Abstract
Worsening breathless in a patient with severe chronic obstructive pulmonary disease (COPD) is a common diagnostic and management challenge in primary care. A systematic approach to history-taking and examination combined with targeted investigation of pulmonary, cardiovascular, thromboembolic and systemic causes is essential if co-morbidities are to be identified and managed. Distinguishing between heart failure and COPD is a particular challenge as symptoms and signs overlap. In low and middle income countries additional priorities are the detection of infections such as tuberculosis and human immunodeficiency virus (HIV). Clinicians need to be alert to the possibility of atypical presentations (such as pain-free variants of angina) and less common conditions (including chronic thromboembolic pulmonary hypertension) in order not to overlook important potentially treatable conditions.
Similar content being viewed by others
Clinical Scenario
A 52 year old lady consults her family doctor complaining of breathlessness. You can see from her medical record that she has chronic obstructive pulmonary disease (COPD) for which she uses a salbutamol inhaler when needed. Two years ago she had an FEV1 of 45% predicted and a Medical Research Council dyspnoea score of 3. She has smoked since her late teens, but she had attended a well woman clinic several months ago when she requested help with quitting smoking. She had a BMI of 27 at that consultation and a blood pressure of 145/85. Until recently she has not been too troubled by breathlessness. Over the last few months, however, she has noticed that climbing the stairs at work is making her short of breath. Over the weekend she had to abandon a walk with the grandchildren because her breathing was so uncomfortable, and her family persuaded her that she needed to see her doctor.
Respiratory or cardiac?
Congestive Heart Failure (CHF) and chronic obstructive pulmonary disease (COPD) coexist in about 20% of our patients,1,2 linked by a common pathophysiology of low-grade systemic inflammation.3 Two years ago this woman had severe COPD,4 and her severity is likely to be worse now as she has continued to smoke. She may also have developed CHF.
Distinguishing COPD and CHF
Classic historical and investigative findings of CHF may overlap or be altered in a patient with COPD which can make the distinction difficult.5 Symptoms common to both conditions include dyspnoea, cough, exercise intolerance, fatigue, muscle weakness, disturbed sleep, anorexia, low mood, and anxiety.6–8 Differentiating questions for CHF include ankle swelling, chest pain, nocturia, orthopnoea and paroxysmal nocturnal dyspnoea.
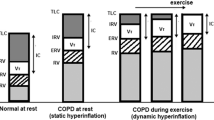
Examination findings for COPD include barrel chest, hyperinflation, and wheezing. Those of heart failure include jugular venous distension, ankle oedema, third and fourth heart sounds and hepatomegaly. These signs, however, can be obscured. Stigmata of right ventricular failure (cor pulmonale), which complicates advanced COPD, can cause jugular venous distension, peripheral oedema, and hepatomegaly. Lung hyperinflation causes hepatic displacement which mimics left heart failure without the presence of cardiomegaly and the auscultation of rales or a third heart sound.
Investigations
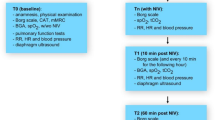
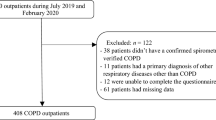
A summary of appropriate investigations is given in Table 1, with the classical results for COPD and CHF. However, our patient already has COPD and this may affect classical appearances: for example, radiological evidence of CHF can be influenced by the hyperinflation of COPD.9–11 Acoustic windows may be impeded by air trapping in pulmonary disease, thus affecting the quality of echocardiographic images. B-type natriuretic peptide (BNP) is substantially elevated in acute heart failure but may also be raised in cor pulmonale, and levels overlap with those in stable CHF (see Figure 1).12 Normal BNP thus excludes CHF, but a raised level does not confirm the diagnosis.
BNP levels in COPD vs CHF (reproduced with permission12)
It is disturbing how few patients are appropriately investigated. Only 31% of patients hospitalised with COPD have had spirometry; this compares with hospitalised CHF patients, 78% of whom in one study had had previous echocardiography.13
Managing the co-morbidities of COPD and CHF
Whether our patient has worsening COPD or has developed CHF, her management will need to include advice and support to help her quit smoking.4,14
Choosing appropriate therapy in a patient with CHF with coexistent COPD is often uncertain; the available evidence derives from randomised clinical trials from which patients with co-morbidity have been excluded,5 or is based on retrospective studies and/or subgroup analysis of single disease trials.15
Pharmacologic management of CHF includes angiotensin-converting enzyme (ACE) inhibitors or angiotensin-II receptor blockers (ARBs) to assist in wall remodelling, diuretics to reduce fluid overload, digoxin for rate-related issues, and β-blockers to improve prognosis and reduce mortality in all patients with systolic dysfunction.16 Pharmacological therapy of COPD includes maximal bronchodilation (including with β2-agonists) and anti-inflammatory treatments to help reduce exacerbations.
