Abstract
Background:
Caregivers of children with asthma provided with a written asthma action plan (WAAP) are reported to be more confident in their ability to provide care for their child during an asthma exacerbation. However, little is known about how a WAAP impacts on their care processes that contributed to this increased confidence.
Aims:
To determine the effects of a WAAP on caregivers' understanding of asthma symptoms, their use of asthma medications for their children, and acute care visits to consult their physicians.
Methods:
A questionnaire survey to caregivers of children with a WAAP (CW) and without a WAAP (CNW) who were followed up at nine public primary care clinics in Singapore. χ2 test was used to determine the differences in outcomes between the CW and CNW groups, followed by logistic regression to adjust for potential covariates.
Results:
A total of 169 caregivers were surveyed (75 CNW, 94 CW). Caregivers in the CW group were more likely to understand bronchoconstriction (adjusted odds ratio (AOR) 4.51, p=0.025), to feel capable (AOR 2.77, p=0.004), safe (AOR 2.63, p=0.004), and had increased confidence (AOR 2.8, p=0.003) to change doses of inhaled medications during an asthma exacerbation. The CW group perceived inhaled asthma medication to be safe (AOR 3.42, p=0.015) and understood the use of controller medication (AOR 3.28, p=0.006). No difference was noted between caregivers in their likelihood to stop medications without consulting their physician, seek acute care consultation, and confidence in self-management of their children's asthma at home.
Conclusions:
The WAAP improved caregivers' understanding of the disease and use of inhaled asthma medications during asthma exacerbations but did not affect their decision regarding acute visits to their physician.
Similar content being viewed by others
Introduction
Asthma is the most common chronic respiratory disease in Singapore.1 Patients, including children with asthma, can be asymptomatic if their asthma is controlled, but may suffer from acute exacerbations (AE) due to episodic bronchoconstriction secondary to airway inflammation. Since exacerbations increase morbidity and can potentially be life-threatening, it is important to educate patients on early symptom recognition so that they can embark on timely use of appropriate inhaled asthma medications and seek prompt medical attention to mitigate the AE. These measures are collated in a set of instructions known as the asthma action plan. An individualised written asthma action plan (WAAP) is a plan tailored to the patient's underlying asthma severity and treatment. A systematic review2 showed that, when adult asthma patients were provided with a WAAP and educated on its use as a form of self-monitoring, together with a review of asthma medications and severity, their health outcomes were significantly improved. Thus, local and international clinical practice guidelines3,4 recommend the provision of a WAAP to patients as part of their education on self-management.
Singapore has a dual public-private fee-for-service healthcare system. Asthma is largely managed in local primary care clinics. Since 2008, a generic template of a WAAP has been made available at the local Health Ministry's website5 for use by physicians or healthcare providers to create asthma action plans for their patients. This template is introduced as part of the local asthma clinical practice guidelines and its design was supported by primary care physicians and pulmonologists in the local public primary and secondary healthcare institutions.
The key components of this WAAP,5 based on the ‘traffic lights’ design, include written information on: (1) how to recognise asthma-related symptoms; (2) how to adjust the treatment (action point) based on physician's prescription; and (3) when and how to seek medical attention in the local setting. It is available in the four main languages to cater for the multi-ethnic population of Singapore. Any healthcare professional can easily download the free electronic template (see Appendix 1, available online at www.thepcrj.org) and configure it to suit the individualised plans of both adult and paediatric asthma patients. Currently, the respiratory disease departments in the various local public healthcare institutions, including the main children's hospitals, have adopted and adapted the template to design their WAAP for use by their adult and paediatric asthma patients. However, it is not a medico-legal requirement and, in the local primary healthcare community, WAAP provision varies between clinical practices. Other than public primary care clinics where there are internal processes to monitor the implementation of the WAAP, there is no audit system to monitor asthma patients who receive a WAAP from their private primary care practitioners. Due to the walk-in fee-for-service healthcare system, patients may also have multiple primary care providers, adding to the difficulties of monitoring its implementation.
For children with asthma, their caregivers are also provided with a WAAP for their reference so that they can manage their children's condition appropriately in their respective social environment. However, unlike the benefits of providing adult asthma patients with a WAAP, evidence showing favourable outcomes of such provision to caregivers is lacking due to the paucity of clinical trials.6 Nonetheless, Ducharme et al.7 showed that children provided with a WAAP in a randomised controlled trial in a paediatric emergency room setting had significantly increased adherence to both inhaled and oral corticosteroids, improved asthma control and increased adherence to medical follow-up. It is not known if the favourable outcomes resulted from the subjects acting independently or whether they were due to their caregivers' supervised care. Whether the study results can be extrapolated to a non-emergency environment within primary care clinics where caregivers' perception may be different is another area of doubt.
