Abstract
This study was to describe the use of inverted-L osteotomy of ramus and iliac bone graft for the management of mandibular deficiency in adult patients. From 2008 to 2010, 11 patients (aged 19 to 29 years) with mandibular deficiency underwent intraoral or extraoral inverted-L osteotomy of ramus and iliac crest bone grafting. Data were collected from the patients’ records, photographs and radiographs. The height and width of the ramus were successfully expanded by inverted-L osteotomy and iliac crest bone grafting with minimal complications in all patients, resulting in significant improvement in occlusion and facial appearance. Our early results showed that the inverted-L osteotomy of ramus and iliac crest bone grafting is safe and effective, and should be considered as a good alternative for the patients with mandibular deficiency.
Similar content being viewed by others
Introduction
Mandibular deficiency is a common encountered problem in craniofacial surgery. Different methods have been used to correct mandibular deficiency; however, there is some debate regarding the ideal treatment of mandibular deficiency. The bilateral sagittal split ramus osteotomy is the most common surgical procedure for mandibular deficiency because of its versatility and its amenability to rigid fixation.1,2,3 However, there is a variable but considerable risk of inferior alveolar nerve injury when performing this procedure.4,5,6 In addition, a greater risk of relapse is present when this procedure is used to advance the mandible or correct skeletal open-bite deformities.7,8
Intraoral inverted-L osteotomy (ILO) is a surgical procedure used to correct mandibular prognathism.9,10,11 In 1985, Dattilo et al.12 reported to correct skeletal class II (retrognathic) open-bite deformities using the extraoral ILO technique. In 1999, McMillan et al.13 used this technique to advance the mandible in patients with mandibular deficiency by an intraoral approach. These studies suggested that the ILO should be considered as a surgical option for mandibular deficiency. Unfortunately, we still lack knowledge concerning the clinical effects of this approach because the relevant reports are limited. In this study, we present our data on a clinical and radiographic follow-up on 11 patients with mandibular deficiency and try to evaluate the clinical effects with ILO for mandibular reconstruction.
Patients and methods
Between January 2008 and December 2010, 11 patients with mandibular deficiency underwent intra- or extraoral ILO and iliac crest bone grafting at the Department of Oral and Maxillofacial Surgery in West China Hospital of Stomatology, Sichuan University. There were seven female and four male with a mean age of 24.3 years (range, 19–29 years). In these 11 patients, causes included hemifacial microsomia, posttraumatic hypoplasia, temporomandibular joint ankylosis with hypoplasia, and the first and second branch arch syndrome. All patients enrolled in this study underwent intra- or extraoral ILO because of the high relapse or difficulty of saggital split of ramus osteotomy (SSRO). Among these patients, six patients underwent extraoral ILO as they have skin scars at the submandibular area caused by the former surgery. For the rest of the patients, intraoral ILO was performed. The relevant details about these patients were summarized in Table 1. Each subject in this study signed a detailed informed consent form.
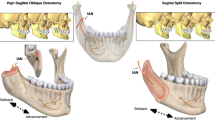
Intraoral or extraoral ILO and iliac crest bone grafting
For the patients via an intraoral approach, Lidocaine 2% with 1∶100 000 epinephrine was infiltrated in the ramus area of the mandible. An intraoral subgingival incision was made, extending from the second premolar to the anterior border of the ramus. A mucoperiosteal flap was elevated inferiorly and posteriorly to expose the lateral aspect of the mandibular body, angle and ramus. The inferior insertion of the temporal muscle on the anterior ramus and coronoid process was stripped using a periosteal elevator. A Kocher clamp was placed on the tip of the coronoid process to aid in retraction and the medial dissection was done as for a sagittal ramus osteotomy, extending just distal to the lingula. The horizontal cut was then made above and behind the lingula with the inferior alveolar nerve using a reciprocating saw. Then an oscillating saw was used to complete the vertical cut from the inferior border of the mandible to the previously made horizontal osteotomy of the ramus (Figure 1a). A thin chisel was carefully inserted to separate the proximal and distal segments. After the completion of surgery on the opposite side, the mandible was advanced and moved to the new position. The desired occlusion was achieved with the final wafer and intermaxillary fixation. The condylar segment is seated centrally in the fossa using gentle upward pressure from the area of the horizontal cut. An iliac crest bone graft was trimmed and placed at the interface of the proximal and distal segments (Figure 1b). Two four-hole ‘L’ miniplates were placed by the transbuccal approach, one at the anterior border and the other at the angle (Figure 1c). Similar surgical procedures were used for the patients underwent extraoral ILO (Figure 2).
