Abstract
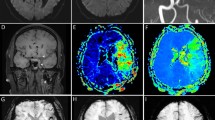
Annually, an estimated 1 million patients undergo heart surgery worldwide. Unfortunately, stroke continues to be a frequent complication of cardiac surgery, with the specific cerebrovascular risk depending upon the particular surgical procedure performed. Neuroimaging has an integral role in the initial evaluation and management of patients who present with acute stroke symptoms following cardiac surgery. The aim of this paper is to review the role brain MRI has in detecting postoperative brain ischemia in these patients. Multimodal MRI—using diffusion-weighted MRI (DWI), perfusion-weighted MRI, and gradient-recalled echo imaging—has an excellent capacity to identify and delineate the size and location of acute ischemic strokes as well as intracerebral hemorrhages. This differentiation is critical in making appropriate treatment decisions in the acute setting, such as determining patient eligibility for thrombolytic or hemodynamic therapies. At present, DWI offers prognostic value in patients with strokes following cardiac surgery. Additionally, DWI could be a valuable tool for evaluating stroke preventive measures as well as therapeutic interventions in patients undergoing CABG surgery.
Key Points
-
Stroke is a known complication of cardiac surgery
-
Brain imaging has an essential role in the evaluation and management of patients who present with acute stroke symptoms following cardiac surgery
-
Multimodal MRI–with the use of diffusion-weighted, perfusion-weighted, and gradient-recalled echo imaging–is useful in delineating the presence, size and location of acute ischemic strokes and intracerebral hemorrhage
-
Multimodal MRI is essential for making appropriate acute treatment decisions in patients with stroke symptoms after cardiac surgery
-
DWI offers prognostic value in patients who have had a stroke following cardiac surgery, and could prove a valuable tool for evaluating preventive and therapeutic interventions in patients undergoing CABG surgery
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Barbut D and Caplan LR (1997) Brain complications of cardiac surgery. Curr Prob Cardiol 22: 455–476
Wolman RL et al.; for the Multicenter Study of Perioperative Ischemia (McSPI) Research Group and the Ischemia Research and Education Foundation (IREF) Investigators (1999) Cerebral injury after cardiac surgery: identification of a group at extraordinary risk. Stroke 30: 514–522
Bucerius J et al. (2003) Stroke after cardiac surgery: a risk factor analysis of 16,184 consecutive adult patients. Ann Thorac Surg 75: 472–478
Naylor AR et al. (2002) Carotid artery disease and stroke during coronary artery bypass: a critical review of the literature. Eur J Vasc Endovasc Surgery 23: 283–294
The Bypass Angioplasty Revascularization Investigation (BARI) Investigators (1996) Comparison of coronary bypass surgery with angioplasty in patients with multivessel disease. N Engl J Med 335: 217–225
King SB et al. (1994) A randomized trial comparing coronary angioplasty with coronary bypass surgery. Emory Angioplasty versus Surgery Trial (EAST). N Engl J Med 331: 1044–1050
Ricotta JJ et al. (2003) Modeling stroke risk after coronary artery bypass and combined coronary artery bypass and carotid endarterectomy. Stroke 34: 1212–1217
Wityk RJ et al. (2001) Diffusion- and perfusion-weighted brain magnetic resonance imaging in patients with neurologic complications after cardiac surgery. Arch Neurol 58: 571–576
Roach GW et al. (1996) Adverse cerebral outcomes after coronary bypass surgery. Multicenter Study of Peripoerative Ischemia Research Group and the Ischemia Research and Education Foundation Investigators. N Eng J Med 335: 1857–1863
Salzberg SP et al. (2005) Coronary artery surgery: conventional coronary artery bypass grafting versus off-pump coronary artery bypass grafting. Curr Opin Cardiol 20: 509–516
Lund C et al. (2005) Cerebral ischemic injury and cognitive impairment after off-pump and on-pump coronary artery bypass grafting surgery. Ann Thorac Surg 80: 2126–2131
Wijeysundera DN et al. (2005) Off pump coronary artery surgery for reducing mortality and morbidity: meta-analysis of randomized and observational studies. J Am Coll Cardiol 46: 872–882
