Abstract
Obstructive sleep apnea syndrome (OSAS) may predispose patients to congestive heart failure, suggesting a deleterious effect of OSAS on myocardial contractility. We investigated whether essential hypertensive individuals with OSAS are characterized by decreased right and left ventricular myocardial performance. Our study population consisted of 45 consecutive patients with newly diagnosed untreated stage I–II essential hypertension suffering from OSAS (35 men, aged 49±8 years) and 48 hypertensives without OSAS, matched for age, sex, level of blood pressure, heart rate, body mass index and smoking status. All subjects underwent polysomnography and echocardiography. Right and left ventricular functions were evaluated using the myocardial performance index (MPI). Right and left ventricular functions were altered in hypertensives with OSAS. The mean right MPI was 0.26±0.11 in hypertensives without OSAS and 0.51±0.16 in hypertensives with OSAS (P<0.01). The mean left MPI values were 0.29±0.07 and 0.44±0.13, respectively (P<0.01). Right and left MPI correlated positively and significantly with apnea-hypopnea index (ρ=0.40, P=0.002).OSAS is associated with impaired right and left ventricular function. These phenomena were independent of hypertension.
Similar content being viewed by others
Introduction
Obstructive sleep apnea syndrome (OSAS) is characterized by repetitive collapse of the upper airway during sleep.1 The obstructive apneic event is associated with considerable breathing efforts against a totally or partially occluded upper airway, and apnea is terminated by an arousal and heavy snoring as airflow is restored. Severity of OSAS is described according to the total number of apneas and hypopneas per hour of sleep, which is named as the apnea-hypopnea index (AHI).
Obstructive sleep apnea syndrome is highly prevalent, affecting an estimated 20% of the adult population. Cardiovascular disturbances are the most serious complications of OSAS. These complications include heart failure, acute myocardial infarction, nocturnal arrhythmias, stroke and systemic and pulmonary hypertension. All these cardiovascular complications increase the morbidity and the mortality of OSAS.2
Currently, sleep apnea is accepted as one of the identifiable causes of hypertension.3 In clinical practice, ventricular function is evaluated commonly using echocardiography to measure systolic and diastolic functions. The myocardial performance index (MPI) incorporates parameters of both systolic and diastolic functions, and therefore might be a more accurate and reflective measure of global ventricular function.4 The MPI has been shown to be a valid, reproducible and simple noninvasive method to estimate global right and left ventricular functions, with important prognostic implications.5, 6
In this study, we sought to estimate the right and left ventricular myocardial performance and other commonly used echocardiographic parameters in patients with newly diagnosed essential hypertensives with or without OSAS. We hypothesized that hypertensives with OSAS have impaired right and left ventricular myocardial performance when compared with control subjects, independent of hypertension.
Methods
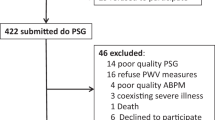
Study population
Our study population consisted of 45 consecutive patients (age range 37–65 years) with newly diagnosed (<2 years) untreated and uncomplicated stage I–II essential hypertension and presented with clinical evidence of OSAS. The latter was based on the Epworth sleepiness scale questionnaire with high scores (ESS 10). Office blood pressure measurements were obtained by a mercury sphygmomanometer, according to the recent guidelines of the Chinese Society of Hypertension. All subjects underwent the usual clinical and laboratory tests to rule out secondary and complicated hypertension.7, 8
Exclusion criteria
Exclusion criteria were as follows: (1) any cardiovascular disease or syncope, rhythm or conduction abnormalities, diabetes mellitus, familial hypercholesterolemia and any other clinically significant concurrent medical condition, such as renal, hepatic or gastrointestinal illness; (2) to exclude chronic respiratory diseases (obstructive or restrictive), chest X-ray, arterial blood gas analysis and a spirometry test were performed; (3) patients with an estimated pulmonary systolic pressure of ⩾45 mm Hg; (4) subjects with proteinuria detectable by dipstick; (Any participant receiving hypolipidemic agents for at least 1 month before entry into the protocol and women on long-term estrogen replacement therapy were not included in this study.) (5) chronic severe alcoholism; (6) suboptimal echocardiographic images for measurements; (7) lack of patient authorization for clinical research.
