Abstract
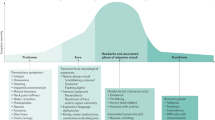
Migraine is a common disabling brain disorder that—considering its clinical and economic impact—is understudied and in need of additional management options. Currently, treatments are classified as preventive or acute-attack therapies, although it is expected that this distinction will become blurred over time. The gap-junction blocker tonabersat, an inducible nitric oxide synthase (NOS) inhibitor and botulinum toxin A are all being investigated in clinical trials as preventive therapies. Device-based approaches using neurostimulation of the occipital nerve have provided promising results, whereas the first study of patent foramen ovale closure for migraine prevention produced disappointing results. Calcitonin gene-related peptide receptor antagonists, vanilloid TRPV1 receptor antagonists and NOS inhibitors are all being investigated in clinical trials for acute migraine. There is much cause for optimism in this area of neurology and considerable benefit awaits our patients.
Key Points
-
Migraine is a common, disabling, inherited brain disorder that affects 12% of the US population; it is treated with medicines described as being either preventive or acute-attack therapies
-
Preventive medicines currently in development include the gap-junction blocker tonabersat, an inducible nitric oxide synthase inhibitor and botulinum toxin A; the first study of patent foramen ovale closure for migraine prevention failed; neurostimulation of the occipital nerve is currently being explored as an alternative device-based preventive approach
-
For acute-attack treatment two calcitonin gene-related peptide receptor antagonists have now been studied, and both were effective in the treatment of acute migraine
-
Vanilloid TRPV1 receptor antagonists, nitric oxide synthase inhibitors and serotonin receptor 5-HT1F agonists are all being investigated in clinical trials for acute migraine, each of which is exploring a new mechanism of action and offering the possibility of avoiding the cardiovascular side effects that limit the use of triptans
-
The future of neurological therapeutics seems bright and no more so than in the field of migraine where neuroscience and clinical neurology practice meet to advance the management of our patients
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Goadsby PJ et al. (2002) Migraine—current understanding and treatment. N Engl J Med 346: 257–270
Stewart WF et al. (2003) Lost productive time and cost due to common pain conditions in the US workforce. JAMA 290: 2443–2454
Andlin-Sobocki P et al. (2005) Cost of disorders of the brain in Europe. Eur J Neurol 12 (Suppl 1): 1–27
Lipton RB et al. (2001) Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache 41: 646–657
Lipton RB et al. (2007) Migraine prevalence, disease burden, and the need for preventive therapy. Neurology 68: 343–349
Lance JW and Goadsby PJ (2005) Mechanism and Management of Headache, edn 7. New York: Elsevier
Ferrari MD et al. (2001) Oral triptans (serotonin, 5-HT1B/1D agonists) in acute migraine treatment: a meta-analysis of 53 trials. Lancet 358: 1668–1675
Dodick D et al. (2004) Consensus statement: cardiovascular safety profile of triptans (5-HT1B/1D agonists) in the acute treatment of migraine. Headache 44: 414–425
Goadsby PJ (2006) Migraine pathophysiology. In Encyclopedic Reference of Pain, 1148–1155 (Eds Schmidt RF and Willis WD) Berlin: Springer
Burstein R and Jakubowski M (2005) Unitary hypothesis for multiple triggers of the pain and strain of migraine. J Comp Neurol 493: 9–14
Hoskin KL et al. (1996) Central activation of the trigeminovascular pathway in the cat is inhibited by dihydroergotamine: a c-Fos and electrophysiology study. Brain 119: 249–256
Hoskin KL et al. (1996) Sumatriptan can inhibit trigeminal afferents by an exclusively neural mechanism. Brain 119: 1419–1428
Moskowitz MA and Cutrer FM (1993) Sumatriptan: a receptor-targeted treatment for migraine. Annu Rev Med 44: 145–154
Peroutka SJ (2005) Neurogenic inflammation and migraine: implications for therapeutics. Mol Interv 5: 306–313
