Abstract
Molecular characterization of patients with Duchenne or Becker muscular dystrophies is essential for establishing a differential diagnosis, allowing appropriate clinical follow-up, patient management and genetic counseling. In light of the recent mutation-based therapeutic approaches, DMD gene analysis has gained further relevance. Owing to the size and complexity of the DMD gene and the diversity of mutation types, molecular analysis is not always a straightforward task requiring the combination of several methodologies. Our national genetic diagnostic service genetically characterized 308 dystrophinopathy patients (284 unrelated families), leading to the identification of 175 distinct mutations, including 39 unpublished variants. These studies revealed several potential diagnostic pitfalls (because of technical limitations or related with DMD’s genetic heterogeneity) that may be overlooked even considering the international disease-specific diagnostic guidelines. Comprehensive analysis involved expression studies at the mRNA level, the identification of splicing changes and ultimately providing evidence for apparent exceptions to the reading-frame rule. Besides increasing the mutation detection rate, this detailed molecular characterization is indispensable for the identification of suitable candidates for the new mutation-centered therapies. As patient registries are internationally recognized as essential for clinical trial recruitment, this led us to develop the Portuguese Duchenne and Becker Muscular Dystrophy registry in collaboration with the Translational Research in Europe—Assessment and Treatment of Neuromuscular Diseases network.
Similar content being viewed by others
Introduction
Duchenne and Becker Muscular Dystrophy (DMD and BMD, or D/BMD), collectively known as dystrophinopathies, are the most common neuromuscular disorders in childhood. The newborn male incidence of DMD ranges between 1 in 3500 and 6000,1 whereas that of BMD is 1 in 12 000 and 30 000 male births.1, 2 DMD (MIM#310200) is characterized by progressive muscle wasting with onset at the age of 3–5 years, and patients being wheelchair bound at the age of 10–12 years, with death in their twenties often as a result of respiratory or cardiac insufficiency. Mental retardation is observed in approximately one-third of DMD patients.3, 4 BMD (MIM#300376) is a milder allelic form with a later onset and slower progression, with variable degrees of disease severity ranging from a more severe DMD-like presentation to an almost asymptomatic status maintained until the fifth or sixth decade of life.
Both DMD and BMD are caused by mutations in the DMD gene (MIM*300377), one of the largest known human genes, spanning about 2.4 Mb of genomic DNA.5 The gene encodes several transcripts, the most relevant in the muscular disease being a 14-kb muscle-specific isoform. The protein product of the DMD gene—dystrophin—is part of the large dystrophin-associated glycoprotein complex. This structure is necessary for maintaining the link between the cytoskeleton and the extracellular matrix, playing an essential role in preserving the integrity of the muscle cell membrane.6, 7, 8 The lack of dystrophin leads to sarcolemmal fragility, triggering a cascade of events that eventually result in muscle cell death.
The large size of DMD contributes toward a high mutation rate and it has been estimated that ∼25–33% of all cases result from de novo mutational events.9, 10 The most common mutations in the DMD gene are the deletion or duplication of one or more exons, accounting all together for about two-thirds of D/BMD patients. These types of mutations can occur almost anywhere along the gene; however, most are clustered in two hotspot regions: a ‘minor hotspot’ spanning exons 2–20 and a ‘major hotspot’ spanning exons 45–53. The standard diagnostic approach, using techniques such as Multiplex Ligation-Probe Amplification (MLPA), Southern Blot and multiplex PCR, easily detects these mutations. The remaining 30% of pathogenic changes are essentially sub-exonic or sub-intronic, and include nonsense mutations, splice mutations, frameshifts (small deletions or insertions), mid-intronic variants that activate cryptic splice sites and, to a lesser extent, missense mutations. These are usually detected by DMD gene sequencing performed at the genomic and/or complementary DNA (cDNA) level.
DMD phenotype is usually caused by mutations that disrupt the reading frame leading to the complete loss of dystrophin expression, whereas BMD patients are generally associated with in-frame mutations leading to the production of abnormal yet semi-functional protein (with intact N and C termini).11 This genotype–phenotype correlation is known as the ‘reading-frame rule’ and has been demonstrated in about 91% of cases.12 However, several exceptions to this rule have been reported.12, 13 These exceptions are more commonly found in BMD patients and their frequency depends on the type of genetic defect involved: 15% of cases with DMD deletions14 and approximately 30–34% of cases with duplications.14, 15
Comprehensive genetic analysis and detailed molecular characterization of individual case reports and more extensive patient cohorts are essential not only for academic purposes, but also for the generation of useful information for disease prognosis and even for the development of new therapeutic approaches.