Lamy A et al. (2005) The Canadian off-pump cornary artery bypass graft registry: a one-year prospective comparison with on-pump coronary artery bypass grafting. Can J Cardiol 21: 1175–1181
Panesar SS et al. (2006) Early outcomes in the elderly: a meta-analysis of 4,921 patients undergoing coronary artery bypass grafting—comparison between off-pump and on-pump techniques. Heart 92: 1808–1816
Van Dijk D et al.; Octopus Study Group (2002) Cognitive outcome after off-pump and on-pump coronary artery bypass graft surgery: a randomized trial. JAMA 287: 1405–1412
Novick RJ et al. (2002) Effect of off-pump coronary artery bypass grafting on risk-adjusted and cumulative sum failure outcomes after coronary artery surgery. J Card Surg 17: 520–528
Lev-Ran O et al. (2005) No-touch aorta off-pump coronary surgery: the effect on stroke. J Thorac Cardiovasc Surg 129: 307–313
Sellke FW et al. (2005) Comparing on-pump and off-pump coronary artery bypass grafting—Numerous studies but few conclusions: a scientific statement from the American Heart Association council on cardiovascular surgery and anesthesia in collaboration with the interdisciplinary working group on quality of care and outcomes research. Circulation 11: 2858–2864
Gansera B et al. (2003) Simultaneous carotid endarterectomy and cardiac surgery—additional risk or safety procedure? Thorac Cardiovasc Surg 51: 22–27
Sharony R et al. (2006) Minimally invasive reoperative isolated valve surgery: early and mid-term results. J Card Surg 21: 240–244
Aklog L et al. (1998) Techniques and results of direct-access minimally invasive mitral valve surgery: a paradigm for the future. J Thorac Cardiovasc Surg 116: 705–715
Likosky DS et al. (2003) Determination of etiologic mechanisms of strokes secondary to coronary artery bypass graft surgery. Stroke 34: 2830–2834
Shaw PJ et al. (1985) Early neurological complications of coronary artery bypass surgery. Br Med J 291: 1384–1387
Breuer AC et al. (1983) Central nervous system complications of coronary artery bypass graft surgery: prospective analysis of 421 patients. Stroke 14: 682–687
Ropper AH et al. (1982) Carotid bruit and the risk of stroke in elective surgery. N Engl J Med 307: 1388–1390
Furlan AJ and Craciun AR (1985) Risk of stroke during coronary artery bypass graft surgery in patients with internal carotid artery disease documented by angiography. Stroke 16: 797–799
Sila C (1991) Neuroimaging of cerebral infarction associated with coronary revascularization. AJNR 12: 817–818
Hise JH et al. (1991) Stroke associated with coronary artery bypass surgery. AJNR 12: 811–814
Breuer AC et al. (1983) Central nervous system complications of coronary artery bypass graft surgery: prospective analysis of 421 patients. Stroke 14: 682–687
Wijdicks EFM and Jack CR (1996) Coronary artery bypass grafting-associated stroke. J Neuroimag 6: 20–22
Roach GW et al. (1996) Adverse cerebral outcomes after coronary bypass surgery. Multicenter Study of Perioperative Ischemia Research Group and the Ischemia Research and Education Foundation Investigators. N Engl J Med 335: 1857–1863
Naylor AR et al. (2003) A systematic review of outcomes following staged and synchronous carotid endarterectomy and coronary artery bypass. Eur J Vasc Endovasc Surg 25: 380–389
Mills SA (1995) Risk factors for cerebral injury and cardiac surgery. Ann Thorac Surg 59: 1796–1799
Lynn GM et al. (1992) Risk factors for stroke after coronary artery bypass. J Thorac Cardiovasc Surg 104: 1518–1523
Mangano DT and Mora Mangano CT (1997) Perioperative stroke encephalopathy and CNS dysfunction. J Intensive Care Med 12: 148–160
Barbut D et al. (1994) Cerebral emboli detected during bypass surgery are associated with clamp removal. Stroke 25: 2398–2402
Boivie P et al. (2005) Side differences in cerebrovascular accidents after cardiac surgery: a statistical analysis of neurologica symptoms and possible implications for anatomic mechanisms of aortic particle embolization. J Thorac Cardiovasc Surg 129: 591–598
Pugsley W et al. (1994) The impact of microemboli during cardiopulmonary bypass on neuropsychological functioning. Stroke 25: 1393–1399
Petaja J et al. (1996) Fibrinolysis, antithrombin III, and protein C in neonates during cardiac operations. J Thorac Cardiovasc Surg 112: 665–671