Finally, 45 essential hypertensive patients fulfilled the above criteria and were selected for participation in this study.
A control group of 48 hypertensive individuals without clinical evidence of OSAS matched for age, sex, level of blood pressure, heart rate (HR), body mass index (BMI) and smoking status were selected from our pool.
Polysomnography study
Polysomnography was carried out on all subjects on the night of diagnosis.9 Subjects were asked not to eat for 4 h before the study and to refrain from tea, coffee and alcohol consumption.10 Data were collected and stored on an Alice-4 (Healthdyne/Respironics Inc., Murrysville, PA, USA) recording computerized system. The following variables were recorded: central referential electroencephalogram, bilateral electroculogram, submental and anterior tibialis electromyogram, electrocardiogram with precordial surface electrodes, nasal and oral airflow measured by thermistors and nasal pressure transducers, respiratory movements of rib cage and abdomen with piezosensor bands and arterial saturation with finger pulse oxymeter. Sleep staging and arousals were measured using standard methods.11, 12 Obstructive apneas were defined as a cessation of airflow for at least 10 s in the presence of thoracoabdominal efforts, and hypopneas were defined as significant reductions in airflow for at least 10 s accompanied by oxyhemoglobin desaturation of 2% from baseline. All studies were interpreted by a board-certified sleep specialist. The obstructive AHI was defined according to the American Academy of Sleep Medicine Task Force clinical research criteria13, as the number of apnea plus hypopnea episodes per hour of sleep. The lowest AHI class (<5) was defined as normal.14 Oxygen saturation before polysomnography and the lower oxygen saturation value (minSatO2) were also recorded.
Echocardiography
The echocardiographic study was performed using a Philips iE33 ultrasound imager equipped with a 2.5–5 MHz transducer. All measurements were performed with the subjects in the left lateral decubitus position by M-mode, two dimensional and Doppler ultrasound echocardiography. The duration of the examination was 20 min. The ventricular diameters, (EDD, dimensions in end diastole) volumes and functions were measured according to the recommendations of the American Society of Echocardiography.15 Basic measurements of left ventricular dimensions in diastole and systole, thickness of IVS (interventricular septum), LVPW (left ventricular posterior wall) and left ventricular mass (LVM) were measured by the M-mode technique, and LVM was divided by body surface area to obtain the LVMI (LVM index). Left ventricular EF was calculated by the Simpson's method. Early (E) and atrial (A) transmitral maximal flow velocities, the ratio (E/A) and deceleration time of E-wave were registered. The left and right ventricular MPI was calculated as (isovolumic contraction time of the right/left ventricle+isovolumetric relaxation time of right/left ventricle)/pulmonary–aortic ejection time. Fractional area change was calculated as (end-diastolic area–end-systolic area)/end-diastolic area for the right and left ventricle in the apical four-chamber view. Three consecutive beats were measured and averaged for each measurement. In this protocol, the echocardiographic study was carried out by experienced senior operators who were blinded to the clinical status of the subject. Five random measurements were repeated 1 week, after the first measurements, to calculate the intraobserver variability of echocardiographic measurements including MPI, whereas for the interobserver variability, five random echocardiographic measurements were made by two persons. The percentage of variation in the means and s.e. of the measurements was compared using a paired t-test.
Laboratory and anthropometric measurements
Venous blood samples were obtained from each participant after overnight fasting, just after the polysomnography study for the determination of glucose, lipid profile and hemoglobin, according to established methods.
Physical examination was carried out on all subjects. Systolic and diastolic blood pressures were measured consecutively in the sitting position on the right arm using a mercury sphygmomanometer, after 5 min of rest. The mean of the two measurements was used for analysis. Hypertension was defined as blood pressure ⩾140/90 mm Hg. HR per minute was measured in the sitting position, and the BMI of the patients was calculated as weight divided by height squared (kg m–2).
Statistical analysis
The SPSS statistical package, release 11.0 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses. Owing to the skewed distribution, AHI values were logarithmically (log 10) transformed before statistical testing. Significant differences between the study subgroups were determined using the Student independent samples t-test or the chi-squared test where appropriate. Correlation analysis was performed using Pearson's correlation coefficient. To assess the relative strength of association of AHI and left MPI, multiple step-wise regression analysis was applied to hypertensive subjects with OSAS. Descriptive statistics were arithmetic means±s.d. or medians (range) for skewed data. Statistical significance was set at P<0.05.
