Abstract
Pain is a nonmotor symptom that substantially affects the quality of life of at least one-third of patients with Parkinson disease (PD). Interestingly, patients with PD frequently report different types of pain, and a successful approach to distinguish between these pains is required so that effective treatment strategies can be established. Differences between these pains are attributable to varying peripheral pain mechanisms, the role of motor symptoms in causing or amplifying pain, and the role of PD pathophysiology in pain processing. In this Review, we propose a four-tier taxonomy to improve classification of pain in PD. This taxonomy assigns nociceptive, neuropathic and miscellaneous pains to distinct categories, as well as further characterization into subcategories. Currently, treatment of pain in PD is based on empirical data only, owing to a lack of controlled studies. The facultative symptom of 'dopaminergically maintained pain' refers to pain that benefits from antiparkinson medication. Here, we also present additional pharmacological and nonpharmacological treatment approaches, which can be targeted to a specific pain following classification using our taxonomy.
Key Points
-
Up to 80% of patients with Parkinson disease (PD) experience chronic pain
-
The basal ganglia are involved in pain processing, but their exact contribution to pain in PD is unclear
-
In a four-tier taxonomy on pains in PD, nociceptive pain must be distinguished from neuropathic and miscellaneous pain
-
'Dopaminergically maintained pain' refers to pain that can be alleviated by antiparkinson medication
-
Symptomatic analgesic treatment based on clinical pain classification includes pharmacological, nonpharmcological and invasive approaches
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Chaudhuri, K. R. & Schapira, A. H. Non-motor symptoms of Parkinson's disease: dopaminergic pathophysiology and treatment. Lancet Neurol. 8, 464–474 (2009).
Lees, A. J., Hardy, J. & Revesz, T. Parkinson's disease. Lancet 373, 2055–2066 (2009).
Lee, M. A., Walker, R. W., Hildreth, T. J. & Prentice, W. M. A survey of pain in idiopathic Parkinson's disease. J. Pain Symptom Manage. 32, 462–469 (2006).
Ford, B. Pain in Parkinson's disease. Mov. Disord. 25 (Suppl. 1), S98–S103 (2010).
Negre-Pages, L., Regragui, W., Bouhassira, D., Grandjean, H. & Rascol, O. Chronic pain in Parkinson's disease: the cross-sectional French DoPaMiP survey. Mov. Disord. 23, 1361–1369 (2008).
Wasner, G. & Deuschl, G. Chapter 50 Pain in Parkinson's disease. Handb. Clin. Neurol. 81, 747–760 (2006).
Parkinson, J. An Essay on the Shaking Palsy (Whittingham and Rowland, London, 1817).
Barone, P. et al. The PRIAMO study: a multicenter assessment of nonmotor symptoms and their impact on quality of life in Parkinson's disease. Mov. Disord. 24, 1641–1649 (2009).
Defazio, G. et al. Pain as a nonmotor symptom of Parkinson disease: evidence from a case–control study. Arch. Neurol. 65, 1191–1194 (2008).
Giuffrida, R., Vingerhoets, F. J., Bogousslavsky, J. & Ghika, J. Pain in Parkinson's disease [French]. Rev. Neurol. (Paris) 161, 407–418 (2005).
Mott, S., Kenrick, M., Dixon, M. & Bird, G. Pain as a sequela of Parkinson disease. Aust. Fam. Physician 33, 663–664 (2004).
Koller, W. C. Sensory symptoms in Parkinson's disease. Neurology 34, 957–959 (1984).
Snider, S. R., Fahn, S., Isgreen, W. P. & Cote, L. J. Primary sensory symptoms in parkinsonism. Neurology 26, 423–429 (1976).
Beiske, A. G., Loge, J. H., Ronningen, A. & Svensson, E. Pain in Parkinson's disease: Prevalence and characteristics. Pain 141, 173–177 (2009).
Goetz, C. G., Tanner, C. M., Levy, M., Wilson, R. S. & Garron, D. C. Pain in Parkinson's disease. Mov. Disord. 1, 45–49 (1986).