Several therapeutic strategies are currently being developed for DMD.16 These include approaches not directly depending on DMD genotype of the patient, such as (i) myostatin blocking to increase fiber size and bulk, (ii) utrophin upregulation, to compensate the dystrophin deficiency and ameliorate symptoms, and (iii) gene therapy (‘viral’ and ‘non-viral’), with the aim of introducing a non-native functional copy of the DMD gene. Other strategies intend to restore the reading frame or correct the native dystrophin; these include (i) stop codon read-through drugs, such as gentamycin and ataluren (PTC124), (ii) exon skipping using antisense oligonucleotides and (iii) DMD gene modification with meganucleases or zinc finger nucleases. Some of these experimental treatments currently under clinical trials are considered personalized approaches in the sense that their application and effectiveness will depend on the DMD gene mutation and its effect at the mRNA/protein level. Patient selection and recruitment for these clinical trials are facilitated by the development of detailed disease registries. To that end, the network of excellence TREAT-NMD (Translational Research in Europe—Assessment and Treatment of Neuromuscular Diseases) has been promoting the creation of national registries in several European countries and worldwide.17 These national registries feed into a single global database managed by the network. For this integration, information regarding the DMD genotype profile of patients is required, as well as a clinical data set of items harmonized across all national registries.18
In this study, we present the profile of 39 unpublished DMD mutations detected in Portuguese patients in the course of our national diagnostic service. We exemplify the importance of detailed molecular characterization with special focus on the pitfalls and challenges regarding the molecular diagnosis of the dystrophinopathies.
Materials and methods
Patients
In the course of our genetic diagnostic service, provided on a national basis since 1989, 503 index cases/families were referred to our laboratory for DMD analysis. The present study describes a cohort of 312 unrelated cases (Supplementary Data I), with inclusion criteria based on compatible muscle biopsy, family history and/or clinical signs. It comprised 139 cases, including a female patient with irregular immunostaining for the three dystrophin domains (N-terminus, rod and C-terminus). The remaining 173 cases were selected on the basis of a highly suggestive clinical presentation and/or evidence of X-linked inheritance. These included two female relatives of deceased patients, who presented the at-risk haplotype.
The genetic studies had informed consent from the patients or their legal tutors, and laboratory registries were authorized by the National Committee for Data Protection.
Genomic DNA (gDNA) analysis
gDNA was extracted from peripheral blood by the salting-out method.19
The first studies relied on linkage analysis with polymorphic markers and Southern blotting and hybridization with cDNA probes.20 After 1991, this was preceded by deletion screening using two multiplex PCR reactions21, 22 for 18 DMD fragments (17 exons plus the muscle specific promoter Dp427m/exon1). As of 2005, initial deletion/duplication screening has been carried out by multiplex PCR and MLPA analysis, the latter substituting Southern blotting. The two multiplexed PCR mixes were adjusted to include a further two exons (namely 21 and 27). PCR products were labeled with FAM or NED fluorochromes and resolved on an ABI 3130xl capillary sequencer (Applied Biosystems, Foster City, CA, USA) using Genescan 500 size standards (Applied Biosystems), and data analyzed with GeneMapper v4.0 (Applied Biosystems). MLPA analysis was carried out using P034 and P035 kits (MRC Holland, Amsterdam, the Netherlands), according to the manufacturer’s recommendations. MLPA was done using 150 ng of gDNA obtained from peripheral blood, according to the manufacturer’s instructions. PCR products were run on an ABI 3130xl Genetic Analyzer (Applied Biosystems). The resulting fragments were analyzed by using GeneMarker v.1.5 software (Softgenetics, State College, PA, USA).
Detection of variants other than gross deletions or duplications, determination of breakpoint junctions and detailed characterization of mutations were carried out by partial or whole DMD gene sequencing—the latter introduced as a service in 2007. The 79 exonic sequences and flanking intronic borders were amplified by PCR using M13-tailed primers. Amplicons were purified with ExoSAP-IT® (USB, Cleveland, OH, USA) and sequenced using M13 universal primers and BigDyeTM Terminator Cycle Sequencing Kit V1.1 (Applied Biosystems). Products were resolved on an ABI 3130xl Genetic Analyzer and mutation analysis was aided by Seqscape V2.5 (Applied Biosystems).
cDNA analysis
Expression studies at the mRNA level were required for the delineation of breakpoint junctions, the identification of splicing changes or the detection of alterations caused by deep intronic mutations. Total RNA was isolated from cryopreserved muscle specimens using the PerfectPure RNA Fibrous Tissue Kit (5 Prime, Hamburg, Germany). cDNA was obtained using the High-capacity cDNA Reverse Transcription kit (Applied Biosystems). Specific primers were used to amplify either the mutated transcript region or the complete DMD cDNA sequence, using the bio-X-Act Long Range DNA polymerase kit (Bioline, Taunton, MA, USA). Resulting amplicons were sized on agarose gels and/or sequenced as described above.
Bioinformatics
For mutation nomenclature, the cDNA reference sequence NM_004006.2 was used, corresponding to DMD transcript Dp427m that encodes the main dystrophin protein found in skeletal muscle. Sequence variants were described following the recommendations of the Human Genome Variation Society.23 Variant description and impact on the reading-frame was confirmed with Mutalyzer.24 In our mutation validation strategy, we crosschecked each variant with the Human Genome Variation Society-listed Locus-Specific Database for DMD, available in the Leiden Muscular Dystrophy pages. This Locus-Specific Database is currently subdivided into two databases, one for whole exon changes25 (http://www.lovd.nl/DMD_d) and the other for smaller mutations12 (http://www.lovd.nl/DMD). For new point mutations, the Human Splicing Analyser software (http://www.umd.be/HSF/) was used for in silico evaluation of their possible effect on splicing.