Results
On the basis of the polysomnography study findings, our final hypertensive OSAS group consisted of 42 subjects with AHI class >5 (out of 45 with high clinical evidence of OSAS), and our final hypertensive-without-OSAS group consisted of 45 subjects with a negative polysomnography study (out of 48 without high clinical evidence of OSAS, two subjects refused to undergo the study).
As selected initially, the two groups of hypertensive subjects with and without OSAS were matched for age, sex, level of blood pressure, HR, BMI and smoking status (Table 1). As expected by definition in the OSAS hypertensive group, log AHI values were increased by 1.48±0.36 episodes/h (P=0.0001), minSatO2 was lower by 17±7% (P=0.0001), whereas oxygen saturation during wakefulness was similar in the two groups (Table 2).
Hypertensive subjects with OSAS compared with those without OSAS did not differ in hemoglobin levels, fasting serum glucose, triglycerides, total cholesterol and low- and high-density lipoprotein cholesterol levels (P=NS for all cases) (Table 2).
Reproducibility of echocardiographic measures
For patients with right ventricular MPI, the interobserver and intraobserver variability were 5.8 and 4.9%, respectively, whereas they were 3.6 and 2.1%, respectively, for patients with left ventricular MPI.
Basic echocardiographic measurements
Basic echocardiographic measurements of the left ventricle in the two groups are shown in Table 3. The left ventricular end-diastolic and end-systolic diameters were not statistically different between the two groups. In patients withOSAS, thickness of IVS, LVPW, LVM and LVMI were higher. Left atrial diameter was significantly higher in hypertensive patients with OSAS than in those without OSAS (P<0.01).
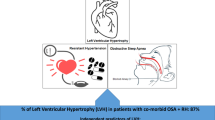
Association between OSAS and left ventricular function
The left ventricular systolic and diastolic functions in patients with OSAS are shown in Table 3. The left ventricular systolic function (EF and fractional shortening) and the diastolic function were not significantly different in the two groups and were in normal limits. The left ventricular MPI was significantly higher in patients with OSAS (0.44±0.13) than in those without OSAS (0.29±0.07; P<0.001). A positive correlation was shown between left ventricular MPI and AHI. Correlation between MPI and log AHI in OSAS patients is shown in Figure 1, (r=0.522, P<0.001).
Multiple step-wise regression analysis of left MPI
Using the multiple step-wise regression analysis of left MPI as a dependent variable, and LVM, left atrial volume, EDD, lowest oxyhemoglobin saturation and log AHI as independent variables, only log AHI and LVM were found to be independent predictors of the left MPI in hypertensive patients with OSAS (adjusted r2=0.489) (Table 4).
Association between OSAS and right ventricular function
Echocardiographic measurements in the right ventricle and the P-values for trend are displayed in Table 3. There was an impaired global right ventricular function measured by the MPI across severity of patients with OSAS. Figure 2 shows the significant and positive correlation between right ventricular MPI and AHI (=0.583; P<0.001). The systolic function measured by the fractional area change was impaired in hypertensive patients with OSAS.
The mean and lowest oxyhemoglobin saturation percentages were not related to any of the echocardiographic measures of the right and left ventricles across the AHI groups (P>0.05 for all).
Discussion
In our study, diabetes mellitus and coronary artery disease were excluded, and there was no significant difference in age, BMI and level of blood pressure of the patients. We found that IVS and LVPW diameters, and left ventricular hypertrophy (LVH), LVM and LVMI, were slightly higher in hypertensive patients with OSAS. A multivariate analysis should have been used in a large study population, to explain the effects of blood pressures or hypoxemia on LVH. Hedner et al.16 reported that OSAS causes LVH in a study that compared 61 males with OSAS with 61 male control subjects. The OSAS group was heavier and 50% had systemic hypertension. They reported that LVM was 15% higher among normotensive OSAS patients compared with that in normotensive control subjects, despite comparison of subjects with matching BMI. More recently, Noda et al.17 reported echocardiographic evidence of LVH in 50% of patients with an AHI>20 h–1 compared with 21.4% in those with an AHI <20 h–1. In contrast, Davies et al.18 did not find a significant difference in LVM, determined by echocardiography, between 19 patients with OSAS, 19 nonapneic snorers and 38 control subjects matched for age, sex and BMI. In our study, blood pressure level was matched, so we conclude that OSAS can cause LVH.