Parolari A et al. (2003) Coagulation and fibrinolytic markers in a two-month follow-up of coronary bypass surgery. J Thorac Cardiovasc Surg 125: 336–343
Gilman S (1965) Cerebral disorders after open-heart operations. N Engl J Med 272: 489–498
Coffey CE et al. (1983) Natural history of cerebral complications of coronary artery bypass graft surgery. Neurology 33: 1416–1421
Perez-Vela JL et al. (2005) Neurologic complications in the immediate postoperative period after cardiac surgery: role of magnetic resonance imaging [Spanish]. Rev Esp Cardiol 58: 1014–1021
Humphreys RP et al. (1975) Cerebral hemorrhage following heart surgery. J Neurosurg 43: 671–675
Sila CA (1989) Spectrum of neurologic events following cardiac transplantation. Stroke 20: 1586–1589
Caplan LR (1988) Intracerebral hemorrhage revisited. Neurology 38: 624–627
Kidwell CS et al. (2004) Comparison of MRI and CT for detection of acute intracerebral hemorrhage. JAMA 292: 1823–1830
Gonzalez RG (2006) Imaging-guided acute ischemic stroke therapy: from “time is brain” to “physiology is brain”. AJNR 27: 728–735
Ringlestein EB et al. (1989) Computed tomographic patterns of proven embolic brain infarcts. Ann Neurol 26: 759–765
Smajlovic D and Sinanovic O (2004) Sensitivity of the neuroimaging techniques in ischemic stroke. Med Arh 58: 282–284
McConnell JR et al. (1990) Magnetic resonance imaging of the brain in infants and children before and after cardiac surgery. Am J Dis Child 144: 374–378
Wityk RJ and Restrepo L (2002) Cardiac surgery and magnetic resonance imaging of the brain. Arch Neurol 59: 1074–1075
Harris DN et al. (1993) Brain swelling in first hour after coronary artery bypass surgery. Lancet 342: 586–587
Vanninen R et al. (1998) Subclinical cerebral complications after coronary artery bypass grafting: prospective analysis with magnetic resonance imaging, quantitative electroencephalography, and neuropsychological assessment. Arch Neurol 55: 618–627
Toner I et al. (1994) Magnetic resonance imaging and neuropsychological changes after coronary artery bypass graft surgery: preliminary findings. J Neurosurg Anesthesiol 6: 163–169
Kohn A (2002) Magnetic resonance imaging registration and quantitation of the brain before and after coronary artery bypass graft surgery. Ann Thorac Surg 73 (Suppl): S363–S365
Steinberg GK et al. (1996) MR and cerebrospinal fluid enzymes as sensitive indicators of subclinical cerebral injury after open-heart valve replacement surgery. Am J Neuroradiol 17: 205–212
Restrepo L et al. (2002) Diffusion- and perfusion-weighted magnetic resonance imaging of the brain before and after coronary artery bypass grafting surgery. Stroke 33: 2909–2915
Lovblad KO et al. (1998) Clinical experience with diffusion-weighted MR in patients with acute stroke. AJNR 19: 1061–1066
Marks MP et al. (1996) Acute and chronic stroke: navigated spin-echo diffusion-weighted MR imaging. Radiology 199: 403–408
Schaefer PW et al. (2000) Diffusion-weighted MR imaging of the brain. Radiology 217: 331–345
Lansberg MG et al. (2000) Advantages of adding diffusion-weighted magnetic resonance imaging to conventional magnetic resonance imaging for evaluating acute stroke. Arch Neurol 57: 1311–1316
Kidwell CS et al. (2002) Late secondary injury in patients receiving intraarterial thrombolysis. Ann Neurol 52: 698–703
Schaefer PW et al. (2004) Characterization and evolution of diffusion MR imaging abnormalities in stroke patients undergoing intraarterial thrombolysis. AJNR 25: 951–957
Beauchamp NJ Jr and Bryan RN (1998) Acute cerebral ischemic infarction: a pathophysiologic review and radiologic perspective. AJR Am J Roentgenol 171: 73–84
Rosen B et al. (1990) Perfusion imaging with NMR contrast agents. Magn Reson Med 14: 249–265
Knipp SC et al. (2005) Small ischemic brain lesions after cardiac valve replacement detected by diffusion-weighted magnetic resonance imaging: relation to neurocognitive function. Eur J Cardiothoracic Surg 28: 88–96
Floyd TF et al. (2006) Clinically silent cerebral ischemic events after cardiac surgery: their incidence, regional vascular occurrence, and procedural dependence. Ann Thorac Surg 81: 2160–2166
Stolz E et al. (2004) Diffusion-weighted magnetic resonance imaging and neurobiochemical markers after aortic valve replacement: implications for future neuroprotective trials? Stroke 35: 888–892
