Abstract
Background:
Knowledge of factors associated with the course of lower urinary tract symptoms (LUTS) before treatment is needed to inform preventive interventions. In a prospective study of elderly men untreated for LUTS, we identified factors associated with symptom progression and remission.
Methods:
In community-dwelling US men aged ⩾65 years, the American Urological Association Symptom Index (AUA-SI) was repeated four times, once at baseline (2000–2002) and then every 2 years thereafter. Analyses included 1740 men with all four AUA-SI assessments, who remained free from diagnosed prostate cancer, and who reported no treatment for LUTS or BPH during follow-up that averaged 6.9 (±0.4) years. LUTS change was determined with group-based trajectory modelingof the repeated AUA-SI measures. Multivariable logistic regression was then used to determine the baseline factors associated with progressing compared with stable trajectories, and with remitting compared with progressing trajectories. Lifestyle, body mass index (BMI) (kg/m2), mobility, mental health (Short-Form 12), medical history and prescription medications were considered for selection. Odds ratios (ORs) and 95% confidence intervals (CIs) were estimated for variables in each model.
Results:
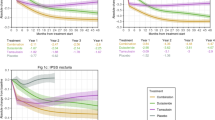
We identified 10 AUA-SI trajectories: 4 stable (1277 men, 73%), three progressing (345 men, 20%), two remitting (98 men, 6%) and one mixed (20 men, 1%). Men in progressing compared with stable trajectories were more likely to have mobility limitations (OR=2.0, 95% CI: 1.0–3.8), poor mental health (OR=1.9, 95% CI: 1.1–3.4), BMI⩾25.0 kg m−2 (OR=1.7, 95% CI: 1.0–2.8), hypertension (OR=1.5, 95% CI: 1.0–2.4) and back pain (OR=1.5, 95% CI: 1.0–2.4). Men in remitting compared with progressing trajectories more often used central nervous system medications (OR=2.3, 95% CI: 1.1–4.9) and less often had a history of problem drinking (OR=0.4, 95% CI: 0.2–0.9).
Conclusions:
Several non-urological lifestyle and health factors were independently associated with risk of LUTS progression in older men.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Boyle P, Robertson C, Mazzetta C, Keech M, Hobbs FD, Fourcade R et al. The prevalence of lower urinary tract symptoms in men and women in four centres. The UrEpik study. BJU Int 2003; 92: 409–414.
Irwin DE, Kopp ZS, Agatep B, Milsom I, Abrams P . Worldwide prevalence estimates of lower urinary tract symptoms, overactive bladder, urinary incontinence and bladder outlet obstruction. BJU Int 2011; 108: 1132–1138.
Parsons JK, Bergstrom J, Silberstein J, Barrett-Connor E . Prevalence and characteristics of lower urinary tract symptoms in men aged>or=80 years. Urology 2008; 72: 318–321.
Haidinger G, Waldhor T, Madersbacher S, Schatzl G, Vutuc C . Prevalence of lower urinary tract symptoms in Austrian males: update 2009. Urol Int 2011; 87: 385–391.
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U et al. The standardisation of terminology in lower urinary tract function: report from the standarization sub-committee of the International Continence Society. Urology 2003; 61: 37–49.
Barry MJ, Fowler FJ Jr., O'Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol 1992; 148: 1549–1557.
Taylor BC, Wilt TJ, Fink HA, Lambert LC, Marshall LM, Hoffman AR et al. Prevalence, severity, and health correlates of lower urinary tract symptoms among older men: the MrOS study. Urology 2006; 68: 804–809.
Kupelian V, Wei JT, O’Leary MP, Kusek JW, Litman HJ, Link CL et al. Prevalence of lower urinary tract symptoms and effect on quality of life in a racially and ethnically diverse random sample: the Boston Area Community Health (BACH) Survey. Arch Inter Med 2006; 166: 2381–2387.
Parsons JK, Mougey J, Lambert L, Wilt TJ, Fink HA, Garzotto M et al. Lower urinary tract symptoms increase the risk of falls in older men. BJU Int 2009; 104: 63–68.
Kupelian V, Fitzgerald MP, Kaplan SA, Norgaard JP, Chiu GR, Rosen RC . Association of nocturia and mortality: results from the Third National Health and Nutrition Examination Survey. J Urol 2011; 185: 571–577.
Wei JT, Calhoun E, Jacobsen SJ . Urologic diseases in America project: benign prostatic hyperplasia. J Urol 2005; 173: 1256–1261.