Ford, B. Pain in Parkinson's disease. Clin. Neurosci. 5, 63–72 (1998).
Lev, N. & Melamed, E. Sensory symptoms and pain in Parkinson disease [Hebrew]. Harefuah 138, 324–326 (2000).
Sage, J. I. Pain in Parkinson's Disease. Curr. Treat. Options Neurol. 6, 191–200 (2004).
Quittenbaum, B. H. & Grahn, B. Quality of life and pain in Parkinson's disease: a controlled cross-sectional study. Parkinsonism Relat. Disord. 10, 129–136 (2004).
Politis, M. et al. Parkinson's disease symptoms: the patient's perspective. Mov. Disord. 25, 1646–1651 (2010).
Bergman, H. & Deuschl, G. Pathophysiology of Parkinson's disease: from clinical neurology to basic neuroscience and back. Mov. Disord. 17 (Suppl. 3), S28–S40 (2002).
Obeso, J. A. et al. The basal ganglia in Parkinson's disease: current concepts and unexplained observations. Ann. Neurol. 64 (Suppl. 2), S30–S46 (2008).
Braak, H. et al. Staging of brain pathology related to sporadic Parkinson's disease. Neurobiol. Aging 24, 197–211 (2003).
Wakabayashi, K. & Takahashi, H. Neuropathology of autonomic nervous system in Parkinson's disease. Eur. Neurol. 38 (Suppl. 2), 2–7 (1997).
Mouraux, A., Diukova, A., Lee, M. C., Wise, R. G. & Iannetti, G. D. A multisensory investigation of the functional significance of the “pain matrix”. Neuroimage 54, 2237–2249 (2011).
Chudler, E. H. & Dong, W. K. The role of the basal ganglia in nociception and pain. Pain 60, 3–38 (1995).
Becerra, L., Breiter, H. C., Wise, R., Gonzalez, R. G. & Borsook, D. Reward circuitry activation by noxious thermal stimuli. Neuron 32, 927–946 (2001).
Jensen, J. et al. Direct activation of the ventral striatum in anticipation of aversive stimuli. Neuron 40, 1251–1257 (2003).
Shu, S. Y., McGinty, J. F. & Peterson, G. M. High density of zinc-containing and dynorphin B- and substance P-immunoreactive terminals in the marginal division of the rat striatum. Brain Res. Bull 24, 201–205 (1990).
Shu, S. Y., Penny, G. R. & Peterson, G. M. The 'marginal division': a new subdivision in the neostriatum of the rat. J. Chem. Neuroanat. 1, 147–163 (1988).
Anagnostakis, Y., Zis, V. & Spyraki, C. Analgesia induced by morphine injected into the pallidum. Behav. Brain Res. 48, 135–143 (1992).
Baumeister, A. A., Hawkins, M. F., Anticich, T. G., Moore, L. L. & Higgins, T. D. Bilateral intranigral microinjection of morphine and opioid peptides produces antinociception in rats. Brain Res. 411, 183–186 (1987).
Baumeister, A. A. et al. Evidence that the substantia nigra is a component of the endogenous pain suppression system in the rat. Brain Res. 447, 116–121 (1988).
Gao, D. M., Jeaugey, L., Pollak, P. & Benabid, A. L. Intensity-dependent nociceptive responses from presumed dopaminergic neurons of the substantia nigra, pars compacta in the rat and their modification by lateral habenula inputs. Brain Res. 529, 315–319 (1990).
Pay, S. & Barasi, S. A study of the connections of nociceptive substantia nigra neurones. Pain 12, 75–89 (1982).
Harper, J. A., Labuszewski, T. & Lidsky, T. I. Substantia nigra unit responses to trigeminal sensory stimulation. Exp. Neurol. 65, 462–470 (1979).
Richards, C. D. & Taylor, D. C. Electrophysiological evidence for a somatotopic sensory projection to the striatum of the rat. Neurosci. Lett. 30, 235–240 (1982).
Barnes, C. D., Fung, S. J. & Adams, W. L. Inhibitory effects of substantia nigra on impulse transmission from nociceptors. Pain 6, 207–215 (1979).