The proposed causes of LVH in OSAS include associated changes in left ventricular afterload, intermittent hypoxemia and recurrent arousals during sleep. Left ventricular afterload increases during sleep in patients with OSAS because of the combined effects of increased negative intrathoracic pressure, associated with attempted breathing against an occluded upper airway,19 and increased systemic blood pressure20, 21 associated with elevated sympathetic nervous system activity, hypoxemia and arousal from sleep.22
As the systolic and diastolic dysfunctions coexist frequently , it was shown that a combined measure of ventricular performance with calculation of MPI might be more reflective of overall cardiac dysfunction than systolic or diastolic measures alone. Our study shows an association between the severity of AHI and decreased right and left ventricular performance in patients with newly diagnosed systolic–diastolic essential hypertension with OSAS. The impairment in the left and right ventricular myocardial performance was most evident in patients with newly diagnosed systolic–diastolic essential hypertension without OSAS. We also showed that the left atrial diameter was increased significantly in patients with newly diagnosed systolic–diastolic essential hypertension with OSAS.
Association between OSAS and right ventricular dysfunction
There are several factors related closely to OSAS that can affect right ventricle structure and function, including obesity, elevations in the intrathoracic negative pressure related to apneic events and nocturnal increases in pulmonary vascular resistance, all of which have been related to impaired right ventricular filling and diastolic dysfunction. Earlier studies23, 24, 25 assessing right ventricular function in patients with OSAS have been controversial and have had important limitations, including the use of right ventricular measurements with poor reproducibility, nonblinded measures, lack of a control group for comparisons and inadequate adjustment for known confounders.
In an earlier study, Dursunoglu et al.26 studied global right ventricular function using the MPI in patients with OSAS, who had no history of cardiac and lung diseases. This study reported an excellent correlation between the right ventricular MPI and AHI (r=0.84; P<0.001). After adjusting for some known confounders, including pulmonary systolic pressure and BMI, the correlation between global right ventricular dysfunction and AHI diminished but remained significantly correlated (=0.40; P=0.002) in Abel et al.'s study. That study supported the notion that obesity and pulmonary pressures are also important contributors to right ventricular dysfunction in patients with OSAS. For the association between OSAS and right ventricular ejection fraction, Sanner et al.27 have earlier reported in a sample of patients without cardiovascular and pulmonary diseases, a significant negative correlation between AHI and right ventricular ejection fraction measured by radionuclide ventriculography (r=−0.24; P<0.01).
In our study, the two groups were matched for age, sex, BMI and absence of any chronic respiratory diseases (obstructive or restrictive) and absence of pulmonary hypertension. We found a good correlation between the right ventricular MPI and AHI. Our study did not reach statistical significance between right fractional area change and AHI, which was similar to Abel et al.'s outcome. We found that the right ventricular function was related to the AHI and not to the lowest oxyhemoglobin saturation, suggesting that the pathophysiological interactions between OSAS and right ventricular function could be related more to the number of apneic events and the changes in the intrathoracic negative pressure, rather than primarily to oxygen desaturation.28
Association between OSAS and left ventricular dysfunction
In this study, we found that global left ventricular function, measured by MPI is impaired in patients newly diagnosed with hypertension with OSAS compared with the control hypertension subjects without OSAS. Our findings confirm and extend the results from earlier investigators,29, 30, 31 who have found that left ventricular structure and function are affected in patients with OSAS. Global left ventricular function in patients with OSAS has been earlier reported. This study found a significant and positive correlation between the left ventricular MPI and AHI. However, in this study, the echocardiographic measures and analyses were not conducted blinded to polysomnography results. Nevertheless, this study is supportive of the notion that OSAS affects left ventricular function. In our study, LVH was founded in both groups. In a small sample of patients, Noda et al24 reported that OSAS is associated with LVH, possibly because of the long-standing hypertension associated with OSAS. In this study, we found that global function measured by MPI was impaired in hypertension patients with OSAS, and that AHI is an independent predictor for the left MPI. But other parameters, including systolic function, were not different between groups. These findings suggest that OSAS can affect left ventricular function independently.