In a separate study,8 parents with a WAAP were reported to be more confident in their ability to provide domiciliary asthma care for their children during an exacerbation. Whether this increased parental confidence is related to their understanding of the care processes as stipulated in the WAAP for their children has yet to be explored.
This study aimed to determine the effect of a WAAP on caregivers' recognition of a child's asthma symptoms in the home environment, their views on the use of asthma medications for their children, and the decision to consult a physician.
Methods
This PEACE (Pediatric Asthma Caregiver Empowerment) study consisted of two phases: initial qualitative research to explore the understanding and management of paediatric asthma by the caregivers followed by a questionnaire survey to determine the use of a WAAP for children with asthma aged ≤16 years in the local community. Qualitative data collated from three focus group discussions were analysed and formed the basis of the content and design of a structured questionnaire.
Caregivers were identified as potential subjects when they brought their children with asthma for review at the survey sites at nine public primary care clinics located in the eastern and southern districts of Singapore. These clinics managed 29,983 asthma attendances in 2012, of which 12.5% were asthma consultations by young patients aged <20 years. These patients and their caregivers are routinely educated on the disease and its treatment, including inhaled medications, as part of their standard care.
The child's asthma diagnosis was verified with reference to the disease coding system (ICD-9) of their medical records at the survey sites by the attending physicians. The target participants were screened and only the primary caregivers who looked after the child at least 75% of the awake hours were recruited to the study. The survey was carried out by student nurses from a local nursing school as part of the training curriculum between May and July 2008 and 2010. The survey was interrupted by an outbreak of influenza in the local community in 2009, causing a delay in the completion of the study.
At the survey sites, patients with asthma are routinely directed to ‘health monitoring stations’ within the clinics where their asthma control status is assessed using the Asthma Control Test.9 The student nurses administered the questionnaire to consecutive target caregivers at these stations. They also approached the caregivers in the waiting area prior to their consultation with the physician.
Caregivers provided written consent for study participation and indicated in the questionnaire if they had previously been provided with a WAAP for their children by any physician. The caregivers of some of the children may not be provided with a WAAP as they do not have a regular family doctor or they may consult multiple healthcare providers out of convenience due to the local primary healthcare system. They were subsequently classified into two groups: those with a WAAP (CW) and those with no WAAP (CNW).
Studies using electronic monitoring devices to determine adherence to controller asthma medication have reported adherence rates of 50–77%.10 The investigators hypothesised that 50% of caregivers in the CNW group agreed it was safe to change the doses of inhaled controller asthma medication for a short period of time by themselves and anticipated a 50% improvement in response (i.e. 75% agreed) for the CW group. Based on a 5% level of statistical significance and a power of 85%, the minimum sample size required would be 75 patients per group (150 in total).
The χ2 test was used to compare differences in the understanding of asthma symptoms, use of asthma medications, as well as acute care consultation and self-management between the CW and CNW groups. Logistic regression analysis was further implemented to obtain a measure of the effect of a WAAP on the above outcomes adjusted for the potential confounding effects of age, ethnicity, and number of children with asthma in the family which, to a limited extent, measures the experience of taking care of children with asthma. The effect was quantified using the odds ratio (OR) estimate and its corresponding 95% confidence interval (CI). All statistical analyses were generated using STATA software V.11 (StataCorp, College Station, Texas, USA) assuming a two-sided test at the conventional 5% level of significance.
The study was sponsored by seed funding from SingHealth Polyclinics and Ngee Ann Polytechnic and was approved by the institution review board.
Results
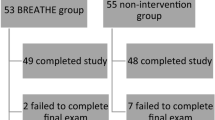
A total of 169 caregivers (75 CNW (44%), 94 CW (56%)) were recruited to the study. The respondents were similar in terms of age distribution and number of children with asthma in the family. More Malay caregivers were given a WAAP while, notably, more Chinese did not receive a WAAP (Table 1).
With regards to the understanding and recognition of symptoms, caregivers in the CW group were more likely to understand airway narrowing during an asthma exacerbation (adjusted odds ratio (AOR) 4.51, 95% CI 1.21 to 16.89, p=0.025) and to differentiate between asthma and an upper respiratory tract viral infection including common cold and flu (AOR 5.71, 95% CI 1.71 to 19.13, p=0.005). No statistical difference was noted in terms of airway mucus production or the recognition of cough and phlegm as part of asthma symptoms.