Ferrari MD et al. (2007) Migraine as a cerebral ionopathy with impaired central sensory processing. In Molecular Neurology, 439–461 (Ed. Waxman SG) London: Elsevier
Afridi SK and Goadsby PJ (2006) Neuroimaging of migraine. Curr Pain Headache Rep 10: 221–224
Hadjikhani N et al. (2001) Mechanisms of migraine aura revealed by functional MRI in human visual cortex. Proc Nat Acad Sci USA 98: 4687–4692
Matharu MS et al. (2004) Central neuromodulation in chronic migraine patients with suboccipital stimulators: a PET study. Brain 127: 220–230
Goadsby PJ (2005) Can we develop neurally-acting drugs for the treatment of migraine? Nat Rev Drug Discov 4: 741–750
Leao AAP (1944) Spreading depression of activity in cerebral cortex. J Neurophysiol 7: 359–390
Lauritzen M (1994) Pathophysiology of the migraine aura: the spreading depression theory. Brain 117: 199–210
Ayata C et al. (2006) Suppression of cortical spreading depression in migraine prophylaxis. Ann Neurol 59: 652–661
Goadsby PJ (2001) Migraine, aura and cortical spreading depression: why are we still talking about it? Ann Neurol 49: 4–6
Brennan KC et al. (2007) Distinct vascular conduction with cortical spreading depression. J Neurophysiol 97: 4143–4151
Read SJ et al. (1999) SB-220453, a potential novel antimigraine compound, inhibits nitric oxide release following induction of cortical spreading depression in the anaesthetized cat. Cephalalgia 20: 92–99
Smith MI et al. (2000) Repetitive cortical spreading depression in a gyrencephalic feline brain: inhibition by the novel benzoylamino-benzopyran SB-220453. Cephalalgia 20: 546–553
MaassenVanDenBrink A et al. (2000) The potential anti-migraine compound SB-220453 does not contract human isolated blood vessels or myocardium; a comparison with sumatriptan. Cephalalgia 20: 538–545
Parsons AA et al. (2001) Tonabersat (SB-220453) a novel benzopyran with anticonvulsant properties attenuates trigeminal nerve-induced neurovascular reflexes. Br J Pharmacol 132: 1549–1557
Tvedskov JF et al. (2004) A double-blind study of SB-220453 (Tonerbasat) in the glyceryltrinitrate (GTN) model of migraine. Cephalalgia 24: 875–882
Tvedskov JF et al. (2004) The effect of propranolol on glyceryltrinitrate-induced headache and arterial response. Cephalalgia 24: 1076–1087
Goadsby PJ et al. Double-blind placebo-controlled trial of tonabersat in the preventive management of migraine. Cephalalgia, in press
Simpson LL (1981) The origin, structure, and pharmacological activity of botulinum toxin. Pharmacol Rev 33: 155–188
Jankovic J (2004) Botulinum toxin in clinical practice. J Neurol Neurosurg Psychiat 75: 951–957
Cui M et al. (2004) Subcutaneous administration of botulinum toxin A reduces formalin-induced pain. Pain 107: 125–133
Aoki KR (2005) Review of a proposed mechanism for the antinociceptive action of botulinum toxin type A. Neurotoxicology 26: 785–793
Evers S et al. (2002) Treatment of headache with botulinum toxin A—a review according to evidence-based medicine criteria. Cephalalgia 22: 699–710
Silberstein SD et al. (2006) Botulinum toxin type A in the prophylactic treatment of chronic tension-type headache: a multicentre, double-blind, randomized, placebo-controlled, parallel-group study. Cephalalgia 26: 790–800
Silberstein S et al. (2000) Botulinum toxin type A as a migraine preventive treatment: for the BOTOX Migraine Clinical Research Group. Headache 40: 445–450
Brin MF et al. (2000) Botox for migraine: double-blind, placebo-controlled, region-specific evaluation. Cephalalgia 20: 421–422
Evers S et al. (2004) Botulinum toxin A in the prophylactic treatment of migraine—a randomized, double-blind, placebo-controlled study. Cephalalgia 24: 838–843
Relja M et al. (2005) A multicentre, double-blind, randomised, placebo-controlled, parallel group study of multiple treatments of botulinum toxin type A (BoNTA) for the prophylaxis of migraine headaches. J Neurol 252 (Suppl 2): ii62
