Abstract
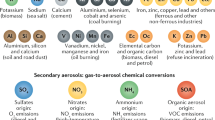
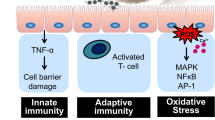
Air pollution is increasingly recognized as an important and modifiable determinant of cardiovascular disease in urban communities. Acute exposure has been linked to a range of adverse cardiovascular events including hospital admissions with angina, myocardial infarction, and heart failure. Long-term exposure increases an individual's lifetime risk of death from coronary heart disease. The main arbiter of these adverse health effects seems to be combustion-derived nanoparticles that incorporate reactive organic and transition metal components. Inhalation of this particulate matter leads to pulmonary inflammation with secondary systemic effects or, after translocation from the lung into the circulation, to direct toxic cardiovascular effects. Through the induction of cellular oxidative stress and proinflammatory pathways, particulate matter augments the development and progression of atherosclerosis via detrimental effects on platelets, vascular tissue, and the myocardium. These effects seem to underpin the atherothrombotic consequences of acute and chronic exposure to air pollution. An increased understanding of the mediators and mechanisms of these processes is necessary if we are to develop strategies to protect individuals at risk and reduce the effect of air pollution on cardiovascular disease.
Key Points
-
Exposure to air pollution is associated with increased cardiovascular morbidity and deaths from myocardial ischemia, arrhythmia, and heart failure
-
Fine particulate matter derived from the combustion of fossil fuels is thought to be the most potent component of the air pollution cocktail
-
Particulate matter upregulates systemic proinflammatory and oxidative pathways, either through direct translocation into the circulation or via secondary pulmonary-derived mediators
-
Exposure to particulate matter has the potential to impair vascular reactivity, accelerate atherogenesis, and precipitate acute adverse thrombotic events
-
In patients with coronary heart disease, exposure to combustion-derived particulate can exacerbate exercise-induced myocardial ischemia
-
Improving air quality standards, reducing personal exposures, and the redesign of engine and fuel technologies could all have a role in reducing air pollution and its consequences for cardiovascular morbidity and mortality
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Dockery DW et al. (1993) An association between air-pollution and mortality in six US cities. N Engl J Med 329: 1753–1759
Pope CA III et al. (2004) Cardiovascular mortality and long-term exposure to particulate air pollution: epidemiological evidence of general pathophysiological pathways of disease. Circulation 109: 71–77
Miller KA et al. (2007) Long-term exposure to air pollution and incidence of cardiovascular events in women. N Engl J Med 356: 447–458
Hoek G (2002) Association between mortality and indicators of traffic-related air pollution in the Netherlands: a cohort study. Lancet 360: 1203–1209
Samet JM et al. (2000) Fine particulate air pollution and mortality in 20 US cities, 1987–1994. N Engl J Med 343: 1742–1749
Peters A et al. (2001) Increased particulate air pollution and the triggering of myocardial infarction. Circulation 103: 2810–2815
Mann JK et al. (2002) Air pollution and hospital admissions for ischemic heart disease in persons with congestive heart failure or arrhythmia. Environ Health Perspect 110: 1247–1252
World Health Organization (2002) World Health Report. Geneva [http:www.who.int/whr/2002/en] (accessed 20 October 2008)
Ware JH (2000) Particulate air pollution and mortality—clearing the air. N Engl J Med 343: 1798–1799
Pope CA III (2007) Mortality effects of longer term exposures to fine particulate air pollution: review of recent epidemiological evidence. Inhal Toxicol 19 (Suppl 1): 33–38
Brook RD (2008) Cardiovascular effects of air pollution. Clin Sci (Lond) 115: 175–187
Simkhovich BZ et al. (2008) Air pollution and cardiovascular injury: epidemiology, toxicology, and mechanisms. J Am Coll Cardiol 25: 719–726
Scheepers PT and Bos RP (1992) Combustion of diesel fuel from a toxicological perspective. Int Arch Occup Environ Health 64: 163–177
Donaldson K et al. (2005) Combustion-derived nanoparticles: a review of their toxicology following inhalation exposure. Part Fibre Toxicol 2: 10
Brunekreef B and Forsberg B (2005) Epidemiological evidence of effects of coarse airborne particles on health. Eur Respir J 26: 309–318
Seaton A et al. (1995) Particulate air pollution and acute health effects. Lancet 345: 176–178
Li XY et al. (1996) Free radical activity and pro-inflammatory effects of particulate air pollution (PM10) in vivo and in vitro. Thorax 51: 1216–1222
Elder A et al. (2004) On-road exposure to highway aerosols. 2. Exposures of aged, compromised rats. Inhal Toxicol 16 (Suppl 1): 41–53
