Abstract
Purpose: To determine when, in reference to the course of their treatment, women with ovarian cancer are seen for genetic counseling, as well as to determine what factors influence this timing.
Methods: Single institution retrospective chart review of patients with ovarian cancer who underwent BRCA1/BRCA2 genetic testing.
Results: Thirty-three percent of our sample (n = 100) were seen for genetic counseling after ovarian cancer recurrence. In four cases, genetic test results were disclosed to next of kin. Thirty percent of women seen for genetic counseling after recurrence received their initial treatment elsewhere. Women with a history of breast cancer were significantly more likely to be seen for genetic counseling at an earlier phase of their treatment than women with no history of breast cancer.
Conclusion: We found that one third of patients with ovarian cancer who underwent genetic testing were seen for initial genetic counseling after disease recurrence. In some cases, genetic counseling took place during the end of life care, with genetic test results disclosed to next of kin. Given the poor prognosis of women with recurrent ovarian cancer, we advocate providing genetic counseling at the time of initial ovarian cancer treatment both in comprehensive cancer centers and in community oncology settings.
Similar content being viewed by others
Main
Ovarian cancer accounts for 3% of all cancers diagnosed in women. In 2008, an estimated 21,650 women were diagnosed with ovarian cancer.1 Approximately 8% to 15% of these ovarian cancers are attributable to a hereditary predisposition to breast and ovarian cancer caused by germ line mutation of the BRCA1 or BRCA2 gene.2–4 In addition, a small percentage of ovarian cancers are attributable to other hereditary cancer syndromes such as hereditary nonpolyposis colorectal cancer syndrome (Lynch syndrome). Genetic evaluation for Lynch syndrome should be considered for patients with ovarian cancer who have a suggestive personal and/or family history of colon, endometrial, or other Lynch-associated cancers. In contrast, a smaller percentage of breast, colorectal, and endometrial cancers are attributable to a hereditary predisposition; approximately 5% of breast cancers are attributable to BRCA1 or BRCA2,5 and approximately 2% of colorectal and endometrial cancers are attributable to Lynch syndrome.6–8
BRCA1/BRCA2 genetic testing of women with ovarian cancer has significant implications for both the patients with ovarian cancer and for family members. For the patient, a positive genetic test result indicates an increased risk for primary breast cancer, which may be particularly significant for patients with ovarian cancer who were diagnosed at an early stage and/or are long-term survivors. A growing body of evidence also indicates that patients with ovarian cancer with BRCA mutations have improved survival when compared with patients with sporadic ovarian cancers.9–13
For family members, the information gained from genetic testing of their relative with ovarian cancer is of utmost importance. Once a BRCA1/BRCA2 mutation has been identified in a woman with ovarian cancer, her siblings, children, and other family members can be offered accurate predictive genetic testing for the known mutation. In the context of a known familial mutation, both positive and negative predictive genetic test results are interpretable and informative. Given the high risks of breast and ovarian cancer that are associated with BRCA1 and BRCA2, and the availability of proven risk reduction strategies, the potential benefit of predictive genetic testing is clear.
In contrast, if the patient with ovarian cancer does not undergo genetic testing, family members cannot be offered site-specific genetic testing for a known familial mutation. Family members may still elect to undergo comprehensive BRCA1/BRCA2 genetic testing in this case. However, in this scenario, the ability to interpret a negative result of comprehensive BRCA1/BRCA2 genetic testing for an individual unaffected by breast or ovarian cancer is limited. It could be that there is a detectable BRCA1/BRCA2 mutation in the family, and in this case the negative result would be reassuring. However, it is also possible that there is some other hereditary cause for the cancer(s) in the family (either an undetectable BRCA1/BRCA2 mutation or an entirely different hereditary cancer predisposition such as Lynch syndrome), and in this case the negative result would not be reassuring. Given this ambiguity, the preferable scenario is to first test a family member affected by cancer, then offer predictive genetic testing to at-risk relatives based on those results.
