Abstract
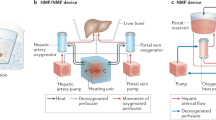
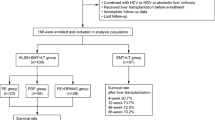
Emergency orthotopic liver transplantation (OLT) is currently the only standard treatment for fulminant hepatic failure (FHF). The waiting time for transplantation can exceed a week—using a liver assist device to bridge patients with FHF to OLT might therefore decrease the mortality rate. Several liver support systems have been described, but no system has gained FDA approval or widespread clinical acceptance. Although the results of many experimental and clinical trials are encouraging, the field is still in its initial stages. Using nonbiologic liver support is based on the assumption that several toxins that cause hepatic coma can be removed from the circulation by blood or plasma sorption methods. As these toxins could be involved in many FHF complications recovery without the need for transplantation is the ultimate aim. Biologic liver support uses xenogeneic livers or hepatocytes to support the failed human liver, exploiting biological cell functions, namely detoxification, metabolism, and biosynthesis. The classical nonbiologic dialysis methods could decrease mortality in patients with acute-on-chronic liver failure, but definitive conclusions are impossible to draw because of the small number of patients studied and inadequate follow-up. Larger studies performed in specialty centers should provide conclusive data about the role of the bioartificial liver support system as a possible universal bridge to OLT. This article presents an overview of published experience with liver support systems since the 1960s.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
van de Kerkhove MP et al. (2004) Clinical application of bioartificial liver support systems. Ann Surg 240: 216–230
Punch JD (2004) Bridges to transplantation. Anesthesiol Clin North Am 22: 863–869
Millis JM et al. (2002) Initial experience with the modified extracorporeal liver-assist device for patients with fulminant hepatic failure: system modifications and clinical impact. Transplantation 74: 1735–1746
Kamohara Y et al. (1998) Artificial liver: review and Cedars-Sinai experience. J Hepatobiliary Pancreat Surg 5: 273–285
George J (2004) Artificial liver support systems. J Assoc Physicians India 52: 719–722
Lee C and Tink A (1958) Exchange transfusion in hepatic coma. Report of a case. Med J Austr 1: 40–42
Trey MB et al. (1966) Treatment of hepatic coma by exchange blood transfusion. N Engl J Med 274: 473–481
Sabin S and Meritt JA (1968) Treatment of hepatic coma in cirrhosis by plasmapheresis and plasma infusion (plasma exchange). Ann Int Med 68: 1–7
Takahashi T et al. (1991) Artificial liver: state of the art. Dig Dis Sci 36: 1327–1340
Merrill JP et al. (1950) The use of an artificial kidney II: clinical experience. J Clin Invest 29: 452–438
Opolon P (1979) High permeability membrane hemodialysis and hemofiltration in acute hepatic coma. Experimental and clinical results. Artif Organs 3: 354–360
Yoshiba M et al. (1993) Development of reliable artificial liver support (ALS) plasma exchange in combination with hemodiafiltration using high-performance membrane. Dig Dis Sci 38: 469–476
Khurshid I et al. (2002) Sickle cell disease, extreme hyperbilirubinemia, and pericardial tamponade: case report and review of the literature. Crit Care Med 30: 2363–2367
Ayuub M et al. (2000) Usefulness of exchange transfusion in acute liver failure due to severe P. falciparum malaria. Am J Gastroenterol 95: 802–804
Rifai K et al. (2003) Liver replacement therapy. Reliable indications in acute liver failure. Internist 44: 1485–1490
Stockmann HB and Ijzermans JN (2002) Prospects for the temporary treatment of acute liver failure. Eur J Gastroenterol Hepatol 14: 195–203
Singer AL et al. (2001) Role of plasmapheresis in the management of acute hepatic failure in children. Ann Surg 234: 418–424
Kazama JJ et al. (2003) Successful perioperative blood purification therapy in patients with maintenance hemodialysis therapy who underwent living donor liver transplantation. Clin Nephrol 59: 229–233
Borra M et al. (2002) Advanced technology for extracorporeal liver support system devices. Int J Artif Organs 25: 939–949
Agarwal R and Farber MO (2002) Is continuous veno-venous hemofiltration for acetaminophen-induced acute liver and renal failure worthwhile? Clin Nephrol 57: 167–170
Bellomo R and Ronco C (2000) Continuous haemofiltration in the intensive care unit. Crit Care 4: 339–345
Gimson AE et al. (1982) Earlier charcoal hemoperfusion in fulminant hepatic failure. Lancet 2: 681–683
O'Grady JG et al. (1988) Controlled trials of charcoal hemoperfusion and prognostic factors in fulminant hepatic failure. Gastroenterology 94: 1186–1192
Wilkinson AH et al. (1998) Hemodiabsorption in treatment of hepatic failure. J Transplant Coord 8: 43–50
Ellis AJ et al. (1999) Temporary extracorporeal liver support for severe acute alcoholic hepatitis using the BioLogic-DT. Int J Artif Organs 22: 27–34
Hughes RD (2002) Review of methods to remove protein-bound substances in liver failure. Int J Artif Organs 25: 911–917
Hughes RD and Williams R (1993) Use of sorbent columns and haemofiltration in fulminant hepatic failure. Blood Purif 11: 163–169
Sen S et al. (2005) Emerging indications for albumin dialysis. Am J Gastroenterol 100: 468–475
Felldin M et al. (2003) Treatment with the molecular adsorbent recirculating system in patients with acute liver failure. Transpl Proc 35: 822–823
