin in serum did not differ between groups, and within groups did not differ significantly from the half-life in brain.
The starting albumin value was significantly lower in the hyperosmolar group than in the two other groups, and within the hyperosmolar group it was significantly lower at start than on the later samples. Similarly, the starting hematocrit was also low in the hyperosmolar group. It is possible that these changes are due to acute hemodilution after the establishment of hyperosmolality. Neither of them are likely to have influenced the main results. The reduction of hematocrit from start to sacrifice in the control and hypercarbia groups are due to sampling-related blood loss.
The degree of hyperosmolality and respiratory acidosis induced in the respective study groups parallels that in previous studies using this model(29, 31, 33, 44, 45). Because these studies have shown that osmolality and pH/Pco2 do not change in the groups not so treated, these parameters were measured only in the relevant group.
DISCUSSION
The data presented here show that increases in brain bilirubin during hyperbilirubinemia may involve different mechanisms. Thus, it is clear that both the entry phase and the clearance phase may be affected. It appears that in hypercarbia an increase in the acute entry of bilirubin into brain may be the main factor responsible for the elevated brain bilirubin relative to controls previously observed in this condition(29, 31, 44). On the other hand, the increase in brain bilirubin which has been shown to occur in hyperosmolality(29, 33, 45), is primarily brought about by a delay in the clearance of bilirubin from brain.
These observations may be important relative to the neurotoxic effects of bilirubin. Delayed clearance of bilirubin from the brain after osmotic opening of the blood-brain barrier would cause the brain to be exposed to higher concentrations of bilirubin for a longer period of time. This would fit with data which suggest that not only the level of bilirubin, but also the duration of exposure is important for toxicity(46). Toxic effects of bilirubin on neuronal function have been documented under experimental conditions not associated with opening of the blood-brain barrier(47–49). However, in other studies opening of the blood-brain barrier has been necessary to produce measurable changes in neuronal function, particularly as it applies to energy metabolism(50, 51). Previous in vitro studies have shown that bilirubin is to a significant extent “detoxified” when bound to albumin(52, 53). Further studies will therefore be needed to clarify whether delayed clearance of bilirubin from brain after opening of the blood-brain barrier is important relative to the neurotoxic effects previously documented(50, 51), and what the relative roles of unbound versus albumin-bound bilirubin are in this context.
Levine et al.(54) studied the half-life of bilirubin in the brains of rats whose blood-brain barriers had been opened by hyperosmolality. The value they found, 1.7 h, was much longer than the≅18.5 min which we found in our previous study of rats with intact blood-brain barriers(35). We speculated then that hyperosmolality might be the most important explanation for the difference in our findings. The present results, which show a significant delay of bilirubin clearance from brain during hyperosmolality, seem to confirm this hypothesis. The brain bilirubin concentrations found in Levine et al.'s(54) study were much higher than those found in studies where more physiologic serum concentrations of bilirubin were produced(29, 31, 33, 44, 45). This might conceivably explain the longer half-time in their study relative to the≅38 min found in the present study. It is not clear why hyperosmolar opening of the blood-brain barrier would delay clearance of bilirubin from brain, but one could speculate that albumin-bound bilirubin might be more tightly bound to brain tissue elements, or that permeability or transport characteristics of the barrier might be affected, e.g. gradual closure of the blood-brain barrier after the initial opening could make it more difficult for albumin-bound bilirubin to cross back into the blood stream.
Rates of bilirubin clearance from brain regions to our knowledge have been studied only once previously(35). The same applies to the acute entry of bilirubin into brain regions(36). Neither in those studies nor in the present is there any evidence of a kernicteric pattern of staining, nor of differences in rates of bilirubin clearance or acute entry that might contribute to such a staining pattern. Although kernicterus occurs in the congenitally jaundiced Gunn rat model, the evidence that kernicterus, sensu strictu, can be produced in the non-Gunn young rat by bilirubin infusion is conflicting. Electrophysiologic evidence suggests, however, that bilirubin encephalopathy can be mimicked, with effects on the auditory brainstem respose and the EEG(47, 50). Long-term behavioral changes can also be induced by bilirubin infusions(55). In a blinded neuropathologic examination of the brains from the latter study we could not distinguish the bilirubin-treated rats from the controls(56). It is possible that bilirubin encephalopathy in this sense occurs in the absence of a kernicteric staining pattern. However, a staining pattern “consistent with regional differences noted in human kernicterus” has been observed after unilateral opening of the blood-brain barrier in rats, making it plausible that kernicterus in this sense can be created in a non-Gunn rat model(57).
