Abstract
Purpose: To evaluate the impact of acquired and inherited factors on the development of lipodystrophic syndrome in patients on highly active antiretroviral therapy.
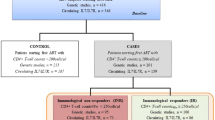
Methods: Two hundred forty-three human immunodeficiency virus-infected Caucasians on highly active antiretroviral therapy were prospectively followed-up for 3 years. Eleven were naÍve and 232 were on antiretrovirals (mean, 93.0 months ± 43.8 months). Lipodystrophic syndrome was diagnosed clinically with a lipodystrophy severity grading scale. Polymorphisms of cytokines (IL-1β, IL-6, TNF-α), TLR4, and NOS genes were genotyped.
Results: Ninety (37%) patients developed lipodystrophic syndrome. The polymorphic T allele of the (+3954C/T) polymorphism of IL-1β was less frequent in patients with lipodystrophic syndrome compared with those without (17.8% vs. 27.0%, P = 0.03). Factors significantly associated with lipodystrophic syndrome were time on stavudine (P < 0.001), use of stavudine (P = 0.001), absence of the T allele of the (+3954C/T) IL-1β polymorphism (P = 0.02), acquired immune deficiency syndrome diagnosis (P = 0.005), nadir levels of CD4 (P = 0.003), and time on highly active antiretroviral therapy (P = 0.003). Of these factors, only the time on stavudine (hazard ratio [95% confidence intervals] 1.007 [1.001–1.013]), use of stavudine (1.678 [1.048–2.68]), and absence of the T allele of the IL-1β (+3954C/T) polymorphism (0.569 [0.347–0.931]) were significantly associated with lipodystrophic syndrome by Cox regression.
Conclusions: Genotyping of the (+3954C/T) polymorphism of IL-1β could be useful in patients starting highly active antiretroviral therapy, especially in potential users of stavudine, to predict their risk of developing lipodystrophic syndrome.
Similar content being viewed by others
Main
Lipodystrophic syndrome (LD) is a frequent medical condition found in human immunodeficiency virus (HIV)-infected patients, characterized by redistribution of body fat (lipoatrophy and fat accumulation) and metabolic abnormalities (hyperlipidemia, insulin resistance, and hyperlactatemia). Different studies have reported a variable prevalence of LD in HIV-infected patients on highly active antiretroviral therapy (HAART), between 17% and 75%, probably due to clinical variability in the diagnosis of LD.1–8 LD is considered an inflammatory syndrome and is associated with increased serum cytokine levels.9–11 High serum levels of cytokines have also been observed in HIV-related wasting syndrome, similar in its adipose tissue alterations to the lipoatrophic form of LD.12,13
Early reports associated LD with the use of different protease inhibitors,1,2 while later reports linked LD to thymidine nucleoside analogue use that produced mitochondrial toxicity, hyperlactatemia, and lipoatrophy.14–17 LD improves after antiretroviral change, mostly after the switching of protease inhibitors or stavudine to a non-nucleoside reverse transcriptase inhibitor.18,19 Thus, the association between antiretrovirals and LD seems clear. However, factors other than antiretrovirals could influence the development of LD, for example, sex of the patient.20 In addition, there is support for a role of a genetic background of patients in the development of LD: (1) there are some congenital syndromes, not related to HIV infection that are associated with LD21; (2) only some of the HIV-infected patients on HAART develop LD, despite receiving the same therapy1–8; (3) some patients naÍve for antiretrovirals develop LD; and (4) recent works have shown some association between the TNF-α (−238) promoter polymorphism and the development of LD.22–24
In addition to LD, HIV-infected patients who are carriers of the TNF-α (−238) and (−308) promoter polymorphisms have a higher susceptibility to developing HIV-associated dementia, and these polymorphisms could play some role in the evolution of HIV infection as well.25 Polymorphisms of other cytokines have also been associated with susceptibility to, or protection against, HIV and other infections.26,27
The presence of the HIV gp120 protein stimulates both the nonadaptive immune response with release of IL-1 and TNF-α, and the toll-like receptors (TLRs) of the surface of monocytes and macrophages, contributing through nuclear factor κ B activation to the transcription of HIV and to the expression of cytokines.28 Polymorphisms of the TLR 2, 4, and 9 genes have been associated, in addition to HIV infection, with a predisposition to different infections by Gram-positive bacteria (TLR2) or Gram-negative bacteria (TLR4).29–32
Nitric oxide (NO) is a free-radical gas that has an important contribution to the host defense against different microorganisms including HIV. NO is formed by the action of NO synthase (NOS). There are three isoforms of the NOS family: endothelial (eNOS or NOS3), neuronal (nNOS or NOS1), and inducible (iNOS or NOS2).33 Different polymorphisms of NOS have been associated with abnormal serum levels of NO as well as with susceptibility or protection against infections,34,35 although an association between HIV infection pathogenesis or LD and NOS polymorphisms has so far not been found.36
Because the etiology of LD remains elusive and its consequences are so important for HIV-infected patients, the genetic background, which could play a critical role in LD pathogenesis, merits further evaluation. In the present work, we have analyzed the incidence of LD in 243 HIV-infected Caucasian patients on HAART followed for at least 3 years. In addition, we have studied different demographic, clinical, analytical, and therapeutic factors and their possible association with LD. Finally, we have analyzed a possible association between LD and different polymorphisms of cytokines, TLRs, and NOS.