Patient registry
The Portuguese patient registry was implemented using the Leiden Open Variation Database (LOVD) software version 2.0.26 LOVD was installed in a dedicated server, accessible only to the curators. Besides default LOVD columns, a set of custom database fields was used (listed in Supplementary data II), which included those defined by TREAT-NMD as mandatory or highly encouraged items in the network’s global DMD registry.
In the organization model (Supplementary Data III), three clinical coordinators from geographically dispersed major hospitals (north, center and south of the Country, to facilitate patient access) are assigned to the collection of personal, clinical and pathology data as well as to the promotion of the patients’ regular clinical (re)evaluation. Registry inclusion is completely voluntary and requires specific informed consent for registration purposes. All the information, namely, data sent by the clinician, signed consent forms and the genetic data obtained in the laboratory, is gathered by the registry curator and introduced in the D/BMD database after validation.
Results
Mutation profile
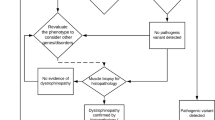
In our cohort of 312 unrelated cases selected on the basis of inclusion criteria for DMD analysis, an underlying mutation was identified in 284 (91%) cases. Among the remaining 28 cases, where no DMD mutation was detected, 19 had revealed dystrophin deficiency in the muscle biopsy (Supplementary Data I). In two of these, with irregular immunostaining for dystrophin, muscle specimens were available and were used for cDNA analysis, but still no alteration was identified.
The mutation distribution by type was found to be 67.9% (n=193) deletions, 15.2% (n=43) duplications and 16.9% (n=48) sub-exonic and sub-intronic (‘point’) mutations.
Overall, 175 different mutations were characterized, 39 of which were undocumented variants (Table 1) detected in patients and in a female obligate carrier with deceased DMD family members. The majority (n=24) of these new variants are point mutations that create premature termination codons. Among these are 13 small deletions, 5 mutations affecting splicing (4 of these are depicted in detail in Figure 1), 3 nonsense mutations, 2 deletion/insertions and 1 insertion. The remaining new variants correspond to gross deletions (n=8, where 4 are predictably in-frame) and duplications (n=7, where 2 are predictably in-frame). All 39 newly described variants were submitted to the DMD Locus-Specific Database available in the Leiden Muscular Dystrophy pages, as encouraged by the Human Variome Project.27
Importance of mRNA studies in DMD gene analysis. (a) In patient 36 (P36), a G to A substitution in the intronic 3′ splice site (intron 65) originated the skipping of exon 66. (b) In patient 34 (P34), a similar G to A substitution located in intron 63 originated a partial exon deletion because of the use of a cryptic exonic splice site. (c) Patient 18 (P18) presents a novel nonsense mutation in exon 25. Besides the transcript with the stop codon, a second transcript with an in-frame deletion (exon 25 skipping) is also produced. (d) Full complementary DNA sequencing showed a deep intronic substitution in patient 33 (P33). This change generates a stronger splice site score that completely overweighs that of the native splice site sequence, leading to the inclusion of a portion of intron 62 (46nt) at the mRNA level. gDNA, genomic DNA. A full color version of this figure is available at the Journal of Human Genetics journal online.
gDNA sequencing of the entire DMD gene was carried out in 50 unrelated individuals (including one female patient and two carriers). Among these, muscle specimens were available for cDNA studies in 17 cases where further characterization was considered necessary. These included 12 cases with new variants and 2 with known mutations but where their effect at the mRNA level had not been described.
Overall, complete or targeted gDNA and cDNA sequencing enabled the detailed characterization of 44 cases with point mutations, mainly of the splicing, nonsense and frameshift types (small deletions or duplications). Four examples taken from the newly detected variants (Table 1) are shown in Figure 1. In patient 36, the c.9564-1G>A mutation abolishes the 3′ splice site of intron 65 causing skipping of exon 66 (Figure 1a). A similar mutation in patient 34 (c.9287-1G>A) located in intron 63 originates a partial exonic deletion at the mRNA level (Figure 1b). Although nonsense mutations are usually only studied at the gDNA level, they too may have additional and unsuspected effects on splicing. This is exemplified with patient 18 (Figure 1c), where, besides the predicted transcript with a stop codon (r.3281u>a), there is also residual production of a second transcript with an in-frame deletion that results from skipping of exon 25. This finding is in agreement with the apparently intermediate phenotype observed in the patient, who has shown a slowly progressive clinical course. The fourth example shows how full cDNA sequencing enabled the identification of the deep intronic mutation c.9224+9192C>A in patient 33 (Figure 1d). This single-nucleotide substitution promotes the inclusion of a small portion of intron 62 at the mRNA level, predictably originating a truncated polypeptide (p.His3076Leufs*37).