Yamamoto, T., Samejima, A. & Oka, H. An intracellular analysis of the entopeduncular inputs on the centrum medianum-parafascicular nuclear complex in cats. Brain Res. 348, 343–347 (1985).
Kemel, M. L., Desban, M., Gauchy, C., Glowinski, J. & Besson, M. J. Topographical organization of efferent projections from the cat substantia nigra pars reticulata. Brain Res. 455, 307–323 (1988).
Vives, F., Gayoso, M. J., Osorio, C. & Mora, F. Afferent pathways to points of self-stimulation in the medial prefrontal cortex of the rat as revealed by the horseradish peroxidase technique. Behav. Brain Res. 8, 23–32 (1983).
Seifert, F. & Maihofner, C. Functional and structural imaging of pain-induced neuroplasticity. Curr. Opin. Anaesthesiol. 24, 515–523 (2011).
Magnusson, J. E. & Fisher, K. The involvement of dopamine in nociception: the role of D1 and D2 receptors in the dorsolateral striatum. Brain Res. 855, 260–266 (2000).
Dennis, S. G. & Melzack, R. Effects of cholinergic and dopaminergic agents on pain and morphine analgesia measured by three pain tests. Exp. Neurol. 81, 167–176 (1983).
Gao, X., Zhang, Y. & Wu, G. Effects of dopaminergic agents on carrageenan hyperalgesia in rats. Eur. J. Pharmacol. 406, 53–58 (2000).
Hagelberg, N. et al. Striatal dopamine D2 receptors in modulation of pain in humans: a review. Eur. J. Pharmacol. 500, 187–192 (2004).
Pertovaara, A. et al. Striatal dopamine D2/D3 receptor availability correlates with individual response characteristics to pain. Eur. J. Neurosci. 20, 1587–1592 (2004).
Jensen, T. S. & Yaksh, T. L. Effects of an intrathecal dopamine agonist, apomorphine, on thermal and chemical evoked noxious responses in rats. Brain Res. 296, 285–293 (1984).
Burkey, A. R., Carstens, E. & Jasmin, L. Dopamine reuptake inhibition in the rostral agranular insular cortex produces antinociception. J. Neurosci. 19, 4169–4179 (1999).
Rosland, J. H., Hunskaar, S., Broch, O. J. & Hole, K. Acute and long term effects of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) in tests of nociception in mice. Pharmacol. Toxicol. 70, 31–37 (1992).
Carey, R. J. Acute ipsilateral hyperalgesia and chronic contralateral hypoalgesia after unilateral 6-hydroxydopamine lesions of the substantia nigra. Exp. Neurol. 91, 277–284 (1986).
Lewis, G. N. & Byblow, W. D. Altered sensorimotor integration in Parkinson's disease. Brain 125, 2089–2099 (2002).
Djaldetti, R. et al. Quantitative measurement of pain sensation in patients with Parkinson disease. Neurology 62, 2171–2175 (2004).
Zambito Marsala, S. et al. Spontaneous pain, pain threshold, and pain tolerance in Parkinson's disease. J. Neurol. 258, 627–633 (2011).
Mylius, V. et al. Pain sensitivity and descending inhibition of pain in Parkinson's disease. J. Neurol. Neurosurg. Psychiatry 80, 24–28 (2009).
Perrotta, A. et al. Facilitated temporal summation of pain at spinal level in Parkinson's disease. Mov. Disord. 26, 442–448 (2011).
Schestatsky, P. et al. Neurophysiologic study of central pain in patients with Parkinson disease. Neurology 69, 2162–2169 (2007).
Gerdelat-Mas, A. et al. Levodopa raises objective pain threshold in Parkinson's disease: a RIII reflex study. J. Neurol. Neurosurg. Psychiatry 78, 1140–1142 (2007).
Brefel-Courbon, C. et al. Effect of levodopa on pain threshold in Parkinson's disease: a clinical and positron emission tomography study. Mov. Disord. 20, 1557–1563 (2005).