MATERIALS AND METHODS
Study population
HIV-infected patients at the Hospital Universitario Central de Asturias, Oviedo, Spain, were considered for this study. All patients had documented HIV-1 infection, were at least 16 years of age, and were already on HAART or started HAART at the time of enrollment in the study. Patients with adherence to HAART below 75% before and during the 3 years of follow-up were excluded from the study. Antiretrovirals could be changed during the study at the discretion of the attending doctor. Patients receiving drugs with metabolic effects (such as steroids, androgens, thyroid hormones and antithyroid agents, ketoconazole, cytotoxic drugs, and lipid-lowering agents) were excluded. Blood donors at the Blood Bank of Centro Comunitario de Transfusiones del Principado de Asturias, matched for age and sex with the patients, were used as controls for genetic and analytical studies.
LD diagnosis was based on body fat changes measured in every follow-up visit by a direct patient-self and doctor assessment, following a previously reported visit score.7,37,38 Briefly, the evaluation of body changes included enlarged abdomen, dorsocervical fat accumulation, breast fat accumulation, thinning of the arms, thinning of the legs, thinning of the hips/buttocks, and sunken cheeks or other facial changes (fat deposition over parotid glands, temporal wasting). All changes were graded, both subjectively (by report) and objectively (by examination), as “absent” (0 point), “subtle” (noticeable only if specifically looked for, no change in clothing fit) (1 point), “moderate” (easily noted by patient or physician, clothing has become tight or loose) (2 points), and “severe” (obvious to the casual observer, has required a change in clothing size) (3 points). The final severity rating for each sign was based on patient and physician agreement. Patients with a total score >7 of 28 were diagnosed with LD. In addition, patients with the severe sign were also diagnosed with LD independent of the total score. Once diagnosed, LD was further subdivided into lipoatrophic and lipohypertrophic, including the mixed forms into the lipoatrophic category. Patients were evaluated 4 times/yr. LD-associated metabolic abnormalities (total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, triglyceride levels, and insulin resistance) were also evaluated although were not included in the clinical LD score (these data have been published elsewhere7). Patients and controls were members of a homogeneous population, all Caucasians and residents of the same region (Asturias, Northern Spain). Each participant gave informed consent for the study, which was approved by the Ethics Committee of the Hospital Universitario Central de Asturias.
General metabolic assessments
CD4+ lymphocyte counts, HIV RNA viral load, total cholesterol, low-density lipoprotein and high-density lipoprotein cholesterol, triglycerides (all measured after a 12-hr overnight fast), as well as renal and liver tests, and other metabolic parameters were evaluated at the start of the study and every 3 months thereafter.
Genotypic analysis
Blood (10 mL) from HIV-infected patients and controls was collected in a tube containing potassium-EDTA. Genomic DNA was extracted from peripheral leukocytes following a salting-out method.39 Polymorphisms of cytokines [(−889C/T) IL-1α, (+3954C/T) IL-1β, (−174G/C) IL-6 and (−238G/A) and (−308G/A) TNF-α], TLR4 (Asp299Gly), NOS3 [(−27 bp repeat, intron 4), (−786T/C), (E298D)], and NOS2 (+37498G/A) were assessed by polymerase chain reaction (PCR) following the characteristics described in Table 1. The PCR results were confirmed by sequencing representative samples for each genotype of each polymorphism. PCR products were electrophoresed on a 2% low-melting agarose gel, the fragments were excised from the gel, purified with spin columns (DNA Gel Extraction Kit, Millipore, Billerica, MA), and sequenced on an ABI Prism 310 Genetic Analyser (Applied Biosystems, Foster City, CA).
