Abstract
The pathophysiology of cerebral ischemia in the borderzones between the large cerebral arteries has been the topic of considerable debate since this disease entity was defined in the first half of the twentieth century. Hemodynamic failure and microembolization were two seemingly mutually exclusive pathophysiological concepts that were proposed to explain the phenomenon of borderzone infarction in patients with arterial occlusive disease. Sufficient evidence has now accumulated, however, to indicate that borderzone infarcts are in fact caused by an interaction between hypoperfusion and microembolization. In this Review, we summarize the historical background of borderzone infarction and current knowledge regarding the various possible pathophysiological concepts. We present a representative survey of publications from the 1950s to the present day, starting with early autopsy-based studies, followed by later anatomical and in vitro studies, as well as CT-based and MRI-based investigations. The clinical symptoms of borderzone infarction and the possibility of a clinical distinction between borderzone and territorial infarcts are discussed. In addition, we consider techniques to localize hemodynamic risk zones in patients with arterial occlusive disease, such as perfusion-weighted MRI, and techniques to identify a hemodynamic component of stroke, such as investigation of the cerebrovascular reserve capacity with transcranial Doppler ultrasound.
Key Points
-
First described in the 1950s, borderzone infarcts located at the edges of vascular territories of the large cerebral arteries are a common infarction pattern in patients with occlusive artery disease or hemodynamic failure
-
Borderzone infarcts can be subdivided into cortical and internal borderzone infarcts; the prevalence of cortical borderzone infarcts varies from 4.7 to 7.9% among all cerebral infarcts, whereas the prevalence of internal borderzone infarcts ranges from 4.4–6%, rising to 26–41% in patients with internal carotid artery occlusive disease
-
Two seemingly distinct concepts have been proposed to explain the pathophysiology of borderzone infarcts—hemodynamic failure caused by hypoperfusion in patients with internal carotid artery occlusive disease or acute decrease of blood pressure, and arterio-arterial or cardial microembolization
-
The impaired washout concept combines hemodynamic failure and microembolization, postulating impaired clearance of microemboli as the probable underlying pathophysiology in patients with borderzone infarcts
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Bogousslavsky J and Regli F (1986) Borderzone infarctions distal to internal carotid artery occlusion: prognostic implications. Ann Neurol 20: 346–350
Bogousslavsky J (1991) Topographic patterns of cerebral infarcts. Cerebrovasc Dis 1 (Suppl 1): S61–S68
Schneider M (1953) Cerebral blood flow and oxygen supply [German]. Verh Dtsch Ges Kreislaufforsch 19: 3–12
Bladin CF et al. (1993) Confusing stroke terminology: watershed or borderzone infarction? Stroke 24: 477–478
Zülch K (1961) On the development and localization of cerebral infarctions [German]. Zentralbl Neurochir 21: 158–178
Zülch K (1960) On the development and treatment of cerebral infarctions [German]. Dtsch Med Wochenschr 85: 1524–1530
Zülch K (1960) On the development and treatment of cerebral infarctions [German]. Dtsch Med Wochenschr 85: 1585–1590
Ringelstein EB et al. (1983) The pathogenesis of strokes from internal carotid artery occlusion: diagnostic and therapeutical implications. Stroke 14: 867–875
van der Zwan A (1991) The Variability of the Major Vascular Territories of the Human Brain. The Netherlands: University of Utrecht
van der Zwan A and Hillen B (1991) Review of the variability of the territories of the major cerebral arteries. Stroke 22: 1078–1984