a) Cardiovascular drugs in people with COPD
Some interactions are positive: ACE inhibitors and ARBs may also decrease pulmonary inflammation and vascular constriction.17 Others are potentially harmful: intensive diuretic therapy may cause metabolic alkalosis which theoretically could interfere with the respiratory drive of COPD patients, causing hypoventilation with subsequent worsening of hypercapnia, though this is rarely reported at standard doses.18 There is evidence that statins may reduce morbidity and/or mortality in COPD patients.19
β-blocker therapy is recommended,20 but underused,21,22 in patients with coexistent COPD and heart failure for fear of precipitating bronchospasm.23 β-blockers, however, have proved to be safe and generally well tolerated in patients with pulmonary disease.24,25 Cardio-selective β1-blockers26 such as nebivolol, bisoprolol and atenolol27 can be safely used to treat heart failure in patients with respiratory disease,28 potentially even in those with reversible obstruction.25 A pooled relative risk of mortality related to β-blockers in a recent meta-analysis of COPD patients was 0.69 (95% CI 0.62–0.78).29
b) COPD drugs in people with CHF
Inhaled bronchodilators (antimuscarinics and β2-agonists) in COPD patients with concomitant CHF cause some concerns.3 Short-acting β2-agonists (SABAs) increase myocardial oxygen consumption due to tachycardia30 and a few studies have shown an increase in mortality and heart failure exacerbations.31,32 Reassuringly, however, a large study of long-acting β2-agonists (LABAs) in people with COPD did not increase adverse cardiovascular events.33 Further large trials of LABA with and without inhaled steroids are on-going, examining all-cause mortality in patients with moderate COPD and co-morbid cardiovascular disease.34
There continues to be debate that short-acting antimuscarinics (SAMA) may have some cardiovascular toxicity.35 The safety of long-acting antimuscarinics (LAMAs) has been questioned after trials with tiotropium delivered via the Respimat soft mist inhaler showed an increased mortality in the intervention group compared with placebo.36 In contrast, a trial with the dry powder inhaler demonstrated fewer deaths in the tiotropium group.37 A Cochrane review concluded that non-fatal serious adverse events were less frequent with tiotropium than with LABA.38 A recent study comparing tiotropium by Handihaler (dry powder) versus Respimat (fine mist) did not show any difference in cardiovascular outcomes.39
A practical approach to managing our patient
So, how might we approach this woman who presents to our primary care office today?
-
Assess for proper COPD inhaler device technique and adherence, and consider a trial of stepping up treatment.
-
Convince ourselves clinically using the Well's score that DVT or PE is unlikely.40
-
Do a full examination and look for evidence of CHF, albeit this could be difficult to detect.
-
Arrange a chest X-ray (CXR) and an electrocardiogram (ECG)
-
Consider repeating spirometry, but recognise that some obstruction may be related to fluid overload, making it best to do the test when patients are clinically euvolaemic.41
-
Order some blood tests including a full blood count, kidney function, thyroid function and BNP measurement if it is available.
If CHF is possible, begin therapy with some diuretics and most importantly, arrange follow-up. Asking the patient to do daily weights at home to establish their dry weight will assist long term follow-up. If diuresis helps, arrange for an echocardiogram, institute ACE-I or ARB therapy and consider β-blockers and statins. Referral may be necessary for those who do not respond, worsen, have diagnostic issues, or are suspected of cardiac ischaemia.
What else might be the problem?
Other principal causes of chronic breathlessness (i.e. breathlessness occurring over a few months) are shown in Table 2.
History
The aims of accurate history taking are to determine the cause of breathlessness, ascertain the impact of the breathlessness on the patient's life, and understand the patient's views to facilitate future management decisions. In addition to cardiovascular causes, there are a number of other specific conditions to consider:
-
A major cause of mortality in COPD patients is lung cancer.42 “Red flag” symptoms include haemoptysis and/or persistent (i.e. lasting more than 3 weeks) symptoms of cough, chest/shoulder pain, breathlessness, weight loss or hoarseness. A normal CXR does not exclude lung cancer, so if the patient is in a high risk group (i.e. over the age of 40, and a smoker or ex-smoker) they should be referred urgently to a chest physician.43
-
The presence of a persistent cough, with or without haemoptysis, might be a presentation of tuberculosis in a patient residing in or travelling from an area where the disease is endemic.44
-
Community acquired pneumonia tends to present with symptoms developing over days,45 but may be more insidious in the elderly or in opportunistic infection in immunocompromised patients.
-
Haemoptysis may also be a symptom of bronchiectasis. This commonly presents in a non-smoking middle-aged patient with recurrent dyspnoea, cough with purulent sputum, and is often associated with sinusitis.46 In one primary care study, bronchiectasis was found by high resolution CT scanning (HRCT) in 29% patients with COPD.47
-
Whilst weight loss can be a “red flag” symptom, weight gain can also cause an increase in breathlessness. This may be due to oedema (e.g. due to cor pulmonale) or due to obesity (defined as a Body Mass Index (BMI) >30). Obese COPD patients have increased dyspnoea at rest and poorer health status. They also have a reduction in functional residual capacity compared with non-obese subjects.48
-
The term dysfunctional breathing is often used synonymously with “hyperventilation syndrome” where there is over-breathing, but the term may also include irregular patterns of breathing. There is an association with symptoms of light headedness, tingling in the hands, anxiety and a feeling of inability to hold one's breath.
-
Drug therapy may exacerbate breathlessness either by a direct cardiac/pulmonary toxic effect (e.g. amiodarone) or indirectly by increasing cardiac load (e.g. non-steroidal anti-inflammatory drugs, NSAIDs).
Examination
The examination will be directed by the history, but should include a general examination including searching for anaemia, looking for clubbing and lymphadenopathy as well as full pulmonary and cardiovascular examinations.
Investigations
There will be specific investigations as guided by the clinical history (e.g. sputum sample for suspected TB, D-Dimer testing for suspected thromboembolic disease) but in this lady it will be important to check post-bronchodilator spirometry, CXR, and electrocardiogram. Blood tests should include full blood count, thyroid function, C-reactive protein and/or erythrocyte sedimentation rate (ESR). Some primary care centres may have direct access to HRCT scanning if there is suspected bronchiectasis, though the high dose of radiation involved means that a clear indication will be needed.
Referral and subsequent management
Urgent referral will be needed if there is a clinical or radiological suspicion of malignancy, if tuberculosis is suspected, or if there is high suspicion of pulmonary embolism.40 Our patient does not have any reasons for urgent referral, but specialist advice may be still be needed if there is suspicion of interstitial lung disease, concern about cardiac disease, if there is diagnostic doubt, or if a second opinion is requested by the patient.49 Other conditions may warrant discussion with a specialist (e.g. thyrotoxicosis) but can generally be treated in primary care.