Cytokine levels
Serum cytokine levels (IL-1β, IL-6, TNF-α) were measured by ELISA (R&D Systems Inc, MN). The limits of detection of each cytokine according to the manufacturer were as follows: IL-1β, 0–250 pg/mL; IL-6, 0–600 pg/mL; and TNF-α, 0–1000 pg/mL.
Serum nitrate and nitrite levels
Serum nitrate and nitrite (NOx) determinations were performed using the Griess reaction as previously described.40 Results were expressed as μM of NOx/sample.
Statistical analysis
The demographic and analytical variables were compared at baseline among the groups by analysis of variance for the quantitative variables and χ2 (Fisher exact test when appropriate) for the qualitative variables. The χ2 test was also used to compare allelic and genotypic frequencies between the groups. Odds ratios (ORs) and their 95% confidence intervals (CI) were also calculated. All the reported P values were two-sided. A P value <0.05 was considered significant. Only the significant variables at P < 0.05 in the univariate analysis were used for further LD predictive analysis. Cox proportional hazard models were also used to determine the multivariate factors associated with LD and its lipoatrophic and lipohypertrophic variants. The statistical analysis was performed using SPSS Software (Version 13.0, Chicago).
RESULTS
Study population
Two hundred forty-three HIV-infected patients were recruited between July 2002 and July 2003 and observed until July 2006. No missing patients were reported because those individuals with a show-up at the trimester revisions below 75% were excluded from the study. A total of 11 (4.5%) patients were naÍve for antiretrovirals and 232 (95.5%) were already on HAART for at least 36 months (mean, 64.6 months ± 36.5 months; range, 36–141), had received antiretrovirals previously in a pre-HAART era for even longer (mean, 93.0 months ± 43.8 months; range, 36–216), and 96 patients were on or had received stavudine. Ninety (37.0%) patients were diagnosed with LD, 65 (26.7%) in the lipoatrophic or mixed variants and 25 (10.3%) in the lipohypertrophic variant, at the end of the 3-year follow-up, whereas 153 (63.0%) patients did not develop LD.
The demographic, clinical, and analytical characteristics of the 243 HIV-infected patients and 300 individuals of the Blood Bank of Centro Comunitario de Transfusiones del Principado de Asturias, used as healthy controls, are described in Table 2. After comparing the different variables between HIV-infected patients with and without LD, those associated significantly with LD were a diagnosis of acquired immune deficiency syndrome (P = 0.0004), nadir CD4 cell count (P = 0.003), duration of HAART (P = 0.003), having received stavudine (P = 0.006), and duration of stavudine therapy (P < 0.0001).
Genotype study
All the cytokines, NOS, and TLR polymorphisms studied were in Hardy–Weinberg equilibrium in the HIV-infected patients with or without LD. Among the cytokine polymorphisms, carrying the polymorphic T allele of the (+3954C/T) polymorphism of IL-1β gene (17.8% vs. 27.0%, OR 1.68 [95%CI 1.03–2.77]; P = 0.03) and the (−889C/T) polymorphism of the IL-1α gene (22.8% vs. 34.6%, OR 1.75 [95%CI 1.12–2.75]; P = 0.013) were significantly associated with the absence of LD (Table 3). The heterozygous TC genotype of the polymorphism of IL-1 β and α genes were significantly less frequent in those patients with LD compared with those without (24.4% vs. 38.4%, OR 1.93 [95%CI 1.03–3.64]; P = 0.04 for the IL-1β gene polymorphism and 30.0% vs. 43.5%, OR 1.79 [95%CI 0.99–3.28]; P = 0.04 for the IL-1α gene polymorphism). No allelic or genotypic frequency differences between HIV-infected patients with and without LD or with the noninfected controls for the (−238G/A) and (−308G/A) promoter polymorphisms of the TNF-α (−174G/C) of IL-6 and (Asp299Gly) of the TLR4 genes were found (Table 3, other data not shown).
With regard to the NOS genes, no significant associations between the different polymorphisms studied and LD were observed. Interestingly, carriers of the CC genotype (23.2% vs. 14.3%, OR 1.81 [95%CI 1.13–2.90]; P = 0.012) and of the C allele of the (−786T/C) promoter polymorphism of NOS3 (51.3% vs. 37.2%, OR 1.78 [95%CI 1.38–2.30]; P < 0.0001) were significantly more frequent among HIV-infected patients compared with noninfected controls. Similar observations were found for carriers of the heterozygous genotypes of the E298D polymorphism of NOS3 and (+37498 G/A) polymorphism of NOS2.