Hennerici M et al. (1998) Failure to identify cerebral infarct mechanisms from topography of vascular territory lesions. AJNR Am J Neuroradiol 19: 1067–1074
van der Zwan A et al. (1992) The variability of the territories of the major cerebral arteries. J Neurosurg 77: 927–942
Jorgensen L and Torvik A (1966) Ischaemic cerebrovascular diseases in an autopsy series: I prevalence, location and predisposing factors in verified thrombo-embolic occlusions, and their significance in the pathogenesis of cerebral infarction. J Neurol Sci 3: 490–509
Mounier-Vehier F et al. (1994) Borderzone infarct subtypes: preliminary study of the presumed mechanism. Eur Neurol 34: 11–15
Yong SW et al. (2006) Internal and cortical border-zone infarction: clinical and diffusion-weighted imaging features. Stroke 37: 841–846
Bladin CF and Chambers BR (1993) Clinical features, pathogenesis, and computed tomographic characteristics of internal watershed infarction. Stroke 24: 1925–1932
Del Sette M et al. (2000) Internal borderzone infarction: a marker for severe stenosis in patients with symptomatic internal carotid artery disease. For the North American Symptomatic Carotid Endarterectomy (NASCET) Group. Stroke 31: 631–636
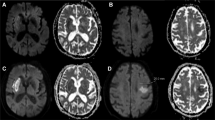
Szabo K et al. (2001) Acute stroke patterns in patients with internal carotid artery disease: a diffusion-weighted magnetic resonance imaging study. Stroke 32: 1323–1329
Meyer J (1953) Localization of brain injuries in arterial areas in early childhood [German]. Arch Psychiatr Nervenkr ZGesamte Neurol Psychiatr 190: 328–341
Meyer J (1958) Localization of arteriosclerotic foci of softening in arterial regions of the brain [German]. Arch Psychiatr Nervenkr Z Gesamte Neurol Psychiatr 196: 421–432
Brierley JB and Excell BJ (1966) The effects of profound systemic hypotension upon the brain of M. rhesus: physiological and pathological observations. Brain 89: 269–298
Adams JH et al. (1966) The effects of systemic hypotension upon the human brain: clinical and neuropathological observations in 11 cases. Brain 89: 235–268
Romanul FC and Abramovicz A (1964) Changes in brain and pial vessels in arterial border zones; a study of 13 cases. Arch Neurol 11: 40–65
Bogousslavsky J and Regli F (1986) Unilateral watershed cerebral infarcts. Neurology 36: 373–377
Bladin CF and Chambers BR (1994) Frequency and pathogenesis of hemodynamic stroke. Stroke 25: 2179–2182
Waterston JA et al. (1990) Small deep cerebral infarcts associated with occlusive internal carotid artery disease: a hemodynamic phenomenon? Arch Neurol 47: 953–957
Hennerici M et al. (1987) Natural history of asymptomatic extracranial arterial disease: results of a long-term prospective study. Brain 110: 777–791
Hupperts RM (1997) Severe stenosis of the internal carotid artery is not associated with borderzone infarcts in patients randomised in the European Carotid Surgery Trial. J Neurol 244: 45–50
Weiller C et al. (1991) Clinical and hemodynamic aspects of low-flow infarcts. Stroke 22: 1117–1123
Kumral E et al. (2004) Mechanisms of single and multiple borderzone infarct: transcranial Doppler ultrasound/magnetic resonance imaging correlates. Cerebrovasc Dis 17: 287–295
Kim SJ et al. (2006) Acute-stage evolution of watershed infarction assessed on diffusion-weighted MR imaging. Cerebrovasc Dis 21: 357–362
Hendrikse J et al. (2002) Magnetic resonance angiography of collateral compensation in asymptomatic and symptomatic internal carotid artery stenosis. J Vasc Surg 36: 799–805
Hendrikse J (2001) Collateral ability of the circle of Willis in patients with unilateral internal carotid artery occlusion: border zone infarcts and clinical symptoms. Stroke 32: 2768–2773
Hartkamp MJ et al. (1999) Circle of Willis collateral flow investigated by magnetic resonance angiography. Stroke 30: 2671–2678
Patel MR et al. (1995) Preoperative assessment of the carotid bifurcation: can magnetic resonance angiography and duplex ultrasonography replace contrast arteriography? Stroke 26: 1753–1758