Subsequent management will depend on the diagnosis of the co-morbid condition and management of the COPD according to national guidelines.4,49
What might be the problem from the perspective of a resource limited setting?
COPD is rarely diagnosed in resource-limited primary care settings, where the acronym ‘COPD’ is hardly known by the people. Few health workers have the knowledge and capacity to diagnose COPD and manage it. Patients who present with respiratory problems in primary care facilities are usually assessed for tuberculosis or other infectious problems, and if found negative are referred to as “TB negative”; little more is then done for these patients until the condition is advanced.
Despite this, COPD is emerging as a major public health problem in low and middle income countries (LMIC). A study in urban areas of South Africa found a prevalence of 22.2% in males and 16.7% in females,50,51 and in Rwanda it was 9.6%.52 A recent study in rural Uganda found a prevalence of 16.2% affecting mainly young people in their thirties.53
At secondary and tertiary healthcare facilities a cardiac problem is usually the first diagnosis considered in patients with breathlessness. Because COPD may co-exist with cardiovascular disease, this may delay assessment of COPD until patients cardiovascular management shows little improvement.
However, the history presented in this case scenario of a prior diagnosis of COPD in a current smoker with worsening breathlessness over a couple of months and recent increase in symptoms may suggest COPD exacerbation, COPD progression, or a co-morbid condition — especially the commonly encountered infectious pulmonary diseases such as tuberculosis and pneumonia. Each diagnostic possibility should be tested using information from history, physical examination and tests, though the limited range of tests available in resource limited settings increases the reliance on a thorough history and physical examination.
Is it an exacerbation of COPD?
A COPD exacerbation is defined as “an acute event characterised by a worsening of the patient's respiratory symptoms that is beyond normal day-to-day variation and leads to change in medications”.4 The worsening symptoms are usually cough, sputum production and breathlessness.4
The initial focus should be on whether the patient is the right ‘host’ for a COPD exacerbation. Consider risk factors such as advancing age, productive cough, and longer duration since COPD diagnosis and history of exacerbations in the previous year.54–56 Past medical history can help identify pre-existing comorbidities (chronic heart failure, ischaemic heart disease and diabetes mellitus) known to increase the risk of COPD exacerbation.57 It has been shown in longitudinal follow-up studies that the most significant predictor of a future COPD exacerbation is the number of exacerbations in the previous year.56 However, in LMICs these may not have been recognised as such. Therefore any hospitalisation with respiratory illness may be considered as a surrogate of COPD exacerbation.
The next issue to consider is identification of a precipitating factor for exacerbation. Usual precipitants are respiratory infection and environmental pollution.58–60 In LMICs common pollutants include dust, car fumes, biomass smoke exposure, and fumes from paraffin lamps used for lighting.
Is it progression of COPD?
COPD disease progression could also be responsible for the worsening symptoms over the past few months. It is important to check whether our patient has quit smoking: COPD is generally a progressive disease and progression is worse with continued exposure to tobacco or biomass fuels.
Is it a co-morbid condition?
Differential diagnoses such as ischaemic heart disease, heart failure, lung cancer, pulmonary embolism and pulmonary artery hypertension should be considered although these tend to be less common in LMIC.61,62 On the other hand tuberculosis, pneumonia and HIV-associated pulmonary infections especially Pneumocystis jirovecii pneumonia (PJP) are commonly seen.63
An electrocardiogram, echocardiogram and other tests can be done depending on the clinical findings, and level of care. Generally these are not available in primary care facilities in resource-poor settings and patients will need to be referred. However, healthcare workers should always bear in mind that not all patients can reach their referral facilities because of the cost of transport among other reasons. This emphasises the need for good clinical skills locally to be able to offer care to these patients.
Management challenges in a resource limited setting
Management of COPD presents challenges in resource-limited settings because of limited availability of tests to assess severity and drugs. Clinical assessment consisting of pulse rate, blood pressure, respiratory rate, listening to the chest, level of consciousness and orientation may be all that is available to guide immediate treatment.
Arterial blood gases are not readily available, though in some facilities oximetry can be done. Therefore, judgment of oxygen need and severity of airflow obstruction should be based on ability to speak in full sentences, use of accessory muscles of respiration, respiratory rate, and extent of wheezes on chest auscultation.
Internationally recommended treatment for COPD exacerbations — such as oxygen therapy, short-acting bronchodilators, antibiotics and systemic corticosteroids4 — may be available at secondary and tertiary health care facilities, but are not readily available at lower level health facilities.
The commonly available bronchodilator in LMIC is salbutamol. Nebulisation is not usually available, so frequent use of a metered dose inhaler is an alternative, though the latter requires a spacer which is not usually available. The route of administration of bronchodilators is usually an issue in LMIC. Firstly, the inhaled short-acting β2-agonists (SABAs) are not readily available because of cost. In one report it was found that the cost of asthma medicines was higher than that of a nurse's monthly salary in resource limited settings.64 Where no other option is available, oral salbutamol can be used. Theophylline drugs, such as aminophylline, are no longer recommended for management of acute exacerbations of COPD, but they may be the only drug available in some facilities.64 These may be used as a temporary measure whilst urgent referral is made subject to the constraints of distance and transport.
The choice of antibiotics is usually amoxicillin, trimethoprim-sulfamethixazole (Septrin), doxycycline, macrolides, cephalosporin and respiratory quinolones.65 Septrin has been used widely as a prophylaxis drug in HIV, so it tends not to be used regularly. Quinolones are active against mycobacteria, but with the high prevalence of tuberculosis in these settings quinolones tend not to be used. Therefore, amoxicillin and doxycycline are the common choices. Influenza and pneumococcal vaccinations recommended by international guidelines are not routinely used because of cost and lack of local guidelines.