Cytokines and NOx serum levels
HIV-infected patients with and without LD had similar levels of serum cytokines (Table 4). HIV-infected homozygous carriers of the TT genotype of the (+3954C/T) polymorphism of the IL-β gene had slightly lower serum levels of cytokines compared with patients with other genotypes of this polymorphism. Similar cytokine results were observed with the TT genotype of (−889C/T) of IL-1α and AA genotype of (−308G/A) promoter polymorphism of TNF-α gene when compared with HIV-infected patients with other genotypes of these polymorphisms (Table 4).
Patients without LD had minimally lower serum levels of nitrates-nitrites (NOx) than those with LD, and HIV-infected patients, with and without LD had significantly lower serum NOx levels compared with noninfected controls (Table 5). Furthermore, HIV-infected patients with the TT genotype of the (−786T/C) polymorphism of NOS3 had significantly lower serum NOx levels than healthy controls (P < 0.0001). Finally, serum NOx levels were similar in carriers of the different genotypes of the IL-1β (+3954C/T) polymorphism (Table 5).
Multivariate analysis
Using multivariate Cox proportional hazard models to study the variables that were significantly associated with LD, in the univariate analysis it was found that the total time on stavudine, the use of stavudine, and the absence of the T allele of the (+3954C/T) polymorphism of the IL-1β gene were the only variables independently associated with LD (Table 6). The enhancing or protective effect of lacking or having the polymorphic T allele of the (+3954C/T) polymorphism of the IL-1β gene on LD is shown graphically using Cox survival function curves in Figure 1,A andB. As can be seen in the figure, the LD-protective effect of the polymorphic T allele is more evident after longer exposure to antiretrovirals and did not seem to differ between carriers of the homozygous TT and heterozygous TC genotypes.
Cox survival function curves comparing the development of lipodystrophic syndrome (LD) over time (months of antiretroviral therapy), according to the presence or absence of the polymorphic T allele of the (+3954C/T) polymorphisms of IL-1β gene. In (A) carriers of the T allele (TT+TC) are represented together while in (B) all the TT, TC and CC genotypes are represented separately.
When we used multivariate Cox proportional hazard models to analyze the data, we found that the total time on stavudine (P = 0.0018, hazard ratio 1.010, 95% CI 1.004–1.016) was the only variable significantly associated with lipoatrophy, whereas the use of stavudine (P = 0.06) and the absence of the polymorphic T allele of the (+3954C/T) polymorphism of the IL-1β gene (P = 0.058) were at the limit of statistical significance. Regarding lipohypertrophy, we found that the only variable with a P value <0.1 was the absence of the polymorphic T allele of the (+3954C/T) polymorphism of the IL-1β gene (P = 0.052, hazard ratio 0.330, 95% CI 0.108–1.012).
DISCUSSION
In this study, we report for the first time that being a carrier of the polymorphic T allele of the (+3954C/T) polymorphism of the IL-1β gene had a protective effect against the development of LD in HIV-infected patients on HAART. This protective effect counterbalanced, at least partially, the well-known LD-inducing effect of stavudine, a thymidine nucleoside analogue that despite its strong antiviral potency has been relegated to a position of last choice or salvage-therapy nucleoside in the current HIV infection guidelines because of its severe lipoatrophic effect.8,41,42 Although the use of stavudine increased the risk for developing LD by 68%, the presence of the polymorphic T allele of the (+3954C/T) polymorphism of IL-1β gene decreased the risk to 43%. No differences in the protective effect against LD were observed between carriers of the homozygous TT or heterozygous TC genotypes of the (+3954) polymorphisms of the IL-1β gene, although a type II error cannot be dismissed due to the relatively low number of patients with the TT genotype. The strong association of the lack of the (+3954C/T) polymorphism of the IL-1β gene with LD in the multivariate analysis, but not of the (−889C/T) polymorphism of IL-1α, suggests that the effect of this IL-1α polymorphism is due to linkage disequilibrium with the (+3954C/T) polymorphism of the IL-1β gene, because both IL-1 α and β genes are located very closely in the long arm of chromosome 2.43 The protective effect of the polymorphic T allele of the (+3954C/T) polymorphism of IL-1β gene against LD was less evident after separating lipoatrophic from lipohypertrophic LD patients. This was most likely due to the lower number of patients in each of these groups, although this variable was at the limit of significance (P < 0.06). This suggests that the protective effect of this polymorphic T allele extends equally to two pathogenically different forms of LD and, consequently, it is not associated with a specific drug or pathogenic mechanism.