Saper JR et al. (2005) A double-blind, randomised, placebo-controlled exploratory study comparing injection sites with low doses of botulinum toxin type A in the prevention of episodic migraine. J Neurol 252 (Suppl 2): ii58
Chankrachang S et al. (2005) Botulinum toxin type A in migraine without aura prophylaxis; a 12-week prospective, multicentre, double-blind, randomized, placebo-controlled trial. Cephalalgia 25: 992–993
Olesen J et al. (2006) New appendix criteria open for a broader concept of chronic migraine. Cephalalgia 26: 742–746
Silberstein SD et al. (2005) Botulinum toxin type A for the prophylactic treatment of chronic daily headache: a randomized, double-blind, placebo-controlled trial. Mayo Clin Proc 80: 1126–1137
Mathew NT et al. (2005) Botulinum toxin type A (BOTOX) for the prophylactic treatment of chronic daily headache: a randomized, double-blind, placebo-controlled trial. Headache 45: 293–307
Dodick DW et al. (2005) Botulinum toxin type A for the prophylaxis of chronic daily headache: subgroup analysis of patients not receiving other prophylactic medications: a randomized double-blind, placebo-controlled study. Headache 45: 315–324
NCT00168428 [http://www.clinicaltrials.gov/ct/show/NCT00168428?order=1]
NCT00156910 [http://www.clinicaltrials.gov/ct/show/NCT00156910?order=1]
Goadsby PJ et al. (2006) Towards a definition of intractable headache for use in clinical practice and trials. Cephalalgia 26: 1168–1170
Schulman EA et al. (2007) Defining refractory migraine and chronic migraine: proposed diagnostic criteria from the refractory migraine special interest section (RHSIS) of AHS [abstract]. Headache 47: 747
Thompson T and Evans W (1930) Paradoxical embolism. Q J Med 23: 135–152
Hagen PT et al. (1984) Incidence and size of patent foramen ovale during the first 10 decades of life: an autopsy study of 965 normal hearts. Mayo Clin Proc 59: 17–20
Anzola GP et al. (1999) Potential source of cerebral embolism in migraine with aura: a transcranial Doppler study. Neurology 52: 1622–1625
Wilmshurst P et al. (2005) Re-evaluation of the relationship between migraine and persistent foramen ovale and other right-to-left shunts. Clin Sci 108: 365–367
Wilmshurst P and Nightingale S (2001) Relationship between migraine and cardiac and pulmonary right-to-left shunts. Clin Sci 100: 215–220
Wilmshurst PT et al. (2000) Effect on migraine of closure of cardiac right-to-left shunts to prevent recurrence of decompression illness or stroke or for haemodynamic reasons. Lancet 356: 1648–1651
Dowson AJ et al. (2005) A propsective, multicentre, double-blind, placebo-controlled study to evaluate the efficacy of patent foramen ovale closure for the resolution of refractory migraine headache (the MIST Study): prevalence and size of shunts. Headache Care 2: 223–227
Dowson A et al. (2006) A prospective, multicenter, randomized, double-blind, placebo-controlled trial to evaluate the efficacy of patent foramen ovale closure with the StarFlex septal repair implant to prevent refractory migraine headaches: the MIST trial. Presented at the 55th Annual Scientific Session of the American College of Cardiology: 2006 March 11–14, Atlanta, GA, USA
ISRCTN45687883 [http://www.controlled-trials.com/ISRCTN45687883/ISRCTN45687883]
Kruit MC et al. (2004) Migraine as a risk factor for subclinical brain lesions. J Am Med Assoc 291: 427–434
Schoenen J et al. (2007) Prevalence of patent foramen ovale and MRI white matter lesions in migraine with aura. Cephalalgia 27: 578
Rozen TD (2007) Vanishing cerebellar infarcts in a migraine patient. Cephalalgia 27: 557–560
Weiner RL and Reed KL (1999) Peripheral neurostimulation for control of intractable occipital neuralgia. Neuromodulation 2: 217–221
Dodick DW et al. (2003) Occipital nerve stimulation for intractable chronic primary headache disorders. Cephalalgia 23: 701
Burns B et al. (2007) Successful treatment of medically intractable cluster headache using occipital nerve stimulation (ONS). Lancet 369: 1099–1106
Magis D et al. (2007) Occipital nerve stimulation for drug-resistant chronic cluster headache: a prospective pilot study. Lancet Neurol 6: 314–321