Tables 2,3,4,5 show that more caregivers in the CW group felt capable (AOR 2.77, 95% CI 1.38 to 5.53, p=0.004), confident (AOR 2.80, 95% CI 1.43 to 5.47, p=0.003), and safe (AOR 2.63, 95% CI 1.35 to 5.12, p=0.004) to change doses of inhaled controller and/or reliever medications during an asthma exacerbation. They perceived inhaled asthma medication to be generally safe (AOR 3.42, 95% CI 1.27 to 9.16, p=0.015) and understood the purpose of using controller medication (AOR 3.28, 95% CI 1.41 to 7.60, p=0.006). However, there was no difference between the two groups in their likelihood to stop inhaled medication without first consulting their physician when the children were well (AOR 0.53, 95% CI 0.27 to 1.03, p=0.061). Likewise, there was no statistical difference in the perceived long-term side-effects of the asthma medications, understanding the duration of action of the reliever medication, and reducing the dose of inhaled asthma medication on their own if their children's asthma was improving.
Table 4 shows that there was no difference in caregivers' preference for self-adjustment of their children's asthma medication (p=0.382) and confidence in self-management of their children's asthma at home (p=0.817). With regard to caregivers’ preference for seeking a consultation with their physician when their child developed asthma symptoms, there was a greater tendency to bring the child to see a physician as soon as he or she developed asthma symptoms in the CW group, although this did not reach statistical significance (86% vs. 75%, p=0.058).
Discussion
Main findings
The results of this study show that a written asthma action plan (WAAP) enhanced caregivers' understanding of the disease and increased their symptom recognition and use of appropriate asthma medications for their children with asthma. Most caregivers were aware of and familiar with asthma-related airway constriction leading to dyspnoea and wheezing. This could be attributed to the inclusion of this information during routine counselling of asthma patients or their caregivers on the disease aetiology. Caregivers provided with a WAAP appeared to have the relevant knowledge to carry out some measures of self-management compared with those without a WAAP.
The findings are significant, since the provision of a WAAP to children with asthma entails unique challenges. The design and content of the WAAP usually caters to adult users, who will largely be the caregivers, as the child's age, maturity and asthma literacy are barriers to its direct use by the child. For young children, the caregivers will inadvertently act as surrogate observers in symptom recognition and initiate measures in their attempt to abort the exacerbation. This, in turn, will be influenced by the caregivers' understanding of the disease, their perception of the safety of the prescribed medications, their help-seeking behaviour, and the social milieu in which the caregiver interacts with the child. These interrelated factors are complex and inevitably affect the caregivers' use of the WAAP.
Strengths and limitations of this study
To understand the complex processes as to how a WAAP can impact on caregivers' management of their children with asthma, a triangulation approach was used in the design, which is the main strength of this study. A qualitative study of the caregivers was carried out, followed by this questionnaire survey. Qualitative data from the first stage were used to construct the questionnaire to enhance its internal validity.
However, a number of limitations could hinder the generalisability of the study results. The absence of information on the caregivers' educational background constituted a potential limitation of the study. In the local setting the WAAP is intended for any patient or child with asthma, regardless of the patient's or caregiver's education or socioeconomic status. The overall literacy rate11 of the Singapore population aged ≥15 years is 95.9%, and 91.7% of the non-student population aged 25–39 years have a secondary or higher qualification. In spite of the high local literacy rate, the investigators recognise that the education status of the caregiver is potentially a confounding factor as caregivers with ‘lower education’ may not be able to optimise the use of the WAAP. Nonetheless, the plan is available in all major languages and provision of the WAAP to children with asthma is supported by trained asthma nurse educators in the public primary care clinics. These nurses work in teams to capitalise on different language proficiencies and use various asthma educational materials to educate patients and their caregivers on the key components and function of the WAAP. The caregiver's socioeconomic status, which is often correlated with their educational status, is another potential confounder in this study. However, the standardised and subsidised fee-for-service at the survey sites ensures equal access to patients and their caregivers of all socioeconomic status. The nine survey sites are located in various geographical districts of Singapore, so variations in the socioeconomic background of the caregivers will be minimal.
The qualitative study showed that some of the children with asthma were prescribed oral bronchodilators, which are not included in the WAAP as the doses do not allow for titration for safety reasons. In addition, these children were prescribed different brands of controller and reliever asthma medications, including combination drugs with both inhaled long-acting β2-agonist and corticosteroid. Thus, the investigators chose the encompassing term ‘inhaled asthma medication’ in the questionnaire, which refers to both inhaled controller and/or reliever medication. The focus was on the awareness and willingness of caregivers to adjust the inhaled form of these medications rather than assessing their ability to distinguish the different types of medications.