In addition, BRCA mutation status may, in the future, help dictate the course of treatment for ovarian cancer. Although the functions of BRCA1 and BRCA2 are incompletely understood, they do seem to play a role in double-stranded DNA break repair.14,15 BRCA1- or BRCA2-deficient tumors may be particularly responsive to a class of drugs known as poly (ADP-ribose) polymerase (PARP) inhibitors. PARP also facilitates DNA repair, and increased PARP activity has been observed in multiple tumor cell lines.16 PARP inhibitors are currently under study for their potential role as chemotherapeutic agents both as single agents and as potentiators.16 PARP inhibition sensitizes tumor cells to cytotoxic therapy and radiation therapy.16 Cells deficient in BRCA1/BRCA2 seem to be especially sensitive to PARP inhibition; in these cells, a PARP inhibitor alone can cause cell-cycle arrest and apoptosis.17,18 The prospect of therapy tailored to BRCA-deficient cancers has therefore been raised and is currently under study.
Women with ovarian cancer, therefore, comprise a unique population in which consideration of genetic testing is especially important both because the yield is high and because the implications of the genetic test results are so significant. Unfortunately, the window of opportunity for offering genetic testing is limited in many cases. Sixty-three percent of ovarian cancers are diagnosed at Stage III or IV.19 The 5-year survival rates for Stages III and IV ovarian cancers are 15% to 20% and <5%, respectively.19 These late-stage ovarian cancers frequently recur, and the overall prognosis for women with recurrent ovarian cancer remains poor. Response rates for treatment of recurrent ovarian cancer range from 12% to 60%, with median survival ranging from 9 to 12 months.20 Given this limited window of opportunity, consideration should be given to when, during this disease course, genetic testing should be offered. We, therefore, sought to determine when, in reference to the course of their treatment, women with ovarian cancer are being seen for genetic counseling, as well as to determine what factors influence when patients are seen for genetic counseling.
MATERIALS AND METHODS
Through retrospective chart review, we identified a total of 100 women who both underwent some or all of their treatment for ovarian, fallopian tube, or primary peritoneal cancer at our institution, and had BRCA1/BRCA2 genetic testing, from 1998 to 2006, at our institution. Women who underwent genetic counseling, but did not have genetic testing at our institution during the study period, were not included in this study (n = 32). Data collected from the medical records included demographics, information related to ovarian cancer diagnosis and treatment, other personal history of cancer, dates of genetic counseling and genetic testing, and results of genetic testing. The study protocol was reviewed and approved by the U.T. M.D. Anderson Cancer Center's Institutional Review Board.
We defined the initiation of the genetic testing process as the date of the initial genetic counseling visit. We then classified this date as occurring during one of three treatment phases: “initial treatment” was defined as before or during initial surgery and chemotherapy; “during first remission” was defined as after initial therapy was completed and before any recurrence; and “recurrence” was defined as at or after first recurrence of ovarian cancer. These phases are delineated by two clinically significant benchmark events in the treatment course, which are the end of initial treatment and the recurrence of ovarian cancer. During the initial treatment phase, family history is assessed during the primary medical evaluation, and patients have frequent interactions with the health care team. Once initial treatment is completed, the patient is in remission and is seen for follow-up less frequently. The length of remission varies greatly from patient to patient, but once ovarian cancer has recurred, at that point life span is limited and the window of opportunity for genetic testing may, therefore, be short.
Summary statistics for age at diagnosis, stage of ovarian cancer, area of residence, history of breast cancer, genetic test results, and year of initial genetic counseling were calculated by treatment phase at the time of genetic counseling. Fisher exact test was used to determine whether any of these factors were associated with treatment phase at the time of genetic counseling. The Cochran-Armitage trend test was used to further examine the relationship of a history of breast cancer to treatment phase at the time of genetic counseling.
RESULTS
Demographic summary statistics are presented in Table 1. Of note, 45 of 100 (45%) patients with ovarian cancer who underwent genetic testing tested positive for a BRCA1 or BRCA2 mutation. Median age at ovarian cancer diagnosis for the whole sample was 55.
Women were equally likely to be seen for genetic counseling during each of the treatment phases: 33 of 100 (33%) were seen before or during their initial treatment for ovarian cancer, 34 of 100 (34%) were seen during first remission, and 33 of 100 women (33%) were not seen for genetic counseling until recurrence of ovarian cancer.