LD is considered an inflammatory syndrome and is associated with increased serum levels of cytokines such as TNF-α, IL-6, IL-1β,9 interferon-α,10 and IL-18.11 Therefore, different authors have studied the association of cytokine polymorphisms, especially TNF-α, and LD. Of them, only the (−238G/A) promoter polymorphism of the TNF-α gene was associated with the development of LD.22–24
Our results do not support these observations as we did not find any association between the TNF-α gene (−238G/A) or (−308G/A) promoter polymorphisms and LD despite genotyping a large Spanish Caucasian cohort, one of the largest HIV-infected populations genotyped from a single hospital. Our patients were on antiretrovirals for a longer period of time (mean, 93 months) than those of Maher et al.23 (96 HIV-infected Caucasians from the UK on antiretrovirals for 50 months) or Nolan et al.24 (220 HIV-infected Caucasians from Australia on antiretrovirals for 45 months). Interestingly, the frequency of the carriers of the heterozygous AG genotype among HIV-infected patients was similar in the three series (Maher et al., 8.3%; Nolan et al., 13.1%; and our cohort, 10.1%) and among patients with LD (Maher et al., 13.1% and our cohort, 9.7%). Whereas Maher et al. did not find the AG genotype among HIV-infected individuals without LD, we found this genotype in 9.7% of our patients (Nolan et al. does not report [−238G/A] TNF-α polymorphism genotypic data regarding LD status). This discordance could be due to clinical variability in the diagnosis of lesser forms of LD, perhaps less accurately diagnosed in our cohort using Lipodistrophy Severity Grading Scale (LSGS) compared with a different LD clinical scale reported by Maher et al.1,23 or with dual-energy x-ray absorptiometry (DEXA) scanning described by Nolan et al.
So far only cytokine polymorphisms that are inducers of LD were investigated, though there must be some mutations inducing and some protecting against LD. The polymorphic T allele of the (+3954C/T) polymorphism of the IL1-β gene showed a strong association against LD in the Cox multivariate analysis whereas the (−238) promoter polymorphism of the TNF-α gene and the other cytokine, TLR, and NOS polymorphisms genotyped showed no statistically significant association with LD. The (+3954C/T) IL-1β gene polymorphism TT genotype has been associated with an increased in vitro LPS-induced production of IL-1β by peripheral monocytes in insulin-dependent diabetic patients,44 but no changes in IL-1β serum levels were observed in carriers of this polymorphism in other large healthy Caucasian populations.45,46 Interestingly, in our study, the (+3954C/T) IL-1β gene polymorphism TT genotype was associated with low serum levels of TNF-α and other cytokines that are known to decrease body mass by increasing the subcutaneous adipocyte apoptosis in the HIV-related wasting syndrome and in the lipoatrophic form of LD.47 Therefore, low serum levels of cytokines could imply lower adipocyte apoptosis and lower LD. However, homozygous carriers of other cytokine polymorphisms also had low serum cytokine levels but did not show any protection against LD implying that the effect of the IL-1β gene polymorphism against LD could be due to other unknown factors.
HIV-infected patients had significantly lower serum NOx levels compared with healthy controls. HIV infection normally increases NOx serum levels; however, low NOx levels are observed in HIV-infected patients on HAART, as was the case for all the patients in our cohort.33 No clear association between the different NOS3 and NOS2 polymorphisms studied and LD was found. However, (−786T/C) promoter and (E298D) exon 7 polymorphisms of the NOS3 gene and (+37498G/A) of the NOS2 gene were significantly more frequent among HIV-infected patients compared with controls. The reason for this association is not clear. We did not find any significant association between NOx serum levels and any NOS2 or NOS3 polymorphism. This fact does not support a hypothesis based on the effect of the NOx increase on HIV-infection, which needs further research. In addition, because healthy controls in our cohort were probably never exposed to HIV infection being volunteer blood donors, we cannot conclude that a specific polymorphism in the NOS gene enhances or protects against HIV infection.