A secondary care approach to dyspnoea
Although it is tempting to attribute the patient's symptoms of worsening dyspnoea to her known COPD, it is imperative to conduct a thorough and meticulous history and physical examination to exclude other possible causes of the patient's symptoms. With a careful history and examination, it is usually possible to generate a focussed differential diagnosis and to confirm the most likely diagnosis with a small number of appropriately selected investigations. The initial danger in this case would be to assume the patient's symptoms are entirely attributable to her COPD before such an assessment has been completed.
Clinical history
COPD is a progressive condition that normally leads to a predictable worsening of dyspnoea with age and time (between exacerbations). Therefore, any sub-acute worsening of dyspnoea that is out of keeping of the slowly progressive pattern of COPD would be concerning for other pathologies, especially cardiac, pulmonary or systemic disorders:
-
Systemic conditions such as thyroid disease and anaemia should have been excluded in primary care.
-
Cardiac disease might be suggested by an exertional component to the dyspnoea (often without chest pain, the so-called “angina variant”) or a past medical history of known heart disease, but additional cardiac risk factors should be sought (hypertension, diabetes, family history etc). Paroxysmal nocturnal dyspnoea and orthopnoea might point to cardiac failure; it is important to consider that ankle swelling is not specific for left heart failure and does not exclude right heart failure secondary to COPD. Palpitations are not specific for left heart disease and might point to atrial arrhythmias, a well-recognised complication of COPD independent of atrial distension, pulmonary hypertension or lung function.66 Higher p wave dispersion (the difference between maximum and minimum p wave duration measurable on an ECG) suggests increased atrial stress as a precursor to atrial arrhythmias.
-
The widest differential is in additional pulmonary disorders. Copious sputum production and recurrent infections (with/without haemoptysis) might suggest bronchiectasis complicating the COPD, persistent low-grade infective systemic and pulmonary symptoms might suggest a non-tuberculous mycobacterial infection. A viral prodrome with predominant wheeze might suggest bronchiolitis. A more subacute than insidious progression of dyspnoea might suggest pulmonary emboli (especially if there are additional risk factors of recent immobility (including long-haul travel), previous embolic disease, family history of thrombo-embolism or known malignancy or parenchymal lung disease, but a small pneumothorax is also possible. Pleurisy or pleural symptoms might suggest pleural disease as a consequence of either pleural infection or malignancy. The latter may also be suggested by ‘red flag’ symptoms such as haemoptysis, weight loss and lethargy. Ankle swelling with presyncope and progressive dyspnoea without infective symptoms should prompt consideration of secondary pulmonary hypertension. Finally, an elevated Nijmegen Score67 or Epworth Score68 might point to hyperventilation or obstructive sleep apnoea, respectively.
A careful focused history should allow generation of a narrowed down list of differential diagnoses to account for the patient's deterioration, and this will include progression of their known COPD as the final explanation.
Clinical examination
Clinical examination should ideally confirm or narrow down the differential diagnosis suggested by the history. Signs of thyroid disease and anaemia are readily apparent if looked for.
Cardiac disease might be suggested by the presence of atrial fibrillation, a displaced apex, valvular disease and signs of left heart failure including a gallop rhythm, a third heart sound and bilateral crackles, with features of right heart failure co-existent in severe cases.
Additional pulmonary disease beyond COPD is more challenging to detect. An elevated BMI and narrow oropharynx might suggest obstructive sleep apnoea. Finger clubbing might suggest malignancy (look for supraclavicular adenopathy and cachexia), bronchiectasis or fibrosis, crackles might point to either bronchiectasis (if coarse) or fibrosis (if fine and end-inspiratory). Wheeze might suggest occult malignancy (if monophonic, predominantly inspiratory or stridulous) or bronchiolitis (if associated with ‘squawks’). Stony dullness to percussion or a pleural rub points to pleural disease. A loud pulmonary component and exaggerated splitting of the second heart sound (P2) plus isolated signs of right heart failure (elevated jugular venous pressure, tricuspid regurgitation, a right ventricular gallop, hepatomegaly and ankle oedema) suggest secondary pulmonary hypertension. Tracheal deviation is concerning for either malignancy or pneumothorax.
Investigations
Investigations should ideally confirm the diagnosis suggested by the history and examination and are dictated by the findings.
-
For systemic disease, thyroid function and full blood count may be confirmatory.
-
For cardiac disease an ECG and echocardiogram are usually indicated, the latter clarifying (if the ECG is non-diagnostic) any pulmonary hypertension (a dilated left atrium in the setting of pulmonary hypertension points to left heart disease, a normal left atrium suggests the pulmonary hypertension is secondary to the COPD). If an angina variant is possible, either an exercise test (often not possible in COPD) or myocardial perfusion scan might be done to look for reversible ischemia that might warrant revascularisation. The ECG may also show p wave depolarisation.69
-
For lung disease, exercise oximetry can be very helpful (significant lung disease typically leads to desaturation). A CXR helps to confirm heart failure, pleural disease (effusion or pneumothorax), malignancy, lung infection and fibrosis, and might suggest pulmonary hypertension (enlarged interlobar pulmonary arteries with oligaemia70) or more severe bronchiectasis. Milder cases of bronchiectasis or pulmonary hypertension would require HRCT (helpful for bronchiolitis too) and echocardiography respectively. True bronchiectasis can only be diagnosed on the HRCT when the patient is clinically stable: infection can cause a false positive “pseudobronchiectasis” due to airway traction.71 Pulmonary emboli usually require a CT pulmonary angiogram as a VQ scan will be indeterminate in our patient due to ventilation defects from the COPD.70 Spirometry might be used to exclude restrictive causes and prompt the need for full lung function tests (pulmonary vascular disease and interstitial lung disease both reduce gas transfer: the latter also reduces total lung capacity and residual volume. Overnight oximetry might be used to confirm sleep apnoea and a hyperventilation provocation test for hyperventilation. A diagnosis of hyperventilation should never be made before excluding significant pulmonary vascular disease.