Mitzner SR et al. (2000) Improvement of hepatorenal syndrome with extracorporeal albumin dialysis MARS: results of a prospective, randomized, controlled clinical trial. Liver Transpl 6: 277–286
Rifai K et al. (2003) Prometheus—a new extracorporeal system for the treatment of liver failure. J Hepatol 39: 984–990
de Kerkhove MP et al. (2003) MARS treatment in posthepatectomy liver failure. Liver Int 23 (Suppl 3): 44–51
Sauer IM et al. (2004) In vitro comparison of the molecular adsorbent recirculation system (MARS) and single-pass albumin dialysis (SPAD). Hepatology 39: 1408–1414
Krebs HA and Henseleit K (1932) Untersuchungen uber die harnstoffbildung im tierkorper. Hoppe-Seyler's Zentralblatt fur Physische Chemie 210: 33–66
Otto JJ et al. (1958) The use of a donor liver in experimental animals with elevated blood ammonia. Surgery 43: 301–309
Lie TS (1980) Treatment of acute hepatic failure by extracorporeal hemoperfusion over human and baboon liver. In: Artificial liver support, 268–273 (Eds Brunner G and Schmidt FW) Berlin: Springer
Wolf CF and Munkelt BE (1975) Bilirubin conjugation by an artificial liver composed of cultured cells and synthetic capillaries. ASAIO Trans 21: 16–26
Argibay PF et al. (2000) Polyacrylonitrile membrane interposition between a xenograft and a patient in fulminant liver failure: the concept of xenohemodiafiltration in clinical practice. ASAIO J 46: 505–510
Linke R et al. (1998) Prevention of initial perfusion failure during xenogeneic ex vivo liver perfusion by selectin inhibition. Transplantation 66: 1265–1272
Pascher A et al. (1997) Immunopathological observations after xenogeneic liver perfusions using donor pigs transgenic for human decay-accelerating factor. Transplantation 64: 384–391
Abouns GM et al. (2001) Successful ex vivo liver perfusion system for hepatic failure pending liver regeneration or liver transplantation. Transplant Proc 33: 1962–1964
Chowdhury JR et al. (1998) Human hepatocyte transplantation: gene therapy and more? Pediatrics 102: 647–648
Mito M et al. (1979) Studies on ectopic liver utilizing hepatocyte transplantation into the rat spleen. Transpl Proc 11: 585–591
Darby H et al. (1986) Observations on rat spleen reticulum during the development of syngeneic hepatocellular implants. Br J Exp Pathol 67: 329–339
Selden AC et al. (1991) Further observations on the survival, proliferation and function of ectopically implanted syngeneic and allogeneic liver cells in rat spleen. Eur J Hepatol Gastroenterol 3: 607–611
Selden C and Hodgson H (2004) Cellular therapies for liver replacement. Transpl Immunol 12: 273–288
Soriano H (2002) Liver cell transplantation: human applications in adults and children. In: Hepatocyte transplantation: proceedings of Falk Symposium 126 (Progress in Gastroenterology and Hepatology Part III) held in Hannover, Germany, October 2–3, 2001, 99–105 (Eds Gupta S et al.) Dordrecht, Boston, London: Kluwer Academic Publishers
Strom SC et al. (1997) Hepatocyte transplantation as a bridge to orthotopic liver transplantation in terminal liver failure. Transplantation 63: 559–569
Bilir BM et al. (2000) Hepatocyte transplantation in acute liver failure. Liver Transplant 6: 32–40
Filippi C et al. (2004) Improvement of C3A cell metabolism for usage in bioartificial liver support systems. J Hepatol 41: 599–605
Gregory PG et al. (2000) In vitro characterization of porcine hepatocyte function. Cell Transplant 9: 1–10
Ellis AJ et al. (1996) Pilot-controlled trial of the extracorporeal liver assist device in acute liver failure. Hepatology 24: 1446–1451
Samuel D et al. (2002) Neurological improvement during bioartificial liver sessions in patients with acute liver failure awaiting transplantation. Transplantation 73: 257–264
Rozga J et al. (1994) A bioartificial liver to treat severe acute liver failure. Ann Surg 219: 538–544
Watanabe FD et al. (1997) Clinical experience with a bioartificial liver in the treatment of severe liver failure. A phase 1 clinical trial. Ann Surg 225: 484–491
van de Kerkhove MP et al. (2003) Bridging of a patient with acute liver failure to liver transplantation by the AMC-bioartificial liver. Cell Transplant 12: 563–568
Sauer IM et al. (2003) Extracorporeal liver support based on primary human liver cells and albumin dialysis—treatment of a patient with primary graft non-function. J Hepatol 39: 649–653
Mazariegos GV et al. (2002) First clinical use of a novel bioartificial liver support system (BLSS). Am J Transplant 2: 260–266
Demetriou AA et al. (2004) Prospective, randomized, multicenter, controlled trial of a bioartificial liver in treating acute liver failure. Ann Surg 239: 660–667
Kjaergard LL et al. (2003) Artificial and bioartificial support systems for acute and acute-on-chronic liver failure: a systematic review. JAMA 289: 217–222
Liu JP et al. (2004) Artificial and bioartificial support systems for liver failure. The Cochrane Database of Systematic Reviews, Issue 1, Art No. CD003628.pub2
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Millis, J., Losanoff, J. Technology Insight: liver support systems. Nat Rev Gastroenterol Hepatol 2, 398–405 (2005). https://doi.org/10.1038/ncpgasthep0254
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/ncpgasthep0254
This article is cited by
-
Efficacy of Fluidized Bed Bioartificial Liver in Treating Fulminant Hepatic Failure in Pigs: A Metabolomics Study
Scientific Reports (2016)
-
Potential of bioengineering processes for therapeutic repopulation of the liver with cells
Biotechnology and Bioprocess Engineering (2007)