Recent reports emphasize the value of the genetic background in the response to different antiretrovirals or to HIV infection. It was observed that abacavir and nevirapine sensitivity were related to the HLA genes (HLA-B*5701 and HLA-DRB1*0101).48,49 Genetic variations could also influence the response against HIV infection (CCR5delta32) and perhaps could predispose or protect against LD as well.50
Limitations of our study include the lack of an objective standardized measurement of LD by image techniques (DEXA or computed tomography) that we replaced by LSGS. However, the LSGS we used has proved to be valuable in diagnosing moderate to severe LD. In addition, LSGS showed a good correlation with anthropometric and echographic measurements of subcutaneous and visceral fat thickness for diagnosis of LD in HIV-infected patients.38 Finally, although there could be some LD adscription mistakes, errors would randomly affect patients with and without the (+3954C/T) polymorphism of the IL-1β gene and, expectedly, the results would not be substantially modified.
Although caution is needed due to the relatively small number of our Caucasian-only cohort—and our findings need to be validated in larger populations of other ethnic backgrounds—our results suggest that genotyping the (+3954 C/T) IL-1β gene polymorphism could be helpful for evaluation of the risk of developing LD and for tailoring antiretroviral therapy to each patient's risk. In this context, stavudine, even with its potential mitochondrial toxicity, could be introduced at an earlier time of HAART in carriers of the polymorphic T allele of the (+3954 C/T) IL-1β gene polymorphism, because these individuals will have a lower probability of developing LD due to this thymidine analogue.
References
Carr A, Samaras K, Burton S, Law M, et al. A syndrome of peripheral lipodystrophy, hyperlipidaemia and insulin resistance in patients receiving HIV protease inhibitors. AIDS 1998; 12: F51–F58.
Martinez E, Mocroft A, Garcia-Viejo MA, Perez-Cuevas JB, et al. Risk of lipodystrophy in HIV-1 infected patients treated with protease inhibitors: a prospective cohort study. Lancet 2001; 357: 592–598.
Carr A . HIV lipodystrophy: risk factors, pathogenesis, diagnosis and management. AIDS 2003; 7: S141–S148.
Lichtenstein KA . Redefining lipodystrophy syndrome: risks and impact on clinical decision making. J Acquir Immune Defic Syndr 2005; 39: 395–400.
Milinkovic A, Martinez E . Current perspectives on HIV-associated lipodystrophy syndrome. J Antimicrob Chemother 2005; 56: 6–9.
Grinspoon S, Carr A . Cardiovascular risk and body-fat abnormalities in HIV-infected adults. N Engl J Med 2005; 352: 48–62.
Asensi V, Martin-Roces E, Carton JA, Collazos J, et al. Perirenal fat diameter measured by echography could be an early predictor of lipodystrophy in HIV-infected patients receiving highly active antiretroviral therapy. Clin Infect Dis 2004; 39: 240–247.
Carr A, Miller J, Law M, Cooper DA . A syndrome of lipoatrophy, lactic acidaemia and liver dysfunction associated with HIV nucleoside analogue therapy: contribution to protease inhibitor-related lipodystrophy syndrome. AIDS 2000; 14: F25–F32.
Johnson J, Albu JB, Engelson ES, Fries SK, et al. Increased systemic and adipose tissue cytokines in patients with HIV-associated lipodystrophy. Am J Physiol Endocrinol Metab 2004; 286: 261–271.
Christeff N, Melchior JC, de Truchis P, Perronne C, et al. Increased serum interferon alpha in HIV-1 associated lipodystrophy syndrome. Eur J Clin Invest 2002; 32: 43–50.
Lindegaard B, Hansen AB, Gerstoft J, Pedersen BK . High plasma level of interleukin-18 in HIV-infected subjects with lipodystrophy. J Acquir Immune Defic Syndr 2004; 36: 588–593.
Belec L, Meillet D, Gresenguet G, Gherardi RK . Increased tumor necrosis factor-alpha serum levels in patients with HIV wasting syndrome and euthiroid sick syndrome. J Acquir Immune Defic Syndr Hum Retrovirol 1995; 8: 212–214.
Constans J, Pellegrin I, Pellegrin JL, Peuchant E, et al. Plasma interferon alpha and the wasting syndrome in patients infected with the human immunodeficiency virus. Clin Infect Dis 1995; 20: 1069–1070.
Brinkman K, Smeitink JA, Romijn JA, Reiss P . Mitochondrial toxicity induced by nucleoside-analogue reverse-transcriptase inhibitors is a key factor in the pathogenesis of antiretroviral-therapy-related lipodystrophy. Lancet 1999; 354: 1112–1115.
Cherry C, Gahan ME, McArthur JC, Lewin SR, et al. Exposure to dideoxynucleosides is reflected in lowered mitochondrial DNA in subcutaneous fat. J Acquir Immune Defic Syndr 2002; 30: 271–277.