Chronic thromboembolic pulmonary hypertension
An increasingly common scenario is patients with a history of pulmonary embolism who remain breathless despite six months anticoagulation, or who present to their general practitioner having finished their anticoagulation (typically 12–24 months after the initial clot) breathless again. After excluding recurrent embolism, these patients require referral for active consideration of chronic thromboembolic pulmonary hypertension (CTEPH).
CTEPH is the only definitively treatable cause of pulmonary hypertension.70,72 It occurs in approximately 4% of patients in a 2-year period following an acute pulmonary embolus and 10% of those with recurrent pulmonary emboli. Risk factors include a previous pulmonary embolism (especially if idiopathic and large), young age, a large perfusion defect and a high clot burden.72,73
Clinical suspicion is key, since gas transfer and the echo may not show typical abnormalities in early disease. CT pulmonary angiography may show signs of pulmonary hypertension, chronic thrombus and residual webs but no acute embolism.70 Unexplained presyncope with breathlessness and signs of a right ventricular strain and right heart failure would be concerning for significant pulmonary hypertension.
Without surgical treatment (pulmonary endarterectomy), CTEPH has a poor prognosis with an 80% 2-year mortality (if mean pulmonary artery pressure is greater than 50mmHg). Even 5-year mortality is 65% with lower pressures of 30mmHg. With surgery, 3-year mortality decreases to 6% or less,74,75 once the perioperative period is survived (perioperative mortality only 5%76).
References
Rutten FH, Cramer MJ, Grobbee DE, et al. Unrecognised heart failure in elderly patients with stable chronic obstructive pulmonary disease. Eur Heart J 2005;26:1887–94. http://dx.doi.org/10.1093/eurheartj/ehi291
McCullough PA, Hollander JE, Nowak RM, et al. Uncovering heart failure in patients with a history of pulmonary disease: rationale for the early use of B-type natriuretic peptide in the emergency department. Acad Emerg Med 2003;10:198–204. http://dx.doi.org/10.1111/j.1553-2712.2003.tb01990.x
Hawkins NM, Petrie MC, Macdonald MR, et al. Heart failure and chronic obstructive pulmonary disease the quandary of beta-blockers and beta-agonists. J Am Coll Cardiol 2011;57:2127–38. http://dx.doi.org/10.1016/j.jacc.2011.02.020
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management and Prevention of COPD. Updated 2013. Available from http://www.goldcopd.org Accessed September 4, 2013
Hawkins N, Petrie M, Jhund P, Chalmers G, Dunn F, McMurray J . Heart failure and chronic obstructive pulmonary disease: diagnostic pitfalls and epidemiology. Eur J Heart Failure 2009;11:130–9. http://dx.doi.org/10.1093/eurjhf/hfn013
Janssen DJ, Spruit MA, Uszko-Lencer NH, Schols JM, Wouters EF . Symptoms, comorbidities, and health care in advanced chronic obstructive pulmonary disease or chronic heart failure. J Palliat Med 2011;14:735–43. http://dx.doi.org/10.1089/jpm.2010.0479
Walke LM, Byers AL, Tinetti ME, Dubin JA, McCorkle R, Fried TR . Range and severity of symptoms over time among older adults with chronic obstructive pulmonary disease and heart failure. Arch Intern Med 2007;167:2503–08. http://dx.doi.org/10.1001/archinte.167.22.2503
Caroci AS, Lareau SC . Descriptors of dyspnea by patients with chronic obstructive pulmonary disease versus congestive heart failure. Heart Lung 2004;33:102–10. http://dx.doi.org/10.1016/j.hrtlng.2003.11.004
Milne EN, Bass H . Roentgenologic and functional analysis of combined chronic obstructive pulmonary disease and congestive cardiac failure. Invest Radiol 1969;4:129–47. http://dx.doi.org/10.1097/00004424-196905000-00001
Hublitz UF, Shapiro JH . Atypical pulmonary patterns of congestive failure in chronic lung disease. The influence of pre-existing disease on the appearance and distribution of pulmonary edema. Radiology 1969;93:995–1006
Rutten FH, Moons KG, Cramer MJ, et al. Recognising heart failure in elderly patients with stable chronic heart failure and chronic obstructive pulmonary disease in primary care: cross sectional diagnostic study. BMJ 2005;331:1379. http://dx.doi.org/10.1136/bmj.38664.661181.55
Hawkins NM, Virani S, Ceconi C . Heart failure and chronic obstructive pulmonary disease: the challenges facing physicians and health services. Eur Heart J 2013; http://dx.doi.org/10.1093/eurheartj/eht192 (e-pub ahead of print)
Damarla M, Celli B, Mullerova H, Pinto-Plata V . Discrepancy in the Use of Confirmatory Tests in Patients Hospitalized With the Diagnosis of Chronic Obstructive Pulmonary Disease or Congestive Heart Failure. Respir Care 2006;51:1120–24
van Schayck OCP, Pinnock H, Ostrem A, Litt J for the IPCRG. IPCRG Consensus statement: Tackling the smoking epidemic -practical guidance for primary care. Prim Care Respir J 2008;17:185–93. http://dx.doi.org/10.3132/pcrj.2008.00060
Villar Alvarez F, Méndez Bailón M, de Miguel Díez J . Chronic obstructive pulmonary disease and heart failure. Arch Bronconeumol 2009;45:387–93. http://dx.doi.org/10.1016/S1579-2129(09)72937-4
Dickstein K, Cohen-Solal A, Filippatos G, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008. Eur Heart J 2008;29:2388–42. http://dx.doi.org/10.1093/eurheartj/ehn309