Interpretation of findings in relation to previously published work
In this study 56% of caregivers reported that their children had been prescribed a WAAP by their physician. This is higher than the prevalence reported in other studies, which ranges from 5.2% to 31%.12,13 This could be attributed to the case-encountered method of subject recruitment at the survey sites. Randomised sampling of the asthma patient registry would be a more precise method to determine the prevalence of WAAP provision, but this is not possible in the local walk-in healthcare system.
However, there were still knowledge gaps including the lack of ability by caregivers to associate their child's cough, phlegm, and mucus production with asthma-related airway inflammation. Consequently, parents and caregivers often rely on cough medications to relieve their children symptomatically of cough and phlegm.14 The attending physician, asthma nurse educator, or other member of the healthcare team may not have covered this association adequately, but this hypothesis needs further evaluation. The routine use of a composite assessment tool such as the validated Childhood Asthma Control Test9 — which includes a review of asthma control determinants from both the child and the caregiver — could bridge this gap as it enhances caregivers’ global understanding of the disease presentation and medication usage. It was introduced in Singapore in 2008 but has not yet resulted in universal usage.
More caregivers in the CW group were familiar with the action of inhaled controller medication, which may reflect the benefits of asthma education during WAAP prescription. Over 80% of both groups of caregivers were aware of the action of the inhaled reliever medication. Regardless of WAAP, they perceived side-effects with long-term use of inhaled asthma medication. This may explain why caregivers had the tendency to reduce the dose of inhaled medication once their child's asthma control improved. Consistent with this observation, Conn et al.15 showed that parental concern about asthma medication will affect their adherence to prescribed therapy.
In their 2008 systematic review of randomised controlled trials, Zemek et al.6 showed that children assigned to a symptom-based WAAP compared with those based on peak flow monitoring had a lower risk of acute care visits than the control subjects. However, in this cross-sectional study, both groups of caregivers preferred to consult a doctor rather than change the dose of the inhaled medication themselves. The caregivers have access to healthcare services round the clock at selected primary care clinics and all emergency departments of public and private hospitals in various localities over the entire island.16 While a WAAP is intended to empower the caregiver in managing their child's asthma symptoms at home, both groups preferred to seek medical consultation when their child developed asthma symptoms. This dependency on a doctor's consultation is likely to impact on caregivers' practice of self-management of their children's condition. Nonetheless, positive feedback from physicians and healthcare teams to caregivers who have taken appropriate action according to their WAAP may gradually enhance their confidence level in self-management.
Implications for future research, policy and practice
Despite free and easy accessibility to the electronic version of the WAAP by physicians in Singapore, implementation varies in primary care practices for several reasons including physicians’ adverse perception of its benefits, varying competency and confidence in providing a WAAP for young asthma patients, and education of caregivers.17 As a result, some caregivers were not provided with a WAAP. However, this study shows the value of providing a WAAP to caregivers, which includes enhancing their understanding of symptoms and recognition and appropriate use of asthma medications. These outcomes should be shared with local primary healthcare professionals so that they proactively incorporate a WAAP into the routine care of children with asthma and engage their caregivers in using it.
In addition, the impact of a WAAP on acute care visits among local children with asthma should be examined more objectively in a future randomised controlled trial, but its execution may be ethically challenged as a WAAP has been introduced as routine management in the local setting. What will be more illuminating is the advent of an electronic asthma action plan, incorporating the function of remote data transmission to the healthcare provider when activated by the patient or caregiver; this will allow us objectively to determine the effect of asthma action plan usage and clinical outcomes in prospective studies.
Conclusions
A WAAP improved the understanding and utilisation by caregivers of key processes in managing their children's asthma, including symptom recognition and use of asthma medications, but did not affect their decision for acute consultation with a physician. The next step is to determine the association between the frequency and timeliness of WAAP usage by caregivers and their children's clinical outcomes. This is achievable with the advent of an electronic asthma action plan using the rapidly evolving field of mobile phone technology.
References
Epidemiology and Disease Control Division, Ministry of Health. National Health Survey 2010. ISBN 978-981-08-8540-3.
Gibson PG, Powell H, Coughlin J, et al. Self management education and regular practitioner review for adults with asthma (Cochrane review). In: The Cochrane Library, Issue 1. Oxford: Update Software, 2003.
Global Initiative for Asthma (GINA). Global Strategy for Asthma Management and Prevention. 2010. http://www.ginasthma.org/.
Ministry of Health, Singapore. Management of asthma. MOH Clinical Practice Guidelines 1/2008. ISBN 978-981-08-0074-1. http://www.moh.gov.sg/cpg
Ministry of Health, Singapore. Template for Written Asthma Action Plan. Last access to website on 18 April 2013. Management of asthma. http://www.moh.gov.sg/content/dam/moh_web/HPP/Doctors/cpg_medical/current/2008/Written%20Asthma%20Action%20Plan_template.pdf (accessed 9 Apr 2012).
