Abstract
Both prognosis and quality of life are poor for severely symptomatic patients with stage D heart failure, and treatment options are limited. Few individuals are eligible for cardiac transplantation, and ventricular resynchronization therapy provides only marginal benefit in select patients. The aim of this Review is to highlight the promise of blood pumps in this setting. Circulatory support devices were first developed to act as a bridge to recovery in patients who had failed to wean from cardiopulmonary bypass. As blood pumps developed, they were used to support patients with cardiogenic shock until a donor heart became available. Implantable left ventricular assist devices were then shown to relieve heart failure symptoms and prolong life in patients ineligible for transplant. The limitations of first-generation device technology have meant that the development of an 'off the shelf' solution for advanced heart failure has been slow to progress. New rotary blood pumps already show much promise in this regard but have not yet been subject to rigorous clinical trials. Anecdotal evidence from 7.5 years of event-free survival in the first patient to receive a 'destination' axial flow pump permits justifiable optimism about the future of this approach. It is now time for real progress.
Key Points
-
Severely symptomatic (stage D or NYHA class IV) heart failure is an expanding problem, with patients having a poor prognosis and limited treatment options
-
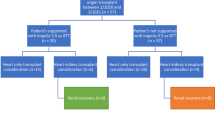
Cardiac allotransplantation does not address the epidemiological problem and lacks a firm evidence base, particularly for ambulatory United Network for Organ Sharing status II candidates
-
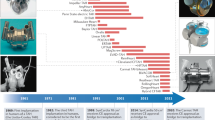
Mechanical blood pumps were first developed to sustain life in patients with cardiogenic shock during heart surgery, then were used in selected patients with end-stage heart failure pending acquisition of a donor heart
-
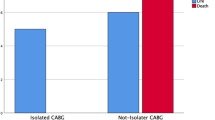
The REMATCH trial provided firm though inauspicious evidence for the use of blood pumps as an alternative to medical therapy in the end-stage heart failure population not eligible for transplant
-
Destination therapy with the new rotary blood pumps provides a promising 'off the shelf' solution to heart failure, but more rigorous, independent, non-industry-sponsored clinical trials are needed to provide a firm evidence base for the use of these devices
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Redfield MM (2002) Heart failure—an epidemic of uncertain proportions. N Engl J Med 347: 1442–1444
Park SJ et al. (2005) Left ventricular assist devices as destination therapy: a new look at survival. J Thorac Cardiovasc Surg 129: 9–17
Frazier OH et al. (1995) Improved mortality and rehabilitation of transplant candidates treated with a long-term implantable left ventricular assist system. Ann Surg 222: 327–336
Cadeiras M et al. (2007) Cardiac transplantation: any role left? Heart Fail Clin 3: 321–347
Rose EA et al. for the Randomized Evaluation of Mechanical Assistance for the Treatment of Congestive Heart Failure (REMATCH) Study Group (2001) Long term mechanical left ventricular assistance for end-stage heart failure. N Engl J Med 345: 1435–1443
Young JB (2007) Heart failure's near dead and dying: reconsidering our heart transplant wait list scheme. J Am Coll Cardiol 50: 1291–1293
Westaby S (2007) Surgery for heart failure: now something for everyone? Heart Fail Clin 3: 139–157
Lietz K and Miller LW (2007) Improved survival of patients with end-stage heart failure listed for heart transplantation: analysis of organ procurement and transplantation network/U.S. United Network of Organ Sharing data, 1990 to 2005. J Am Coll Cardiol 50: 1282–1290
Deng MC et al. for the Comparative Outcome and Clinic Profiles in Transplantation (COCPIT) Study Group (2000) Effect of receiving a heart transplant: analysis of a national cohort entered onto a waiting list, stratified by heart failure severity. Br Med J 321: 540–545
Shah NR et al. (2004) Survival of patients removed from the heart transplant waiting list. J Thorac Cardiovasc Surg 127: 1481–1485