Dellapina, E. et al. Apomorphine effect on pain threshold in Parkinson's disease: a clinical and positron emission tomography study. Mov. Disord. 26, 153–157 (2011).
Tinazzi, M. et al. Hyperalgesia and laser evoked potentials alterations in hemiparkinson: evidence for an abnormal nociceptive processing. J. Neurol. Sci. 276, 153–158 (2009).
Tinazzi, M. et al. Abnormal processing of the nociceptive input in Parkinson's disease: a study with CO2 laser evoked potentials. Pain 136, 117–124 (2008).
Gierthmuhlen, J. et al. Influence of deep brain stimulation and levodopa on sensory signs in Parkinson's disease. Mov. Disord. 25, 1195–1202 (2010).
Rolke, R. et al. Quantitative sensory testing in the German Research Network on Neuropathic Pain (DFNS): standardized protocol and reference values. Pain 123, 231–243 (2006).
Nolano, M. et al. Sensory deficit in Parkinson's disease: evidence of a cutaneous denervation. Brain 131, 1903–1911 (2008).
Toth, C. et al. Levodopa, methylmalonic acid, and neuropathy in idiopathic Parkinson disease. Ann. Neurol. 68, 28–36 (2010).
Toth, C., Brown, M. S., Furtado, S., Suchowersky, O. & Zochodne, D. Neuropathy as a potential complication of levodopa use in Parkinson's disease. Mov. Disord. 23, 1850–1859 (2008).
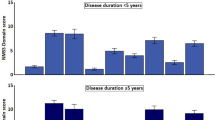
Tinazzi, M. et al. Pain and motor complications in Parkinson's disease. J. Neurol. Neurosurg. Psychiatry 77, 822–825 (2006).
Chaudhuri, K. R., Odin, P., Antonini, A. & Martinez-Martin, P. Parkinson's disease: the non-motor issues. Parkinsonism Relat. Disord. 17, 717–723 (2011).
Ford, B., Louis, E. D., Greene, P. & Fahn, S. Oral and genital pain syndromes in Parkinson's disease. Mov. Disord. 11, 421–426 (1996).
Verhaak, P. F., Kerssens, J. J., Dekker, J., Sorbi, M. J. & Bensing, J. M. Prevalence of chronic benign pain disorder among adults: a review of the literature. Pain 77, 231–239 (1998).
Breivik, H., Collett, B., Ventafridda, V., Cohen, R. & Gallacher, D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur. J. Pain 10, 287–333 (2006).
Bouhassira, D., Lanteri-Minet, M., Attal, N., Laurent, B. & Touboul, C. Prevalence of chronic pain with neuropathic characteristics in the general population. Pain 136, 380–387 (2008).
Fox, P. L., Raina, P. & Jadad, A. R. Prevalence and treatment of pain in older adults in nursing homes and other long-term care institutions: a systematic review. CMAJ 160, 329–333 (1999).
Loeser, J. D. & Treede, R. D. The Kyoto protocol of IASP Basic Pain Terminology. Pain 31, 473–477 (2008).
Treede, R. D. et al. Neuropathic pain: redefinition and a grading system for clinical and research purposes. Neurology 70, 1630–1635 (2008).
Baron, R., Binder, A. & Wasner, G. Neuropathic pain: diagnosis, pathophysiological mechanisms, and treatment. Lancet Neurol. 9, 807–819 (2010).
Wasner, G. Central pain syndromes. Curr. Pain Headache Rep. 14, 489–496 (2010).
Sethi, K. Levodopa unresponsive symptoms in Parkinson disease. Mov. Disord. 23 (Suppl. 3), S521–S533 (2008).
Ashour, R., Tintner, R. & Jankovic, J. Striatal deformities of the hand and foot in Parkinson's disease. Lancet Neurol. 4, 423–431 (2005).
Ashour, R. & Jankovic, J. Joint and skeletal deformities in Parkinson's disease, multiple system atrophy, and progressive supranuclear palsy. Mov. Disord. 21, 1856–1863 (2006).
Riley, D., Lang, A. E., Blair, R. D., Birnbaum, A. & Reid, B. Frozen shoulder and other shoulder disturbances in Parkinson's disease. J. Neurol. Neurosurg. Psychiatry 52, 63–66 (1989).
