Abstract
Background:
Evidence suggests that dietary calcium intake may be inversely related to body weight. One explanatory mechanism is that dietary calcium increases fecal fat excretion, due to either calcium soap formation and/or binding of bile acids (BAs) in the intestine.
Objective:
To examine the effect of calcium from low-fat dairy products on fecal fat excretion.
Design:
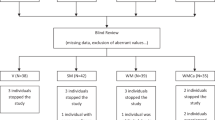
A randomized crossover study with 11 subjects, comparing two 7-d diets: one high in calcium from low-fat dairy products (high-Ca; 2300 mg Ca per d) and one low in calcium (low-Ca; 700 mg Ca per d).
Measurements:
All feces were collected during the last 5 days of each diet period and analyzed for fat, energy and calcium content and fatty acid (FA) and BA composition.
Results:
Dairy calcium significantly increased the total fecal fat excretion from 5.4±0.5 g d−1 on the low-Ca diet to 11.5±1.4 g d−1 on the high-Ca diet (P<0.001). The fecal energy excretion increased almost correspondingly. Saturated, monounsaturated and polyunsaturated FAs were all excreted in larger amounts on the high-Ca diet (P<0.001 for all), with the effect of calcium being greater for monounsaturated than for saturated FAs. The fecal excretion of BAs was unaffected of calcium intakes.
Conclusions:
Increasing the intake of calcium from low-fat dairy products by 1600 mg d−1 for 7 days doubled total fecal fat excretion, but did not affect the excretion of BAs. The results may partially explain why a high-calcium diet can produce weight loss.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
McCarron DA, Morris C, Henry H, Stanton J . Blood pressure and nutrient intake in the United States. Science 1984; 224: 1392–1398.
Zemel MB, Shi H, Greer B, DiRienzo D, Zemel PC . Regulation of adiposity by dietary calcium. FASEB J 2000; 14: 1132–1138.
Davies KM, Heaney RP, Recker RR, Lappe JM, Barger-Lux MJ, Rafferty K et al. Calcium intake and body weight. J Clin Endocrinol Metab 2000; 85: 4635–4638.
Heaney RP, Davies KM, Barger-Lux MJ . Calcium and weight: clinical studies. J Am Coll Nutr 2002; 21: 152S–155S.
Zemel MB, Thompson W, Milstead A, Morris K, Campbell P . Calcium and dairy acceleration of weight and fat loss during energy restriction in obese adults. Obes Res 2004; 12: 582–590.
Zemel MB . The role of dairy foods in weight management. J Am Coll Nutr 2005; 24 (suppl_6): 537S–546S.
Zemel MB, Richards J, Mathis S, Milstead A, Gebhardt L, Silva E . Dairy augmentation of total and central fat loss in obese subjects. Int J Obes 2005; 29: 391–397.
Bowen J, Noakes M, Clifton PM . Effect of calcium and dairy foods in high protein, energy-restricted diets on weight loss and metabolic parameters in overweight adults. Int J Obes 2005; 29: 957–965.
Gunther CW, Legowski PA, Lyle RM, McCabe GP, Eagan MS, Peacock M et al. Dairy products do not lead to alterations in body weight or fat mass in young women in a 1-y intervention. Am J Clin Nutr 2005; 81: 751–756.
Harvey-Berino J, Gold BC, Lauber R, Starinski A . The impact of calcium and dairy product consumption on weight loss. Obes Res 2005; 13: 1720–1726.
Haub M, Simons T, Cook C, Remig V, Al-Tamimi E, Holcomb C . Calcium-fortified beverage supplementation on body composition in postmenopausal women. Nutr J 2005; 4: 21.
Reid IR, Horne A, Mason B, Ames R, Bava U, Gamble GD . Effects of calcium supplementation on body weight and blood pressure in normal older women: a randomized controlled trial. J Clin Endocrinol Metab 2005; 90: 3824–3829.
Shapses SA, Heshka S, Heymsfield SB . Effect of calcium supplementation on weight and fat loss in women. J Clin Endocrinol Metab 2004; 89: 632–637.