Edvinsson L et al. (1987) Calcitonin gene-related peptide and cerebral blood vessels: distribution and vasomotor effects. J Cereb Blood Flow Metab 7: 720–728
Goadsby PJ (2005) Calcitonin gene-related peptide antagonists as treatments of migraine and other primary headaches. Drugs 65: 2557–2567
Zhang Z et al. (2007) Sensitization of calcitonin gene-related peptide receptors by receptor activity-modifying protein-1 in the trigeminal ganglion. J Neurosci 27: 2693–2703
Goadsby PJ et al. (1988) Release of vasoactive peptides in the extracerebral circulation of man and the cat during activation of the trigeminovascular system. Ann Neurol 23: 193–196
Goadsby PJ et al. (1990) Vasoactive peptide release in the extracerebral circulation of humans during migraine headache. Ann Neurol 28: 183–187
Gallai V et al. (1995) Vasoactive peptides levels in the plasma of young migraine patients with and without aura assessed both interictally and ictally. Cephalalgia 15: 384–390
Goadsby PJ and Edvinsson L (1993) The trigeminovascular system and migraine: studies characterizing cerebrovascular and neuropeptide changes seen in humans and cats. Ann Neurol 33: 48–56
Goadsby PJ and Edvinsson L (1994) Human in vivo evidence for trigeminovascular activation in cluster headache. Brain 117: 427–434
Fanciullacci M et al. (1995) Increase in plasma calcitonin gene-related peptide from extracerebral circulation during nitroglycerin-induced cluster headache attack. Pain 60: 119–123
Durham PL et al. (1997) Repression of the calcitonin gene-related peptide promoter by 5-HT1 receptor activation. J Neurosci 17: 9545–9553
Durham PL and Russo AF (1999) Regulation of calcitonin gene-related peptide secretion by a serotonergic antimigraine drug. J Neurosci 19: 3423–3429
May A and Goadsby PJ (2001) Substance P receptor antagonists in the therapy of migraine. Expert Opin Investig Drugs 10: 1–6
Feindel W et al. (1960) The tentorial nerves and localization of intracranial pain in man. Neurology 10: 555–563
Zagami AS et al. (1990) Stimulation of the superior sagittal sinus in the cat causes release of vasoactive peptides. Neuropeptides 16: 69–75
Knight YE et al. (1999) Blockade of CGRP release after superior sagittal sinus stimulation in cat: a comparison of avitriptan and CP122,288. Neuropeptides 33: 41–46
Knight YE et al. (2001) 4991W93 inhibits release of calcitonin gene-related peptide in the cat but only at doses with 5HT1B/1D receptor agonist activity. Neuropharmacology 40: 520–525
Bellamy J et al. (2006) Nitric oxide regulation of calcitonin gene-related peptide gene expression in rat trigeminal ganglia neurons. Eur J Neurosci 23: 2057–2066
Doods H et al. (2000) Pharmacological profile of BIBN4096BS, the first selective small molecule CGRP antagonist. Br J Pharmacol 129: 420–423
Moreno MJ et al. (2002) Efficacy of the non-peptide CGRP receptor antagonist BIBN4096BS in blocking CGRP-induced dilations in human and bovine cerebral arteries: potential implications in acute migraine treatment. Neuropharmacology 42: 568–576
Petersen KA et al. (2003) The effect of the nonpeptide CGRP-antagonist, BIBN406BS on human-alphaCGRP induced headache and hemodynamics in healthy volunteers. Cephalalgia 23: 725
Storer RJ et al. (2004) Calcitonin gene-related peptide (CGRP) modulates nociceptive trigeminovascular transmission in the cat. Br J Pharmacol 142: 1171–1181
Fischer MJ et al. (2005) The nonpeptide calcitonin gene-related peptide receptor antagonist BIBN4096BS lowers the activity of neurons with meningeal input in the rat spinal trigeminal nucleus. J Neurosci 25: 5877–5883
Olesen J et al. (2004) Calcitonin gene-related peptide (CGRP) receptor antagonist BIBN4096BS for the acute treatment of migraine. N Engl J Med 350: 1104–1110
Petersen KA et al. (2003) The novel CGRP-antagonist, BIBN4096BS does not affect the cerebral hemodynamics in healthy volunteers. Cephalalgia 23: 729
Williams TM et al. (2006) Non-peptide calcitonin gene-related peptide receptor antagonists from a benzodiazepinone lead. Bioorg Med Chem Lett 16: 2595–2598
