Abstract
Revascularization therapy is pivotal to saving ischemic brain from infarction. Two major randomized trials of intravenous thrombolytic therapy have established clear clinical benefit, especially for strokes caused by small-vessel occlusion. Ischemic stroke caused by large-vessel intracranial occlusion carries higher morbidity, however, and intravenous thrombolytics are less capable of opening these large vessels. This observation makes a case for delivering thrombolytics directly into the clot, or simply removing the clot mechanically. Intra-arterial thrombolytic drugs have been shown to be effective for treating middle cerebral artery occlusions in a major randomized trial. In the past 2 years, a family of mechanical thrombectomy catheters designed to remove rather than dissolve the offending clot has received FDA clearance. Such devices offer alternative therapy to patients who cannot receive thrombolytics, and can also be used in combination with thrombolytics to safely restore cerebral perfusion. Mechanical techniques have not been directly compared with intra-arterial thrombolytic strategies, but these devices might be superior to thrombolytics within vessels with particularly high clot burden, such as the carotid terminus and the basilar artery. Comprehensive stroke centers are currently available in major metropolitan areas to treat stroke via intra-arterial means, and are likely to become 'hubs' to 'spoke' hospitals that are credentialed as primary stroke centers. This design will allow any patient timely access to state-of-the-art stroke treatment tailored to their needs.
Key Points
-
Intravenous recombinant tissue plasminogen activator (rtPA) has been shown to improve outcome in patients with ischemic stroke if given within the first 3 hours, and perhaps up to 4.5 hours
-
Strokes from large-vessel intracranial occlusion carry high morbidity and respond poorly to intravenously administered thrombolytics
-
Intra-arterial thrombolytics significantly restore perfusion within intracranial large arteries, particularly the middle cerebral artery, but no drug is FDA approved for this use
-
Mechanical thrombectomy significantly restores patency in large-vessel stroke, and revascularization portends better clinical outcome
-
Mechanical thrombectomy can be safely combined with intravenous and intra-arterial thrombolytic treatments
-
The exact selection of treatment modalities is probably patient-specific, and is the subject of ongoing investigations
-
The marriage of primary and comprehensive stroke centers in the US is likely to be a viable solution to bring state-of-the-art stroke treatment to anyone with acute stroke
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Smith WS et al. (2006) Prognostic significance of angiographically confirmed large vessel intracranial occlusion in patients presenting with acute brain ischemia. Neurocrit Care 4: 14–17
Furlan A et al. (1999) Intra-arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. Prolyse in Acute Cerebral Thromboembolism. JAMA 282: 2003–2011
Hacke W et al. (1996) 'Malignant' middle cerebral artery territory infarction: clinical course and prognostic signs. Arch Neurol 53: 309–315
Christou I et al. (2002) Intravenous tissue plasminogen activator and flow improvement in acute ischemic stroke patients with internal carotid artery occlusion. J Neuroimaging 12: 119–123
Jansen O et al. (1995) Thrombolytic therapy in acute occlusion of the intracranial internal carotid artery bifurcation. AJNR Am J Neuroradiol 16: 1977–1986
Becker KJ et al. (1996) Intraarterial thrombolysis in vertebrobasilar occlusion. AJNR Am J Neuroradiol 17: 255–262
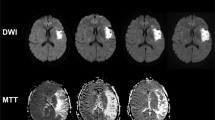
Ostrem JL et al. (2004) Acute basilar artery occlusion: diffusion–perfusion MRI characterization of tissue salvage in patients receiving intra-arterial stroke therapies. Stroke 35: e30–e34
Hacke W et al. (1988) Intra-arterial thrombolytic therapy improves outcome in patients with acute vertebrobasilar occlusive disease. Stroke 19: 1216–1222
Smith WS: Intraarterial thrombolytic therapy for acute basilar occlusion: pro. Stroke, in press
The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group (1995) Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 333: 1581–1587
Eckert B et al. (2002) Endovascular therapy of acute vertebrobasilar occlusion: early treatment onset as the most important factor. Cerebrovasc Dis 14: 42–50