In conclusion the present study shows that increased bilirubin content in brain may come about in different ways, and that both the kinetics of entry into and clearance from brain may be affected. Differences in brain regional concentrations of bilirubin could not be explained on the basis of differences in the in-out kinetics of bilirubin in brain. The present findings may have implications for the understanding of bilirubin encephalopathy and kernicterus, as well as for the planning of further studies in the pathogenesis and pathophysiology of bilirubin neurotoxicity.
References
Day RL 1954 Inhibition of brain respiration in vitro by bilirubin: reversal of inhibition by various means. Am J Dis Child 88: 504–506
Zetterstrom R, Ernster L 1956 Bilirubin, an uncoupler of oxidative phosphorylation in isolated mitochondria. Nature 178: 1335–1337
Noir BA, Boveris A, Garaz Pereira AM, Stoppani AOM 1972 Bilirubin: a multisite inhibitor of mitochondrial respiration. FEBS Lett 27: 270–274
Karp WB 1979 Biochemical alterations in neonatal hyperbilirubinemia and bilirubin encephalopathy: a review. Pediatrics 64: 361–368
Kashiwamata S, Asai M, Semba RK 1981 Effect of bilirubin on the Arrhenius plots for Na,K-ATPase activities of young and adult rat cerebra. J Neurochem 36: 826–829
Hackney DD 1980 Photodynamic action of bilirubin on the inner mitochondrial membrane. Implications for the organization of the mitochondrial ATPase. Biochem Biophys Res Commun 94: 875–880
Constantopoulos A, Matsaniotis N 1976 Bilirubin inhibition of protein kinase: its prevention by cyclic AMP. Cytobios 17: 17–20
Sano K, Nakamura H, Matsuo T 1985 Mode of inhibitory action of bilirubin on protein kinase C. Pediatr Res 19: 587–590
McLoughlin DJ, Howell ML 1987 Bilirubin inhibition of enzymes involved in the mitochondrial malate-aspartate shuttle. Biochim Biophys Acta 893: 7–12
Bradbury MWB, Bloom DS, McDowell M 1983 An inhibitor of cerebral uptake of noradrenaline in jaundiced blood plasma. J Cereb Blood Flow Metab 3: 516–520
Wardle EN, Williams R 1980 Depressed uptake of serotonin by platelets in hepatic encephalopathy. Biochem Med 24: 223–227
Brann BSIV, Cashore WJ, Patrick R, Oh W 1985 In vitro effect of bilirubin on dopamine synthesis in adult rat brain synaptosomes. Pediatr Res 19: 335A( abstr)
Cashore WJ, Chung CE 1988 Bilirubin inhibits depolarization-induced dopamine synthesis in synaptosomes. Pediatr Res 23: 403A
Cowger ML 1971 Mechanism of bilirubin toxicity on tissue culture cells: Factors that affect toxicity, reversibility by albumin, and comparison with other respiratory poisons and surfactants. Biochem Med 5: 1–16
Kaul R, Bajpai VK, Shipstone AC, Kaul HK, Murti CRK 1981 Bilirubin-induced erythrocyte membrane cytotoxicity. Exp Mol Pathol 34: 290–298
Deziel MR, Girotti AW 1980 Photodynamic action of bilirubin on liposomes and erythrocyte membranes. J Biol Chem 255: 8192–8198
Mayor F, Diez-Guerra J, Valdivieso F, Mayor F 1986 Effect of bilirubin on the membrane potential of rat brain synaptosomes. J Neurochem 47: 363–369
O'Callaghan A, Duggan PF 1984 Possible biochemical basis for bilirubin neurotoxicity. Biochem Soc Trans 12: 483
Morphis L, Constantopoulos A, Matsaniotis N 1982 Bilirubin-induced modulation of cerebral protein phosphorylation in neonate rabbits in vivo. Science 218: 156–158