Hunt SA (2006) Taking heart—cardiac transplantation, past, present and future. N Engl J Med 355: 231–235
Cleland JG et al. for the Cardiac Resynchronization-Heart Failure (CARE-HF) Study Investigators (2005) The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med 352: 1539–1549
Bardy GH et al. for the Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators (2005) Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 352: 225–237
Beshai JF et al. for the RethinQ Study Investigators (2007) Cardiac-resynchronization therapy in heart failure with narrow QRS complexes. N Engl J Med 357: 2461–2471
McAlister FA et al. (2007) Cardiac resynchronization therapy for patients with left ventricular systolic dysfunction: a systematic review. JAMA 297: 2502–2514
Lee H et al. (2002) Cost analysis of ongoing care of patients with end-stage renal disease: the impact of dialysis modality and dialysis access. Am J Kidney Dis 40: 611–622
The United States Renal Data System. 2004 Annual Data Report. [http://www.usrds.org/adr_2004.htm]
Lietz K et al. (2007) Outcomes of left ventricular assist device implantation as destination therapy in the post-REMATCH era: implications for patient selection. Circulation 116: 497–505
Rogers JG et al. for the INTrEPID Investigators (2007) Chronic mechanical circulatory support inotrope-dependent heart failure patients who are not transplant candidates. J Am Coll Cardiol 50: 741–747
Warner-Stevenson L and Couper G (2007) On the fledgling field of mechanical circulatory support. J Am Coll Cardiol 50: 748–751
Haft J et al. (2007) Hemodynamic and exercise performance with pulsatile and continuous-flow left ventricular assist devices. Circulation 116 (Suppl 11): I8–I15
Westaby S (2004) Ventricular assist devices as destination therapy. Surg Clin North Am 84: 91–123
Siegenthaler M et al. (2006) Mechanical reliability of the Jarvik 2000 Heart. Ann Thorac Surg 81: 1752–1758
Frazier OH et al. (2004) Clinical experience with an implantable intracardiac continuous flow circulatory support device: physiologic implications and their relationship to patient selection. Ann Thorac Surg 77: 133–142
Miller LW et al. for the HeartMate II Clinical Investigators (2007) Use of a continuous flow device in patients awaiting heart transplantation. N Engl J Med 357: 885–896
Westaby S et al. (2006) Six years of continuous mechanical circulatory support. N Engl J Med 335: 325–327
Potapov EV et al. (2006) Patients supported for over 4 years with left ventricular assist devices. Eur J Heart Fail 8: 756–759
Hetzer R et al. (1999) Cardiac recovery in dilated cardiomyopathy by unloading with a left ventricular assist device. Ann Thorac Surg 68: 742–749
Birks EJ et al. (2006) Left ventricular assist device and drug therapy for reversal of heart failure. N Engl J Med 255: 1873–1884
Maybaum S et al. for the LVAD Working Group (2007) Cardiac improvement during mechanical circulatory support: a prospective multicentre study of the LVAD Working Group. Circulation 115: 2497–2505
Levy WC et al. (2006) The Seattle Heart Failure Model: prediction of survival in heart failure. Circulation 113: 1424–1433
Stewart G et al. (2006) Heart failure patients define threshold for left ventricular assist devices [abstract]. Circulation 114: II484
Lee DS et al. (2003) Predicting mortality among patients hospitalized for heart failure: derivation and validation of a clinical model. JAMA 290: 2581–2587
Westaby S (2007) Lifetime circulatory support must not be restricted to transplant centres. Heart Failure Clin 3: 369–376
Poole-Wilson PA (2008) Focus on mechanical assist devices for the treatment of heart failure. Nat Clin Pract Cardiovasc Med 5: 59
Author information
Authors and Affiliations
Ethics declarations
Competing interests
The author declares no competing financial interests.
Rights and permissions
About this article
Cite this article
Westaby, S. Destination therapy: time for real progress. Nat Rev Cardiol 5, 477–483 (2008). https://doi.org/10.1038/ncpcardio1255
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ncpcardio1255