Qureshi AI et al. (2004) Reocclusion of recanalized arteries during intra-arterial thrombolysis for acute ischemic stroke. AJNR Am J Neuroradiol 25: 322–328
Hacke W et al. (2004) Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet 363: 768–774
Alexandrov AV et al. (2004) Ultrasound-enhanced systemic thrombolysis for acute ischemic stroke. N Engl J Med 351: 2170–2178
Alberts MJ et al. (2000) Recommendations for the establishment of primary stroke centers. Brain Attack Coalition. JAMA 283: 3102–3109
Alberts MJ et al. (2005) Recommendations for comprehensive stroke centers: a consensus statement from the Brain Attack Coalition. Stroke 36: 1597–1616
Suzuki S et al. (2004) Access to intra-arterial therapies for acute ischemic stroke: an analysis of the US population. AJNR Am J Neuroradiol 25: 1802–1806
Lewandowski CA et al. (1999) Combined intravenous and intra-arterial r-TPA versus intra-arterial therapy of acute ischemic stroke: Emergency Management of Stroke (EMS) Bridging Trial. Stroke 30: 2598–2605
IMS Investigators (2004) Combined intravenous and intra-arterial recanalization for acute ischemic stroke: the Interventional Management of Stroke Study. Stroke 35: 904–911
IMS II Investigators (2006) Preliminary results of the IMS II trial [abstract]. Stroke 37: 708
Welch K (1956) Excision of occlusive lesions of the middle cerebral artery. J Neurosurg 13: 73–80
Meyer FB et al. (1985) Emergency embolectomy for acute occlusion of the middle cerebral artery. J Neurosurg 62: 639–647
Eggers F et al. (1979) Iatrogenic carotid-cavernous fistula following Fogarty catheter thromboendarterectomy. Case report. J Neurosurg 51: 543–545
Wikholm G (2003) Transarterial embolectomy in acute stroke. AJNR Am J Neuroradiol 24: 892–894
Mayer TE et al. (2002) Treatment of basilar artery embolism with a mechanical extraction device: necessity of flow reversal. Stroke 33: 2232–2235
Felten RP et al. (2005) The Food and Drug Administration medical device review process: clearance of a clot retriever for use in ischemic stroke. Stroke 36: 404–406
Smith WS et al. (2005) Safety and efficacy of mechanical embolectomy in acute ischemic stroke: results of the MERCI trial. Stroke 36: 1432–1438
Smith WS (2005) Comparison of MERCI Mortality with NINDS. Stroke 36: 490
Smith WS (2006) Safety of mechanical thrombectomy and intravenous tissue plasminogen activator in acute ischemic stroke. Results of the multi Mechanical Embolus Removal in Cerebral Ischemia (MERCI) trial, part 1. AJNR Am J Neuroradial 27: 1177–1182
Saver JL (2006) Does the Merci Retriever work? For. Stroke 37: 1340–1341
Wechsler LR (2006) Does the Merci Retriever work? Against. Stroke 37: 1341–1342
Davis SM and Donnan GA (2006) Merci Retriever: does it work? Stroke 37: 1343–1344
Becker KJ and Brott TG (2005) Approval of the MERCI clot retriever: a critical view. Stroke 36: 400–403
Furlan AJ and Fisher M (2005) Devices, drugs, and the Food and Drug Administration: increasing implications for ischemic stroke. Stroke 36: 398–399
Lev MH et al. (2001) CT angiography in the rapid triage of patients with hyperacute stroke to intraarterial thrombolysis: accuracy in the detection of large vessel thrombus. J Comput Assist Tomogr 25: 520–528
Smith WS et al. (2003) Safety and feasibility of a CT protocol for acute stroke: combined CT, CT angiography, and CT perfusion imaging in 53 consecutive patients. AJNR Am J Neuroradiol 24: 688–690
Author information
Authors and Affiliations
Ethics declarations
Competing interests
The author has declared associations with the following company: Concentric Medical.
WS Smith owns stock in Concentric Medical.
Rights and permissions
About this article
Cite this article
Smith, W. Technology Insight: recanalization with drugs and devices during acute ischemic stroke. Nat Rev Neurol 3, 45–53 (2007). https://doi.org/10.1038/ncpneuro0372
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/ncpneuro0372
This article is cited by
-
Translational initiatives in thrombolytic therapy
Frontiers of Medicine (2017)
-
CT Density Changes with Rapid Onset Acute, Severe, Focal Cerebral Ischemia in Monkeys
Translational Stroke Research (2012)
-
Workflow Optimization in Vertebrobasilar Occlusion
CardioVascular and Interventional Radiology (2012)
-
A case of acute ischemic stroke: optimizing management with penumbra and vessel imaging
Nature Clinical Practice Neurology (2007)