Shikuma CM, Hu N, Milne C, Yost F, et al. Mitochondrial DNA decrease in subcutaneous adipose tissue of HIV-infected individuals with peripheral lipoatrophy. AIDS 2001; 15: 1801–1809.
Nolan D, Hammond E, Martin A, Taylor L, et al. Mitochondrial DNA depletion and morphologic changes in adipocytes associated with nucleoside reverse transcriptase inhibitor therapy. AIDS 2003; 17: 1329–1338.
Martinez E, Conget I, Lozano L, Casamitjana R, et al. Reversion of metabolic abnormalities after switching from HIV-protease inhibitors to nevirapine. AIDS 1999; 13: 805–810.
Carr A, Workman C, Smith DE, Hoy J, et al. Abacavir substitution for nucleoside analogs in patients with HIV lipoatrophy: a randomized trial. JAMA 2002; 288: 207–215.
Galli M, Veglia F, Angarano G, Santambrogio S, et al. Gender differences in antiretroviral drug-related adipose tissue alterations. Women are at higher risk than men and develop particular lipodystrophy patterns. J Acquir Immune Defic Syndr 2003; 34: 58–61.
Magré J, Delepine M, Khallouf E, Gedde-Dahl T Jr . et al. Identification of the gene altered in Beradinelli-Seip congenital lipodystrophy on chromosome 11q13. Nat Genet 2001; 28: 365–370.
Nolan D, John M, Mallal S . Antiretroviral therapy and the lipodystrophy syndrome, part 2: concepts in aetiopathogenesis. Antivir Ther 2001; 6: 145–160.
Maher B, Alfirevic A, Vilar FJ, Wilkins EG, et al. TNFα promoter region gene polymorphisms in HIV-positive patients with lipodystrophy. AIDS 2002; 16: 2013–2018.
Nolan D, Moore C, Castley A, Sayer D, et al. Tumour necrosis factor-alpha gene −238 G/A promoter polymorphism associated with a more rapid onset of lipodystrophy. AIDS 2003; 17: 121–123.
Quasney MW, Zhang Q, Sargent S, Mynatt M, et al. Increased frequency of the tumor necrosis factor-alpha-308 A allele in adults with human immunodeficiency virus dementia. Ann Neurol 2001; 50: 157–162.
Brinkman BM, Keet IP, Miedema F, Verweij CL, et al. Polymorphisms within the human tumor necrosis factor-alpha promoter region in human immunodeficiency virus type 1-seropositive persons. J Infect Dis 1997; 175: 188–190.
Modi WS, Lautenberger J, An P, Scott K, et al. Genetic variation in the CCL-18-CCL3-CCL4 chemokine gene cluster influences HIV type 1 transmission and AIDS diseases progression. Am J Hum Genet 2006; 79: 120–128.
Bafica A, Scanga CA, Schito M, Chaussabel D, et al. Influence of coinfecting pathogens on HIV expression: evidence for a role of Toll-like receptors. J Immunol 2004; 172: 7229–7234.
Bochud PY, Hersberger M, Taffé P, Bochud M, et al. Polymorphisms in Toll-like receptor 9 influence the clinical course of HIV-1 infection. AIDS 2007; 10: 441–446.
Lorenz E, Mira JP, Cornish KL, Arbour NC, et al. A novel polymorphisms in the Toll-like receptor 2 gene and its potential association with staphylococcal infection. Infect Immun 2002; 68: 6398–6401.
Lorenz E, Mira JP, Frees KL, Schwartz DA . Relevance of mutations in the TLR receptor in patients with Gram-negative septic shock. Arch Intern Med 2002; 162: 1028–1032.
Montes AH, Asensi V, Alvarez V, Valle E, et al. The Toll-like receptor 4(Asp299Gly) polymorphisms is a risk factor for Gram negative and haematogenous osteomyelitis. Clin Exp Immunol 2006; 143: 404–413.
Torre D, Pugliese A, Speranza F . Role of nitric oxide in HIV-1 infection: friend or foe?. Lancet Infect Dis 2002; 2: 273–280.
MacMicking JD, North RJ, LaCourse R, Mudgett JS, et al. Identification of nitric oxide synthase as a protective locus against tuberculosis. Proc Natl Acad Sci USA 1997; 94: 5243–5248.
Asensi V, Montes AH, Valle E, Ocaña MG, et al. The NOS3 (27-bp repeat, intron 4) polymorphisms is associated with susceptibility to osteomyelitis. Nitric Oxide 2007; 16: 44–53.