The wound was then irrigated with antibiotic solution and closed over a suction drain which was removed 48 h later. A compression dressing was also applied for 5 days. All patients had presurgical orthodontic treatment to level and align the dental arches. Postoperative maxillomandibular fixation commenced on the second day after surgery, and continued for a period of 2–4 weeks.
Other procedures
Various concomitant procedures were also performed including Le Fort I osteotomy in nine patients, sagittal split ramus osteotomy on the opposite side in nine and advancement sliding genioplasty in 11 (Table 1).
Outcome assessment
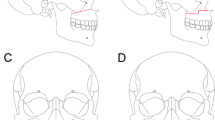
The clinical criteria used for evaluation of the patients included frontal, lateral and panoramic radiography and medical photography. The lines and points used to collect data were shown in Figure 3. A line ‘W’ representing the ramus width was drawn at the level of the second lower molar. A vertical line ‘H’ representing the ramus height was drawn perpendicular to the previous line from midpoint of the sigmoid notch to inferior margin of the ramus. By comparing the values of H and W obtained from the preoperative and postoperative cephalometric phtotographs, the amount of horizontal and vertical movement created by surgery could be measured.
Results
All patients tolerated the surgical procedures well without severe complications. Rami treated by ILO were expanded in both width and height. Horizontal and vertical changes of early results were shown in Table 1. Horizontal movement ranged from 5.4 to 12.5 mm (average=8.003 5 mm), and vertical movement ranged from 8.6 to 15.5 mm (average=11.6 mm) immediately after surgery. The follow-up time was from 7 to 14 months (average=9.7 months). The measurement at the different follow-up further demonstrated the stability of ramus width (average=8.4 mm) and height (average=11.5 mm). Only one of the patients reported mild levels of hypoesthesia after operation, which was disappeared at 1 month postoperatively. Two cases via an extraoral approach showed temporary facial nerve paresis but recovered after 1 to 3 months postoperatively. There was no permanent facial nerve damage. All of the patients involved had significant improvements in occlusion and aesthetic appearances postoperatively.
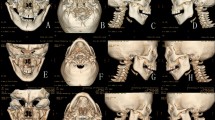
Representative case
A 23-year-old male patient presented with temporomandibular joint (TMJ) ankylosis in the right side and severe facial asymmetry. He underwent right extraoral ILO and iliac bone graft to move the affected mandible anteriorly and inferiorly, and other surgeries including Lefort I osteotomy to bring the shortened hemimaxilla down and level the occlusal canting, SSRO on the left side to set back the mandible, genioplasty to advance and bring the chin to the midline. Significant improvements in facial symmetry were achieved as shown in Figure 4. Considerable increase in height and width of her affected mandible was shown in the panoramic radiography (Figure 5).
Photographs of a 23-year-old man with right-sided TMJ ankylosis treated with left extraoral ILO and iliac bone graft to move the ramus anteriorly and inferiorly, right SSRO, genioplasty and Lefort I osteotomy. (a) The frontal view pre-operatively; (b) the frontal view 7 months postoperatively. ILO, inverted-L osteotomy; SSRO, saggital split of ramus osteotomy. TMJ, temporomandibular joint.