Strengths and limitations
The strengths of our study include the availability of polysomnography data, which is the ‘gold standard’ for OSAS diagnosis, and the existence of a control group without OSAS. In addition, we obtained good reproducibility of measurements of MPI and fractional area change, which were carried out blinded to the polysomnography results. The limitations of this study include the fact that we used office blood pressure measurements instead of ambulatory monitoring to evaluate the blood pressure level. OSAS is associated generally with the disappearance of nocturnal blood pressure dipping. Second, the population of this study is rather limited and selective. Third, despite having adjusted our results for confounders such as BMI, office blood pressure and plasma lipid levels, an absolute causal relationship between OSAS and MPI could not be derived easily, possibly because of the observational nature of the study.
Conclusions
This study shows that increased AHI in patients with obstructive sleep apnea syndrome may result in biventricular dysfunction. In this study, a significant positive correlation was shown between MPI and AHI of obstructive sleep apnea syndrome. These phenomena were independent of hypertension.
Conflict of interest
The authors declare no conflict of interest.
Abbreviations
- AHI:
-
apnea-hypopnea index
- BMI:
-
body mass index
- CHF:
-
congestive heart failure
- IVSD:
-
interventricular septal distance
- LVH:
-
left ventricular hypertrophy
- LVM:
-
left ventricular mass
- LVPWT:
-
left ventricular posterior wall thickness
- MPI:
-
myocardial performance index
- OSAS:
-
obstructive sleep apnea syndrome.
References
Guilleminault C, Tilkian A, Dement WC . The sleep apnea syndromes. Annu Rev Med 1976; 27: 465–484.
Romero-Corral A, Somers VK, Pellikka PA, Olson EJ, Bailey KR, Korinek J, Orban M, Sierra-Johnson J, Kato M, Amin RS, Lopez-Jimenez F . Decreased right and left ventricular myocardial performance in obstructive sleep apnea. Chest 2007; 132: 1863–1870.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr JL, Jones DW, Materson BJ, Oparil S, Wright Jr JT, Roccella EJ, National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure and National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289: 2560–2572.
Tei C, Dujardin KS, Hodge DO, Kyle RA, Tajik AJ, Seward JB . Doppler index combining systolic and diastolic myocardial performance: clinical value in cardiac amyloidosis. J Am Coll Cardiol 1996; 28: 658–664.
Tei C, Ling LH, Hodge DO, Bailey KR, Oh JK, Rodeheffer RJ, Tajik AJ, Seward JB . New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function: a study in normals and dilated cardiomyopathy. J Cardiol 1995; 26: 357–366.
Tei C, Dujardin KS, Hodge DO, Bailey KR, McGoon MD, Tajik AJ, Seward SB . Doppler echocardiographic index for assessment of global right ventricular function. J Am Soc Echocardiogr 1996; 9: 838–847.
The JNC 7 Report. The seventh report of the joint national committee on prevention, detection, evaluation and treatment of high blood pressure. JAMA 2003; 289: 2560–2572.
European Society of Hypertension–European Society of Cardiology Guidelines Committee. 2003 European Society of Hypertension–European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens 2003; 21: 1011–1153.
Indications for Polysomnography Task Force, American Sleep Disorders Association Standards of Practice Committee. Practice parameters for the indications for polysomnography and related procedures. Sleep 1997; 20: 406–422.
García-Río F, Racionero MA, Pino JM, Martínez I, Ortuño F, Villasante C, Villamor J . Sleep apnea and hypertension. Chest 2000; 117: 1417–1425.
Rechtschaffen A, Kales A . A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. 1968 US Goverment Printing Office. Washington DC: NIH Publication No. 204.
American Sleep Disorders Association. EEG arousals: scoring rules and examples; a preliminary report from the Sleep Disorders Atlas Task Force of the American Sleep Disorders Association. Sleep 1992; 15: 173–184.
The Report of an American Academy of Sleep Medicine Task Force. Sleep related breathing disorders in adults. Sleep 1999; 22: 667–689.
Whitney CW, Gottlieb DJ, Redline S, Norman RG, Dodge RR, Shahar E, Surovec S, Nieto FJ . Reliability of scoring respiratory disturbance indexes and sleep staging. Sleep 1998; 21: 749–757.
Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, Gutgesell H, Reichek N, Sahn D, Schnittger I . Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr 1989; 2: 358–367.
Hedner J, Ejnell H, Caidahl K . Left ventricular hypertrophy independent of hypertension in patients with obstructive sleep apnea. J Hypertens 1990; 8: 941–946.
Noda A, Okada T, Yasuma F, Nakashima N, Yokota M . Cardiac hypertrophy in obstructive sleep apnea syndrome. Chest 1995; 107: 1538–1544.
Davies RJ, Crosby J, Prothero A, Stradling JR . Ambulatory blood pressure and left ventricular hypertrophy in subjects with untreated obstructive sleep apnea and snoring, compared with matched control subjects, and their response to treatment. Clin Sci 1994; 86: 417–424.
Buda AJ, Pinsky MR, Ingels Jr NB, Daughters II GT, Stinson EB, Alderman EL . Effect of intrathoracic pressure on left ventricular performance. N Engl J Med 1979; 301: 453–459.
Hedner J, Ejnell H, Sellgren J, Hedner T, Wallin G . Is high and fluctuating muscle nerve sympathetic activity in the sleep apnoea syndrome of pathogenetic importance for the development of hypertension? J Hypertens 1988; 6: 529–531.
Noda A, Nakata S, Fukatsu H, Yasuda Y, Miyao E, Miyata S, Yasuma F, Murohara T, Yokota M, Koike Y . Aortic pressure augmentation as a marker of cardiovascular risk in obstructive sleep apnea syndrome. Hypertens Res 2008; 31: 1109–1114.
Dursunoglu D, Dursunoglu N, Evrengül H, Ozkurt S, Kuru O, Kiliç M, Fisekci F . Impact of obstructive sleep apnoea on left ventricular mass and global function. Eur Respir J 2005; 26: 283–288.
Guidry UC, Mendes LA, Evans JC, Levy D, O’Connor GT, Larson MG, Gottlieb DJ, Benjamin EJ . Echocardiographic features of the right heart in sleep-disordered breathing: the Framingham Heart Study. Am J Respir Crit Care Med 2001; 164: 933–938.
Noda A, Okada T, Yasuma F, Nakashima N, Yokota M . Cardiac hypertrophy in obstructive sleep apnea syndrome. Chest 1995; 107: 1538–1544.
Weitzenblum E, Chaouat A . Sleep and chronic obstructive pulmonary disease. Sleep Med Rev 2004; 8: 281–294.
Dursunoglu N, Dursunoglu D, Kiliç M . Impact of obstructive sleep apnea on right ventricular global function: sleep apnea and myocardial performance index. Respiration 2005; 72: 278–284.
Sanner BM, Konermann M, Sturm A, Müller HJ, Zidek W . Right ventricular dysfunction in patients with obstructive sleep apnoea syndrome. Eur Respir J 1997; 10: 2079–2083.
Lopez-Jimenez F, Somers VK . Stress measures linking sleep apnea, hypertension and diabetes: AHI vs arousals vs hypoxemia. Sleep 2006; 29: 743–744.
Sidana J, Aronow WS, Ravipati G, Di Stante B, McClung JA, Belkin RN, Lehrman SG . Prevalence of moderate or severe left ventricular diastolic dysfunction in obese persons with obstructive sleep apnea. Cardiology 2005; 104: 107–109.
Niroumand M, Kuperstein R, Sasson Z, Hanly PJ . Impact of obstructive sleep apnea on left ventricular mass and diastolic function. Am J Respir Crit Care Med 2001; 163: 1632–1636.
Shiina K, Tomiyama H, Takata Y, Usui Y, Asano K, Hirayama Y, Nakamura T, Yamashina A . Concurrent presence of metabolic syndrome in obstructive sleep apnea syndrome exacerbates the cardiovascular risk: a sleep clinic cohort study. Hypertens Res 2006; 29: 433–441.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gao, J., Hua, Q., Li, J. et al. The incremental effect of obstructive sleep apnea syndrome on right and left ventricular myocardial performance in newly diagnosed essential hypertensive subjects. Hypertens Res 32, 176–181 (2009). https://doi.org/10.1038/hr.2008.22
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2008.22