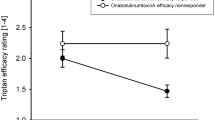
Ho T et al. (2007) Efficacy and tolerability of a novel, oral CGRP antagonist, MK-0974, in the acute treatment of migraine. Cephalalgia 27: 759
Powell KJ et al. (2000) Blockade and reversal of spinal morphine tolerance by peptide and non-peptide calcitonin gene-related peptide receptor antagonists. Br J Pharmacol 131: 875–884
Guo A et al. (1999) Immunocytochemical localization of the vanilloid receptor 1 (VR1): relationship to neuropeptides, the P2X3 purinoceptor and IB4 binding sites. Eur J Neurosci 11: 946–958
Ichikawa H and Sugimoto T (2001) VR1-immunoreactive primary sensory neurons in the rat trigeminal ganglion. Brain Res 890: 184–188
Markowitz S et al. (1987) Neurogenically mediated leakage of plasma proteins occurs from blood vessels in dura mater but not brain. J Neurosci 7: 4129–4136
Hou M et al. (2002) Capsaicin receptor immunoreactivity in the human trigeminal ganglion. Neurosci Lett 330: 223–226
Akerman S et al. (2003) Vanilloid type 1 receptor (VR1) evoked CGRP release plays a minor role in causing dural vessel dilation via the trigeminovascular system. Br J Pharmacol 140: 718–724
Williamson DJ et al. (1997) Sumatriptan inhibits neurogenic vasodilation of dural blood vessels in the anaesthetized rat—intravital microscope studies. Cephalalgia 17: 525–531
Williamson DJ et al. (1997) Intravital microscope studies on the effects of neurokinin agonists and calcitonin gene-related peptide on dural blood vessel diameter in the anaesthetized rat. Cephalalgia 17: 518–524
Shepheard SL et al. (1997) Differential effects of 5-HT1B/1D receptor agonists on neurogenic dural plasma extravasation and vasodilation in anaesthetized rats. Neuropharmacology 36: 525–533
Williamson DJ et al. (1997) The novel anti-migraine agent rizatriptan inhibits neurogenic dural vasodilation and extravasation. Eur J Pharmacol 328: 61–64
Rami HK et al. (2006) Discovery of SB-705498: A potent, selective and orally bioavailable TRPV1 antagonist suitable for clinical development. Bioorg Med Chem Lett 16: 3287–3291
NCT00269022 [http://www.clinicaltrials.gov/ct/show/NCT00269022?order=1]
Thomsen LL and Olesen J (2001) Nitric oxide in primary headaches. Curr Opin Neurol 14: 315–321
Olesen J et al. (1995) The nitric oxide hypothesis of migraine and other vascular headaches. Cephalalgia 15: 94–100
Iversen HK et al. (1989) Intravenous nitroglycerin as an experimental headache model: basic characteristics. Pain 38: 17–24
Afridi S et al. (2004) Glyceryl trinitrate triggers premonitory symptoms in migraineurs. Pain 110: 675–680
Giffin NJ et al. (2003) Premonitory symptoms in migraine: an electronic diary study. Neurology 60: 935–940
Kruuse C et al. (2003) Migraine can be induced by sildenafil without changes in middle cerebral artery diameter. Brain 126: 241–247
Hansen JM et al. (2006) Vasoactive intestinal polypeptide evokes only a minimal headache in healthy volunteers. Cephalalgia 26: 992–1003
Rahmann A et al. (2007) Vasoactive intestinal peptide causea marked cephalic vasodilatation but does not induce migraine. Cephalalgia 27: 615
Reuter U et al. (2001) Delayed inflammation in rat meninges: implications for migraine pathophysiology. Brain 124: 2490–2502
Hoskin KL et al. (1999) Fos expression in the trigeminocervical complex of the cat after stimulation of the superior sagittal sinus is reduced by L-NAME. Neurosci Lett 266: 173–176
De Alba J et al. (2006) GW274150, a novel and highly selective inhibitor of the inducible isoform of nitric oxide synthase (iNOS), shows analgesic effects in rat models of inflammatory and neuropathic pain. Pain 120: 170–181
Bergerot A et al. (2006) Animal models of migraine: looking at the component parts of a complex disorder. Eur J Neurosci 24: 1517–1534
Lassen LH et al. (1997) Nitric oxide synthesis inhibition in migraine. Lancet 349: 401–402
Alderton WK et al. (2005) GW274150 and GW273629 are potent and highly selective inhibitors of inducible nitric oxide synthase in vitro and in vivo. Br J Pharmacol 145: 301–312
NCT00319137 [http://www.clinicaltrials.gov/ct/show/NCT00319137?order=1]