Angeloni U et al. (1990) Internal borderzone infarction following acute middle cerebral artery occlusion. Neurology 40: 1196–1198
Wong KS et al. (2002) Mechanisms of acute cerebral infarctions in patients with middle cerebral artery stenosis: a diffusion-weighted imaging and microemboli monitoring study. Ann Neurol 52: 74–81
Torvik A and Skullerud K (1982) Watershed infarcts in the brain caused by microemboli. Clin Neuropathol 1: 99–105
Pollanen MS and Deck JH (1989) Directed embolization is an alternate cause of cerebral watershed infarction. Arch Pathol Lab Med 113: 1139–1141
Pollanen MS and Deck JH (1990) The mechanism of embolic watershed infarction: experimental studies. Can J Neurol Sci 17: 395–398
Belden JR et al. (1999) Mechanisms and clinical features of posterior border-zone infarcts. Neurology 53: 1312–1318
Caplan LR and Hennerici M (1998) Impaired clearance of emboli (washout) is an important link between hypoperfusion, embolism, and ischemic stroke. Arch Neurol 55: 1475–1482
Caplan LR et al. (2006) Is hypoperfusion an important cause of strokes? If so, how? Cerebrovasc Dis 21: 145–153
Sedlaczek O et al. (2005) Impaired washout—embolism and ischemic stroke: further examples and proof of concept. Cerebrovasc Dis 19: 396–401
Gottesman RF et al. (2006) Watershed strokes after cardiac surgery: diagnosis, etiology and outcome. Stroke 37: 2306–2311
Wityk RJ et al. (2007) Diffusion- and perfusion-weighted brain magnetic resonance imaging in patients with neurologic complications after cardiac surgery. Arch Neurol 58: 571–576
Fisher M and McQuillen JB (1981) Bilateral cortical border-zone infarction: a pseudobrainstem stroke. Arch Neurol 38: 62–63
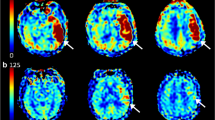
Chaves CJ et al. (2000) Diffusion- and perfusion-weighted MRI patterns in borderzone infarcts. Stroke 31: 1090–109649
Maeda H et al. (1993) Reactivity of cerebral blood flow to carbon dioxide in various types of ischemic cerebrovascular disease: evaluation by the transcranial Doppler method. Stroke 24: 670–675
Wiart M et al. (2000) Vasodilatory response of border zones to acetazolamide before and after endarterectomy: an echo planar imaging-dynamic susceptibility contrast-enhanced MRI study in patients with high-grade unilateral internal carotid artery stenosis. Stroke 31: 1561–1565
Bisschops RH et al. (2003) Association between impaired carbon dioxide reactivity and ischemic lesions in arterial border zone territories in patients with unilateral internal carotid artery occlusion. Arch Neurol 60: 229–233
Ackerstaff RG et al. (1995) The significance of microemboli detection by means of transcranial Doppler ultrasonography monitoring in carotid endarterectomy. J Vasc Surg 21: 963–969
Ackerstaff RG et al. (1997) Reliability in the identification of Doppler embolic transient signals: a statistical problem? Stroke 28: 876
Gandolfo C et al. (1998) Internal borderzone infarction in patients with ischemic stroke. Cerebrovasc Dis 8: 255–258
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Förster, A., Szabo, K. & Hennerici, M. Mechanisms of Disease: pathophysiological concepts of stroke in hemodynamic risk zones—do hypoperfusion and embolism interact?. Nat Rev Neurol 4, 216–225 (2008). https://doi.org/10.1038/ncpneuro0752
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ncpneuro0752
This article is cited by
-
Transient ischemic attack and minor stroke as “surgeons affairs”: a narrative review
Neurological Sciences (2023)
-
Cerebral vasomotor reactivity in border zone infarcts; a transcranial Doppler study
The Egyptian Journal of Neurology, Psychiatry and Neurosurgery (2019)
-
Cerebral border zone infarction: an etiological study
The Egyptian Journal of Neurology, Psychiatry and Neurosurgery (2018)
-
A Rich-Club Organization in Brain Ischemia Protein Interaction Network
Scientific Reports (2015)