Hersberger M, Bonhoeffer S, Rampini SK, Opravil M, et al. CCTTT-repeat polymorphisms of the inducible nitric oxide synthase is not associated with HIV pathogenesis. Clin Exp Immunol 2004; 137: 566–569.
Lichtenstein KA, Ward DJ, Moorman AC, Delaney KM, et al. Clinical assessment of HIV-associated lipodystrophy in an ambulatory population. AIDS 2001; 15: 1389–1398.
Asensi V, Martin-Roces E, Collazos J, Carton JA, et al. Association between physical and echographic fat thickness assessments and a lipodystrophy grading scale in lypodystrophic HIV patients. Practical implications. AIDS Res Hum Retroviruses 2006; 22: 830–836.
Miller SA, Dykes DD, Polesky HF . A simple salting-out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res 1988; 16: 1215–1222.
Giovannoni G, Land JM, Keir G, Thompson EJ, et al. Adaptation of the nitrate reductase and Griess reaction methods for the measurement of serum nitrate plus nitrite levels. Ann Clin Biochem 1997; 34: 193–198.
Mallal SA, John M, Moore CB, James IR, et al. Contribution of nucleoside analogue reverse transcriptase inhibitors to subcutaneous fat wasting in patients with HIV infection. AIDS 2000; 14: 1309–1316.
Hammer SM, Saag MS, Schechter M, Montaner JS, et al. Treatment for adult HIV infection: 2006 recommendations of the International AIDS Society–USA panel. JAMA 2006; 296: 827–843.
Nicklin MJ, Weith A, Duff GW . A physical map of the region encompassing the human interleukin-1 alpha, interleukin-1 beta, and interleukin-1 receptor antagonist genes. Genomics 1994; 19: 382–384.
Pociot F, Molvig J, Wogensen L, Worsaae H, et al. A TaqI polymorphism in the human interleukin-1 beta (IL-1beta) gene correlates with IL-1 beta secretion in vitro. Eur J Clin Invest 1992; 22: 396–402.
Hefler LA, Tempfer CB, Unfried G, Schneeberger C, et al. A polymorphism of the interleukin-1 beta gene and the idiopathic recurrent miscarriage. Fertil Steril 2001; 76: 377–379.
Wieser F, Hefler L, Tempfer C, Vlach U, et al. Polymorphism of the interleukin-1 beta gene and endometriosis. J Soc Gynecol Investig 2003; 10: 172–175.
Domingo P, Vidal F, Domingo JC, Veloso S, et al. Tumour necrosis factor alpha in fat redistribution syndrome associated with combination antiretroviral therapy in HIV-1 infected patients: potential role in subcutaneous adypocyte apoptosis. Eur J Clin Invest 2005; 35: 771–780.
Telenti A, Goldstein DB . Genomics meets HIV-1. Nat Rev Microbiol 2006; 4: 865–873.
Owen A, Pirmohamed M, Khoo SH, Back DJ . Pharmacogenetics of HIV therapy. Pharmacogenet Genomics 2006; 16: 693–703.
Brumme ZL, Harrigan PR . The impact of human genetic variation on HIV disease in the era of HAART. AIDS Rev 2006; 8: 78–87.
Acknowledgements
This study was supported by the research Grant SAF2007-64566, Programa Nacional de Biomedicina, Ministerio de Educación y Ciencia de España (to V.A.).
An abstract related to this article (abstract H-377) was presented at the 47th Intersciences Conference on Antimicrobial Agents and Chemotherapy, September 17–20, 2007, Chicago, USA.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure: The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Asensi, V., Rego, C., Montes, A. et al. IL-1β (+3954C/T) polymorphism could protect human immunodeficiency virus (HIV)-infected patients on highly active antiretroviral treatment (HAART) against lipodystrophic syndrome. Genet Med 10, 215–223 (2008). https://doi.org/10.1097/GIM.0b013e3181632713
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e3181632713
Keywords
This article is cited by
-
Pharmacogenomics and COVID-19: clinical implications of human genome interactions with repurposed drugs
The Pharmacogenomics Journal (2021)
-
Interleukin gene polymorphisms and susceptibility to HIV-1 infection: a meta-analysis
Journal of Genetics (2018)
-
IL-1β (−511T/C) gene polymorphism not IL-1β (+3953T/C) and LT-α (+252A/G) gene variants confers susceptibility to visceral leishmaniasis
Molecular Biology Reports (2012)