Djaiani G et al. (2004) Mild to moderate atheromatous disease of the thoracic aorta and new ischemic brain lesions after conventional coronary artery bypass graft surgery. Stroke 35: 356–358
Gottesman RF et al. (2006) Watershed strokes after cardiac surgery: diagnosis, etiology, and outcome. Stroke 37: 2306–2311
Bendszus M and Stoll G (2006) Silent cerebral ischaemia: hidden fingerprints of invasive medical procedures. Lancet Neurol 5: 364–372
Bendszus M et al. (2004) Heparin and air filters reduce embolic events caused by intra-arterial cerebral angiography: a prospective, randomized trial. Circulation 110: 2210–2215
Choi SH et al. (2000) Diffusion-weighted MRI in vascular dementia. Neurology 54: 83–89
Fiebach JB et al. (2005) Diffusion and perfusion MR imaging in stroke [German]. Radiologe 45: 412–419
Schalug G et al. (1999) The ischemic penumbra: operationally defined by diffusion and perfusion MRI. Neurology 52: 1784–1792
Sunshine JL et al. (1999) Hyperacute stroke: ultrafast MR imaging to triage patients prior to therapy. Radiology 212: 391–401
Warach S (2003) Measurement of the ischemic penumbra with MRI: it's about time. Stroke 34: 2533–2534
Wittsack HJ et al. (2002) MR imaging in acute stroke: diffusion-weighted and perfusion imaging parameters for predicting infarct size. Radiology 222: 397–403
Oliveira-Filho J and Koroshetz WJ (2000) Magnetic resonance imaging in acute stroke: clinical perspective. Top Magn Reson Imaging 11: 246–258
Bui JD and Caplan LR (2006) Magnetic resonance imaging in intracerebral hemorrhage. Semin Cerebrovasc Dis Stroke 5: 172–177
Fiebach JB et al. (2004) Stroke magnetic resonance imaging is accurate in hyperacute intracerebral hemorrhage. Stroke 35: 502–507
Katz JM and Gobin YP (2006) Merci retriever in acute stroke treatment. Expert Rev Med Devices 3: 273–280
Smith WS et al.; MERCI Trial Investigators (2005) Safety and efficacy of mechanical embolectomy in acute ischemic stroke: results of the MERCI trial. Stroke 36: 1432–1438
Liebeskind DS et al. (2003) Neuroimaging of cerebral ischemia in clinical practice [abstract]. Stroke 34: 255
Ruland S et al. (2002) Acute stroke care in Illinois. Stroke 33: 1334–1339
Edwards MB et al. (2005) Assessment of magnetic field (4.7T) induced forces on prosthetic heart valves and annuloplasty rings. J Magn Reson Imaging 22: 311–317
Pruefer D et al. (2001) In vitro investigation of prosthetic heart valves in magnetic resonance imaging: evaluation of potential hazards. J Heart Valve Dis 10: 410–414
Shellock FG (2001) Prosthetic heart valves and annuloplasty rings: assessment of magnetic field interactions, heating, and artifacts at 1.5 Tesla. J Cardiovasc Magn Res 3: 317–324
Hartnell GG et al. (1997) Safety of MR imaging in patients who have retained metallic materials after cardiac surgery. Am J Roentgenol 168: 1157–1159
Gerber TC et al. (2003) Clinical safety of magnetic resonance imaging early after coronary artery stent placement. J Am Coll Cardiol 42: 1295–1298
Porto I et al. (2005) Safety of magnetic resonance imaging one to three days after bare metal and drug-eluting stent implantation. Am J Cardiol 96: 366–368
Schroeder AP et al. (2000) Magnetic resonance imaging seems safe in patients with intracoronary stents. J Cardiovasc Magn Reson 2: 43–49
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
MC Leary was an investigator for the MERCI trial, which was sponsored by Concentric Medical, Inc., Mountain View, CA. LR Caplan declared he has no competing interests.
Rights and permissions
About this article
Cite this article
Leary, M., Caplan, L. Technology Insight: brain MRI and cardiac surgery—detection of postoperative brain ischemia. Nat Rev Cardiol 4, 379–388 (2007). https://doi.org/10.1038/ncpcardio0915
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/ncpcardio0915
This article is cited by
-
Observation of post-MCAO cortical inflammatory edema in rats by 7.0Tesla MRI
Journal of Huazhong University of Science and Technology [Medical Sciences] (2014)
-
Kardiopulmonaler Bypass in der Herzchirurgie
Der Anaesthesist (2012)
-
Neurologische Komplikationen nach herzchirurgischen Operationen
Zeitschrift für Herz-,Thorax- und Gefäßchirurgie (2011)