In four cases, targeted gDNA sequencing enabled the identification of the underlying cause of changes initially detected by MLPA (n=3) and multiplex PCR (n=1, patient 12 in Table 1 and Figure 2).
DMD deletions undetected by Multiplex Ligation-Probe Amplification (MLPA). (a) Southern blotting and hybridization using HindIII-digested genomic DNA (gDNA) and complementary DNA (cDNA) probe 30-222 showing a deletion of exon 17 and the presence of a junction fragment (patient 12 (P12) in Table 1). This fragment also elucidated the carrier status of the patient’s mother (P12 mother). (b) No amplification was obtained for the fragment corresponding to exon 17 using the multiplex PCR technique. (c) MLPA analysis revealed the presence of exon 17 (probe P035). (d) Targeted gDNA sequencing revealed a deletion encompassing the last 220 nucleotides of intron 16 and the first 8 nucleotides of exon 17. (e) Schematic representation of resulting transcript. cDNA analysis confirmed that this mutation compromises the splicing process of the intron 16/exon17 boundary: the deletion encompasses the 3′consensus region (including the native AG splice site and the branch point), such that the pre-mRNA processing resorts to a cryptic acceptor splice site located upstream in intron 16. A full color version of this figure is available at the Journal of Human Genetics journal online.
Genotyping pitfalls
The molecular diagnosis of our patients revealed potential genotyping pitfalls owing to either technical limitations and/or genetic heterogeneity. With MLPA, false negatives may result from partial exonic deletions that are not coincident with the ligation site of the respective exonic probes, as exemplified in Figure 2. In this case, both Southern blotting followed by hybridization with a cDNA probe (Figure 2a) and multiplex PCR (Figure 2b) suggested a deletion of exon 17 in patient 12. In contrast, MLPA results were not compatible with a deletion (Figure 2c). This apparent discrepancy was sorted out by genomic sequencing, where a 228-bp deletion that includes intron 16 and exon 17 was detected (Figure 2d). As the acceptor splice site was included in the deleted region, the mutation was further characterized at the mRNA level. Results demonstrated that normal splicing is compromised and that a cryptic acceptor splice site located upstream in intron 16 is alternatively used (Figure 2e). The resulting polypeptide would be truncated, if produced.
False-positive results with MLPA mainly arise from inadequate probe hybridization because of the presence of sequence variants (polymorphisms or point mutations) in targeted regions. Two representative cases are depicted in Figure 3. In the first, MLPA analysis suggested a deletion of exon 51 in patient 27. However, gDNA sequencing revealed a single base pair deletion (c.7425delC) in the ligation site for the respective MLPA probe (Figure 3a). The second case (not listed in Table 1) is one where, rather than absence, a signal reduction was observed with the MLPA probe for exon 70. Upon sequencing, this was explained by the presence of a nonsense mutation (Figure 3b), responsible for the observed sub-optimal ligation of the probe.
Point mutations initially identified by Multiplex Ligation-Probe Amplification (MLPA) as single exonic deletions. (a) MLPA analysis revealed a deletion of exon 51 in patient 27 (P27; Table 1). Direct sequencing of exon 51 showed a frameshift mutation (p.Phe2475Leufs*19) in the ligation site for the respective MLPA probe. (b) In another patient (not listed in Table 1), an apparent reduction of amplification with the exon 70 probe was observed. When sequenced, a previously reported nonsense mutation (p.Arg3391*) was detected in this exon, coincident with the probe’s ligation site. A full color version of this figure is available at the Journal of Human Genetics journal online.
The high mutation rate of the DMD locus can also induce errors in genotyping. One such situation that may be overlooked is the presence of two distinct mutations running in the same family where, as exemplified in Figure 4a, the pedigree reflects the apparently normal X-linked transmission of a single mutation. In this family, referral was triggered by the request for prenatal diagnosis in a woman with family history of DMD, whose affected brother and maternal uncle were already deceased. A deletion encompassing exons 17 and 18 was identified in the male fetus (IV-1 in Figure 4a), but the pregnancy was carried to term as the same deletion (Figure 4b) was also detected in the fetus’ 11-year-old maternal cousin (patient 13 in Table 1, IV-2 in Figure 4a), who was clinically asymptomatic except for elevated creatine kinase levels. This newly documented mutation is consistent with the BMD phenotype as it is not predicted to cause a frameshift, according to the ‘reading-frame rule’. More recently, an affected male first-cousin (patient 28 in Table 1, IV-3 in Figure 4a) presenting clinical features of DMD was referred for molecular studies. At 7 years of age, he presented physical and cognitive developmental delay, limb and facial muscle weakness and difficulty to stand-up. However, in this patient a distinct (and also novel) gross DMD deletion was detected, encompassing exons 52–78. This in-frame deletion extends into the cysteine-rich and also carboxy-terminal portion of the protein, which is essential for proper dystrophin function. The loss of these functional domains might explain the DMD phenotype. In view of these findings, all family members available for study were genetically reanalyzed. Interestingly, the mothers of all three patients (sisters III-4, -6 and -8) were found to be carriers of both mutations, one on each of the parental X chromosomes (Figures 4a and c). In light of these new genetic findings, the clinical reevaluation of these females was encouraged; however, there has been no further follow-up. Figure 5 shows a co-occurrence of two DMD mutations in the same patient (not listed in Table 1). This is an example of a patient with a severe DMD phenotype, presenting with delayed developmental and intellectual milestones, becoming wheelchair-bound by the age of 7 years. On referral for molecular diagnosis, two distinct changes were detected by MLPA: a gross deletion involving exons 46–50 and deletion of exon 79 (Figure 5a). Genomic sequencing of exon 79 revealed a deletion of 13 base pairs in the 3′-untranslated region (c.*23_*35del, Figure 5b). This mutation is located within the genomic sequence recognized by the MLPA probe, thereby explaining the absence of amplification of exon 79. Transcript analysis in the muscle specimen confirmed the presence of both alterations, designated as r.[6615_7309del; *23_*35del]. Although the former is a well-documented and recurrent out-of-frame mutation that also compromises expression of the Dp140 isoform, the *23_*35del mutation has been reported only twice in patients with a DMD-type phenotype.28, 29 This change lies in a highly conserved part of the 3′-untranslated region of DMD and predictably disrupts the reading frame of the Dp71b isoform (NM_004016.2), thought to have an important role during human neural development.30 Moreover, as Dp71b and Dp140 are expressed in the CNS, the loss of both isoforms may have a cumulative effect on brain development,30, 31 thereby explaining the patient’s mental impairment.