Forth R, Montgomery H . ACE in COPD: a therapeutic target? Thorax 2003;58: 556–8. http://dx.doi.org/10.1136/thorax.58.7.556
Rutten FH, Cramer MJ, Lammers JW, et al. Heart failure and chronic obstructive pulmonary disease: an ignored combination? Eur J Heart Fail 2006;8:706–11. http://dx.doi.org/10.1016/j.ejheart.2006.01.010
Dobler C, Wong K, Marks G . Associations between statins and COPD: a systematic review. BMC Pulmonary Medicine 2009;9:32. http://dx.doi.org/10.1186/1471-2466-9-32
The Heart Failure Society of America. Executive summary: HFSA 2006 comprehensive heart failure practice guideline. J Card Fail 2006;12:10–38. http://dx.doi.org/10.1016/j.cardfail.2005.12.001
Groote P, Isnard R, Assyag P, et al. Is the gap between guidelines and clinical practice in heart failure treatment being filled? Insights from the IMPACT RECO survey. Eur J Heart Fail 2007;9:1205–11. http://dx.doi.org/10.1016/j.ejheart.2007.09.008
Groote P, Isnard R, Clerson P, et al. Improvement in the management of chronic heart failure since the publication of the updated guidelines of the European Society of Cardiology. The Impact-Reco Programme. Eur J Heart Fail 2009;11:85–91. http://dx.doi.org/10.1093/eurjhf/hfn005
Komajda M, Follath F, Swedberg K, et al, The Study Group of Diagnosis of the Working Group on Heart Failure of the European Society of Cardiology. The EuroHeart Failure Survey programme: a survey on the quality of care among patients with heart failure in Europe. Part 2: treatment. Eur Heart J 2003;24:464–74. http://dx.doi.org/10.1016/S0195-668X(02)00700-5
Ashrafian H, Violaris AG . Beta-blocker therapy of cardiovascular diseases in patients with bronchial asthma or COPD: the pro viewpoint. Prim Care Respir J 2005;14:236–41. http://dx.doi.org/10.1016/j.pcrj.2005.06.005
Salpeter SR, Ormiston TM, Salpeter EE, et al. Cardioselective beta-blockers for chronic obstructive pulmonary disease: a meta-analysis. Respir Med 2003;97:1094–101. http://dx.doi.org/10.1016/S0954-6111(03)00168-9
van der Woude HJ, Zaagsma J, Postma DS, et al. Detrimental effects of beta-blockers in COPD: a concern for non-selective beta-blockers. Chest 2005;127:818–24. http://dx.doi.org/10.1378/chest.127.3.818
Nuttall SL, Routledge HC, Kendall MJ . A comparison of the beta1-selectivity of three beta1-selective beta-blockers. J Clin Pharm Ther 2003;28:179–86. http://dx.doi.org/10.1046/j.1365-2710.2003.00477.x
Sirak TE, Jelic S, Le Jemtel TH . Therapeutic update: non-selective beta- and alpha-adrenergic blockade in patients with coexistent chronic obstructive pulmonary disease and chronic heart failure. J Am Coll Cardiol 2004;44:497–502. http://dx.doi.org/10.1016/j.jacc.2004.03.063
Etminan M, Jafari S, Carleton B, Fitzgerald JM . Beta-blocker use and COPD mortality: a systematic review and meta-analysis. BMC Pulm Med 2012;12:48. http://dx.doi.org/10.1186/1471-2466-12-48
Salpeter SR, Ormiston TM, Salpeter EE . Cardiovascular effects of beta-agonists in patients with asthma and COPD: a meta-analysis. Chest 2004;125:2309–21. http://dx.doi.org/10.1378/chest.125.6.2309
Au DH, Udris EM, Fan VS, et al. Risk of mortality and heart failure exacerbations associated with inhaled beta-adrenoceptor agonists among patients with known left ventricular systolic dysfunction. Chest 2003;123:1964–9. http://dx.doi.org/10.1378/chest.123.6.1964
Hirono O, Kubota I, Minamihaba O, et al. Left ventricular diastolic dysfunction in patients with bronchial asthma with long-term oral beta2-adrenoreceptor agonists. Am Heart J 2001;142:E11. http://dx.doi.org/10.1067/mhj.2001.118117
Calverley PM, Anderson JA, Celli B, et al, TORCH investigators. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med 2007;356:775–89. http://dx.doi.org/10.1056/NEJMoa063070
Vestbo J, Anderson J, Brook RD, et al. The study to understand mortality and morbidity in COPD (summit) study protocol. Eur Respir J 2013;41:1017–22. http://dx.doi.org/10.1183/09031936.00087312
Ogale SS, Lee TA, Au DH, Boudreau DM, Sullivan SD . Cardiovascular events associated with ipratropium bromide in COPD. Chest 2010;137:13–19. http://dx.doi.org/10.1378/chest.08-2367
Karner C, Chong J, Poole P . Tiotropium versus placebo for chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2012, Issue 7. Art. No.: CD009285. http://dx.doi.org/10.1002/14651858.CD009285.pub2
Tashkin DP, Celli B, Senn S, et al. A 4-year trial of tiotropium in chronic obstructive pulmonary disease N Engl J Med 2008;359:1543–54. http://dx.doi.org/10.1056/NEJMoa0805800
Chong J, Karner C, Poole P . Tiotropium versus long-acting beta-agonists for stable chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD009157. http://dx.doi.org/10.1002/14651858.CD009157.pub2
Wise R, Anzueto A, Cotton D, et al. Tiotropium Respimat Inhaler and the Risk of Death in COPD. N Engl J Med 2013;369:1491–501. http://dx.doi.org/10.1056/NEJMoa1303342
National Institute for Health and Clinical Excellence. Venous thromboembolic diseases: the management of venous thromboembolic diseases and the role of thrombophilia testing NICE Guideline CG144. NICE 2012 Available from http://guidance.nice.org.uk (Accessed September 2013)