Hu TW, Wagner TH, Bentkover JD, LeBlanc K, Piancentini A, Stewart WF et al. Estimated economic costs of overactive bladder in the United States. Urology 2003; 61: 1123–1128.
National Center for Health Statistics. Health United States, 2013: With Special Feature on Emergency Care. Hyattsville, MD. 2013. Available at http://www.cdc.gov/nchs/data/hus/hus12.pdf. (last accessed 19 July 2013).
Burke JP, Rhodes T, Jacobson DJ, McGree ME, Roberts RO, Girman CJ et al. Association of anthropmetric measures with the presence and progression of benign prostatic hyperplasia. Am J Epidemiol 2006; 164: 41–46.
Kok ET, Schouten BW, Bohnen AM, Groeneveld FP, Thomas S, Bosch JL . Risk factors for lower urinary tract symptoms suggestive of benign prostatic hyperplasia in a community based population of healthy aging men: the Krimpen study. J Urol 2009; 181: 710–716.
Parsons JK, Messer K, White M, Barrett-Connor E, Bauer DC, Marshall LM . Obesity increases and physical activity decreases lower urinary tract symptom risk in older men: the Osteoporotic Fractures in Men (MrOS) Study. Eur Urol 2011; 60: 1173–1180.
Martin S, Lange K, Haren MT, Taylor AW, Wittert G . Risk factors for progression and improvement of lower urinary tract symptoms (LUTS) in a prospective cohort of men. J Urol 2014; 191: 130–137.
Wolters R, Wensing M, van Weel C, van der Wilt GJ, Grol RP . Lower urinary tract symptoms: social influence is more important than symptoms in seeking medical care. BJU Int 2002; 90: 655–661.
Krambeck AE, Jacobson DJ, McGree ME, Lightner DJ, Lieber MM, Jacobsen SJ et al. Effectiveness of medical and surgical therapies for lower urinary tract symptoms in the community setting. BJU Int 2012; 110: 1332–1337.
Jacobsen SJ, Girman CJ, Guess HA, Rhodes T, Oesterling JE, Lieber MM . Natural history of prostatism: longitudinal changes in voiding symptoms in community dwelling men. J Urol 1996; 155: 595–600.
Lee AJ, Garraway WM, Simpson RJ, Fisher W, King D . The natural history of untreated lower urinary tract symptoms in middle-aged and elderly men over a period of five years. Eur Urol 1998; 34: 325–332.
Masumori N, Tsukamoto T, Rhodes T, Girman CJ . Natural history of lower urinary tract symptoms in men—result of a longitudinal community-based study in Japan. Urology 2003; 61: 956–960.
Temml C, Brossner C, Schatzl G, Ponholzer A, Knoepp L, Madersbacher S . The natural history of lower urinary tract symptoms over five years. Eur Urol 2003; 43: 374–380.
Sarma AV, McLaughlin JC, Jacobsen SJ, Logie J, Dolin P, Dunn RL et al. Longitudinal change in lower urinary tract symptoms among a chort of black American men: the Flint Men’s Health Study. Urology 2003; 61: 595–600.
Parsons JK, Wilt TJ, Wang PY, Barrett-Connor E, Bauer DC, Marshall LM . Progression of lower urinary tract symptoms in older men: a community based study. J Urol 2010; 183: 1915–1920.
Maserejian NN, Chen S, Chiu GR, Araujo AB, Kupelian V, Hall SA et al. Treatment status and progression or regression of lower urinary tract symptoms in a general adult population sample. J Urol 2014; 191: 107–113.
Jones BL, Nagin DS, Roeder K . A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Method Res 2001; 29: 374–393.
Nagin DS, Odgers CL . Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol 2010; 6: 109–138.
Gill TM, Gahbauer EA, Han L, Allore HG . Trajectories of disability in the last year of life. N Engl J Med 2010; 362: 1173–1180.
Orwoll E, Blank JB, Barrett-Connor E, Cauley J, Cummings S, Ensrud K et al. Design and baseline characteristics of the osteoporotic fractures in men (MrOS) study—a large observational study of the determinants of fracture in older men. Contemp Clin Trials 2005; 26: 569–585.
Blank JB, Cawthon PM, Carrion-Petersen ML, Harper L, Johnson JP, Mitson E et al. Overview of the recruitment for the Osteoporotic Fractures in Men Study (MrOS). Contemp Clin Trials 2005; 26: 557–568.