Two independent DMD mutations identified in one family. (a) Pedigree showing an X-linked transmission but also the presence of two different mutations associated with different phenotypes. (b) Southern blotting and hybridization using the complementary DNA probe 30-2 (genomic DNA digested with BglII and HindIII), revealing a deletion of exons 17 and 18 in individual IV-2 (patient 13 (P13)). (c) Multiplex Ligation-Probe Amplification (MLPA) analysis of a female carrier (III-4) showing the presence of both deletions (compound heterozygosity). BMD, Becker Muscular Dystrophy; DMD, Duchenne Muscular Dystrophy. A full color version of this figure is available at the Journal of Human Genetics journal online.
Two distinct DMD mutations identified in the same patient. (a) Multiplex Ligation-Probe Amplification (MLPA) analysis shows deletions of exons 46–50 and of exon 79. (b) Genomic DNA sequencing of exon 79 revealed a deletion of 13 nucleotides in a conserved part of the 3′-untranslated region (UTR), presumed to alter an alternative open reading frame that normally gives rise to transcripts lacking exon 78.29, 39 (c) Patient’s mother presenting only the small 3′UTR deletion. A full color version of this figure is available at the Journal of Human Genetics journal online.
Patient registry
The detailed clinical and molecular data collected and described in this work for a significant number of dystrophinopathy families and the new emergent mutation-based therapies, motivated the authors to develop a national registry for patients affected with D/BMD, in collaboration with the TREAT-NMD network. The registry database is based on the LOVD system and is located in the ‘Centro de Genética Médica Dr. Jacinto Magalhães’, presently the genetics service of a public central hospital. The Portuguese registry follows the TREAT-NMD charter for patient database/registry, abiding by National and European legislation concerning data protection. Before implementation, this project was submitted for approval by the Institutional Ethics Committee and was granted authorization by the National Committee for Data Protection. The registry was launched in 2012 and since then the clinical coordinators have been actively gathering data from D/BMD patients. Until now (April 2014), only a small fraction of patients (n=18) have been included in the database.18
Regarding the registry’s data content: (i) the average patients’ age is 11.8 years; (ii) all patients, except one, have truncating mutations in the DMD gene; (iii) 11 patients still maintain independent ambulation; (iii) on average the beginning of wheelchair use is 10 years of age; and (iv) 4 patients require noninvasive artificial ventilation.
Discussion
In the cohort totaling 312 unrelated cases that met the inclusion criteria for suspected dystrophinopathy, 284 were confirmed and characterized at the molecular level, corresponding to a mutation detection rate of 91%. Among the 28 cases with no DMD mutation detected, 19 had a muscle biopsy, which was compatible with D/BMD. Some of these are still likely to be dystrophinopathies because the molecular techniques used are not exhaustive for mutation detection. However, abnormal immunostaining for dystrophin may represent a secondary deficiency, particularly in disorders with overlapping clinical signs, as is often the case in certain sarcoglycanopathies.32 Indeed, out of all 503 index cases referred for DMD testing since 1989, 22 cases were subsequently diagnosed with sarcoglycanopathy, and a further 10 were diagnosed with other forms of muscular dystrophy or myopathy.
DMD mutation proportions by type were found to be in agreement with that reported in the literature for large cohorts, with gross deletions in approximately 70% of the cases and with gross duplications and point mutations being equally accountable for the remainder.