Hansen TWR, Bratlid D, Walaas SI 1988 Bilirubin decreases phosphorylation of synapsin I, a synaptic vesicle-associated neuronal phosphoprotein, in intact synaptosomes from rat cerebral cortex. Pediatr Res 23: 219–223
Lande L 1948 Clinical signs and development of survivors of kernicterus due to Rh sensitization. J Pediatr 32: 693–705
Mollison PL, Cutbush M 1954 Haemolytic disease of the newborn. In: Gardner D (ed) Recent Advances in Pediatrics. Churchill Ltd, London, pp 110–132
Beneke R 1907 Ueber den Kernicterus der Neugeborenen. Muench Med Wochenschr 54: 2023–2027
Zuelzer WW, Mudgett RT 1950 Kernicterus. Etiologic study based on analysis of 55 cases. pediatrics 6: 452–474
Zimmerman HM, Yannet H 1933 Kernicterus. Jaundice of the nuclear masses of the brain. Am J Dis Child 45: 740–759
Byers RK, Paine RS, Crothers B 1955 Extrapyramidal cerebral palsy with hearing loss following erythroblastosis. Pediatrics 15: 248–254
Schmorl G 1904 Zur Kenntnis des Ikterus Neonatorum. Verh Dtsch Pathol Ges 6: 109–115
Jacobsen J, Wennberg RP 1974 Determination of unbound bilirubin in the serum of newborns. Clin Chem 20: 783–789
Hansen TWR, Øyasæter S, Stiris T, Bratlid D 1989 Effects of sulfisoxazole, hypercarbia, and hyperosmolality on entry of bilirubin and albumin into young rat brain regions. Biol Neonate 56: 22–30
Hansen TWR, Bratlid D 1986 Bilirubin and brain toxicity. Acta Paediatr Scand 75: 513–522
Burgess GH, Oh W, Bratlid D, Brubakk AM, Cashore WJ, Stonestreet BS 1985 The effects of brain blood flow on brain bilirubin deposition in newborn piglets. Pediatr Res 19: 691–696
Robinson PJ, Rapoport SI 1987 Binding effect of albumin on uptake of bilirubin by brain. Pediatrics 79: 553–558
Burgess GH, Stonestreet BS, Cashore WJ, Oh W 1985 Brain bilirubin deposition and brain blood flow during acute urea-induced hyperosmolality in newborn piglets. Pediatr Res 19: 537–542
Brodersen R, Bartels P 1969 Enzymatic oxidation of bilirubin. Eur J Biochem 10: 468–473
Hansen TWR, Cashore WJ 1995 Rates of bilirubin clearance from rat brain regions. Biol Neonate 68: 135–140
Hansen TWR 1995 Acute entry of bilirubin into rat brain regions. Biol Neonate 67: 203–207
Hansen TWR, Bratlid D 1989 Cerebral blood volumes in young rats without and with in situ flushing of cerebral vasculature. Implications for in vivo studies of brain substance uptake. Biol Neonate 56: 15–21
Martinek RG 1966 Improved micromethod for determination of serum bilirubin. Clin Chim Acta 13: 161–170
Carter P 1969 Microdetermination of serum albumin with bromocresol purple. Enzymol Biol Clin 10: 331–332
Glowinski J, Iversen LL 1966 Regional studies of catecholamines in the rat brain. I. J Neurochem 13: 655–669
Barlow RB 1983 Biodata Handling with Microcomputers. Elsevier Science Publishers, Amsterdam, pp 122–125
Tuerke TM, Farmer CS, Hamilton G, Kerle K, Macy A, Norby J, Rubenstein S, Thompson L, Youtz P, Forood R, Simon S 1991 SigmaPlot Scientific Graphing Software for Windows. Jandel Scientific, San Rafael, CA
Motulsky H, Searle P, Platt M, Pilkinton J 1993 GraphPad InStat Instant Statistics. Graphpad Software, San Diego, CA
Bratlid D, Cashore WJ, Oh W 1984 Effect of acidosis on bilirubin deposition in rat brain. Pediatrics 73: 431–434