Ghio AJ et al. (2000) Concentrated ambient air particles induce mild pulmonary inflammation in healthy human volunteers. Am J Respir Crit Care Med 162: 981–988
Salvi S et al. (1999) Acute inflammatory responses in the airways and peripheral blood after short-term exposure to diesel exhaust in healthy human volunteers. Am J Respir Crit Care Med 159: 702–709
van Eeden SF et al. (2001) Cytokines involved in the systemic inflammatory response induced by exposure to particulate matter air pollutants (PM10). Am J Respir Crit Care Med 164: 826–830
Fujii T et al. (2002) Interaction of alveolar macrophages and airway epithelial cells following exposure to particulate matter produces mediators that stimulate the bone marrow. Am J Respir Cell Mol Biol 27: 34–41
Tan WC et al. (2000) The human bone marrow response to acute air pollution caused by forest fires. Am J Respir Crit Care Med 161: 1213–1217
Elder AC et al. (2004) Systemic effects of inhaled ultrafine particles in two compromised, aged rat strains. Inhal Toxicol 16: 461–471
Cassee FR et al. (2005) Inhalation of concentrated particulate matter produces pulmonary inflammation and systemic biological effects in compromised rats. J Toxicol Environ Health A 68: 773–796
Peters A et al. (2001) Particulate air pollution is associated with an acute phase response in men; results from the MONICA-Augsburg Study. Eur Heart J 22: 1198–1204
Pekkanen J et al. (2000) Daily concentrations of air pollution and plasma fibrinogen in London. Occup Environ Med 57: 818–822
Peters A et al. (1997) Increased plasma viscosity during an air pollution episode: a link to mortality? Lancet 349: 1582–1587
Frampton MW et al. (2006) Inhalation of ultrafine particles alters blood leukocyte expression of adhesion molecules in humans. Environ Health Perspect 114: 51–58
Nemmar A et al. (2001) Passage of intratracheally instilled ultrafine particles from the lung into the systemic circulation in hamster. Am J Respir Crit Care Med 164: 1665–1668
Kreyling WG et al. (2002) Translocation of ultrafine insoluble iridium particles from lung epithelium to extrapulmonary organs is size dependent but very low. J Toxicol Environ Health A 65: 1513–1530
Oberdorster G et al. (2002) Extrapulmonary translocation of ultrafine carbon particles following whole-body inhalation exposure of rats. J Toxicol Environ Health A 65: 1531–1543
Nemmar A et al. (2002) Passage of inhaled particles into the blood circulation in humans. Circulation 105: 411–414
Mills NL et al. (2006) Do inhaled carbon nanoparticles translocate directly into the circulation in humans. Am J Respir Crit Care Med 173: 426–431
Brook RD et al. (2004) Air pollution and cardiovascular disease: a statement for healthcare professionals from the Expert Panel on Population and Prevention Science of the American Heart Association. Circulation 109: 2655–2671
Guzman LA et al. (1996) Local intraluminal infusion of biodegradable polymeric nanoparticles: a novel approach for prolonged drug delivery after balloon angioplasty. Circulation 94: 1441–1448
Sun Q et al. (2005) Long-term air pollution exposure and acceleration of atherosclerosis and vascular inflammation in an animal model. JAMA 294: 3003–3010
Araujo JA et al. (2008) Ambient particulate pollutants in the ultrafine range promote early atherosclerosis and systemic oxidative stress. Circ Res 102: 589–596
Suwa T et al. (2002) Particulate air pollution induces progression of atherosclerosis. J Am Coll Cardiol 39: 935–942
Kunzli N et al. (2005) Ambient air pollution and atherosclerosis in Los Angeles. Environ Health Perspect 113: 201–206
Hoffmann B et al. (2007) Residential exposure to traffic is associated with coronary atherosclerosis. Circulation 116: 489–496
Peters A et al. (2004) Exposure to traffic and the onset of myocardial infarction. N Engl J Med 351: 1721–1730
Gilmour PS et al. (2005) The procoagulant potential of environmental particles (PM10). Occup Environ Med 62: 164–171
Sun Q et al. (2008) Ambient air particulate matter exposure and tissue factor expression in atherosclerosis. Inhal Toxicol 20: 127–137
Khandoga A et al. (2004) Ultrafine particles exert prothrombotic but not inflammatory effects on the hepatic microcirculation in healthy mice in vivo. Circulation 109: 1320–1325
Gatti AM and Montanari S (2006) Retrieval analysis of clinical explanted vena cava filters. J Biomed Mater Res B Appl Biomater 77: 307–314
Baccarelli A et al. (2008) Exposure to particulate air pollution and risk of deep vein thrombosis. Arch Intern Med 168: 920–927
Nemmar A et al. (2003) Diesel exhaust particles in lung acutely enhance experimental peripheral thrombosis. Circulation 107: 1202–1208
Lucking et al. (2008) Diesel exhaust inhalation increases thrombus formation in man. Eur Heart J [10.1093/eurheartj/ehn464]