A total of 175 different mutations were identified in our cohort, 39 (22%) of which had not been described previously. In this subset, the apparent discrepancy in mutation type proportions, with our higher frequency of new point mutations as compared with new large deletions and duplications, reflects a past sub-representation of point mutations in databases and mutation reports in the literature.
gDNA sequence-based interpretation alone may fail to predict the correct mutation outcome, even with the aid of bioinformatics algorithms. Some of the new variants in the present report are used to illustrate the importance of mRNA studies in helping to elucidate the mutation effect on RNA processing, to delineate breakpoint junctions and often to provide explanations for apparent exceptions to the reading-frame rule. In addition, transcript analysis may enable the detection of deep intronic splicing mutations that otherwise remain undetected or with unknown pathogenicity.
In our patient cohort, several cases highlighted the importance of extensive molecular studies for accurate diagnosis and concomitant appropriate genetic counseling. These potential pitfalls are either consequent to technical limitations or derive from the genetic heterogeneity of the DMD locus.
It is recognized that limitations due to sensitivity and experimental design of the various diagnostic techniques may lead to false-negative or false-positive results. As shown in the examples provided, these and other technical pitfalls may be avoided by combining different methodologies with complementary specificities. Indeed, our standard operating procedures in internal quality control for disease-specific molecular diagnoses include, whenever possible, a second alternative and complementary technique.
Genetic heterogeneity constitutes a second factor that can lead to erroneous diagnostic conclusions. Current international guidelines for D/BMD propose that carrier screening and prenatal testing should be orientated toward (thus limited to) the mutation previously identified in the index case.33 However, as shown here, the presence of the same molecular defect in all clinically affected family members should not be presumed categorically, even if the pedigree appears to follow a typical X-linked pattern of inheritance. Clinical diagnosis should be considered definitive only after the molecular confirmation using strategies with a complementary and/or wider scope of mutation detection, and all possible carriers should be tested in cascade.
The co-occurrence of two DMD mutations in the same patient is also exemplified. Here, the patient’s mother was found to carry only one of the mutations, namely c.*23_*35del, but not the gross deletion of exons 46–50, thereby posing a dilemma for counseling and prenatal diagnosis. Further studies in other family members may help elucidate the degree of pathogenicity contributed by each variant, especially the 3′-untranslated region point mutation. Nonetheless, if only the common exon 46–50 deletion had been screened in the mother, her carrier status would have been incorrectly ascertained.
The detection of such cases is more problematic, as in practice it implies performing extensive screening of the DMD gene in each patient. To avoid this pitfall, physicians who request DMD screening, and genetic counselors in particular, should be aware of the specificity of the tests performed in each case and of their respective limitations.
Besides enabling a definitive diagnosis, obtaining a detailed genotype is particularly relevant for both candidate selection and treatment outcome evaluation in light of the emergent mutation-directed therapies for DMD, which are currently under clinical trials. In 2007, TREAT-NMD initiated a global patient registry for DMD.17 This international database network cooperation functions with a twofold purpose—the patient profiles facilitate industry decision-making and simultaneously the trial-ready data contribute to the effectiveness of patient recruitment. This global database collects from national registries, thus each participating country adopted the same data set of mandatory items that are transversal in patient studies. Follow-up and clinical progression are updated regularly, ideally at least once a year.
Three basic models have been used for the deployment of DMD registries: (i) a patient self-report system (DuchenneConnect Registry Report;34 United Dystrophinopathy Project35), where the patient or legal tutor replies to a specific disease questionnaire; (ii) a clinical reporting system (UMD-DMD database;10 Czech DMD/BMD registry36), insuring that the data are collected and validated by physicians and molecular geneticists, or (iii) a mixed model that combines both strategies (New Zealand Duchenne Muscular Dystrophy Registry;37 Japanese Registry of Muscular Dystrophy—Remudy38). The Portuguese DMD registry is currently using the clinical reporting model, which at the time was considered the most adequate, after discussions with professional groups and with the neuromuscular patients’ association. However, the small number of patients registered thus far warrants reevaluation of this model, in an effort to facilitate and ensure a more widespread access of patients to the registry. One measure that is underway is the reference of the registry in all mutation-positive molecular reports. The implementation of clinical trial-sites for DMD in Portugal may also motivate patient registration. Some patients have been recruited on an individual basis, with the help of their clinicians, to ongoing clinical trials in other European countries. However, this strategy does not ensure equitable patient access to the trials. Considering the overall numbers for D/BMD patients in Portugal reported in this work, which were gathered through the genetic studies performed over the last two and a half decades, we believe it is justified to have an operational DMD registry in the country, as well as one or more clinical trial sites for this disease. Finally, the registry data itself can act as an important clinical and epidemiological research tool, to follow the natural history of the disease and to estimate the prevalence of D/BMD in our country.
References
Emery, A. E. Population frequencies of inherited neuromuscular diseases: a world survey. Neuromuscul. Disord. 1, 19–29 (1991).
Bushby, K. M., Thambyayah, M. & Gardner-Medwin, D. Prevalence and incidence of Becker muscular dystrophy. Lancet 337, 1022–1024 (1991).
Bresolin, N., Castelli, E., Comi, G. P., Felisari, G., Bardoni, A., Perani, D. et al. Cognitive impairment in Duchenne muscular dystrophy. Neuromuscul. Disord 4, 359–369 (1994).