Discussion
Although several articles have been written on the use of ILO for correcting mandibular prognathism, we still lack relevant data on the use of this procedure for mandibular deficiency. In this study, the mandibular deficiency was corrected by ILO and iliac bone graft and satisfactory outcomes were achieved in all patients. These results suggest that ILO and iliac bone graft should be considered as a good alternative for the treatment of mandibular deficiency.
ILO can be performed via an extraoral or intraoral approach.12,13 Although it is easier to perform extraorally, it needs skin incision and thus reduces the appeal of the procedure on aesthetic grounds. In this study, six patients underwent extraoral ILO as they have skin scars at the submandibular area caused by the former surgery. The difficulty for intraoral ILO lies in the positioning of the condylar segment and intraoperative rigid fixation.13,14,15 The surgeon performing this operation should be familiar with intraoral ramus osteotomies and transbuccal fixation. Although the osteotomy and rigid fixation usually takes twice as long as a bilateral sagittal split osteotomy, this avoids the external scar that may be of great concern to the patients and significantly shortens the time of maxillomandibular fixation postoperatively. Van Sickels et al.15 described the use of positioning plates to stabilize the condylar segment in patients with mandibular prognathism. However, we feel that this was not necessary for the patients with mandibular deficiency, because the inserted bone graft made bony segment control and placement of rigid fixation easier.
Controversy continues regarding the best way to correct the mandibuar deficiency. The SSRO is the most common surgical procedure for mandibular deficiency because of its versatility and its amenability to rigid fixation. Compared with SSRO, the advantages of ILO are apparent. First of all, ILO can move the mandible inferiorly and anteriorly and thus increase the height and width of the ramus simultaneously. Second, previous studies revealed that the patients who undergo ILO had a lesser incidence of neurosensory disturbance than the BSSO because the osteotomy is performed without exposing the inferior alveolar nerve, by making horizontal and vertical osteotomies just superior and posterior to the mandibular foramen.16,17 Therefore, ILO is more appealing for patients who are concerned about neurosensory injuries. Third, some patients with mandibular deficiency usually have a deformed ramus. On this condition there is a clear preference towards the use of ILO rather than SSRO, because it is hard or impossible to split such a ramus. Finally, previous results indicated that ILO may have more stability in both the horizontal and vertical dimensions than other ramus procedures in the patients with skeletal open-bite deformities.12,13,14,15 The use of interpositional bone grafts and rigid fixation may play a role in the relatively low percentage of relapse.
Distraction osteogenesis is another relatively simple technique that allows for correction of the mandibular deficiency with minimal morbidity.18,19 However, it can also lead to a wide variety of complications, particularly the long treatment period and possible fibrous union or nonunion impeding its further clinical application.20,21 In addition, simultaneously vertical and horizontal elongation of the ramus is needed in the patients presented in this study, but it is hard to use the technique of distraction osteogenesis to move the mandible accurately at these two dimensions.
In conclusion, the results in the present study showed that ILO and iliac crest bone grafting is safe and effective, and should be considered as a good alternative for the patients with mandibular deficiency.
References
Baek RM, Lee SW . A new condyle repositionable plate for sagittal split ramus osteotomy. J Craniofac Surg 2010; 21( 2): 489–490.
Ueki K, Marukawa K, Shimada M et al. Condylar and disc positions after sagittal split ramus osteotomy with and without Le Fort I osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 103( 3): 342–348.
Hwang K, Nam YS, Han SH . Vulnerable structures during intraoral sagittal split ramus osteotomy. J Craniofac Surg 2009; 20( 1): 229–232.
Kohn MW . Analysis of relapse after mandibular advancement surgery. J Oral Surg 1978; 36( 9): 676–684.
Poulton DR, Ware WH . Surgical-orthodontic treatment of severe mandibular retrusion. Am J Orthod 1973; 63( 3): 237–255.
Rubens B, Stoelinga P, Blijdorp P et al. Skeletal stability following sagittal split osteotomy using monocortical miniplate internal fixation. Int J Oral Maxillofac Surg 1988; 17( 6): 371–376.