Radomski A et al. (2005) Nanoparticle-induced platelet aggregation and vascular thrombosis. Br J Pharmacol 146: 882–893
Ray MR et al. (2006) Platelet activation, upregulation of CD11b/CD18 expression on leukocytes and increase in circulating leukocyte–platelet aggregates in Indian women chronically exposed to biomass smoke. Hum Exp Toxicol 25: 627–635
Hosseinpoor AR et al. (2005) Air pollution and hospitalization due to angina pectoris in Tehran, Iran: a time-series study. Environ Res 99: 126–131
Pekkanen J et al. (2002) Particulate air pollution and risk of ST-segment depression during repeated submaximal exercise tests among subjects with coronary heart disease: the Exposure and Risk Assessment for Fine and Ultrafine Particles in Ambient Air (ULTRA) study. Circulation 106: 933–938
Brook RD et al. (2002) Inhalation of fine particulate air pollution and ozone causes acute arterial vasoconstriction in healthy adults. Circulation 105: 1534–1536
Mills NL et al. (2005) Diesel exhaust inhalation causes vascular dysfunction and impaired endogenous fibrinolysis. Circulation 112: 3930–3936
Törnqvist H et al. (2007) Persistent endothelial dysfunction in humans after diesel exhaust inhalation. Am J Respir Crit Care Med 176: 395–400
Mills NL et al. (2007) Air pollution and atherothrombosis. Inhal Toxicol 19 (Suppl 1): 81–89
Sun Q et al. (2008) Air pollution exposure potentiates hypertension through reactive oxygen species-mediated activation of Rho/ROCK. Arterioscler Thromb Vasc Biol 28: 1760–1766
Zanobetti A et al. (2004) Ambient pollution and blood pressure in cardiac rehabilitation patients. Circulation 110: 2184–2189
Auchincloss AH et al. (2008) Associations between recent exposure to ambient fine particulate matter and blood pressure in the Multi-Ethnic Study of Atherosclerosis (MESA). Environ Health Perspect 116: 486–491
Urch B et al. (2005) Acute blood pressure responses in healthy adults during controlled air pollution exposures. Environ Health Perspect 113: 1052–1055
Mills NL et al. (2007) Ischemic and thrombotic effects of dilute diesel-exhaust inhalation in men with coronary heart disease. N Engl J Med 357: 1075–1082
Newby DE et al. (1999) Endothelial dysfunction, impaired endogenous fibrinolysis, and cigarette smoking: a mechanism for arterial thrombosis and myocardial infarction. Circulation 99: 1411–1415
Tsuji H et al. (1996) Determinants of heart rate variability. J Am Coll Cardiol 28: 1539–1546
Kleiger RE et al. (1987) Decreased heart rate variability and its association with increased mortality after acute myocardial infarction. Am J Cardiol 59: 256–262
Liao D et al. (1999) Daily variation of particulate air pollution and poor cardiac autonomic control in the elderly. Environ Health Perspect 107: 521–525
Peters A et al. (2000) Air pollution and incidence of cardiac arrhythmia. Epidemiology 11: 11–17
Dockery DW et al. (2005) Association of air pollution with increased incidence of ventricular tachyarrhythmias recorded by implanted cardioverter defibrillators. Environ Health Perspect 113: 670–674
Lehnert BE (1992) Pulmonary and thoracic macrophage subpopulations and clearance of particles from the lung. Environ Health Perspect 97: 17–46
Acknowledgements
NL Mills is supported by a Michael Davies Research Fellowship from the British Cardiovascular Society. This work was supported by a British Heart Foundation Programme Grant (RG/05/003) and the Swedish Heart Lung Foundation.
Charles P Vega, University of California, Irvine, CA, is the author of and is solely responsible for the content of the learning objectives, questions and answers of the Medscape-accredited continuing medical education activity associated with this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Mills, N., Donaldson, K., Hadoke, P. et al. Adverse cardiovascular effects of air pollution. Nat Rev Cardiol 6, 36–44 (2009). https://doi.org/10.1038/ncpcardio1399
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ncpcardio1399
This article is cited by
-
Effective density of inhaled environmental and engineered nanoparticles and its impact on the lung deposition and dosimetry
Particle and Fibre Toxicology (2024)
-
Long-term exposure to particulate matter and risk of Alzheimer’s disease and vascular dementia in Korea: a national population-based Cohort Study
Environmental Health (2023)
-
Human exposure to diesel exhaust induces CYP1A1 expression and AhR activation without a coordinated antioxidant response
Particle and Fibre Toxicology (2023)
-
Single inhalation exposure to polyamide micro and nanoplastic particles impairs vascular dilation without generating pulmonary inflammation in virgin female Sprague Dawley rats
Particle and Fibre Toxicology (2023)
-
A systematic review and meta-analysis of air pollution and angina pectoris attacks: identification of hazardous pollutant, short-term effect, and vulnerable population
Environmental Science and Pollution Research (2023)