Madden, M. B. & Hall, D. A. Shoulder pain in Parkinson's disease: a case–control study. Mov. Disord. 25, 1105–1106 (2010).
Stamey, W., Davidson, A. & Jankovic, J. Shoulder pain: a presenting symptom of Parkinson disease. J. Clin. Rheumatol. 14, 253–254 (2008).
Ha, A. D. & Jankovic, J. Pain in Parkinson's disease. Mov. Disord. http://dx.doi.org/10.1002/mds.23959.
Etchepare, F. et al. Back problems in Parkinson's disease: an underestimated problem. Joint Bone Spine 73, 298–302 (2006).
Broetz, D., Eichner, M., Gasser, T., Weller, M. & Steinbach, J. P. Radicular and nonradicular back pain in Parkinson's disease: a controlled study. Mov. Disord. 22, 853–856 (2007).
Sandyk, R. Back pain as an early symptom of Parkinson's disease. S. Afr. Med. J. 61, 3 (1982).
Mazanec, D. J. Evaluating back pain in older patients. Cleve. Clin. J. Med. 66, 89–91, 95–99 (1999).
Quinn, N. P., Koller, W. C., Lang, A. E. & Marsden, C. D. Painful Parkinson's disease. Lancet 1, 1366–1369 (1986).
Samii, A., Nutt, J. G. & Ransom, B. R. Parkinson's disease. Lancet 363, 1783–1793 (2004).
Nebe, A. & Ebersbach, G. Pain intensity on and off levodopa in patients with Parkinson's disease. Mov. Disord. 24, 1233–1237 (2009).
Wickremaratchi, M. M. et al. The motor phenotype of Parkinson's disease in relation to age at onset. Mov. Disord. 26, 457–463 (2011).
Poewe, W., Lees, A. J., Steiger, D. & Stern, G. M. Foot dystonia in Parkinson's disease: clinical phenomenology and neuropharmacology. Adv. Neurol. 45, 357–360 (1987).
Jost, W. H. Autonomic dysfunctions in idiopathic Parkinson's disease. J. Neurol. 250 (Suppl. 1), I28–I30 (2003).
Wasner, G. & Baron, R. Systemdegeneration und Morbus Parkinson-Neurovegetative Diagnostik in Evozierte Potentiale, Neurovegetative Diagnostik, Okulographie (eds Buchner, H. & Noth, J.) 200–206 (Thieme Verlag, Stuttgart, 2005).
Wasner, G. & Baron, R. Orthostatic dysregulation—symptoms, pathophysiology and treatment. Akt Neurol. 27, 157–169 (2000).
Bleasdale-Barr, K. M. & Mathias, C. J. Neck and other muscle pains in autonomic failure: their association with orthostatic hypotension. J. R. Soc. Med. 91, 355–359 (1998).
Waseem, S. & Gwinn-Hardy, K. Pain in Parkinson's disease. Common yet seldom recognized symptom is treatable. Postgrad Med 110, 33–34, 39–40, 46 (2001).
Quigley, E. M. Gastrointestinal dysfunction in Parkinson's disease. Semin. Neurol. 16, 245–250 (1996).
Edwards, L., Quigley, E. M., Hofman, R. & Pfeiffer, R. F. Gastrointestinal symptoms in Parkinson disease: 18-month follow-up study. Mov. Disord. 8, 83–86 (1993).
Jost, W. H. Gastrointestinal motility problems in patients with Parkinson's disease. Effects of antiparkinsonian treatment and guidelines for management. Drugs Aging 10, 249–258 (1997).
Lebouvier, T. et al. Colonic biopsies to assess the neuropathology of Parkinson's disease and its relationship with symptoms. PLoS ONE 5, e12728 (2010).
Mengi-Ozsarac, G. Carpal tunnel syndrome in Parkinson's disease. Eur. J. Radiol. 67, 550 (2008).
Schott, G. D. Pain in Parkinson's disease. Pain 22, 407–411 (1985).