Of the 33 women seen for genetic counseling after recurrence, four genetic test results (12%) were disclosed to next of kin instead of the patient herself. In three of these cases, the patient died of ovarian cancer before genetic test results could be disclosed. The fourth patient had end-stage disease and felt too unwell to discuss the genetic test results, therefore requested that her results be discussed with her next of kin; she died shortly thereafter. All four women had progressive recurrent ovarian cancer at the time of initial genetic counseling. Ten of 33 (30%) women seen for genetic counseling after recurrence had first presented at our institution with recurrent ovarian cancer, after receiving their initial treatment elsewhere.
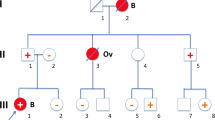
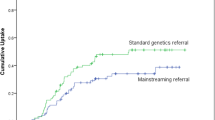
By Fisher exact test, history of breast cancer versus no history of breast cancer did differ significantly by treatment phase at the time of genetic counseling (P = 0.0417, Table 1). Women with a history of breast cancer were seen for genetic counseling significantly earlier in the course of their treatment than women with no history of breast cancer (P = 0.0146 for trend by Cochran-Armitage test, Fig. 1). Age at diagnosis of ovarian cancer, area of residence (local to the institution vs. nonlocal), year of initial genetic counseling, and genetic test results (positive vs. negative or variant of uncertain significance) did not differ significantly between the treatment phases at the time of genetic counseling. Ovarian cancer stage did differ significantly by treatment phase at the time of genetic counseling (P = 0.0379 by Fisher exact test, Table 1).
DISCUSSION
During the study period, there were no standard procedures at our institution regarding referral of patients with ovarian cancer for hereditary cancer risk assessment and genetic counseling. In our study population, we found an even distribution of time of initial genetic counseling in reference to phase of ovarian cancer treatment. One third of our study population was not seen for genetic counseling until their ovarian cancer had recurred.
Once ovarian cancer has recurred, it is difficult to estimate life expectancy, and death can occur suddenly with little or no previous warning.21 Both physicians and patients tend to overestimate life expectancy in this situation.20,22 Among our study patients seen for genetic counseling after ovarian cancer recurrence, four genetic test results were disclosed directly to next of kin because the patients had died or were near death. Our study included only women who underwent BRCA1/2 genetic testing, and as such we cannot directly address the question of how many patients may have died before genetic testing could be performed. However, our findings do highlight the potential pitfalls of delaying genetic testing, given the limited and unpredictable life span of women with recurrent progressive ovarian cancer.
Women with recurrent ovarian cancer, their families, and their health care teams are confronted with many difficult issues. BRCA1/BRCA2 genetic testing poses its own challenges for patients and their families. Disclosing the genetic test results to at-risk family members can be a time consuming and emotionally laden process for the patient, and patients can experience feelings of guilt regarding the possibility of passing on to their children a hereditary predisposition to breast and ovarian cancer.23 Patients faced with both of these sets of challenges simultaneously could become overwhelmed. Genetic testing could get lost in the shuffle of complicated medical care and other immediate decisions that need to be made. Given the significant implications of the genetic test results, we believe that patients would be better served if genetic counseling is provided before ovarian cancer recurrence.
Oncology care is provided both in comprehensive cancer centers and in community-based settings, but cancer genetics clinics tend to be affiliated with comprehensive cancer centers. We found that, of the 33 patients seen for genetic counseling after recurrence of their ovarian cancer, 10 of them had received their primary treatment elsewhere and were referred to our institution (a comprehensive cancer center) for management of recurrent ovarian cancer. To make BRCA genetic testing accessible to women during their initial ovarian cancer treatment, cancer genetic counseling services would need to be available both in community oncology settings and at comprehensive cancer centers.