Pison C, Malo JL, Rouleau JL, Chalaoui J, Ghezzo H, Malo J . Bronchial hyperresponsiveness to inhaled methacholine in subjects with chronic left heart failure at a time of exacerbation and after increasing diuretic therapy. Chest 1989;96:230–5. http://dx.doi.org/10.1378/chest.96.2.230
Sin DD, Anthonisen NR, Soriano JB, Agusti AG . Mortality in COPD: Role of comorbidities. Eur Respir J 2006;28:1245–57. http://dx.doi.org/10.1183/09031936.00133805
National Institute for Health and Clinical Excellence. Diagnosis and treatment of Lung cancer. NICE Guideline 121 NICE 2011 Available from http://guidance.nice.org.uk (Accessed September 2013)
National Institute for Health and Clinical Excellence. Tuberculosis: Clinical diagnosis and management of tuberculosis, and measures for its prevention and control. Nice Guideline CG117 NICE 2011. Available from http://publications.nice.org.uk (Accessed September 2013)
Lim WS, Baudouin SV, George RC . British Thoracic Society Guideline for the management of community acquired pneumonia in adults. Thorax 2009;64 Suppl3:iii1–iii55. http://dx.doi.org/10.1136/thx.2009.121434
Pasteur MC, Bilton D, Hill AT on behalf of the British Thoracic Society Bronchiectasis (non-CF) Guideline Group. Guideline for non-CF Bronchiectasis. Thorax 2010;65 Suppl1:i1–i58
O'Brien C . Guest PJ, Hill SL, Stockley RA . Physiological and radiological characterisation of patients diagnosed with chronic obstructive pulmonary disease in primary care. Thorax 2000;55:635–42. http://dx.doi.org/10.1136/thorax.55.8.635
Franssen F . Obesity. Airflow limitation and respiratory symptoms: does it take three to tango? Prim Care Respir J 2012;21:131–33. http://dx.doi.org/10.4104/pcrj.2012.00040
National Institute for Health and Clinical Excellence. Chronic obstructive pulmonary disease: Management of chronic obstructive pulmonary disease in adults in primary and secondary care (partial update) NICE Guideline G101. NICE 2010 Available from http://guidance.nice.org.uk (Accessed September 2013)
Buist AS, McBurnie MA, Vollmer WM, et al. International variation in the prevalence of COPD (the BOLD Study): a population-based prevalence study. Lancet 2007;370:741–50. http://dx.doi.org/10.1016/S0140-6736(07)61377-4
Buist AS, Vollmer WM, McBurnie MA . Worldwide burden of COPD in high- and low-income countries. Part I. The burden of obstructive lung disease (BOLD) initiative. Int J Tuberc Lung Dis 2008;12:703–08.
Musafiri S, van Meerbeeck J, Musango L, et al. Prevalence of atopy, asthma and COPD in an urban and a rural area of an African country. Respir Med 2011;105:1596–605. http://dx.doi.org/10.1016/j.rmed.2011.06.013
van Gemert F, Kirenga B, Chavannes N, et al. Prevalence of COPD and its risk factors in a rural area of Uganda. Abstract no 1012, European Respiratory Society conference, Barcelona 2013
Burgel PR, Nesme-Meyer P, Chanez P et al, Cough and sputum production are associated with frequent exacerbations and hospitalizations in COPD subjects. Chest 2009;135:975–82. http://dx.doi.org/10.1378/chest.08-2062
Niewoehner DE, Lokhnygina Y, Rice K et al, Risk indexes for exacerbations and hospitalizations due to COPD. Chest 2007;131:20–8. http://dx.doi.org/10.1378/chest.06-1316
Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med 2010;363:1128–38. http://dx.doi.org/10.1056/NEJMoa0909883
Miravitlles M, Guerrero T, Mayordomo C, Sánchez-Agudo L, Nicolau F, Segú JL . Factors associated with increased risk of exacerbation and hospital admission in a cohort of ambulatory COPD patients: a multiple logistic regression analysis. Respiration 2000;67:495–501. http://dx.doi.org/10.1159/000067462
Domenech A ., Puig C, Martí S, et al., Infectious Aetiology of Acute Exacerbations in Severe COPD Patients. J Infect 2013;19:255–7.
Sapey E, RA Stockley . COPD exacerbations. 2: aetiology. Thorax 2006;61:250–8. http://dx.doi.org/10.1136/thx.2005.041822
Patel I . Exacerbations of chronic obstructive pulmonary disease: definition, aetiology and management. Clin Med 2009;9:170–73. http://dx.doi.org/10.7861/clinmedicine.9-2-170
Rizkallah J, Man SF, Sin DD . Prevalence of pulmonary embolism in acute exacerbations of COPD: a systematic review and metaanalysis. Chest 2009;135:786–93. http://dx.doi.org/10.1378/chest.08-1516
Tillie-Leblond I, Marquette C-H, Perez T, et al. Pulmonary embolism in patients with unexplained exacerbation of chronic obstructive pulmonary disease: prevalence and risk factors. Ann Intern Med 2006;144:390–6. http://dx.doi.org/10.7326/0003-4819-144-6-200603210-00005
Zvezdin B, Milutinov S, Kojicic M, et al. A postmortem analysis of major causes of early death in patients hospitalized with COPD exacerbation. Chest 2009;136:376–80. http://dx.doi.org/10.1378/chest.08-2918
Ramakant Bobby . World Asthma DaY: Asthma control is appalling in countries. [cited 2013 September 28]; Available from: http://www.opednews.com/articles/World-Asthma-DaY-Asthma-c-by-Bobby-Ramakant-090503-711.html
Snow V, Lascher S, Mottur-Pilson C . Evidence base for management of acute exacerbations of chronic obstructive pulmonary disease. Ann Intern Med 2001;134:595–9. http://dx.doi.org/10.7326/0003-4819-134-7-200104030-00015
Medford AR . Pulmonary arterial enlargement and COPD exacerbations. N Engl J Med 2012;367:2253–4. http://dx.doi.org/10.1056/NEJMc1212050
Garssen B, Colla P, Van Dixhoorn J, et al. Het herkennen van het hyperventilatiesyndroom. Medisch Contact 1984;35:1122–4.