Zemek RL, Bhogal SK, Ducharme FM . Systematic review of randomized controlled trials examining written action plans in children. Arch Pediatr Adolesc Med 2008;162(2):157–63. http://dx.doi.org/10.1001/archpediatrics.2007.34
Ducharme FM, Zemek RL, Chalut D, et al. Written action plan in pediatric emergency room improves asthma prescribing, adherence, and control. Am J Respir Crit Care Med 2011;183(2):195–203. http://dx.doi.org/10.1164/rccm.201001-0115OC
Deis JN, Spiro DM, Jenkins CA, Buckles TL, Arnold DH . Parental knowledge and use of preventive asthma care measures in two pediatric emergency departments. J Asthma 2010;47(5):551–6. http://dx.doi.org/10.3109/02770900903560225
Liu AH, Zeiger R, Sorkness C, Mahr T, et al. Development and cross-sectional validation of the Childhood Asthma Control Test. J Allergy Clin Immunol 2007;119(4):817–25. http://dx.doi.org/10.1016/j.jaci.2006.12.662
Burgess S, Sly P, Devadason S . Adherence with preventive medication in childhood asthma. Pulm Med Volume 2011(2011), Article ID 973849, 6 pages. http://dx.doi.org/10.1155/2011/973849
Census of Population 2010. Advance Census Release. ISBN 978-981-08-6819-2.
Sun YH, Eun BW, Sim SY, et al. Poor adherence and reasons for non-adherence to the asthma guidelines among pediatricians in Korea. Asian Pac J Allergy Immunol 2010;28(2–3):147–54.
Nelson BW, Awad D, Alexander J, Clark N . The continuing problem of asthma in very young children: a community-based participatory research project. J Sch Health 2009;79(5):209–15. http://dx.doi.org/10.1111/j.1746-1561.2009.00400.x
Tan NC, Soo WF, Ngoh ASH . A qualitative study of parental use of written asthma action plan for their children in Singapore. J Asthma Allergy Educators 2011;2:185. http://dx.doi.org/10.1177/2150129711415850
Conn KM, Halterman JS, Lynch K, Cabana MD . The impact of parents' medication beliefs on asthma management. Pediatrics 2007;120:e521–6. http://dx.doi.org/10.1542/peds.2006-3023
Ministry of Health, Singapore. Our healthcare system: healthcare services. http://www.moh.gov.sg/content/moh_web/home/our_healthcare_system.html. (Last access on 18 April 2013).
Tan NC, Tay IH, Ngoh A, Tan M . A qualitative study of factors affecting family physicians' prescription of written asthma action plan in primary care in Singapore. Singapore Med J 2009;50(2):160–4.
Acknowledgements
Handling editor Sundeep Salvi
Statistical review Gopal Netuveli
The investigators are grateful to the sponsors of the study and to Ms Chau Chain Yan and her student nurses from Ngee Ann Polytechnic for their contribution in executing the survey.
Funding The study received a small grant from SingHealth Polyclinics and Ngee Ann Polytechnic (Singapore).
Author information
Authors and Affiliations
Contributions
NCT: principal investigator of PEACE study, involved in conception and design, interpretation of data, writing the abstract and manuscript, and responsible for the final approval of the version to be published. ZJC: responsible for data analysis and interpretation, writing part of the manuscript and formulating the tables. WFS, ASHN: executing the PEACE study and critical review of the manuscript content. BCT: data analysis and interpretation, and critical review of the abstract, manuscript and data presentation.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no conflicts of interest in relation to this article.
Appendix. Template for Written Asthma Action Plan
Appendix. Template for Written Asthma Action Plan

Rights and permissions
About this article
Cite this article
Tan, N., Chen, Z., Soo, W. et al. Effects of a written asthma action plan on caregivers' management of children with asthma: a cross-sectional questionnaire survey. Prim Care Respir J 22, 188–194 (2013). https://doi.org/10.4104/pcrj.2013.00040
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.4104/pcrj.2013.00040
This article is cited by
-
Asthma care based on Chronic Care Model in an aging Asian community
npj Primary Care Respiratory Medicine (2019)
-
Evaluating the impact of an insulin pump discontinuation action plan on patient or caregiver confidence and anxiety
Journal of Diabetes & Metabolic Disorders (2019)
-
The ‘vicious cycle’ of personalised asthma action plan implementation in primary care: a qualitative study of patients and health professionals’ views
BMC Family Practice (2015)