Thompson WG, Rostad Holdman N, Janzow DJ, Slezak JM, Morris KL, ZEMEL MB . Effect of energy-reduced diets high in dairy products and fiber on weight loss in obese adults. Obes Res 2005; 13: 1344–1353.
Behling A, Kaup S, Choquette L, Greger J . Lipid absorption and intestinal tumour incidence in rats fed on varying levels of calcium and butterfat. Br J Nutr 1990; 64: 505–513.
Yuangklang C, Wensing T, Lankhorst AE, Lemmens AG, Fielmich-Bouman XM, Jittakhot S et al. Cholate and deoxycholate counteract the calcium-induced lowering of fat digestion in rats. J Anim Physiol Anim Nutr 2005; 89: 337–341.
Govers MJ, Termont D, Van Aken G . Characterization of the adsorption of conjugated and unconjugated bile acids to insoluble amorphous calcium phosphate. J Lipid Res 1994; 35: 741–748.
Van der Meer R, Welberg J, Kuipers F, Kleibeuker JH, Mulder N, Termont DSML et al. Effects of supplemental dietary calcium on the intestinal association of calcium, phosphate, and bile acids. Gastroenterology 1990; 99: 1653–1659.
Jacobsen R, Lorenzen JK, Toubro S, Krog-Mikkelsen I, Astrup A . Effect of short-term high dietary calcium intake on 24-h energy expenditure, fat oxidation, and fecal fat excretion. Int J Obes 2005; 29: 292–301.
Shahkhalili Y, Murset C, Meirim I, Duruz E, Guinchard S, Cavadini C et al. Calcium supplementation of chocolate: effect on cocoa butter digestibility and blood lipids in humans. Am J Clin Nutr 2001; 73: 246–252.
Lutwak L, Laster L, Gitelman H, Fox M, Whedon G . Effects of high dietary calcium and phosphorus on calcium, phosphorus, nitrogen and fat metabolism in children. Am J Clin Nutr 1964; 14: 76–82.
Welberg J, Monkelbaan J, de Vries E, Muskiet F, Cats A, Oremus E et al. Effects of supplemental dietary calcium on quantitative and qualitative fecal fat excretion in man. Ann Nutr Metab 1994; 38: 185–191.
Govers MJ, Termont DSML, Lapre JA, Kleibeuker JH, Vonk R, van der Meer R . Calcium in milk products precipitates intestinal fatty acids and secondary bile acids and thus inhibits colonic cytotoxicity in humans. Cancer Res 1996; 56: 3270–3275.
Boon N, Hul GBJ, Stegen JHCH, Sluijsmans WEM, Valle C, Langin D et al. An intervention study of the effects of calcium intake on faecal fat excretion, energy metabolism and adipose tissue mRNA expression of lipid-metabolism related proteins. Int J Obes 2007; 31: 1704–1712.
Denke M, Fox M, Schulte MC . Short-term dietary calcium fortification increases fecal fat. J Nutr 1993; 123: 1047.
Lefevre M, Kris-Etherton PM, Zhao G, Tracy RP . Dietary fatty acids, hemostasis, and cardiovascular disease risk. J Am Diet Assoc 2004; 104: 410–419.
Cummings J, Jenkins D, Wiggins H . Measurement of the mean transit time of dietary residue through the human gut. Gut 1976; 17: 210–218.
Bingham S, Cummings J . Urine nitrogen as an independent validatory measure of dietary intake: a study of nitrogen balance in individuals consuming their normal diet. Am J Clin Nutr 1985; 42: 1276–1289.
Mølgaard C, Sandström B, Michaelsen K . Evaluation of a food frequency questionnaire for assesssing of calcium, protein and phosphorus intakes in children and adolescents. Scand J Nutr 1998; 42: 2–5.
Møller A, Saxholt E, Christensen AT, Hartkopp HB, Hess Ygil K . Danish Food Composition Databank, revision 6.0. Food Informatics, Institute of Food Safety and Nutrition, Danish Institute for Food and Veterinary Research. June 2005. Website: http://www.foodcomp.dk/, 2006.
Alexander J, Andersen S, Aro A, Becker W, Fogelholm M, Lyhne N . et al. Nordic Nutrition Recommendations 2004. Integrating Nutrition and Physical Activity, 4th edn. Norden: Copenhagen, 2004.