Pahor M, Chrischilles EA, Guralnik JM, Brown SL, Wallace RB, Carbonin P . Drug data coding and analysis in epidemiologic studies. Eur J Epidemiol 1994; 10: 405–411.
Ewing JA . Detecting alcoholism. The CAGE questionnaire. JAMA 1984; 25: 1905–1907.
Buchsbaum DG, Buchanan RG, Welsh J, Centor RM, Schnoll SH . Screening for drinking disorders in the elderly using the CAGE questionnaire. J Am Geriatr Soc 1992; 40: 662–665.
Block G, Hartman AM, Naughton D . A reduced dietary questionnaire: development and validation. Epidemiol 1990; 1: 58–64.
Washburn RA, Smith KW, Jette AM, Janney CA . The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol 1993; 46: 153–162.
Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB . Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med 1995; 332: 556–561.
Ware J Jr, Kosinski M, Keller SD . A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996; 34: 220–233.
Gill SC, Butterworth P, Rodgers B, Mackinnon A . Validity of the mental health component scale of the 12-item Short-Form Health Survey (MCS-12) as measure of common mental disorders in the general population. Psychiatry Res 2007; 152: 63–71.
Mokdad AH, Serdula MK, Dietz WH, Bowman BA, Marks JS, Koplan JP . The spread of the obesity epidemic in the United States, 1991-1998. JAMA 1999; 282: 1519–1522.
Perreira KM, Sloan FA . Excess alcohol consumption and health outcomes: a 6-year follow-up of men over age 50 from the health and retirement study. Addiction 2002; 97: 301–310.
Andersson KE, Wein AJ . Pharmacology of the lower urinary tract: basis for current and future treatments of urinary incontinence. Pharmacol Rev 2004; 56: 581–631.
Parsons JK, Sarma AV, McVary K, Wei JT . Obesity and benign prostatic hyperplasia: clinical connections, emerging etiological paradigms and future directions. J Urol 2012; 189: S102–S106.
Parsons JK, Kashefi C . Physical activity, benign prostatic hyperplasia, and lower urinary tract symptoms. Eur Urol 2008; 53: 1228–1235.
De Nunzio C, Aronson W, Freedland SJ, Giovannucci E, Parsons JK . The correlation between metabolic syndrome and prostatic diseases. Eur Urol 2013; 61: 560–570.
McVary KT, Rademaker A, Lloyd GL, Gann P . Autonomic nervous system overactivity in men with lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Urol 2005; 174: 1327–1338.
Yamanishi T, Yasuda K, Sakakibara R, Murayama N, Hattori T, Ito H . Detrusor overactivity and penile erection in patients with lower lumbar spine lesions. Eur Urol 1998; 34: 360–364.
Bartolin Z, Savic I, Persec Z . Relationship between clinical data and urodynamic findings in patients with lumbar intervertebral disk protrusion. Urol Res 2002; 30: 219–222.
Inui Y, Doita M, Ouchi K, Tsukuda M, Fujita N, Kurosaka M . Clinical and radiologic features of lumbar spinal stenosis and disc herniation with neuropathic bladder. Spine 2004; 29: 869–873.
Acknowledgements
This work was supported by the National Institute for Diabetes and Digestive and Kidney Diseases (Grant R21 DK083675 to LMM and JKP). The MrOS Study is supported by National Institutes of Health funding. The following institutes provide support: the National Institute on Aging (NIA), the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Center for Advancing Translational Sciences (NCATS) and NIH Roadmap for Medical Research under the following grant numbers: U01 AG027810, U01 AG042124, U01 AG042139, U01 AG042140, U01 AG042143, U01 AG042145, U01 AG042168, U01 AR066160 and UL1 TR000128.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
Dr Parsons and Dr Marshall received funding as co-Principal Investigators for this research from the US National Institutes of Health under grant R21 DK083675. Dr Parsons also reports relationships with AMS and Sophiris outside the submitted work. All other authors declare no conflict of interests.
Additional information
Supplementary Information accompanies the paper on the Prostate Cancer and Prostatic Diseases website
Supplementary information
Rights and permissions
About this article
Cite this article
Marshall, L., Holton, K., Parsons, J. et al. Lifestyle and health factors associated with progressing and remitting trajectories of untreated lower urinary tract symptoms among elderly men. Prostate Cancer Prostatic Dis 17, 265–272 (2014). https://doi.org/10.1038/pcan.2014.22
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2014.22