Bratlid D, Cashore WJ, Oh W 1983 Effect of serum hyperosmolality on opening of blood-brain barrier for bilirubin in rat brain. Pediatrics 71: 909–912
Nilsen ST, Finne PH, Bergsjø P, Stamnes O 1984 Males with neonatal hyperbilirubinemia examined at 18 years of age. Acta Paediatr Scand 73: 176–180
Karplus M, Lee C, Cashore WJ, Oh W 1988 The effects of brain bilirubin deposition on auditory brain stem evoked responses in rats. Early Hum Dev 16: 185–194
Hansen TWR, Cashore WJ, Oh W 1992 Changes in piglet auditory brainstem response amplitudes without increases in serum or cerebrospinal fluid neuron-specific enolase. Pediatr Res 32: 524–529
Schenker S, McCandless DW, Zollman PE 1966 Studies of cellular toxicity of unconjugated bilirubin in kernicteric brain. J Clin Invest 45: 1213–1220
Wennberg RP, Hance AJ 1986 Experimental bilirubin encephalopathy: importance of total bilirubin, protein binding, and blood-brain barrier. Pediatr Res 20: 789–792
Ives NK, Bolas NM, Gardiner RM 1989 The effects of bilirubin on brain energy metabolism during hyperosmolar opening of the blood-brain barrier: an in vivo study using 31P nuclear magnetic resonance spectroscopy. Pediatr Res 26: 356–361
Cowger ML 1971 Mechanism of bilirubin toxicity on tissue culture cells: Factors that affect toxicity, reversibility by albumin, and comparison with other respiratory poisons and surfactants. Biochem Med 5: 1–16
Bratlid D 1973 Albumin binding and toxicity of bilirubin. Thesis, Universitetsforlaget, Oslo
Levine RL, Fredricks WR, Rapoport SI 1985 Clearance of bilirubin from rat brain after reversible osmotic opening of the blood-brain barrier. Pediatr Res 19: 1040–1043
Hansen TWR, Sagvolden T, Bratlid D 1987 Open-field behavior of rats previously subjected to short-term hyperbilirubinemia with or without blood-brain barrier manipulations. Brain Res 424: 26–36
Hansen TWR, Westre B, Sagvolden T, Bratlid 1988 Lack of neuropathological changes after bilirubin encephalopathy in rats. Pediatr Res 24: 268A( abstr)
Levine RL, Fredericks WR, Rapoport SI 1982 Entry of bilirubin into the brain due to opening of the blood-brain barrier. Pediatrics 69: 255–259
Acknowledgements
The author thanks Siri B. W. Mathiesen and Eva C. Hjeljord for excellent technical assistance.
Author information
Authors and Affiliations
Additional information
Supported by grants from The Norwegian Research Council (grant 100964/310), Ths. Fearnley's Fund, The Medinnova Fund, Alette and Kristian Schreiner's Fund, J. E. Isberg's Fund, and by a donation from Herdis Hollung.
Rights and permissions
About this article
Cite this article
Hansen, T. Bilirubin Entry into and Clearance from Rat Brain during Hypercarbia and Hyperosmolality. Pediatr Res 39, 72–76 (1996). https://doi.org/10.1203/00006450-199601000-00010
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199601000-00010
This article is cited by
-
Bilirubin metabolism: delving into the cellular and molecular mechanisms to predict complications
The Egyptian Journal of Internal Medicine (2024)
-
Molecular events in brain bilirubin toxicity revisited
Pediatric Research (2024)
-
Models of bilirubin neurological damage: lessons learned and new challenges
Pediatric Research (2023)
-
Calculated free bilirubin levels and neurotoxicity
Journal of Perinatology (2009)
-
Bilirubin Brain Toxicity
Journal of Perinatology (2001)