Baecke J, Burema J, Frijters J . A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr 1982; 36: 936–942.
Norman A . Intestinal calcium absorption: a vitamin D-hormone-mediated adaptive response. Am J Clin Nutr 1990; 51: 290–300.
Allen L . Calcium bioavailability and absorption: a review. Am J Clin Nutr 1982; 35: 783–808.
Bingham S, Cummings J . The use of 4-aminobenzoic acid as a marker to validate the completeness of 24 h urine collections in man. Clin Sci 1983; 64: 629–635.
Bligh EG, Dyer WJ . A rapid method of total lipid extraction and purification. Can J Biochem Physiol 1959; 37: 911–917.
Dekker R, van der Meer R, Olieman C . Sensitive pulsed amperometric detection of free and conjugated bile acids in combination with gradient reversed-phase HPLC. Chromatographia 1991; 31: 549–553.
Knarreborg A . The Impact of Microbial Deconjugation of Bile Salts on Fat Digestion in Broiler Chickens. The Royal Veterinary and Agricultural University: Frederiksberg Denmark, 2002.
Ditscheid B, Keller S, Jahreis G . Cholesterol metabolism is affected by calcium phosphate supplementation in humans. J Nutr 2005; 135: 1678–1682.
Lupton JR, Steinbach G, Chang W, O'Brien B, Wiese S, Stoltzfus C et al. Calcium supplementation modifies the relative amounts of bile acids in bile and affects key aspects of human colon physiology. J Nutr 1996; 126: 1421–1428.
Lorenzen JK, Nielsen S, Holst J, Tetens I, Rehfeld J, Astrup A . Effect of dairy calcium and supplementary calcium intake on postprandial fat metabolism, appetite, and subsequent energy intake. Am J Clin Nutr 2007; 85: 678–687.
Guerciolini R, Radu-Radulescu L, Boldrin M, Dallas J, Moore R . Comparative evaluation of fecal fat excretion induced by orlistat and chitosan. Obes Res 2001; 9: 364–367.
Mu H, Høy C-E . The digestion of dietary triacylglycerides. Prog Lipid Res 2004; 43: 105–133.
Acknowledgements
We are grateful to the laboratory and kitchen staff at the Department of Human Nutrition, especially I Timmermann, C Kostecki and Y Rasmussen, for their assistance. JK Lorenzen, NT Bendsen, A-L Hother and A Astrup designed the study. NT Bendsen and A-L Hother were responsible for collection of data and for analyzing the dietary and fecal samples. M Würtz is gratefully acknowledged for assistance with fat and FA analysis and so is L Hymøller for the HPLC part of the BA analysis. NT Bendsen and A-L Hother performed the data analysis. All authors participated in the discussion of the results and commented on the paper. The study was supported by the British Broadcasting Corporation (BBC).
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflicts of interest
A Astrup is a member of Arla Nutrition Advisory Board, The Global Dairy Platform, and receives an honorarium for each board meeting. NT Bendsen, A-L Hother, SK Jensen and JK Lorenzen have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Bendsen, N., Hother, AL., Jensen, S. et al. Effect of dairy calcium on fecal fat excretion: a randomized crossover trial. Int J Obes 32, 1816–1824 (2008). https://doi.org/10.1038/ijo.2008.173
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2008.173
Keywords
This article is cited by
-
Effect of reduced-calcium and high-calcium cheddar cheese consumption on the excretion of faecal fat: a 2-week cross-over dietary intervention study
European Journal of Nutrition (2023)
-
Evaluation of risk factors for insulin resistance: a cross sectional study among employees at a private university in Lebanon
BMC Endocrine Disorders (2020)
-
High phosphorus intake and gut-related parameters – results of a randomized placebo-controlled human intervention study
Nutrition Journal (2018)
-
Whey protein lowers systolic blood pressure and Ca-caseinate reduces serum TAG after a high-fat meal in mildly hypertensive adults
Scientific Reports (2018)
-
Supplementation with dairy calcium and/or flaxseed fibers in conjunction with orlistat augments fecal fat excretion without altering ratings of gastrointestinal comfort
Nutrition & Metabolism (2017)