Klit, H., Finnerup, N. B. & Jensen, T. S. Central post-stroke pain: clinical characteristics, pathophysiology, and management. Lancet Neurol. 8, 857–868 (2009).
Koller, W. C. When does Parkinson's disease begin? Neurology 42, 27–31 (1992).
Calne, D. B. & Stoessl, A. J. Early parkinsonism. Clin. Neuropharmacol. 9 (Suppl. 2), S3–S8 (1986).
Ondo, W. G., Vuong, K. D. & Jankovic, J. Exploring the relationship between Parkinson disease and restless legs syndrome. Arch Neurol 59, 421–424 (2002).
King, S. A. Pain in depression and Parkinson's disease. Am. J. Psychiatry 150, 353–354 (1993).
Cummings, J. L. & Masterman, D. L. Depression in patients with Parkinson's disease. Int. J. Geriatr. Psychiatry 14, 711–718 (1999).
Starkstein, S. E., Preziosi, T. J. & Robinson, R. G. Sleep disorders, pain, and depression in Parkinson's disease. Eur. Neurol. 31, 352–355 (1991).
Schrag, A., Jahanshahi, M. & Quinn, N. How does Parkinson's disease affect quality of life? A comparison with quality of life in the general population. Mov. Disord. 15, 1112–1118 (2000).
Trenkwalder, C. et al. Rotigotine effects on early morning motor function and sleep in Parkinson's disease: a double-blind, randomized, placebo-controlled study (RECOVER). Mov. Disord. 26, 90–99 (2011).
Horstink, M. et al. Review of the therapeutic management of Parkinson's disease. Report of a joint task force of the European Federation of Neurological Societies (EFNS) and the Movement Disorder Society-European Section (MDS-ES). Part II: late (complicated) Parkinson's disease. Eur. J. Neurol. 13, 1186–1202 (2006).
Horstink, M. et al. Review of the therapeutic management of Parkinson's disease. Report of a joint task force of the European Federation of Neurological Societies and the Movement Disorder Society-European Section. Part I: early (uncomplicated) Parkinson's disease. Eur. J. Neurol. 13, 1170–1185 (2006).
Kim, H. J. et al. Chronic subthalamic deep brain stimulation improves pain in Parkinson disease. J. Neurol. 255, 1889–1894 (2008).
Deuschl, G. et al. A randomized trial of deep-brain stimulation for Parkinson's disease. N. Engl. J. Med. 355, 896–908 (2006).
Deuschl, G. et al. Deep brain stimulation: postoperative issues. Mov. Disord. 21 (Suppl. 14), S219–S237 (2006).
Loher, T. J., Burgunder, J. M., Weber, S., Sommerhalder, R. & Krauss, J. K. Effect of chronic pallidal deep brain stimulation on off period dystonia and sensory symptoms in advanced Parkinson's disease. J. Neurol. Neurosurg. Psychiatry 73, 395–399 (2002).
Finnerup, N. B., Sindrup, S. H. & Jensen, T. S. The evidence for pharmacological treatment of neuropathic pain. Pain 150, 573–581 (2010).
Olson, W. L., Gruenthal, M., Mueller, M. E. & Olson, W. H. Gabapentin for parkinsonism: a double-blind, placebo-controlled, crossover trial. Am. J. Med. 102, 60–66 (1997).
Van Blercom, N. et al. Effects of gabapentin on the motor response to levodopa: a double-blind, placebo-controlled, crossover study in patients with complicated Parkinson disease. Clin. Neuropharmacol. 27, 124–128 (2004).
Miyasaki, J. M. et al. Practice Parameter: evaluation and treatment of depression, psychosis, and dementia in Parkinson disease (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 66, 996–1002 (2006).
Rowbotham, M. C., Goli, V., Kunz, N. R. & Lei, D. Venlafaxine extended release in the treatment of painful diabetic neuropathy: a double-blind, placebo-controlled study. Pain 110, 697–706 (2004).
Djaldetti, R., Yust-Katz, S., Kolianov, V., Melamed, E. & Dabby, R. The effect of duloxetine on primary pain symptoms in Parkinson disease. Clin. Neuropharmacol. 30, 201–205 (2007).