Women who have had both breast and ovarian cancer are at high risk to have a BRCA1/2 mutation, and hereditary cancer guidelines recommend genetic counseling for any woman who has had both breast and ovarian cancer.24,25 We found that patients with ovarian cancer who had a history of breast cancer were significantly more likely to have been seen for genetic counseling earlier in the course of their treatment than women who had no personal history of breast cancer. Because women who have had both cancers can be flagged as high risk based on personal history alone, they may have been recognized as appropriate for genetic counseling referral more quickly. However, we did not find that all the women at highest risk to have a BRCA mutation were seen earlier in the course of their treatment, as evidenced by the fact that we found no association between positive genetic test results and phase of treatment at the time of genetic counseling.
We did find that ovarian cancer stage was significantly associated with treatment phase at the time of genetic counseling. However, we feel that this is unlikely to reflect a causal association, but is instead a reflection of the different disease process at different stages. Fewer women with Stage I or II ovarian cancer had genetic counseling at or after recurrence; they are also unlikely to recur at all. Women with Stage III ovarian cancer were seen with an even distribution through the three treatment phases. The small number (n = 12) of women with Stage IV ovarian cancer were seen either during initial treatment or at recurrence.
Limitations
As illustrated by the 45% who tested positive for a BRCA mutation, our study population was a high-risk sample. We studied only women who had been seen for genetic counseling and underwent genetic testing, and therefore the high mutation detection rate can be attributed to referral bias. It is possible that our findings may not be generalizable to a lower-risk population. We also do not know the reasons why women were seen later in the course of their treatment for genetic counseling, and it is possible that they were referred for genetic counseling sooner and chose not to pursue it at that time.
CONCLUSION
We found that one third of patients with ovarian cancer received genetic counseling after disease recurrence. In some of these cases, genetic counseling took place during the end of life care, with genetic test results disclosed directly to next of kin. Given the poor prognosis of women with recurrent ovarian cancer, we believe that genetic counseling should be offered to patients with ovarian cancer at risk for hereditary breast and ovarian cancer at the time of their initial diagnosis and treatment both in comprehensive cancer centers and in community oncology settings.
REFERENCES
American Cancer Society Cancer facts and figures 2008. Atlanta: American Cancer Society, 2008.
Malander S, Ridderheim M, Masback A, et al. One in 10 ovarian cancer patients carry germ line BRCA1 or BRCA2 mutations: results of a prospective study in Southern Sweden. Eur J Cancer 2004; 40: 422–428.
Pal T, Permuth-Wey J, Betts JA, et al. BRCA1 and BRCA2 mutations account for a large proportion of ovarian carcinoma cases. Cancer 2005; 104: 2807–2816.
Risch HA, McLaughlin JR, Cole DE, et al. Prevalence and penetrance of germline BRCA1 and BRCA2 mutations in a population series of 649 women with ovarian cancer. Am J Hum Genet 2001; 68: 700–710.
Malone KE, Daling JR, Doody DR, et al. Prevalence and predictors of BRCA1 and BRCA2 mutations in a population-based study of breast cancer in white and black American women ages 35 to 64 years. Cancer Res 2006; 66: 8297–8308.
Hampel H, Frankel W, Panescu J, et al. Screening for Lynch syndrome (hereditary nonpolyposis colorectal cancer) among endometrial cancer patients. Cancer Res 2006; 66: 7810–7817.
Hampel H, Frankel WL, Martin E, et al. Screening for the Lynch syndrome (hereditary nonpolyposis colorectal cancer). N Engl J Med 2005; 352: 1851–1860.
Hampel H, Panescu J, Lockman J, et al. Comment on: screening for lynch syndrome (hereditary nonpolyposis colorectal cancer) among endometrial cancer patients. Cancer Res 2007; 67: 9603.
Ben David Y, Chetrit A, Hirsh-Yechezkel G, et al. Effect of BRCA mutations on the length of survival in epithelial ovarian tumors. J Clin Oncol 2002; 20: 463–466.
Boyd J, Sonoda Y, Federici MG, et al. Clinicopathologic features of BRCA-linked and sporadic ovarian cancer. JAMA 2000; 283: 2260–2265.
Cass I, Baldwin RL, Varkey T, Moslehi R, Narod SA, Karlan BY . Improved survival in women with BRCA-associated ovarian carcinoma. Cancer 2003; 97: 2187–2195.