Leira JI, Gilhuus-Moe OT . Sensory impairment following sagittal split osteotomy for correction of mandibular retrognathism. Int J Adult Orthod Orthognath Surg 1991; 6( 3): 161–167.
Coghlan KM, Irvine GH . Neurological damage after sagittal split osteotomy. Int J Oral Maxillofac Surg 1986; 15( 4): 369–371.
Hall HD, Chase DC, Payor LG . Evaluation and refinement of the intraoral vertical subcondylar osteotomy. J Oral Surg 1975; 33( 5): 333–341.
Hall HD, McKenna SJ . Further refinement and evaluation of intraoral vertical ramus osteotomy. J Oral Maxillofac Surg 1987; 45( 8): 684–688.
Tuinzing DB, Greebe RB . Complications related to the intraoral vertical ramus osteotomy. Int J Oral MaxilIofac Surg 1985; 14( 4): 319–324.
Dattilo DJ, Braun TW, Sotereanos GC . The inverted L osteotomy for treatment of skeletal open-bite deformities. J Oral Maxillofac Surg 1985; 43( 6): 440–443.
McMillan B, Jones R, Ward-Booth P et al. Technique for intraoral inverted ‘L’ osteotomy. Br J Oral Maxillofac Surg 1999; 37( 4): 324–326.
Muto T, Akizuki K, Tsuchida N et al. Modified intraoral inverted ‘L’ osteotomy: a technique for good visibility, greater bony overlap, and rigid fixation. J Oral Maxillofac Surg 2008; 66( 6): 1309–1315.
Van Sickels JE, Tiner BD, Jeter TS . Rigid fixation of the intraoral inverted ‘L’ osteotomy. J Oral Maxillofac Surg 1990; 48( 8): 894–898.
Naples RJ, Van Sickels JE, Jones DL . Long-term neurosensory deficits associated with bilateral sagittal split osteotomy versus inverted ‘L’ osteotomy. Oral Surg Oral Med Oral Pathol 1994; 77( 4): 318–321.
Kobayashi A, Yoshimasu H, Kobayashi J et al. Neurosensory alteration in the lower lip and chin area after orthognathic surgery: bilateral sagittal split osteotomy versus inverted L ramus osteotomy. J Oral Maxillofac Surg 2006; 64( 5): 778–784.
Qi MC, Zou SJ, Han LC et al. Expression of bone-related genes in bone marrow MSCs after cyclic mechanical strain: implications for distraction osteogenesis. Int J Oral Sci 2009; 1( 3): 143–150.
Chopra S, Enepekides DJ . The role of distraction osteogenesis in mandibular reconstruction. Curr Opin Otolaryngol Head Neck Surg 2007; 15( 4): 197–201.
Kanellopoulos AD, Soucacos PN . Management of nonunion with distraction osteogenesis. Injury 2006; 37 ( Suppl 1): S51–S55.
Wijbenga JG, Verlinden CR, Jansma J et al. Long-lasting neurosensory disturbance following advancement of the retrognathic mandible: distraction osteogenesis versus bilateral sagittal split osteotomy. Int J Oral Maxillofac Surg 2009; 38( 7): 719–725.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Zhu, SS., Feng, G., Li, JH. et al. Correction of mandibular deficiency by inverted-L osteotomy of ramus and iliac crest bone grafting. Int J Oral Sci 4, 214–217 (2012). https://doi.org/10.1038/ijos.2012.75
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijos.2012.75
Keywords
This article is cited by
-
A Clinical Re-Evaluation of an Unexplored Technique for Post Gap Arthroplasty Retrognathic Mandible
Journal of Maxillofacial and Oral Surgery (2022)
-
Combined Bimaxillary Distraction Osteogenesis Associated with Orthognathic Surgery for Hemifacial Microsomia in Adults
Aesthetic Plastic Surgery (2017)
-
Bimaxillary Orthognathic Approach to Correct Skeletal Facial Asymmetry of Hemifacial Microsomia in Adults
Aesthetic Plastic Surgery (2016)