Cotton, S., Voudouris, N. J. & Greenwood, K. M. Intelligence and Duchenne muscular dystrophy: full-scale, verbal, and performance intelligence quotients. Dev. Med. Child. Neurol. 43, 497–501 (2001).
Koenig, M., Hoffman, E. P., Bertelson, C. J., Monaco, A. P., Feener, C. & Kunkel, L. M. Complete cloning of the Duchenne muscular dystrophy (DMD) cDNA and preliminary genomic organization of the DMD gene in normal and affected individuals. Cell 50, 509–517 (1987).
Yoshida, M. & Ozawa, E. Glycoprotein complex anchoring dystrophin to sarcolemma. J. Biochem. 108, 748–752 (1990).
Ervasti, J. M. & Campbell, K. P. Membrane organization of the dystrophin-glycoprotein complex. Cell 66, 1121–1131 (1991).
Ervasti, J. M. & Campbell, K. P. Dystrophin-associated glycoproteins: their possible roles in the pathogenesis of Duchenne muscular dystrophy. Mol. Cell Biol. Hum. Dis. Ser 3, 139–166 (1993).
Laing, N. G. In Molecular and Cell Biology of Muscular Dystrophy ed Partridge T. A., 37–84 (Chapman & Hall: London, 1993).
Tuffery-Giraud, S., Béroud, C., Leturcq, F., Yaou, R. B., Hamroun, D., Michel-Calemard, L. et al. Genotype-phenotype analysis in 2,405 patients with a dystrophinopathy using the UMD-DMD database: a model of nationwide knowledgebase. Hum. Mutat. 30, 934–945 (2009).
Monaco, A. P., Bertelson, C. J., Liechti-Gallati, S., Moser, H. & Kunkel, L. M. An explanation for the phenotypic differences between patients bearing partial deletions of the DMD locus. Genomics 2, 90–95 (1988).
Aartsma-Rus, A., Van Deutekom, J. C., Fokkema, I. F., Van Ommen, G. J. & den Dunnen, J. T. Entries in the Leiden Duchenne muscular dystrophy mutation database: an overview of mutation types and paradoxical cases that confirm the reading-frame rule. Muscle Nerve 34, 135–144 Review (2006).
Ferlini, A., Neri, M. & Gualandi, F. The medical genetics of dystrophinopathies: Molecular genetics diagnosis and its impact on clinical practice. Neuromuscul. Disord. 23, 4–14 (2013).
Takeshima, Y., Yagi, M., Okizuka, Y., Awano, H., Zhang, Z., Yamauchi, Y. et al. Mutation spectrum of the dystrophin gene in 442 Duchenne/Becker muscular dystrophy cases from one Japanese referral center. J. Hum. Genet. 55, 379–388 (2010).
Kesari, A., Pirra, L. N., Bremadesam, L., McIntyre, O., Gordon, E., Dubrovsky, A. L. et al. Integrated DNA, cDNA, and protein studies in Becker muscular dystrophy show high exception to the reading frame rule. Hum. Mutat. 29, 728–737 (2008).
Pichavant, C., Aartsma-Rus, A., Clemens, P. R., Davies, K. E., Dickson, G., Takeda, S. et al. Current status of pharmaceutical and genetic therapeutic approaches to treat DMD. Mol. Ther. 19, 830–840 (2011).
Bushby, K., Lynn, S. & Straub, T. TREAT-NMD Network. Clinical outcome measures for trials in Duchenne muscular dystrophy: report from International Working Group meetings. Acta. Myol. 28, 12–15 (2009).
Bladen, C. L., Rafferty, K., Straub, V., Monges, S., Moresco, A., Dawkins, H. et al. The TREAT-NMD Duchenne muscular dystrophy registries: conception, design and utilization by industry and academia. Hum. Mutat 34, 1449–1457 (2013).
Miller, S. A., Dykes, D. D. & Polesky, H. F. A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res. 16, 1215 (1988).
Curtis, A. & Haggerty, D. In Muscular Dystrophy: Methods and Protocols eds Bushby K., Anderson L. V., 53–84 (Humana Press: Totowa, NJ, 2001).
Beggs, A. H., Koenig, M., Boyce, F. M. & Kunkel, L. M. Detection of 98% of DMD/BMD gene deletions by polymerase chain reaction. Hum. Genet. 86, 45–48 (1990).
Chamberlain, J. S., Gibbs, R. A., Ranier, J. E. & Caskey, C. T. In PCR Protocols: A Guide to Methods and Applications eds Innis M. A., Gelfand D. H., Sninsky J. J., White T. J., pp 272–281 (Academic Press: San Francisco, CA, 1990).
den Dunnen, J. T. & Antonarakis, S. E. Nomenclature for the description of human sequence variations. Hum. Genet. 109, 121–124 (2001).
Wildeman, M., van Ophuizen, E., den Dunnen, J. T. & Taschner, P. E. Improving sequence variant descriptions in mutation databases and literature using the Mutalyzer sequence variation nomenclature checker. Hum. Mutat. 29, 6–13 (2008).