Chetrit A, Hirsh-Yechezkel G, Ben-David Y, Lubin F, Friedman E, Sadetzki S . Effect of BRCA1/2 mutations on long-term survival of patients with invasive ovarian cancer: the National Israeli study of ovarian cancer. J Clin Oncol 2008; 26: 20–25.
Rubin SC, Benjamin I, Behbakht K, et al. Clinical and pathological features of ovarian cancer in women with germ-line mutations of BRCA1. N Engl J Med 1996; 335: 1413–1416.
Venkitaraman AR . Cancer susceptibility and the functions of BRCA1 and BRCA2. Cell 2002; 108: 171–182.
Yoshida K, Miki Y . Role of BRCA1 and BRCA2 as regulators of DNA repair, transcription, and cell cycle in response to DNA damage. Cancer Sci 2004; 95: 866–871.
Ratnam K, Low JA . Current development of clinical inhibitors of poly(ADP-ribose) polymerase in oncology. Clin Cancer Res 2007; 13: 1383–1388.
Bryant HE, Schultz N, Thomas HD, et al. Specific killing of BRCA2-deficient tumours with inhibitors of poly(ADP-ribose) polymerase. Nature 2005; 434: 913–917.
Farmer H, McCabe N, Lord CJ, et al. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature 2005; 434: 917–921.
Ozols RF, Rubin SC, Thomas GM, Robboy SJ . Epithelial ovarian cancer. In: Hoskins WJ, Perez CA, Young RC, Barakat R, Markman M, Randall M, editors. Principles and practice of gynecologic oncology, 4th ed. Philadelphia: Lippincott Williams and Wilkins, 2005: 895–988.
Doyle C, Crump M, Pintilie M, Oza AM . Does palliative chemotherapy palliate? Evaluation of expectations, outcomes, and costs in women receiving chemotherapy for advanced ovarian cancer. J Clin Oncol 2001; 19: 1266–1274.
von Gruenigen VE, Frasure HE, Reidy AM, Gil KM . Clinical disease course during the last year in ovarian cancer. Gynecol Oncol 2003; 90: 619–624.
Vigano A, Dorgan M, Bruera E, Suarez-Almazor ME . The relative accuracy of the clinical estimation of the duration of life for patients with end of life cancer. Cancer 1999; 86: 170–176.
van Oostrom I, Meijers-Heijboer H, Duivenvoorden HJ, et al. A prospective study of the impact of genetic susceptibility testing for BRCA1/2 or HNPCC on family relationships. Psychooncology 2007; 16: 320–328.
Lancaster JM, Powell CB, Kauff ND, et al. Society of Gynecologic Oncologists Education Committee statement on risk assessment for inherited gynecologic cancer predispositions. Gynecol Oncol 2007; 107: 159–162.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in OncologyTM: Genetic/familial high risk assessment: breast and ovarian. VI: National Comprehensive Cancer Network, 2008.
Acknowledgements
This project was supported, in part, by The Lynne Cohen Foundation for Ovarian Cancer Research.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure: The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Daniels, M., Urbauer, D., Stanley, J. et al. Timing of BRCA1/BRCA2 genetic testing in women with ovarian cancer. Genet Med 11, 624–628 (2009). https://doi.org/10.1097/GIM.0b013e3181ab2295
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e3181ab2295
Keywords
This article is cited by
-
Clinical implementation of an oncology‐specific family health history risk assessment tool
Hereditary Cancer in Clinical Practice (2021)
-
Genetics in palliative oncology: a missing agenda? A review of the literature and future directions
Supportive Care in Cancer (2018)
-
Selecting Patients with Ovarian Cancer for Germline BRCA Mutation Testing: Findings from Guidelines and a Systematic Literature Review
Advances in Therapy (2016)
-
Genetic Risk Assessment for Women with Epithelial Ovarian Cancer: Referral Patterns and Outcomes in a University Gynecologic Oncology Clinic
Journal of Genetic Counseling (2013)
-
A clinical perspective on genetic counseling and testing during end of life care for women with recurrent progressive ovarian cancer: opportunities and challenges
Familial Cancer (2011)