Berg, D., Becker, G. & Reiners, K. Reduction of dyskinesia and induction of akinesia induced by morphine in two parkinsonian patients with severe sciatica. J. Neural Transm. 106, 725–728 (1999).
Eichhorn, T. E. & Oertel, W. H. Macrogol 3350/electrolyte improves constipation in Parkinson's disease and multiple system atrophy. Mov. Disord. 16, 1176–1177 (2001).
Ondo, W., Romanyshyn, J., Vuong, K. D. & Lai, D. Long-term treatment of restless legs syndrome with dopamine agonists. Arch. Neurol. 61, 1393–1397 (2004).
Hening, W. A., Allen, R. P., Earley, C. J., Picchietti, D. L. & Silber, M. H. An update on the dopaminergic treatment of restless legs syndrome and periodic limb movement disorder. Sleep 27, 560–583 (2004).
Reuter, I., Ellis, C. M. & Ray Chaudhuri, K. Nocturnal subcutaneous apomorphine infusion in Parkinson's disease and restless legs syndrome. Acta Neurol. Scand. 100, 163–167 (1999).
Ondo, W. G. Methadone for refractory restless legs syndrome. Mov. Disord. 20, 345–348 (2005).
Wetter, T. C., Winkelmann, J. & Eisensehr, I. Current treatment options for restless legs syndrome. Expert Opin. Pharmacother. 4, 1727–1738 (2003).
Chaudhuri, K. R. & Martinez-Martin, P. Quantitation of non-motor symptoms in Parkinson's disease. Eur. J. Neurol. 15 (Suppl. 2), 2–7 (2008).
Siddall, P. J., Yezierski, R. P. & Loeser, J. D. Taxonomy and epidemiology of spinal cord injury pain in Progress in Pain Research and Management, Vol. 23, Spinal Cord Injury Pain: Assessment, Mechanisms, Management (eds Yezierski, R. P. & Burchiel, K.) 9–24 (IASP Press, Seattle, 2002).
Stanton-Hicks, M. et al. Reflex sympathetic dystrophy: changing concepts and taxonomy. Pain 63, 127–133 (1995).
Acknowledgements
The authors' research is supported by the National Health and Medical Research Council of Australia (NHMRC), the German Research Council (SFB 855), the EFIC-Grünenthal-Grant (EGG) and the Ministry for Science and Education of Schleswig-Holstein.
Author information
Authors and Affiliations
Contributions
Both authors contributed to all aspects of this manuscript.
Corresponding author
Ethics declarations
Competing interests
G. Wasner is on the Speakers Bureau for Astellas, Grünenthal, Medtronic, Mundipharma and Pfizer. He is a consultant for Astellas and Amgen and has received research support from Grünenthal. G. Deuschl has received lecture fees from Orion, Lundbeck, Pfizer and Teva and is serving as a consultant for Teva. He has received royalties from Thieme publishers. He is a government employee and receives grant support from the German Research Council, the German Ministry of Education and Health and Medtronic.
Rights and permissions
About this article
Cite this article
Wasner, G., Deuschl, G. Pains in Parkinson disease—many syndromes under one umbrella. Nat Rev Neurol 8, 284–294 (2012). https://doi.org/10.1038/nrneurol.2012.54
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneurol.2012.54
This article is cited by
-
Axial postural abnormalities and pain in Parkinson’s disease
Journal of Neural Transmission (2023)
-
Data-driven subtyping of Parkinson’s disease: comparison of current methodologies and application to the Bochum PNS cohort
Journal of Neural Transmission (2023)
-
Effects of safinamide on non-motor, cognitive, and behavioral symptoms in fluctuating Parkinson’s disease patients: a prospective longitudinal study
Neurological Sciences (2022)
-
Die neue Parkinson-Schmerzklassifikation (PSK)
Der Nervenarzt (2022)
-
Translation, adaptation and validation of the Bulgarian version of the King’s Parkinson’s Disease Pain Scale
BMC Neurology (2021)