Johns MW . A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991;14:540–5.
Medford AR . Arrhythmias in COPD: consider P-wave dispersion and pulmonary hypertension, too. Chest 2013;143:579. http://dx.doi.org/10.1378/chest.12-2199
Wijesuriya S, Chandratreya L, Medford AR . Chronic pulmonary emboli and radiologic mimics on CT pulmonary angiography: a diagnostic challenge. Chest 2013;143:1460–71. http://dx.doi.org/10.1378/chest.12-1384
Agarwal R . Bronchiectasis in acute pneumonia: Pseudobronchiectasis. Chest 2007;132:2054–5. http://dx.doi.org/10.1378/chest.07-1529
Pengo V, Lensing AW, Prins MH, et al; for the Thromboembolic Pulmonary Hypertension Study Group. Incidence of chronic thromboembolic pulmonary hypertension after pulmonary embolism. N Engl J Med 2004;350:2257–64. http://dx.doi.org/10.1056/NEJMoa032274
van Beek E, Elliot C, Kiely D . Diagnosis and initial treatment of patients with suspected pulmonary thromboembolism. Contin Educ Anaesth Crit Care Pain 2009;9:119–24. http://dx.doi.org/10.1093/bjaceaccp/mkp016
Condliffe R, Kiely DG, Gibbs JS et al. Improved outcomes in medically and surgically treated chronic thromboembolic pulmonary hypertension. Am J Respir Crit Care Med 2008;177:1122–7. http://dx.doi.org/10.1164/rccm.200712-1841OC
Corsico AG, D'Armini AM, Cerveri I, et al. Long-term outcome after pulmonary endarterectomy. Am J Respir Crit Care Med 2008;178:419–24. http://dx.doi.org/10.1164/rccm.200801-101OC
Pepke-Zaba J, Delcroix M, Lang I et al. Chronic thromboembolic pulmonary hypertension (CTEPH): results from an international prospective registry. Circulation 2011;124:1973–81. http://dx.doi.org/10.1161/CIRCULATIONAHA.110.015008
Milne EN . Correlation of physiologic findings with chest roentgenology. Radiol Clin North Am 1973;11:17–47.
Gehlbach BK, Geppert E . The pulmonary manifestations of left heart failure. Chest 2004;125:669–82. http://dx.doi.org/10.1378/chest.125.2.669
Boussuges A, Pinet C, Molenat F, et al. Left atrial and ventricular filling in chronic obstructive pulmonary disease. An echocardiographic and Doppler study. Am J Respir Crit Care Med 2000;162:670–5. http://dx.doi.org/10.1164/ajrccm.162.2.9908056
Vizza CD, Lynch JP, Ochoa LL, Richardson G, Trulock EP . Right and left ventricular dysfunction in patients with severe pulmonary disease. Chest 1998;113:576–83. http://dx.doi.org/10.1378/chest.113.3.576
Bozkanat E, Tozkoparan E, Baysan O, Deniz O, Ciftci F, Yokusoglu M . The significance of elevated brain natriuretic peptide levels in chronic obstructive pulmonary disease. J Int Med Res 2005;33:537–44. http://dx.doi.org/10.1177/147323000503300509
Morrison LK, Harrison A, Krishnwswamy P, Kazangra R, Clopton P, Maisal A . Utility of a rapid B-natriuretic peptide assay in differentiating congestive heart failure from lung disease in patients presenting with dyspnea. J Am Coll Cardiol 2002;39:202–09. http://dx.doi.org/10.1016/S0735-1097(01)01744-2
Silver MA, Maisel A, Yancy CW, et al. BNP Consensus Panel 2004: A clinical approach for the diagnostic, prognostic, screening, treatment monitoring, and therapeutic roles of natriuretic peptides in cardiovascular diseases. Congest Heart Fail 2004;10(Suppl. 5 3):1–30
Januzzi JL, van Kimmenade R, Lainchbury J, et al. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: an international pooled analysis of 1256 patients: the International Collaborative of NT-proBNP Study. Eur Heart J 2006;27:330–37. http://dx.doi.org/10.1093/eurheartj/ehi631
Light RW, George RB . Serial pulmonary function in patients with acute heart failure. Arch Intern Med 1983;143:429–33. http://dx.doi.org/10.1001/archinte.1983.00350030039007
Petermann W, Barth J, Entzian P . Heart failure and airway obstruction. Int J Cardiol 1987;17:207–09. http://dx.doi.org/10.1016/0167-5273(87)90132-X
Acknowledgements
Handling editor Hilary Pinnock
Funding None
Author information
Authors and Affiliations
Contributions
AK wrote the section on differentiating respiratory and cardiac causes, and KG-J wrote the section on other causes of breathlessness. FvG and BK considered the management of breathlessness from the perpsective of a resource limited setting, and AM from a secondary care perspective. The handling editor (HP) collated and edited the individual sections.
Corresponding author
Ethics declarations
Competing interests
AK has been on the advisory boards or speaker bureau for Astra Zeneca, Boehringer Ingelheim, Aerocrine, Griffols, Pfizer, Purdue, Novartis and Takeda.
KG-J has spoken on behalf of, or acted as a consultant for, Almirall, Chiesi. Astra Zeneca, Glaxo Smith Kline, Boehringer Ingelheim, Novartis, Napp/Mundi Pharma. Merck, Sharpe and Dohme.
FvG, BK and AM have no conflicts of interest in relation to this article.
Rights and permissions
About this article
Cite this article
Kaplan, A., Gruffydd-Jones, K., van Gemert, F. et al. A woman with breathlessness: a practical approach to diagnosis and management. Prim Care Respir J 22, 468–476 (2013). https://doi.org/10.4104/pcrj.2013.00100
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.4104/pcrj.2013.00100