White, S. J. & den Dunnen, J. T. Copy number variation in the genome; the human DMD gene as an example. Cytogenet. Genome Res 115, 240–246 Review (2006).
Fokkema, I. F., Taschner, P. E., Schaafsma, G. C., Celli, J., Laros, J. F., den Dunnen, J. T. et al. LOVD v.2.0: the next generation in gene variant databases. Hum. Mutat. 32, 557–563 (2011).
Howard, H. J., Beaudet, A., Gil-da-Silva Lopes, V., Lyne, M., Suthers, G., van den Akker, P. et al. Disease-specific databases: Why we need them and some recommendations from the Human Variome Project Meeting, May 28, 2011. Am. J. Med. Genet. 158 A, 2763–2766 (2012).
Nigro, V., Nigro, G., Esposito, M. G., Comi, L. I., Molinari, A. M., Puca, G. A. et al. Novel small mutations along the DMD/BMD gene associated with different phenotypes. Hum. Mol. Genet 3, 1907–1908 (1994).
Spitali, P., Rimessi, P., Fabris, M., Perrone, D., Falzarano, S., Bovolenta, M. et al. Exon skipping-mediated dystrophin reading frame restoration for small mutations. Hum. Mutat. 30, 1527–1534 (2009).
Moizard, M. P., Billard, C., Toutain, A., Berret, F., Marmin, N. & Moraine, C. Are Dp71 and Dp140 brain dystrophin isoforms related to cognitive impairment in Duchenne muscular dystrophy? Am. J. Med. Genet. 80, 32–41 (1998).
Taylor, P. J., Betts, G. A., Maroulis, S., Gilissen, C., Pedersen, R. L., Mowat, D. R. et al. Dystrophin gene mutation location and the risk of cognitive impairment in Duchenne muscular dystrophy. PLoS One 5, e8803 (2010).
dos Santos, M. R., Jorge, P., Ribeiro, E. M., Pires, M. M. & Guimarães, A. Novel mutation (Y184C) in exon 4 of the beta-sarcoglycan gene identified in a Portuguese patient. Hum Mutat. 12, 214–215 (1998).
Abbs, S., Tuffery-Giraud, S., Bakker, E., Ferlini, A., Sejersen, T. & Mueller, C. R. Best practice guidelines on molecular diagnostics in Duchenne/Becker muscular dystrophies. Neuromuscul. Disord 20, 422–427 (2010).
Rangel, V., Martin, A. S. & Peay, H. L. DuchenneConnect Registry Report. Version 2. PLoS Curr 4, RRN1309 (2012).
Flanigan, K. M., Dunn, D. M., von Niederhausern, A., Soltanzadeh, P., Gappmaier, E., Howard, M. T. et al. Mutational spectrum of DMD mutations in dystrophinopathy patients: application of modern diagnostic techniques to a large cohort. Hum. Mutat. 30, 1657–1666 (2009).
Brabec, P., Vondrácek, P., Klimes, D., Baumeister, S., Lochmüller, H., Pavlík, T. et al. Characterization of the DMD/BMD patient population in Czech Republic and Slovakia using an innovative registry approach. Neuromuscul. Disord 19, 250–254 (2009).
Rodrigues, M., Hammond-Tooke, G., Kidd, A., Love, D., Patel, R., Dawkins, H. et al. The New Zealand neuromuscular disease registry. J. Clin. Neurosci. 19, 1749–1750 (2012).
Nakamura, H., Kimura, E., Mori-Yoshimura, M., Komaki, H., Matsuda, Y., Goto, K. et al. Characteristics of Japanese Duchenne and Becker muscular dystrophy patients in a novel Japanese national registry of muscular dystrophy (Remudy). Orphanet J. Rare Dis. 8, 60 (2013).
Ceccarini, M., Rizzo, G., Rosa, G., Chelucci, C., Macioce, P. & Petrucci, T. C. A splice variant of Dp71 lacking the syntrophin binding site is expressed in early stages of human neural development. Brain Res. Dev. Brain Res. 103, 77–82 (1997).
Acknowledgements
We thank all the patients/families and referring clinicians for their collaboration. The authors are indebted to Professor Hans Lochmüller (TREAT-NMD network) for assistance in setting up the patient registry, as well as to Dr Johan den Dunnen and Ivo Fokkema (Leiden University Medical Center) for the respective database platform.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Journal of Human Genetics website
Supplementary information
Rights and permissions
About this article
Cite this article
Santos, R., Gonçalves, A., Oliveira, J. et al. New variants, challenges and pitfalls in DMD genotyping: implications in diagnosis, prognosis and therapy. J Hum Genet 59, 454–464 (2014). https://doi.org/10.1038/jhg.2014.54
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2014.54
This article is cited by
-
EMQN best practice guidelines for genetic testing in dystrophinopathies
European Journal of Human Genetics (2020)
-
Exon skipping induced by nonsense/frameshift mutations in DMD gene results in Becker muscular dystrophy
Human Genetics (2020)
-
Normal and altered pre-mRNA processing in the DMD gene
Human Genetics (2017)