Hall DB et al. (2000) A group sequential adaptive treatment assignment design for proof of concept and dose selection in headache trials. Contemp Clin Trials 26: 349–364
NCT00242866 [http://www.clinicaltrials.gov/ct/show/NCT00242866?order=1]
Goadsby PJ (2000) The pharmacology of headache. Prog Neurobiol 62: 509–525
Castro ME et al. (1997) Differential distribution of [3H]sumatriptan binding sites (5-HT1B, 5-HT1D and 5-HT1F receptors) in human brain: focus on brainstem and spinal cord. Neuropharmacology 36: 535–542
Pascual J et al. (1996) [3H] Sumatriptan binding sites in human brain: regional-dependent labelling of 5HT1D and 5HT1F receptors. Eur J Pharmacol 295: 271–274
Waeber C and Moskowitz MA (1995) [3H]sumatriptan labels both 5-HT1D and 5HT1F receptor bindings sites in the guinea pig brain: an autoradiographic study. Naunyn Schmiedebergs Arch Pharmacol 352: 263–275
Fugelli A et al. (1997) Autoradiographic localization of 5-HT1E and 5-HT1F binding sites in rat brain: effect of serotonergic lesioning. J Recept Signal Transduct Res 17: 631–645
Bouchelet I et al. (1996) Differential expression of sumatriptan-sensitive 5-hydroxytryptamine receptors in human trigeminal ganglia and cerebral blood vessels. Mol Pharmacol 50: 219–223
Maneesi S et al. (2004) Electron microsopic demonstration of pre- and postsynaptic 5-HT1D and 5-HT1F receptor immunoreactivity (IR) in the rat trigeminocervical complex (TCC) new therapeutic possibilities for the triptans. Cephalalgia 24: 148
Mitsikostas DD et al. (1999) Both 5-HT1B and 5-HT1F receptors modulate c-fos expression within rat trigeminal nucleus caudalis. Eur J Pharmacol 369: 271–277
Goadsby PJ and Classey JD (2003) Evidence for 5-HT1B, 5-HT1D and 5-HT1F receptor inhibitory effects on trigeminal neurons with craniovascular input. Neuroscience 122: 491–498
Cohen ML and Schenck K (1999) 5-Hydroxytryptamine1F receptors do not participate in vasoconstriction: lack of vasoconstriction to LY344864, a selective serotonin1F receptor agonist in rabbit saphenous vein. J Pharmacol Exp Ther 290: 935–939
Razzaque Z et al. (1999) Vasoconstriction in human isolated middle meningeal arteries: determining the contribution of 5-HT1B- and 5-HT1F-receptor activation. Br J Clin Pharmacol 47: 75–82
Bouchelet I et al. (2000) No contractile effect for 5-HT1D and 5-HT1F receptor agonists in human and bovine cerebral arteries: similarity with human coronary artery. Br J Pharmacol 129: 501–508
Phebus LA et al. (1997) Characterization of LY334370 as a pharmacological tool to study 5HT1F receptors—binding affinities, brain penetration and activity in the neurogenic dural inflammation model of migraine. Life Sci 61: 2117–2126
Goldstein DJ et al. (2001) Selective serotonin 1F (5-HT1F) receptor agonist LY334370 for acute migraine: a randomised controlled trial. Lancet 358: 1230–1234
NCT00384774 [http://www.clinicaltrials.gov/ct/show/NCT00384774?order=1]
Author information
Authors and Affiliations
Ethics declarations
Competing interests
In the last twelve months the author has been consulted by, lectured in meetings arranged by, or conducted clinical or basic science research with Advanced Bionics, Allergan, Almirall, AstraZeneca, Capnia, CoLucid, Medtronic, Minster and MSD.
Rights and permissions
About this article
Cite this article
Goadsby, P. Emerging therapies for migraine. Nat Rev Neurol 3, 610–619 (2007). https://doi.org/10.1038/ncpneuro0639
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/ncpneuro0639
This article is cited by
-
Economic Evaluation of Treatments for Migraine: An Assessment of the Generalizability Following a Systematic Review
PharmacoEconomics (2020)
-
Therapeutic strategies targeting connexins
Nature Reviews Drug Discovery (2018)
-
Typical aura without headache: a case report and review of the literature
Journal of Medical Case Reports (2015)
-
Animal Models of Chronic Migraine
Current Pain and Headache Reports (2015)
-
Acute Migraine Therapy: New Drugs and New Approaches
Current Treatment Options in Neurology (2011)